Adding Clopidogrel to Aspirin Improves Outcome in STEMI Patients
advertisement

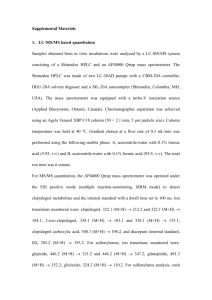
Adding Clopidogrel to Aspirin Improves Outcome in STEMI Patients Receiving Fibrinolytic Therapy CME News Author: Laurie Barclay, MD CME Author: Charles Vega, MD, FAAFP Disclosures To earn CME credit, read the news brief along with the CME information that follows and answer the post test questions. Release Date: March 10, 2005; Valid for credit through March 10, 2006 March 10, 2005 — The addition of clopidogrel to aspirin improves outcome in patients with acute ST-elevated myocardial infarction (STEMI) receiving fibrinolytic therapy, according to the results of a randomized study published in the March 9 Early Release issue of the New England Journal of Medicine. "A substantial proportion of patients receiving fibrinolytic therapy for myocardial infarction [MI] with ST-segment elevation have inadequate reperfusion or reocclusion of the infarct-related artery, leading to an increased risk of complications and death," write Marc S. Sabatine, MD, MPH, from the Brigham and Women's Hospital and Harvard Medical School in Boston, Massachusetts, and colleagues for the Clopidogrel as Adjunctive Reperfusion TherapyThrombolysis in Myocardial Infarction (CLARITY-TIMI) 28 Investigators. "Clopidogrel is an adenosine diphosphatereceptor antagonist, a class of oral antiplatelet agents that block the P2Y12 component of the adenosine diphosphate receptor and thus inhibit the activation and aggregation of platelets. Clopidogrel has been shown to prevent death and ischemic complications in patients with symptomatic atherosclerotic disease, patients who have undergone percutaneous coronary intervention, and patients with unstable angina or myocardial infarction without ST-segment elevation." The investigators enrolled 3,491 patients, 18 to 75 years of age, who presented within 12 hours after STEMI onset and randomized them to receive clopidogrel (300-mg loading dose followed by 75 mg once daily) or placebo. Patients were also treated with a fibrinolytic agent, aspirin, and heparin, when appropriate, based on body weight. Angiography was scheduled for 48 to 192 hours after the start of study medication. The primary efficacy end point, a composite of an occluded infarct-related artery (defined by a TIMI flow grade of 0 or 1) on angiography or death or recurrent MI before angiography, occurred in 21.7% of the placebo group and in 15.0% in the clopidogrel group. Absolute rate reduction was 6.7 percentage points, and clopidogrel therapy reduced the odds of the end point by 36% (95% confidence interval, 24%-47%; P < .001). By 30 days, the clopidogrel group had a 20% reduction in the odds of the composite end point of death from cardiovascular causes, recurrent MI, or recurrent ischemia leading to the need for urgent revascularization by 20% (from 14.1%-11.6%; P = .03). Both groups had similar rates of major bleeding and intracranial hemorrhage. "In patients 75 years of age or younger who have myocardial infarction with ST-segment elevation and who receive aspirin and a standard fibrinolytic regimen, the addition of clopidogrel improves the patency rate of the infarct-related artery and reduces ischemic complications," the authors write. "Still, the administration of a fibrinolytic agent in conjunction with heparin and two antiplatelet agents must be performed with caution." Study limitations include lack of power to detect a survival benefit; and exclusion of patients presenting more than 12 hours after symptom onset, those older than 75 years, and those with a history of coronary artery bypass grafting (CABG), limiting generalizability to these groups. Sanofi-Aventis, maker of clopidogrel, and Bristol-Myers Squibb supported this study in part and have various financial arrangements with some of its authors, some of whom also report various financial arrangements with the National Heart, Lung, and, Blood Institute, AstraZeneca, Merck, GlaxoSmithKline, Guilford Pharmaceuticals, Millennium, Pfizer, Schering-Plough, Vertex, Genentech, Guidant, and/or Eli Lilly. In an accompanying editorial, Richard A. Lange, MD, from Johns Hopkins University in Baltimore, Maryland, and L. David Hillis, MD, from the University of Texas Southwestern Medical Center, Dallas, discuss the limitations of aspirin, administered with or without fibrinolytic therapy, in MI. Drs. Lange and Hillis note several caveats concerning this study: the patient population appeared to be at relatively low risk; lack of enrollment of patients at increased risk of bleeding and those who had previously undergone CABG, preventing generalizing the findings to these groups; lack of data concerning the safety of CABG during clopidogrel therapy; and possible effect on the outcome of the timing of clopidogrel administration in the patients who underwent percutaneous coronary revascularization. "Because many patients are resistant to the effects of a single oral antiplatelet agent, therapy with multiple agents with different mechanisms of action is conceptually attractive, provided that it can be administered without an increased risk of bleeding," the authors write. "For patients who are receiving fibrinolytic therapy, a combination of clopidogrel and aspirin appears, in fact, to be effective and safe." N Engl J Med. Posted online March 9, 2005. Learning Objectives for This Educational Activity Upon completion of this activity, participants will be able to: List the limitations of aspirin in cardiovascular therapy. Specify outcomes improved when clopidogrel is added to standard treatment for MI. Clinical Context While aspirin therapy has proven to reduce the mortality associated with MI and is considered a cornerstone of therapy for patients with coronary artery disease, even this treatment has limitations. An editorial by Lange and Hillis that accompanies the current article describes some of these shortcomings. While aspirin irreversibly inhibits platelet cyclooxygenase, it does not impact other mechanisms of platelet aggregation such as thrombin or serotonin. The editorialists also note that up to 30% of patients with coronary artery disease will be relatively resistant to the benefits of aspirin as defined by laboratory or clinical criteria. Clopidogrel inhibits platelet aggregation through a different mechanism than aspirin, and the two agents can be synergistic for patients with coronary artery disease. The current study examines whether the addition of clopidogrel to standard treatment for MI offers clinical advantages. Study Highlights Study subjects were recruited from 319 sites in 23 countries. All subjects were between the ages of 18 and 75 years and had experienced ischemic discomfort within the previous 12 hours. Electrocardiographic criteria for study eligibility included ST-elevation of at least 1 mm in 2 contiguous limb leads, 2 mm in 2 contiguous precordial leads, or new left bundle branch block. Patients excluded from the trial included those with recent treatment with clopidogrel, those in whom angiography was planned within the first 48 hours of admission, and those with a prior CABG. Participants were assigned randomly to receive routine care plus clopidogrel, which was administered in a 300-mg loading dose followed by 75 mg daily or routine care plus matching placebo. All subjects were to receive a fibrinolytic agent, aspirin, and for those receiving a fibrin-specific lytic agent, heparin. Subjects underwent coronary angiography 48 to 192 hours after receiving the study medication. The primary end point was the composite of an occluded infarct-related artery on angiography, death from any cause prior to angiography, or recurrent MI prior to angiography. Safety data regarding bleeding also were assessed for both groups. Telephone follow-up was arranged at 30 days to quantify clinical and safety events. 3,491 subjects underwent randomization. Baseline characteristics and treatment for MI was similar between subjects in the clopidogrel and placebo groups. The mean age of participants was 57 years old, and 80% of subjects were men. 9% of subjects had experienced a previous MI. Approximately one in five participants did not receive heparin, and the median time from symptom onset to angiography was 84 hours. Participants in the clopidogrel group received a median of 4 doses prior to angiography. 94% of subjects underwent coronary angiography, and 57% had percutaneous coronary intervention. The rates of the primary end point were 21.7% in the placebo group and 15% in the clopidogrel group, a 36% odds reduction. While clopidogrel was superior in terms of artery occlusion and recurrent MI, it was not superior in preventing death prior to angiography. The overall benefit of clopidogrel was similar for all patient subgroups analyzed. Clopidogrel was associated with significant angiographic improvements compared with placebo, including improved optimal epicardial flow, optimal myocardial reperfusion, improved levels of stenosis, and larger luminal diameters of the infarct-related artery. Rates of ST-elevation resolution at 180 minutes were similar between groups. Clopidogrel reduced the need for early angiography and the need for urgent revascularization vs placebo. Clopidogrel was similar to placebo in outcomes of patients receiving percutaneous coronary intervention. At 30 days, the rates of the composite end point of death from cardiovascular causes, recurrent MI, and recurrent ischemia leading to urgent revascularization were 14.1% in the placebo group and 11.6% in the clopidogrel group, a 20% reduction. Again, clopidogrel did not afford a significant survival benefit vs placebo. The rates of major bleeding one day after angiography in the clopidogrel and placebo groups were 1.3% and 1.1%, respectively. Rates of minor bleeding were also similar between study groups. Pearls for Practice Aspirin can reduce mortality associated with MI, but it is limited in that it does not inhibit all mechanisms of platelet aggregation and is not as effective for all patients. Clopidogrel, when added to fibrinolysis as a treatment for MI, can improve the rate of artery patency and reduce ischemic complications when compared with standard therapy.