new vaccines for allergic rhinitis
advertisement

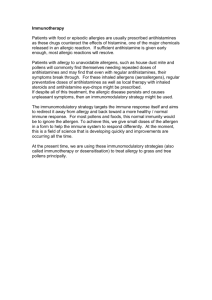
NEW VACCINES FOR ALLERGIC RHINITIS Jennifer Rolland Department of Pathology and Immunology, Monash University Medical School, Alfred Hospital, Melbourne. Allergic diseases are common, irritating and potentially life threatening conditions. Allergic rhinitis is usually induced by aeroallergens which are difficult to avoid. Thus pharmacotherapy to suppress the effects of inflammatory mediators is the mainstay therapy. Allergen-specific immunotherapy (SIT) is used in selected human patients with allergic disease and offers the advantage of being antigen-specific and potentially curative. SIT involves the subcutaneous injection of incremental doses of allergen extract to induce a state of clinical tolerance on reexposure to the allergen. SIT is termed by some a “negative vaccine”. However, despite having been used in clinical practice for several decades, its use remains empirical. Efficacy is only about 60-80% depending on the allergen and there is no laboratory test for monitoring clinical efficacy. Allergen injections are also associated with a significant risk of side effects due to IgEmediated reactions. The precise mechanisms of action of SIT and effective components within the allergen extracts are still to be delineated. A growing body of evidence indicates that clinical efficacy of SIT is associated with an altered allergen-specific T cell response. The CD4+ helper T cell is the key regulatory cell in the immune response to allergens. In allergic individuals, allergen-stimulated T cells produce IL-4 which drives B cell allergen-specific IgE production and IL-5 which promotes eosinophil differentiation, activation and survival. Following SIT, CD4+ T cell proliferative response to allergen is decreased and there is an increase in production of IFN-?, the predominant cytokine produced by non-allergic individuals in response to allergen challenge. Potential mechanisms by which CD4+ T cell responses are altered by SIT include anergy, deletion, immune deviation and induction of regulatory cell activity. Antigen dose, form and antigen presenting cell (APC) type have all been shown to influence T cell response and in particular, cytokine profile. Elucidation of mechanisms of SIT will lead to refinement in SIT allergen preparations and administration regimes. New approaches to SIT allergen preparations include the use of peptides based on dominant T cell epitopes of allergens and mutant allergens which have lost IgE binding activity but retained T cell reactive sites. These modified allergens will provide more rational SIT preparations and should improve safety of injection. Other strategies for refining SIT administration include the use of IFN-? inducing adjuvants. Bacterial proteins used either in conjunction with allergen injection or given as a fusion protein produced recombinantly have been explored in animal models with some success. Bacterial immunostimulatory DNA sequences (ISS) containing CpG motifs drive IL-12 production by antigen presenting cells thus also promoting IFN-? production by T cells. Adjunct treatment or recombinant approaches using ISS have also been examined in animal models. Finally the route of administration of SIT is under review. Standard regimes are given subcutaneously, but sublingual/oral and intranasal routes offer a more practical means of delivering the vaccine. Elucidation of delivery systems which provide the most effective antigen uptake from these sites is an important aspect to developing these new approaches to SIT. The development of more effective and safer strategies for delivering SIT will lead to its more wide-scale use and thus alleviation of the burden of allergic disease. References Bousquet J, Lockey R, Malling H-J. Allergen immunotherapy: Therapeutic vaccines for allergic diseases. J Allergy Clin Immunol 1998; 102:558-562 Burton MD, Blaher B, Suphioglu C, O’Hehir RE, Carbone FR, Rolland JM. T-cell receptor contact and MHC binding residues of a major rye grass pollen allergen T-cell epitope. J Allergy Clin Immunol 1999; 103:255-261 Hoyne GF, Jarnicki AG, Thomas WR, Lamb JR. Characterization of the specificity and duration of T cell tolerance to intranasally administered peptides in mice: a role for intramolecular epitope suppression. Int Immunol 1997; 9:1165-1173 Rolland JM, O’Hehir RE. Allergen immunotherapy: Anergy, deletion and immune deviation. Curr Opin Immunol 1998; 10:640-645 Smith AM, Chapman MD, Taketomi EA, Platts-Mills TA, Sung SS. Recombinant allergens for immunotherapy: a Der p 2 variant with reduced IgE reactivity retains T-cell epitopes. J Allergy Clin Immunol 1998; 101:423-425 Tighe H, Takabayashi K, Schwartz D, et al. Conjugation of immunostimulatory DNA to the short ragweed allergen Amb a 1 enhances its immunogenicity and reduces its allergenicity. J Allergy Clin Immunol 2000; 106:124-134 Figure: The CD4+ T cell orchestrates the immune response to allergen. New insight into factors influencing T cell cytokine response point to new allergen-specific intervention strategies for allergic disease.