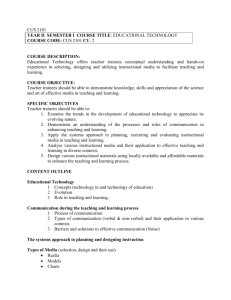
OCR Document - University of Illinois
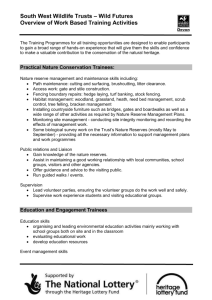
advertisement

August 30, 2004 TO: Robert Mrtek, Chair Senate Committee on Educational Policy FROM: Roger Nelson Assistant Vice Chancellor for Academic Affairs I am submitting for review and action by the Senate Committee on Educational Policy the attached proposal from the College of Medicine to establish the Center for Lung and Vascular Biology. In a memorandum dated February 12, 2004, Dr. Gerald Moss, Dean of the College of Medicine, endorsed the creation of the center. The proposal was originally submitted to the Graduate College Executive Committee in March 2004. The Executive Committee postponed action until additional information could be supplied by the proposed director, Dr. Asrar Malik. I am attaching to this letter Dr. Malik’s response to the Executive Committee. The proposal will be considered at the September 3 meeting of the Executive Committee, and I will report to SCEP at its meeting on September 9 the action taken by the Executive Committee. RN: Attachment Cc: C. Hulse w/o attachment R. Betts G. Moss w/o attachment M. Bailie w/o attachment C. Desjardins w/o attachment A. Malik w/o attachment D. Martinez w/o attachment D. Kellens w/o attachment Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Date: Wed, 25 Aug 2004 14:30:03 -0500 To: "Asrar B. Malik" <abmalik@uic.edu> From: Clark Hulse <chulse@uic.edu> Subject: Re: Center proposal Cc: Bcc: X-Attachments: One of the overall goals of the Center Lung and Vascular Biology as stated in the OBJECTIVES document (as applicable to the Graduate College Executive Committee) is to provide opportunities for the training of doctoral level students in the areas of lung and vascular biology. There is an on-going NIH funded training program in Lung Biology (Program Director A. B. Malik), which currently supports 5-6 doctoral level students trainees (annual budget of $510,000). This NIH program fully supports the stipends, tuition, and travel of these students who work in multiple labs under specific mentors. This program in the future will be integrated within the Center, and as such the program (because it is NIH supported) will provide the necessary infra-structure (such a administrative support) and resources to set up the program in the context of the Center. It is expected being connected with the Center will greatly help in making this program even more competitive and enabling us to recruit trainees (such as MD's finishing their residency training) who may otherwise would have been attracted to this program. Thus, only significant benefits can accrue from having program associated with the Center. Asrar =================================================================== ======== Asrar B. Malik, Distinguished Professor and Head, Pharmacology PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. REQUEST FOR NEW ADMINISTRATIVE, RESEARCH OR PUBLIC SERVICE UNIT BACKGROUND 1. Name of Institution: University of Illinois at Chicago 1. Title of Proposed Unit: Center for Lung and Vascular Biology 3. CIP Code (6-digits): 4. Proposed Date for Initiation of Unit: Fall 2004 5. Contact Person: Dr. Charles Evans 5.1 Telephone 5.2 E-mail 5.3 Fax (217) 333-3079 cevans4@uillinois.edu (217) 244-5763 PURPOSE: OBJECTIVES MISSION AND PRIORITIES 6. Unit Objectives and Contributions 6.1. What are the goals and objectives of the new unit? 6.2. What is the relationship of the unit to the university's mission and priorities? Is the unit involved in instruction and, if so, to what extent? 6.3. What specific needs and measurable contributions will the unit make to statewide priorities and needs? 6.4. What is the demand for the unit's services? What clients or population will the unit serve? 7. Organization 7.1. Describe the proposed unit's organizational structure. 7.2. Explain how the unit is organized to meet its objectives. 4 Temporary approval may be sought through reasonable and moderate extension for creation of a new, formally organized, research or public service unit that bas a temporary mission up to five years. Following that time period, the institution must seek permanent approval if the unit continues operation. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. PURPOSE: OBJECTIVES, MISSION AND PRIORITIES 6. UNIT OBJECTIVES AND CONTRIBUTIONS 6.1 Goals and Objectives Overall Goals The following are the overal1 goals of the Center Lung and Vascular Biology: 1. To develop a center of excellence in the thematic area of lung and vascular biology. This will be accomplished by bringing together a multi-disciplinary group of investigators currently working in this thematic area as well as the recruitment of outstanding tenure-track faculty at the departmental and inter-departmental levels. To this end, the Center will recruit assistant professor level faculty and provide a supportive environment and start-up resources needed to develop research programs. Although the Center will be a new construct, its foundation will be the on-going vibrant research programs in lung and vascular biology; thus, the underlying premise is that the Center will capitalize on the existing strengths at UIC in lung and vascular biology research. 2. To have in place in the five-year time frame a nationally recognized and cohesive Center for Lung and Vascular Biology in which investigators are extramurally funded through NIH grants and through programmatic inter-disciplinary funding such as through the Program Project grant mechanism. 3. To promote the development of synergistic and inter-disciplinary research programs. Synergism is necessary so that the whole is greater than the sum of its parts and inter-disciplinary research is necessary because this will be a philosophical underpinning of the Center; that is, we believe that major and fundamental discoveries will be made at the boundary areas of science where two disciplines interact. Thus, the Center will foster interactive research in lung and vascular biology through multi-disciplinary and multi-departmental efforts. The Center will strive to develop interactions between basic science disciplines but also between basic sciences and clinical departments such as with the Division of Pulmonary and Critical Care Medicine in the Department of Medicine. 4. To train doctoral level students and post-doctoral fellows (Ph.D.s and M.D.s). The current NIH funded training program in Lung Biology (Program Director A. B. Malik), which supports 6 doctoral level students and 6 post-doctoral trainees (annual budget of $510,000) will provide the infra-structure and resources for the training programs of the Center. Specific Research Areas What kinds of research will the Center foster? The Center’s underlying approach will be to address clinically relevant or mechanistically-driven questions at molecular and cellular levels as well as at the integrated functional level. We believe that such a approach will be needed to provide a clear picture of the physiological as well as the disease processes; thus, the intent of the Center would be to go beyond the reductionist view. The emphasis of Center’s research programs will be to increase our understanding of specific disease processes at an integrated level. This will require PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. advanced experimental approaches in molecular and cell biology, molecular genetics, imaging, and integrative physiology and pharmacology as well as ultimately clinical studies in patients. At its inception, the Center for Lung and Vascular Biology will focus on the following specific scientific aims or research objectives, although it is expected that as the Center takes shape other research focuses will emerge: To define mechanisms of lung microvascular injury, a hallmark of acute lung failure, as mediated by various cells such as polymorphonuclear leukocytes To define mechanisms which oxidants generated by vascular endothelial cells, the cells lining blood vessels, orchestrate the diseases processes of tissue injury and inflammation To define the regulation of vascular endothelial barrier function, the blood vascular barrier comprising the layer of endothelial cells, so as to understand the mechanisms by which dysregulation of barrier function leads to tissue edema and lung failure To define mechanisms by which the vascular endothelium is activated resulting in its hyperadhesivity to blood leukocytes, and to ultimately tissue injury To define mechanisms by which blood leukocytes infiltrate tissues via migration across the vessel wall under normal states as well as various diseases such as asthma and lung inflammation. To define mechanisms of how polymorphonuclear leukocytes can be activated via specific signaling pathways under normal conditions to combat infection, but also can be activated inappropriately to produce tissue injury and inflammation. The applied research focus of the Center will be in diseases of the lungs and the vasculature. The Center will provide opportunities for basic scientists and physician scientists to interact in the spirit of inquiry. The research to be carried out in the Center will have the potential to lead to improved clinical care and better prognosis of patients suffering from diseases such as acute lung injury (ALI), asthma, inflammatory diseases, pulmonary hypertension, diabetes, and acute transplant rejection. All these diseases have a significant lung and/or vascular components; e.g., the vascular complication of diabetes is the primary cause of morbidity and mortality in these patients. These diseases are often complex, involve multiple organs, and have high levels of morbidity and mortality. For some diseases (e.g., ALI or acute transplant rejection), there are no current reliable therapies and other diseases (e.g., asthma) therapies are often inadequate. Some of these diseases such as ALI have a mortality of greater 50% even in Intensive Care Units, whereas others such as asthma, pulmonary hypertension, and multiple inflammatory diseases are chronic. These diseases in toto account for tens of billions of dollars in health expenditures. Asthma is now recognized as a major developing problem in urban areas, especially among minority children. In these populations, it has been characterized as an “epidemic”. Acute transplant rejection is the primary reason for the failure of transplants, and thus the process of transplant rejection needs to be addressed systematically by harnessing the approaches and strategies of multiple disciplines so that the organs of these patients can be salvaged. The investigators in the Center will address these important diseases by providing new insights into their mechanisms so that as to better understand their pathogenesis. We believe that with this information, it will possible to design more rational and up-to-date therapeutics with the hope that this will open up new avenues for therapy. 6.2 Relationship to the University's Mission The Center’s focus on research and teaching in health and medical sciences as related to lung and vascular biology is consistent with the UIC Focus Statement (Attachment #1). The Center’s PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. goals in research and training as outlined above are in full accord with the UIC mission. To accomplish its mission, the Center will work with academic departments in the College of Medicine to appoint faculty to the Center and to recruit new outstanding faculty members. The Center will recruit faculty at the assistant professor level and will provide them the supportive and nurturing environment and start-up resources needed to develop independent, vibrant research programs. Although the primary appointments of the faculty will be in College’s academic departments, the Center will serve as their intellectual home. In addition, the Center will recruit Ph.D. and post-doctoral research trainees supported training such as NIH funded training grant entitled “Training Program in Lung Biology and Pathobiology” (Training Program Description; Attachment #2). In this context, the Center faculty will be participate in advanced research training at the bench and will also be involved in instruction of the trainees through course work. An example of the graduate level course to be directed by the Center faculty is provided in Attachment #3 (course title “PHARMACOLOGY AND VASCULAR BIOLOGY”). These aspects of the Center's mission directly parallel the institutional missions and priorities. 6.3 Specific Need and Measurable Contributions to Statewide Priorities and Needs The Center will contribute to statewide priorities as outlined in the document “CITIZEN’S AGENDA FOR ILLINOIS HIGHER EDUCATION”. Specifically, the Center will do its part helping to sustain and foster strong economic growth through the Center’s emphasis in biotechnology and drug development. The Center’s research programs have specific relevance to biotechnology and drug development. Thus, as an example the Center’s research efforts may lead to the development of specific antibodies that could be important in diagnosis or therapy. With the unraveling of the mechanisms mediating diseases processes at their molecular levels, it is likely that new patents would be filed and drug targets and/or drugs would be developed in concert with pharmaceutical and biotechnology companies. An important contribution to state priorities specifically relevant to the biotechnology industry in the State of Illinois will be through the development of molecular therapeutics targeted specifically for lung and vascular diseases. The Center will operate on the premise that these therapeutics can be most effectively developed as the direct result of an advanced understanding of the disease processes at their cellular and molecular levels; that is, on the basis of solid basic research underpinnings and interactions of multiple disciplines. Besides drug discovery, the Center’s investigators will be involved in developing novel approaches for delivery of drugs. This is particular limiting factor with many protein-based drugs today, because these proteins cannot be ingested and must be taken by direct injection into the blood or at other sites. Many protein-based drugs are being developed as the result of the genomic revolution but their clinical usefulness is hampered because they cannot be easily delivered. Even older protein drugs such as insulin need be injected. An important emphasis of the Center in this area will be to develop new approaches for the delivery of these proteins across airway lining epithelial cells following inhalation of the drug. We have an important lead on the basis of a recently issued patent (Attachment #4), but our state of knowledge is now even more sophisticated and thus other patents would be in the offing as the direct result of the work carried out in the Center. Thus, we believe that it will be possible through this inter-disciplinary and concerted research effort to develop new solutions for delivery therapeutic proteins by inhalation. But obviously much more research is PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. needed in an integrated setting such as the proposed Center, which will be an incubator for such developments. Another aspect of the Center’s contribution to statewide priorities will be in its ability to garner significant extramural research and training grant funding as well as major center and program grants. These programs will not only employ and provide opportunities for technical staff but also serve as magnets for other programs, funding, and the recruitment of outstanding faculty and trainees. Thus, a visible and successful Center based on entrepreneurial thinking is likely to serve as an “amplification system” for the development of other research activity. As an example of programmatically based funding which we wish to replicate is the currently funded Program Project grant entitled “Signaling of Endothelial Permeability and Lung Vascular Injury” (Description of this program’s synergism is provided in Attachment #5). This program is currently supported for total budget of $6,493,464, and the pending budget for the next five-year cycle is $11,229,000, almost doubling of the budget. Because of the clear focus of the Center, the leadership to be provided, and the quality of the faculty, it is reasonable to expect that there would be other significant programmatic funding in the future as the result of direct “spin-off” from the Center . Because the Center will provide opportunities for basic and physician scientists to interact, the research carried out in the Center has the potential, and indeed as its key objective, of improving clinical care and better prognosis of patients suffering from diseases such as acute lung injury (ALI), asthma, inflammatory diseases, pulmonary hypertension, diabetes, and acute transplant rejection. As the Center investigators will address these lung- and vascular-related diseases by providing novel insights into their pathogenesis, it will possible to design more rational and up-to-date therapeutics that will open up new treatments. Because these diseases represent a major drain on the economy, even small advances in decreasing morbidity and mortality are likely to have a major benefit. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. 6.4 Demand for Unit Services The Center will serve the needs of researchers across the University of Illinois at Chicago with specific interests in lung and vascular biology in both basic sciences and clinical medicine. The Center will provide opportunities for faculty investigators from multiple disciplines to interact on the basis of research interests and for training of Ph.D. and postdoctoral level research trainees. Besides the specific research interactions and training of students and post-doctoral fellows, the Center will sponsor seminars by visiting professors and senior scientists as a part of its academic programs. The Center will appoint specific existing faculty members (to be selected on the basis of research expertise, discipline relevant to lung and vascular biology, and overall excellence as scholars). The Center will also recruit new faculty by contributing salary support and start-up funds conjointly with academic departments. Besides these formal affiliations with the Center, other constituencies will also be involved with the Center. For example, pharmaceutical or biotech companies interested in the results of the research in development of novel drugs (such as directed towards chronic inflammation, transplant rejection, or asthma) and ways of efficaciously delivering these drugs will work with the Center’s staff in translating the research findings to practical results. Thus, it is expected that research ideas and products of the Center will attract the interest of businesses and industries outside the university as well as of non-governmental foundations and organizations supporting research such as the American Lung Association and American Heart Association. 7. ORGANIZATION 7.1 Proposed Unit's Organizational Structure Internal Structure of the Center The Director of the Center will be Professor Asrar Malik, a leading figure in lung and vascular biology research (curriculum vitae is Attachment #6). He has been among the top 10 funded researcher at UIC for last five years, million plus dollars annually. He has developed and has had successfully funded multi-investigator and inter-disciplinary research and training programs. He sits on many national committees such at NIH where he was a member of the Program Project Review Committee of the National Heart, Lung and Blood Institute and the Pulmonary Disease Advisory Committee. He is currently the chairman of the American Heart Association Vessel Wall Biology Study Section. Dr. Malik has been the recipient of the NIH MERIT Award from 1987-1997. He is currently the editor-in-chief of the leading lung biology journal, The American Journal of Physiology: Lung Cell and Molecular Physiology. An Associate Director will be selected to assist the Director in the management of the Center. The Center faculty will be chosen by the Standing Committee (described below) which will advise the Center Director on all appointments following recommendations made by the Center Director and department heads. The Center will appoint selectively and only specific faculty members. These individuals will be selected on the basis of the following criteria: (i) sophistication of research expertise in specific areas relevant to the Center’s thrust in lung and vascular biology, (ii) research discipline that adds to the Center’s inter-disciplinary focus, (iii) excellence in research as demonstrated by important publications in first-tier journals and extramural funding, and (iv) ability to interact and work in an inter-disciplinary setting. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. The Center Director will report to the Dean of the College of Medicine. The Center Director will be responsible for the day-to-day management, financial issues relevant to the Center, and annual progress reports. An organizational chart showing the reporting lines is indicated in Attachment #7 . External and Internal Advisory Boards The Center will have an External Advisory Committee consisting of nationally prominent individuals to be invited to review its progress. The individuals to be selected are Dr. Joe G. N. Garcia, David Marine Professor of Medicine at Johns Hopkins University School of Medicine and Director of Division of Pulmonary and Critical Care Medicine, Johns Hopkins Hospital, Dr. David Pinsky, Professor Medicine and Head of the Division of Cardiology at the University of Michigan, School of Medicine, Ann Arbor, and Dr. Iasha Sznajder, Professor of Medicine and Chief of Pulmonary Division, Northwestern School of Medicine, Chicago. The Center will also have an Internal Advisory Committee consisting of the new Chief of Pulmonary and Critical Care Medicine, Dr. John Christman and Dr. Lester Lau, Professor of Biochemistry and Molecular Genetics, University of Illinois at Chicago, College of Medicine. The External and Internal Advisory Committees will annually evaluate the Center's performance and provide input to the Center Director. The Center will have a Standing Committee of the following individuals: Dr. Richard Ye, Professor of Pharmacology; Dr. Tatyana Voyno-Yasenetskaya, Associate Professor of Pharmacology; Dr. Robert Costa, Professor of Biochemistry and Molecular Genetics; Dr. C. Tiruppathi, Associate Professor of Pharmacology, and Dr. Richard Minshall, Assistant Professor of Anesthesiology and Pharmacology. The Standing Committee will meet more regularly to advise the Center Director on appointments following the recommendations made by the Center Director. 7.2 Organization of the Center To achieve the Center’s goals and objectives (i.e., to develop a synergistic and inter-disciplinary center of excellence in the thematic area of lung and vascular biology, increase the programmatic research funding in this area, provide an intellectually-charged training environment for doctoral level students and post-doctoral fellows, and foster clinical interactions with hope of improving patient outcomes), the Center will be organized in a manner that fosters interactions and dialog, provides appropriate resources to the newly recruited faculty, supports a nurturing environments in which ideas can take wing, and encourages and rewards innovative thinking, entrepreneurship, and team approach to science and solving difficult problems. The example and leadership of the Center Director are among the factors essential for this task. Thus, Center Director working in concert with other individuals listed in the organizational chart is an absolute requirement for the Center to meets its outlined goals and objectives. The Center Director will be responsible for day-to-day management and progress reports to the Dean of the College of Medicine. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. 8. UNIT OUTCOMES 8.1 Targets for Assessment of Center's Success in Achieving Objectives Gauge of success of the Center: 1. 2. 3. 4. Level of extramural funding (chiefly from NIH). A bench-mark in this regard is the ratio of external-to-internal funding of 5:1 to 10:1 in 5 years. Thus, the Center's success will be assessed by the level of extramural funding generated. Quality tenure-track faculty appointments to the Center and the ultimate success of the faculty as defined by research publications, level of independent research funding, and research contributions to the scientific vitality of the Center. Discoveries, inventions, and patents developed in the Center. Quality and excellence of trainees recruited into the Center receiving advanced training with Center-designated investigators and their ultimate success as funded and independent scientists. 9. RESOURCES 9.1 Number of Faculty and Trainees (PhD students and Postdoctoral fellows) and Served by the Center At its maximum strength, the Center will provide partial salary support for 5-8 tenure-track faculty members with remaining amount provided by individual departments on a cost-sharing basis. An equal number of existing faculty will have an appointment in the Center without salary support at the tenured or tenure-track level. The Center will also have at any given point approximately 10 PhD students and an equal number of postdoctoral (M.D. and/or Ph.D.) level trainees. Other Constituencies Served by the Center: In terms of drug discovery and drug delivery systems, the Center will collaborate with scientists in the pharmaceutical and biotechnology industries. This will be essential for the practical applications of the technologies to be developed by the Center faculty. Total Resource Requirements: Line 1: indicates the total amount (ranging from $300,000-$400,000) needed for the recruitment and salary support of tenure-track faculty at the Assistant Professor level per year. The additional amount in Line 1 in the out years reflects the Center’s contribution to faculty salaries with addition of each new faculty member (approx $40,000). Line 2: approximate amount of ICR/year. This estimate is based on 20% recovery on a NIH with total/year direct costs of approximately $250,000 and IDC of $125,000. . Line 4: this is amount of state support committed by the Dean of COM PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Line 5: reallocations obtained by the Center Director from Department of Pharmacology and other participating departments for recruitment packages. Note: In this scheme, at the end of 5 years, if it is assumed each of the 5 new faculty generate $375,000 in DC and IDC, the total amount will be $1,875,000. The institutional investment of state dollars will be $200,000. Thus, this represents an outstanding return on the investment. Library Resources: The University Library estimates that it currently spends $50 thousand per year for resources that support work in the area of lung and vascular biology. Lung and vascular biology faculty and Library faculty find that current resources are adequate, so that no additional University Library funding will be necessary. 10. QUALITY ASSURANCE PROCESSES In terms of demonstrating ultimately the quality of the Center for Lung and Vascular Biology, there will be three evaluative quality control measures. This assessment can be made on an annual basis under the following categories: 1) evidence that the Center investigators are recipients of NIH support and support from foundations and organizations such as the American Heart Association and American Lung Association (the dollar amount); 2) demonstration of effective recruitment of outstanding junior faculty who are NIH funded or have the potential of NIH funding; 3) publications of appointees to the Center. Each of these criteria can be quantified and the results can be tabulated on an annual basis. Thus, these measures will be used to improve the Center's effectiveness in fulfilling its goals. Quality Assurance. 1. Center's support of university mission and statewide goals: The Center's mission in developing a nationally recognized and intellectually and financially profitable center of excellence is in full accord in the institutional mission in supporting research and scientific activity for the sake of knowledge as well as for the societal good. The development of the Center also serves the state mission in that the Center promises to be a driving engine for new ideas and technologies, recruitment of talented and energetic faculty and technical staff, and partnering with biotechnology companies and other businesses. To measure the quality of the "product", the Center will be reviewed on a yearly basis by advisory committees as described above. The review will address the Center's progress in fulfilling its objectives. An annual report will be generated detailing the funding of the Center's faculty, publications, and other measures of their academic productivity such as awards, patents filed and awarded, grants submitted, trainees mentored, etc. The Center will also be reviewed every eight years as part of the IBHE's review of degree programs and research/public service centers and institutes. 2. Determination of organizational effectiveness: The organizational effectiveness of the Center and its administration will also be evaluated by the aforementioned committees and report provided to the Dean of COM. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. 3. Faculty qualifications and reward structures: The qualifications of the Center faculty will be annually reviewed by the Standing Committee and the Center Director on the basis of their commitment to the Center's goals and objectives and participation in the Center's activities. Faculty will be recommended for promotion and salary increments to the respective department heads on the basis of standard academic criteria including success in extramural funding, publications in prestigious journals, and service and commitment to the Center. 4. Results from evaluation to improve the Center's effectiveness: The constructive feedback obtained from these reviews as well as the input from the Dean of COM and Center's faculty will be used to make the Center a more effective entity and to drive it forward. In this regard, the Center will strive to continually "raise the bar" and excel in its scientific endeavors, the essential elements of the Center’s success. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Table II TOTAL RESOURCE REQUIREMENTS FOR THE NEW UNIT 1 2 Total Resource Requirements Resources Available from Federal Sources 3 4 5 6 Current Budget 2nd 3rd 4th Year Year Year Year Year 365.0 405.0 445.0 485.0 525.0 25.0 (375.0) 25.0 (375.0) 25.0 (375.0) 25.0 (375.0) 25.0 (375.0) 340.0 380.0 420.0 460.0 340.0 40.0 40.0 40.0 40.0 1 2 3 4 5 ' Resources Available from Other Non-State Resources Existing State Resources Resources Available through Internal Reallocation New State Resources Required Breakdown: New State Resources Required 7 FTE Staff 5 8 Personal Services 9 Equipment and Instructional Needs 10 Library 11 Other Support Services6 1. This line reflects total funds to be provided to each new tenure-track Assistant Professor recruit from all sources (state, ICR, and cost-sharing commitments made by departments) in any given year. This total amount represents the 9 month salary component and start-up costs for the junior faculty member. 2. This amount ($25,000) is the expected ICR calculated on the basis of the Center receiving 20% of the total ICR for each faculty member. For example, if the Assistant Professor is to receive a grant of $250,000 per year (a rather typical amount for an NIH grant), the ICR would be $125,000, and the Center would receive 20% of this amount or $25,000. The amount in brackets indicates the total budget of a typical NIH grant with direct amount of $250,000/yr plus indirect cost amount of $125,000. This calculation of $25,000 is based on the assumption that each Assistant Professor recruited into the Center will be successful in generating this support amount on an annual basis. 3. The commitment of state support ($40,000) made by the Dean of COM for the recruitment of one position per year at the Assistant Professor rank for 5 years. 5. This is the amount ($300,000) to be reallocated from other sources such as departmental cost-sharing for the recruitment; i.e., one time $300,000 reallocation in each of the five years. 7. Represents the recruitment of one tenure-track Assistant Professor faculty per year over 5 years, for a cumulative total of 5 recruits; this number of recruits may increase with overall success of the Cent PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. ATTACHMENT #1 UNIVERSITY OF ILLINOIS AT CHICAGO Focus Statement Located in the nation’s third largest metropolitan area, the University of Illinois at Chicago offers instruction at the baccalaureate, master’s, first professional and doctoral levels. The University conducts research and public service in a variety of fields and ranks among the top universities nationally in attracting external support for these activities. A significant proportion of the campus’ undergraduate student body commutes, is older than traditional college age, attends part time, and has transferred from other institutions. In addition to pursuing statewide goals and priorities, the University of Illinois at Chicago: strengthens the economic and social vitality of the Chicago metropolitan area through its urban land grant mission that emphasizes business and industrial development, health care, school improvement, and enhanced opportunities for minority groups; offers instruction, research and public service in traditional fields such as engineering and the arts and sciences complemented and enhanced by a focus on health and medical sciences and services; provides off-campus programs in community college districts in the Chicago metropolitan area; and has a statewide mission to provide off-campus programs in health sciences and in selected other areas not generally available through other colleges and universities in the state. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. ATTACHMENT #2 RESEARCH TRAINING PROGRAM PLAN 1. Background A. Introduction to “Training Program in Lung Biology and Pathobiology” (T32HL07829) Our preeminent goal has been and remains as outlined in this renewal application: to provide state-of-the-art research training for predoctoral and postdoctoral trainees in areas of pulmonary biology and pathobiology. The training approach is a multidisciplinary enterprise with the training faculty having their primary appointments in six academic departments at The University of Illinois (Departments of Pharmacology, Medicine, Molecular Genetics, Biochemistry and Molecular Biology, Physiology and Biophysics, and Microbiology and Immunology) and one at Northwestern University Medical School (Department of Pharmacology and Molecular Biology). The training program is geared to provide research expertise in specific areas relevant to lung biology and pathobiology. The program goes beyond simply the reductionistic level in its approach to research training. The trainees also have opportunities to address specific research questions at the integrative and systems level as we have available in the program expertise ranging from molecular biology to the study of intact lungs. The research expertise of the faculty impacts on important questions in lung biology and pathobiology as indicated in Table 2. The training faculty (listed in Table 1) is exceptionally talented as evident by their research competence and accomplishments. Thus, the training program has fostered the development of an intellectually stimulating environment that provides the critical underpinnings for the training of individuals planning research careers. The interdisciplinary training faculty has been assembled on the basis of their research areas, productivity, competence, and general relevance to research themes in pulmonary biology and pathobiology. All training faculty members have established credentials as independent investigators. Although some members of the faculty are not strictly pulmonary researchers, their specific areas of expertise and disciplines have implications in addressing fundamental research questions in lung biology and pathophysiology of lung injury (Table 2). Therefore, these faculty members complement the pulmonary research strengths of the program and contribute to the unique multidisciplinary training environment, the hallmark of the program. Given the multi-disciplinary nature of today’s research, we believe that the environment fostered by the diverse backgrounds of our faculty provides a unique approach to training in lung research. This “cross-fertilization” of research interests and “cross-training” of fellows enhances the quality of the program and provides the trainees with the up-to-date approaches needed to address their research questions. It is important to note that the multidisciplinary training faculty, although from different academic departments, is a cohesive and experienced group of investigators who know each other well and whose research interests are relevant to the overall theme and thrust of the training program. They have been brought into the training program on the basis of their abilities to offer training in areas that are directly related to the fundamental questions and themes in lung research. B. Rationale for the Lung Research Training Program We seek continuation of support for the following reasons. First, an outstanding training faculty providing in-depth and comprehensive research training has been integrated into the overall theme of the program. Thus, the program is clearly an on-going and vital institutional entity with significant commitment as outlined in Resources Section (page 68). The training faculty members have also been thoroughly integrated into the program on the basis of their strong interests in either lung research or in areas that strongly impact on lung biology. As evident by the detailed descriptions of the research interests, the training program provides a breadth of opportunities for the PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. prospective fellows. All of the training faculty members also have a strong commitment to training predoctoral and postdoctoral fellows as evident by their individual records as preceptors (Table 7). Many of the individuals have had well over 10 years of experience as preceptors. Thus, a committed and dedicated faculty has been assembled under the aegis of the training program. Their commitment to providing training in lung research is well recognized and represents a major rationale for this program. Second, we seek continuation because the program has been a success in attracting an outstanding and highly competitive group of trainees and providing them with state-of-art training even in the short period of four years since the program’s inception. We are confident in saying that the objective of providing research training in specific areas in lung biology and pathobiology of acute lung injury and inflammation is being realized. Third, we believe it is important that the program serves an important function in providing training to predoctoral fellows in aspects of lung biology, an area in which a relatively few Ph.D.s. are trained nationally. Because of the training that they receive at the doctoral level, we believe that these individuals will bring their unique basic science perspectives to research questions that will contribute to future advancements in lung research. We also believe that individuals trained at both predoctoral and postdoctoral levels in an interdisciplinary setting will contribute in tangible ways to the future development of diagnostic tools and therapies. Their skills are highly sought in clinical and basic departments of academic medical centers as well as the burgeoning biotechnology industry where a great deal of high quality research is being carried out. Thus, the training program from these perspectives serves an important purpose and need. Finally, the program adheres to the underlying premise of providing training that will enable trainees to adapt to the multidisciplinary approach of today’s research environment as they progress in their research careers. Thus, the training program stimulates and fosters interdisciplinary thinking, a requisite for a productive career in research. The program provides research expertise in areas ranging from molecular biology to integrative physiology as they impact on lung biology and pathobiology. Although the reductionist approach is useful and valid, we as a training faculty believe it is also important for the trainees to be aware of the systems biology and to integrate approaches and methodologies from multiple disciplines and apply them to addressing important questions in lung research. The program is able to provide a multidisciplinary approach to research problems because the training faculty has been integrated into the program on the basis of the research areas that are fundamental to lung biology and pathobiology. The areas of research in which fellows can receive training include: (1) pulmonary vascular endothelial injury, (2) determinants of pulmonary endothelial barrier function and control of endothelial permeability by second messengers, (3) molecular mechanisms of endothelial-leukocyte interaction, (4) signaling of phagocytic cell activation, (5) mechanisms of activation of interferon receptors and the Jak-Stat pathway, (6) thromboxane receptor activation mechanisms, (7) integrin-regulated signaling, (8) pulmonary vascular processing of peptides via angiotensin converting enzyme and other carboxypeptidases, (9) regulation of NO production in endothelial cells, (10) seven-transmembrane receptor activation mechanisms, (11) regulation of K+ channels, (12) G-protein regulation of cytoskeleton, (13) mechanisms of endothelial cell proliferation and angiogenesis, (14) differentiation of epithelial cells, (15) caspases and regulation of apoptosis, (16) collagen production and its role in fibrosis, (17) alveolar clearance mechanisms regulated by alveolar epithelial cells, (18) pathology of pulmonary hypertension, (19) regulation of thrombin activation and inactivation, (20) molecular determinants in cell proliferation, and (21) oxidant-activated signaling in endothelial cells. As evident by the detailed description of the faculty research interests (Table 2), we can provide a wealth of opportunities for research training in basic lung biology and pathobiology of acute lung injury and inflammation. C. Relationship of Lung Research Training Program to Current Training Activities PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. This program integrates 29 investigators into the activities of the training program. To fulfill its objective of providing multidisciplinary training, the program has breached departmental barriers. We as a training faculty are committed to continuing the dialogue and cross-fertilization fostered by the training program so as to enhance the training experience of our trainees. Since the inception of the program, the multiple faculty interactions developed under the umbrella of this program have made it into an institutional effort, and have led to even greater research collaborations among the training faculty members (as described in detail in Table 6). In terms of relationship of the current training program to research activities, it is evident that all participating departments have strong faculties and training activities. Thus, this training program is embedded in a strong academic and research environment of the institution. The Department of Pharmacology at the University of Illinois has 18 faculty (10 professors, 4 associate professors, and 4 assistant professors) with 28 predoctoral fellows and 20 postdoctoral fellows. The Department of Biochemistry has 13 faculty (7 professors, 5 associate professors, and 1 assistant professor) with 24 predoctoral fellows and 21 postdoctoral fellows. The Department of Physiology and Biophysics has 22 faculty (12 professors, 8 associate professors, and 2 assistant professors) with 25 predoctoral students and 27 postdoctoral fellows. The Department of Molecular Genetics has 15 faculty (4 professors, 4 associate professors, and 3 assistant professors) with 49 predoctoral fellows and 21 postdoctoral fellows. The Department of Microbiology and Immunology has 17 faculty (7 professors, 7 associate professors, and 3 assistant professors) with 23 predoctoral fellows and 13 postdoctoral fellows. The Department of Medicine has 124 faculty (24 professors, 45 associate professors, and 55 assistant professors) and 81 postdoctoral fellows. Table 3 lists the participating departments, the number of faculty participating in this training grant, and trainees working specifically in the laboratories of the participating faculty. This list demonstrates that the training faculty members provide a fertile training environment in their laboratories that attracts a variety of trainees. Table 4 lists the current and pending training support available to the faculty in the various departments. The other institutional training programs in which some of our training faculty members participate center on the theme of signal transduction mechanisms in the cardiovascular system and the general area in cellular signaling (listed in Table 4). This program in lung biology and pathobiology constitutes the only lung research training program in the institution. 5. Program Plan A. Program Direction (a) Program Director The Program Director, Dr. Asrar B. Malik, is professor and head of the Department of Pharmacology at The University of Illinois. He will devote 15% of his time to administration of the training program and has a minimum of 50% effort directed towards his research activities. The Program Director will direct and coordinate the activities of the research training faculty and the program as a whole. Among his activities will be to organize weekly seminars and serve as the point of contact within the pulmonary research group. Other primary functions will be to facilitate faculty interactions and promote an active and continuous dialogue between trainees and faculty by holding frequent meetings and group discussions. The director is also responsible for ensuring the proper functioning of the training quality control mechanisms as outlined in a later section of the proposal. The research of the Program Director, Dr. A.B. Malik, centers on the biology of the pulmonary vascular endothelial cell, a field in which he has worked for 25 years and a research area in which he has been continuously funded by the NIH. He will continue to focus most of his effort to research- and training- related activities. In addition to administration of this training program, his previous experiences include directing a training program in lung research entitled “Mechanisms and Treatment of Pulmonary Insufficiency” initiated by him as Professor of Physiology and Cell Biology at The Albany Medical College. He served as its Program Director for 12 years (3 rd NIH grant cycle) PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. prior to his move to Chicago. Dr. Malik’s research interests cut across the area of pulmonary vascular biology from molecular aspects to analysis of the integrated control of lung fluid balance. He addresses research questions from a multidisciplinary viewpoint (the hallmark of the training program). Dr. Malik’s research focuses on three specific but related areas in pulmonary vascular biology. The first is the study of the mechanisms that regulate endothelial permeability, both the paracellular and transcellular pathways. This work involves addressing questions related to the regulation of paracellular endothelial permeability via cadherins junctions and their associated proteins, catenins, and the determinants of transcellular pathways as regulated by formation of vesicles and their vectorial transport across the endothelial barrier. Another research question being addressed relates to the mechanisms of expression of endothelial adhesion molecules, ICAM-1 and E-selectin. Studies address the intracellular signals that lead to activation of specific transcription factors mediating gene expression and regulate expression of these molecules. The third research area related to the above areas is in defining mechanisms of acute lung injury, in particular, the role of the neutrophil in the mechanism of vascular and alveolar epithelial injury. These studies address the factors and pathways that determine migration of neutrophils across the vascular barrier into the airspace and novel strategies of preventing inappropriate neutrophil adhesion and airspace migration. (b) Experience in Research Training Dr. Malik has been involved in institutional research training programs throughout his academic career. He first served as a training faculty member of the long-standing and successful General Medical Sciences training program in Shock and Trauma Research directed by Dr. Thomas M. Saba at The Albany Medical College. He subsequently conceived and directed a NHLBIsupported lung research training program entitled “Mechanisms and Treatment of Pulmonary Insufficiency” for 12 years at the same institution. The individuals trained in Dr. Malik’s laboratory in the last 10 years are listed in Table 7. Dr. Malik has trained 8 predoctoral students and 38 postdoctoral fellows. Virtually all of his trainees have remained in research-related careers in academia or the pharmaceutical industry. Some of the individuals who have trained in his laboratory include Dr. J. G. N. Garcia, Professor and Head of Pulmonary and Critical Care Division, Johns Hopkins Medical Center, Dr. Philip Barie, Professor of Surgery, Cornell Medical College, and Dr. Arnold Johnson, Research Career Investigator, Albany Veterans Administration Hospital and The Albany Medical College. Currently, there are 2 postdoctoral fellows in his laboratory. Dr. Malik also currently sponsors through the Minority Investigator Research Supplement awards program (NIH grants HL45638-10 and HL27016-19), Mr. Raudel Sandoval (a predoctoral fellow) and Dr. Theresa John (a postdoctoral fellow), respectively. This funding provides Ph.D. training and postdoctoral training to support these individuals engaged in lung research. Both of them are integral members of the training program. (c) Leadership Positions Dr. Malik has been the head of the Department of Pharmacology at The University of Illinois College of Medicine in Chicago for 4 years. During this period, he has recruited 6 tenured or tenure-track faculty members to the department. These individuals (Drs. Du, Colamonici, Ye, Tiruppathi, Kozasa, and Voyno-Yasenetskaya) have been incorporated into the training activities of the program because of their backgrounds and the outstanding research skills they bring to the training activities of the program. He serves on several key committees of the University including the University Senate and the Dean’s Executive Committee. He has been a member of several study sections including Cardiovascular Sciences, Respiratory and Applied Physiology, Lung Biology and Pathobiology, and Program Project Review Committee A. He has also served as a member of the Pulmonary Disease Advisory Committee of NHLBI. His other experience on NIH panels includes reviews of Clinical Sciences Awards, regular ad hoc membership of Surgery, Anesthesiology, and Trauma Study Section, NIH panels reviewing NHLBI awards for support of research development at minority institutions, and the Parent Committee reviewing Specialized Centers of Lung Research. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Dr. Malik has also recently taken on the editorship of American Journal of Physiology (Lung Cellular and Molecular Physiology). In addition, he serves on the editorial boards of several journals (e.g., Circulation Research). (d) Training Grant Administrative Structure The Internal Training Program Committee consists of Dr. Richard Green, Professor of Pharmacology Director of Graduate Training, Department of Pharmacology at University of Illinois, Dr. Heidi Hamm, Department of Pharmacology and Molecular Biology at Northwestern University, Dr. Lester Lau, Professor of Molecular Genetics and Director of Graduate Program in Molecular Genetics at University of Illinois, and Dr. Peter Gettins, Professor of Biochemistry and Molecular Biology and Director of Graduate Training, Department of Biochemistry and Molecular Biology, at University of Illinois. Thus, this training program interacts closely with the graduate committees of basic sciences departments involved in the program. This is of fundamental importance in the recruitment of predoctoral trainees who apply to individual departments represented in the program (as described below). The Internal Training Program Committee working with the Program Director is responsible for the final selection of the predoctoral and postdoctoral fellows admitted into the program as well as monitoring their progress in the program. As the members of this committee are also on the training faculty, they interact with the Program Director on a regular basis both at the weekly seminars as well as regularly scheduled meetings. In addition, the committee meets monthly to discuss the specific applicants who have been recommended for admission into the training program by the various Graduate Committees of the departments participating in the program. The administrative aspects of managing the program are directed by Ms. Barbara Frese, an Administrator of the Department of Pharmacology at the University of Illinois. As indicated above, The graduate students entering the training program are recommended by the Graduate Committee Directors of the departments participating in the program, three of whom, Drs. Green, Gettins, and Lau, are also members of the Internal Training Program Committee. The Graduate Committees of the participating departments to which the students apply for formal entry into the Graduate College act as the initial screening committees for all candidates. At the time of their application to the Ph.D. program, the Graduate Program Directors of each department participating in the program advise the applicant about the training program. Specific candidates who are admitted into the Ph.D. program and express interest in specifically joining the lung research training program are then recommended for admission into the training program. This recommendation is made to the Internal Training Program Committee which makes the final decision regarding admission. All prospective candidates are interviewed by several members of the training faculty as well as the Program Director prior to being admitted into the program. Thus, there is an initial review and recommendation by Departmental Graduate Committees (which approves the admission into the Ph.D. program), and this is followed by screening for admission into the training program by the Internal Training Program Committee. In contrast, the postdoctoral candidates are recruited directly into the program through contact with colleagues at other institutions and letters of interest from prospective candidates. At least three letters of reference are requested for both predoctoral and postdoctoral candidates and all final candidates are invited for an interview with members of the training program. Postdoctoral candidates are also asked to present their research findings in a seminar to which all members of the program training faculty are invited. Trainees are inducted into the program fully cognizant of their responsibilities and made aware that this is a specific and differentiated fellowship program. They are also made aware of their own responsibilities and the need for their participation in lung research seminars and visits by external consultants and professors sponsored by the training program. In addition to the above selection criteria, the training director of two other programs at the University of Illinois College of Medicine (Dr. Peter Gettins who directs the Training Program in Signal Transduction and Dr. John Solaro who directs the Training Program in Cellular Signaling in PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. the Cardiovascular System) meet frequently to discuss candidates applying to their specific programs so that the candidates can be directed to the appropriate program. Thus, there is free communication among the other training Program Directors so as to provide the applying candidates the necessary information concerning the various available training opportunities. B. Program Faculty (a) List of Program Faculty (Table 1) (i) General Faculty Attributes The training faculty consists of 26 individuals with 23 full professors and associate professors (who are all tenured) with 3 advanced level tenure-track assistant professors. There are also 3 faculty members who comprise the Resource Faculty. The faculty members have research strengths in the areas of cell and molecular biology, cell physiology, immunology, and systems physiology (their research areas are detailed in Table 2). It is evident from the faculty list that the training program is truly an interdisciplinary one. There is also significant overlap of the faculty research interests as reflected in the collaborative research carried out by the training faculty members (indicated in Table 6). Moreover, all faculty members are active participants in the training program activities such as research seminars and sharing research core facilities and major instrumentation. All of the faculty members also have ongoing research support (Table 5) and they are active in research as evident by their recent publication records (Biographical Sketches). Three junior faculty members are engaged in research relevant to lung biology, but they are as yet in the early stages of their career development and are relatively inexperienced in training predoctoral and postdoctoral fellows. These faculty members will serve as Resource Faculty for the trainees. Their research areas are detailed in Table 2a and their extramural funding is listed in Table 5a; their collaborations with other members of the training faculty are listed in Table 6. We believe that the addition of these junior faculty members to the program adds strength and vitality to the training environment. Since the last submission, junior faculty members who were originally listed as Resource Faculty have been incorporated as regular faculty upon taking on more training responsibilities and obtaining additional or independent research funding. Thus, with the development of their research programs and increased training responsibilities, members of the Resource Faculty have the possibility of joining the program as regular training faculty members. All faculty members, except one, have their primary appointments in the College of Medicine at The University of Illinois; one faculty member, Dr. Heidi Hamm, is a senior professor at Northwestern University Medical School (a 10 minute drive). Prior to this appointment, she was affiliated with the Department of Physiology and Biophysics at the University of Illinois and still maintains daily research collaborations with several members of the training faculty including the Program Director. She also has a cross-appointment at The University of Illinois. All of the research ties amongst the members of the training faculty are ongoing, strong, and in many cases interdependent. The training program has been essential in maintaining and fostering these interactions. The extent of their collaborations is highlighted below and described in detail in Table 6. From the point of view of institutional geography, the various training faculty members are close to one another (i.e., in the same buildings or in buildings connected with walkways). This helps in the frequent exchange that occurs amongst the faculty members on a daily basis. Thus, the location of their laboratories does not pose any hindrance to frequent communications and exchanges. (b) Research Opportunities Available for Trainees Table 2 details the specific research opportunities available in the laboratories of the Training Faculty; Table 2a indicates research interests of the Resource Faculty. These tables highlight the specific relevance of faculty research areas to providing research training in areas in lung biology and pathobiology. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. (c) Thematic Areas of Lung Research Training The training program can be subdivided into three areas that have been incorporated into the overall theme of the program. These areas are: (1) Vascular Injury and Lung Repair, (2) Cellular and Humoral Basis of Lung Injury, and (3) Cellular Signaling and Regulation of Lung Function. (i) Vascular Injury and Lung Repair Research training under this theme is provided in the laboratories of Drs. Malik, Du, Colamonici, Erdös, Skidgel, Tiruppathi, Lau, Ucker, Schraufnagel, Sznajder, and Varga. The underlying focus of the research in these laboratories has direct relevance to mechanisms of vascular injury and lung repair. This group of training faculty members provides training opportunities in the general area of vascular injury and lung repair from an interdisciplinary perspective. Dr. Malik investigates mechanisms of cellular interactions occurring at the level of the endothelial cell and mechanisms of leukocyte migration across the endothelial barrier. These interactions have a direct bearing on the mechanisms of vascular endothelial injury. Drs. Erdös and Skidgel investigate the role of endothelial-specific carboxypeptidases in modulating endothelial function. Their underlying premise is that these peptidases cleave arginine-containing peptides, thereby releasing arginine and providing it as a substrate for nitric oxide synthetase; thus, the induction of carboxypeptidases and their role in NO production has implications in modulating endothelial injury. Dr. Tiruppathi investigates the mechanisms of loss of endothelial barrier function by studying how thrombin increases endothelial permeability following activation of specific signaling pathways. Dr. Colamonici addresses cytokines such as inteferons implicated as key mediators of endothelial injury, and may under certain instances be involved in repair of lung tissue. Dr. Du investigates apoptosis in endothelial cells, a factor resulting in detachment of endothelial cells from the underlying matrix and denudation of vascular lining cells, and which may also be important in removal of dead endothelial cells after vascular injury. Using similar approaches, Dr. Ucker investigates role of caspases in the induction of apoptosis; his work on apoptosis has similar implications in vascular injury as Dr. Du’s studies. Dr. Sznajder investigates mechanisms of clearance of fluid from the alveolar space by addressing the function of alveolar type II epithelial cell Na+/K+ ATPases. Dr. Varga investigates the deposition of extracellular matrix proteins such as collagen in response to proinflammatory cytokines. He addresses its role in the reorganization of extracellular matrix after lung injury. Dr. Lau investigates role of matrix proteins in endothelial proliferation and induction of angiogenesis. Dr. Tyner investigates the basis of epithelial cell differentiation, which is important in understanding the process of epithelial cell proliferation after lung injury. (ii) Cellular and Humoral Basis of Lung Injury Research training under this theme is provided in the laboratories of Drs. Le Breton, Lam, Ye, Malik, Tiruppathi, Sznajder, Erdös, Skidgel, Gettins, Olson, and Lau. This group of investigators carries out research addressing the role of cellular and humoral mechanisms of lung injury. They study the specific cellular and humoral pathways believed to be critical in the mechanism of lung injury. Each faculty member is involved in the program because of the particular expertise they bring to the understanding of cellular and humoral basis of lung injury. Drs. Le Breton and Lam carry out studies in their laboratories concerned with platelet activation mechanisms; in particular, the regulation of thromboxane receptor and mechanisms and consequences of integrin signaling in platelets, respectively. Dr. Malik carries out research in his laboratory on the mechanisms of loss of endothelial barrier function. Dr. Ye studies the mechanisms of phagocytic cell activation and effects of modulating agents such as NO. Dr. Tiruppathi addresses mechanisms of endothelial cell activation, a critical cell involved in orchestrating lung’s inflammatory response. Dr. Sznajder investigates type II alveolar epithelial cell function during lung injury and the failure of Na+/K+ ATPase-regulated alveolar fluid clearance mechanisms. Dr. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Erdös and Skidgel investigate the function of carboxypeptidases found on the surface of endothelial cells and phagocytic cells in modulating in endothelial and phagocytic cell functions. Drs. Gettins and Olson carry out studies in their laboratories dealing with the mechanisms of activation and inactivation of thrombin and other serpins. These studies shed light on how thrombin function can be modified, thereby affecting how it mediates cell injury. Dr. Lau’s laboratory investigates using transgenic approaches the role of novel matrix proteins released by endothelial cells and other cell types in promoting angiogenesis. (iii) Cellular Signaling and Regulation of Lung Function Research training under this theme is provided in the laboratories of Drs. Ucker, Raychaudhuri, Hamm, Ye, Kozasa, Rasenick, Malik, Benya, Tiruppathi, Green, and Colamonici. The third area deals with signaling pathways and how they bear on the mechanism of lung injury. These investigators provide opportunities for the in-depth analysis of signal transduction pathways, involving G-proteins, second messengers, and the cytoskeleton in the regulation of function of specific lung cells, and role of dysregulation of signaling pathways in mediating cellular impairment. Drs. Du and Ucker study in their laboratories the role of pathways activated by calpain and caspases in the induction of apoptosis. In contrast Dr. Raychaudhuri investigates the signaling pathways that lead to activation of retino-blastoma (Rb) factor and induction of cellular proliferation, an important consequence of repair after lung injury. Drs. Hamm, Ye, Kozasa, and Rasenick investigate from their perspectives the coupling of receptors with heterotrimeric and monomeric Gproteins and how these interactions mediate activation of cells. This is important for understanding not only physiological response of cells, but also the basis of dysregulation of cellular function. Dr. Hamm’s laboratory also investigates interactions of receptors with specific G-proteins with the objective of selectively interfering with the receptor’s binding to particular G-protein without affecting the receptor’s interaction with other G-proteins. Dr. Malik studies in his laboratory how oxidants activate signaling pathways that lead to increased transcription and expression of proteins such as ICAM-1 in endothelial cells. Drs. Green, Colamonici, Ye, Tiruppathi, and Benya each study a specific receptor on a surface of cells (adenosine, α-inteferon, FMLP, thrombin, and GRP receptors, respectively). Their objective is to define the basis of activation of these receptors and how dysregulation of function of these receptors and the altered signals generated by these receptors can lead to impaired cell function. (d) Extent and Evidence of Faculty Collaborations and Interactions The training program provides a strong interactive environment conducive to the development of research trainees as independent and creative thinkers and investigators. Although the interests of some faculty are not primarily in lung research, their participation reflects the intellectual vitality of the program in being able to provide expertise in important research areas that impact lung biology and pathobiology. Thus, the interdisciplinary diversity of training faculty reflects a key strength of the program. The detailed interactions that exist among members of the training faculty are outlined in Table 6. The on-going interactions and collaborations of the training faculty is a distinguishing characteristic of the training environment. We believe that these interactions are a requisite for the program, and are necessary for the development of young scientists for a variety of reasons. The cohesiveness of the faculty has enabled the trainees to have available to them “on-call” research expertise that may be needed to address specific research question. Thus, it is quite common for the trainees in the program to consult informally with members of the training faculty not only to receive critical evaluation of the work, but also to seek out other experimental approaches to help them address a particular research question. Thus, the existing faculty interactions have facilitated an intensive “trainee-faculty dialogue”, the hallmark of an outstanding program. In addition, the faculty interactions and collaborations have contributed to the heralded success of the Lung Research Seminar. These seminars of the lung research group held on Friday mornings and are an anticipated part of the week’s academic calendar. They provide an exciting and formalized venue for the PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. exchange of information and presentation of data by the trainees. This opportunity is important in allowing the progress of the trainees to be evaluated by members of the training faculty, who fully participate in these seminars. Other formalized faculty interactions occur at the level of the regular meetings of Ph.D. Advisory Committees of the predoctoral fellows supported by the training program. As members of these Ph.D. Advisory Committees are also members of the training faculty, this enables members of the training faculty to interact and exchange ideas with each other and the trainees. (e) Past and Current Training Record of Faculty (detailed in Table 7) All of the regular faculty members have served as preceptors, and thus are experienced at taking on this responsibility. Even though Table 7 lists the training record for the past 10 years, it is apparent that most former trainees are occupied in productive research careers. Table 7a lists the honors and awards received by many of the recent trainees working in the laboratories of the training faculty members. It is evident that the recent and current trainees working under the various members of the training faculty have been successful during their research training phase. This portends well for their future careers. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): C. Malik, Asrar B. Proposed Training (a) Overall Aspects of the Program We are seeking continuation of this program that trains highly qualified predoctoral and postdoctoral fellows in specific research areas of pulmonary biology and pathobiology as related to acute lung injury and inflammation. The training program emphasizes an in-depth and intensive research experience at the multidisciplinary level. The training faculty members have been integrated into the training program on the basis of the underlying philosophy of providing multidisciplinary training. The training encompasses all aspects of the research enterprise from formulation of the hypothesis, obtaining preliminary data in support of the hypothesis, the design and conduct of further experiments, and ultimately to submission of the research manuscript and its publications. Advanced level graduate courses in areas relevant to lung biology such as in receptors and signaling and lung and vascular biology are provided by the participating basic science departments, which include the Departments of Physiology and Biophysics, Biochemistry and Molecular Biology, Molecular Genetics, Pharmacology, and Microbiology and Immunology. The Ph.D. degree requirements for the trainees in the program are listed in Table 8. The advanced level required courses and those courses relevant to research being carried out by trainees supported by this program are described in Table 8a. The specific course requirements for the trainees in the program are also described below. Postdoctoral fellows also have the opportunity to take these courses, but only on an audit basis. All trainees also participate in three weekly scheduled seminars (two scheduled at noon on Wednesdays and Fridays and one (Lung Research Seminar) scheduled at 8:30 A.M. on Friday to minimize interference with their research schedules). These are (i) Lung Research Seminar on Friday at 8:30 A.M., attended by lung research trainees and the training faculty; (ii) Graduate Student Seminar (Wednesdays at noon), which are formal seminars presented by all graduate students; and (iii) Visiting Professor Seminar given by distinguished experts are held at noon on Fridays (listed in Table 8c). These three weekly sessions are an important component of the training program and attendance is a requirement for all trainees. (i) Differentiation of Trainees in the Program It is important to note that the cohort of predoctoral and postdoctoral trainees are treated as a distinct group. The first distinction is that they share common experiences in terms of seminars, presentations, and meetings with visiting scientist organized and supported by the program. Second, the trainees share common resources such as the Cell Culture Core and the Imaging Core (described in the Resources and Environment Section on pages 68-70). In addition, the trainees supported by the program are differentiated by the fact that they are addressing research questions in areas with specific relevance to lung biology and pathobiology. The trainees also have available to them a lounge with study carrels and computers. To enhance program cohesiveness, in the last 2 years, we have had a one and half day retreat for the trainees and faculty members (at Lake Geneva, Wisconsin) where posters are presented and talks are given by both trainees and faculty. Finally, all faculty and trainees are connected by an e-mail server list which provides direct linkage to all participants in the program. The specific course requirements for the trainees in the program are described below, which is a key element of differentiating the program. Finally, the trainees are distinct from other trainees who are not a part of the program because the intent is to provide a true sense of fellowship amongst the trainees and faculty. (ii) Number of Trainees In the last cycle, we were approved for 4 predoctoral and 4 postdoctoral fellows per year since this was a number that could be accommodated by the faculty; however, due to NIH budget constraints, the number of positions was reduced to 3 predoctoral and 3 postdoctoral fellows. Although the reduction has not affected the quality of the program, it has prevented us from having an institutionally broad-based program as we initially envisioned. Nevertheless, the program has thrived and the quality and size of the faculty have grown. Thus, we believe that we can easily accommodate 5 predoctoral and 5 postdoctoral fellows per year on a basis of the 26 training faculty members and 3 resource faculty members. Moreover, we have more than enough highly qualified PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. predoctoral and postdoctoral fellowship candidates to fill 5 predoctoral and 5 postdoctoral positions. The number of applications made to participating units of the training program are listed in Table 9. Tables 9b and 9c lists the number of candidates expressing interest in admission into the training program since the beginning of the program. In 1998-1999, we had 29 Ph.D. predoctoral and 65 postdoctoral applicants with superb credentials. The proposed size of the faculty matches well the number of outstanding candidates applying to the program as well as the size of the faculty. The ratio of training faculty-to-predoctoral fellows and-postdoctoral fellows is 5 in each case. It is clear that the trainees will have enough flexibility in choosing preceptors and their specific research projects. Thus, we are requesting an increase in the number of predoctoral and postdoctoral trainees by 1 each over the previously recommended number of 4 in each category because of not only the training faculty size and strength but also the cadre of strong applicants to the program. (iii) Duration of Research Training The duration of training will depend on factors such as the trainee’s career goal and unquantifiable issues such as the difficulty of the research questions under investigation. Predoctoral fellows will be supported by the training program for 3 years. Beyond the 3 years, it is expected that the support be derived from funds of the preceptor. Postdoctoral trainees will be supported for 2 years. Our general experience has been that this represents an optimal period for support of postdoctoral trainees in the program. In the event that the training period needs to be extended to the third year because of a specific research area, there will be a contingency for this. Each case will be evaluated by the Internal Training Program Committee. The postdoctoral trainees will be encouraged in specific cases to apply for outside support such as Parker B. Francis Foundation Fellowship. One of the 6 postdoctoral trainees recruited into the program has received a fellowship by this mechanism. However, in most instances we have felt that it is necessary to have a continuity of fellowship support by the training program mechanism for at least 2 years so that the trainees are committed to the program and its approach, and are able to receive training under the aegis of the program. (iv) Trainee Participation in Research The intent of the program is to provide “hands-on” intensive research training; thus, the research training component is the quintessential element of the program. Courses (listed in Table 8a) are available for postdoctoral fellows on an audit basis to remedy weaknesses in specific areas as may be identified by the trainee or Internal Training Program Committee. Although research is the key element of Ph.D. training, the doctoral students have to meet the set Graduate College requirements (Table 8). The first year the Ph.D. trainee has a number of courses, but this is also the beginning of the research phase of training. The second and third years have fewer course requirements for trainees and a significantly greater amount of research. Predoctoral fellows, thereafter, engage in full-time research. The usual experience has been that in the first year 50% of the time is devoted to research training which increases to 75% in year 02, 90% in year 03, and thereafter 100%. Postdoctoral trainees are involved in full-time research from the outset. (v) Availability of Graduate Courses and Course Requirements Graduate level courses are available for the predoctoral fellows so that they can meet the Ph.D. degree requirements. The predoctoral fellows are required to take Core courses which include physiology and biophysics, biochemistry, and a course in pharmacology for pharmacology graduate students or a course in immunology for immunology and microbiology graduate students. The specific Ph.D. degree requirements are listed in Table 8. The specific course requirements for Ph.D. trainees in this program are the 500 level courses in Molecular Biology offered by the Department of Molecular Genetics (BIOS 524) and the Lung and PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Vascular Biology (PCOL 530) offered by the Department of Pharmacology. In addition, the students are required to take 3 other 500 level courses listed in Table 8a (i.e., courses that would be most pertinent to their research area). This is to be done in consultation with their advisor and approval of the Internal Training Program Committee. Finally, all trainees (predoctoral and postdoctoral) are required to take the course in the responsible conduct of research (Table 8b). We feel that these courses for Ph.D. students are needed to build the basic foundations of a research career. In contrast to the predoctoral trainees, the laboratory phase for the postdoctoral fellows is upon entry into the program. The postdoctoral trainee may have the option of auditing advanced level courses in areas relevant to the research project of the trainee (the relevant courses are listed in Table 8). This will be decided in consultation with the advisor, Program Director, and Internal Training Program Committee. A course can only be audited if it does not interfere with laboratory research of the postdoctoral trainee. We generally will not encourage course work after the first year since postdoctoral fellows are expected to concentrate full-time on the research projects during this period. (vi) Field in Which Trainees Qualify Upon Completion of Training A common career path for the Ph.D. postdoctoral trainee is an academic position in a basic science or clinical department, a position in the biotechnology industry, or a government research laboratory such as NIH. Our recent experience (albeit of only 4 years) has been that the biotechnology industry offers very competitive and intellectually stimulating research positions with outstanding starting packages and with opportunities for independent research; thus, these have become highly desirable for some recent trainees. The general experience of the former trainees employed in biotechnology firms is that they provide a challenging research environment and a considerable degree of independence along the lines of company’s research focus. Thus, in the rapidly changing market for postdoctoral trainees, it is quite apparent that research positions in private industry have become a desirable career objective. Other individuals, however, gravitate towards academia with positions in either basic science or clinical departments. Positions in clinical departments have become particularly attractive for postdoctoral trainees because they present opportunities for interactions with physician-scientists; moreover, for the qualified individuals, these are independent tenure-track positions. This program because of its multidisciplinary and integrated approach to training benefits those individuals planning independent research careers in academic departments or government and research institute laboratories, as well as those entrepreneurial individuals choosing the biotechnology industry. For the doctoral candidate completing the Ph.D. degree, the primary option is postdoctoral training in a recognized laboratory in either an academic institution, NIH, or a research institute. Although this program is relatively new, the postdoctoral trainees have all found challenging positions in academia (both basic and clinical departments) and in pharmaceutic/biotechnology industry. The predoctoral trainees have also found outstanding postdoctoral positions. This information is provided in Table 13 and discussed in the Progress Report on page 93. The Publication records and the various achievements of former trainees in the program are provided in Tables 14 and 14a, respectively. (b) Program Integration and Coordination (i) Program Director’s Role The major responsibilities of the Program Director are in guiding the program and providing the overall integration to the training activities of the program. The integration and coordination require regular and frequent meetings with the trainees, training faculty, and the Advisory Committees. The Program Director chairs the Friday morning Lung Research Seminar and is responsible (in consultation with the training faculty) for organizing visits of professors and consultants for the noon seminars. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. A key mechanism by which the Program Director integrates the training program activities is by bringing together the faculty at seminars and other regularly scheduled events. These group meetings are a vital element of the training process since they provide opportunities for the faculty to gauge trainees’ progress in research and they help to build an esprit de corps amongst both trainees and faculty members. Feedback and evaluations are provided by e-mailing an evaluation form to the faculty for their comments directed to the trainees. In addition, informal feedback is provided after the session by the Program Director as well as the advisor, and, often, by individual faculty members. The Program Director also deals with training-related issues in consultation with the Internal Training Program Committee. A part-time administrative secretary facilitates all of the coordination of the program by scheduling visiting professors/consultants, informal research meetings among members of training faculty, filling out NIH and institutional appointment forms, dealing with administrative matters relating to trainees (e.g. health insurance), assisting in organization of scheduled weekly research meetings, and typing of progress reports. Another critical aspect of the Program Director’s role in coordination of the program is his active and direct participation in the recruitment of trainees (described below). This involves working with the training faculty to establish outreach programs to various regional undergraduate institutions (e.g., Knox College, Oberlin, etc) as well as minority institutions in order to attract trainees into the program. (ii) Role of Training Faculty The intellectual vitality of the training program, and its ultimate success, rest in large measure on the quality and dedication of the faculty. We feel the program is well balanced in this regard because a talented and committed training faculty has been assembled under this umbrella of this program. The faculty has been selected on the basis of several quantifiable criteria: (i) experience as mentors (as outlined in Table 7), (ii) areas of research and disciplines with relevance to pulmonary biology and pathobiology (as outlined in Table 2), (iii) commitment to work with one another (as outlined in Table 6), (iv) a resolute commitment to provide the multidisciplinary underpinnings to the research training program, and (v) independent research support (as outlined in Table 5). For the purposes of coordination and integration of the program, the faculty meets weekly at research seminars organized by the training program: the Lung Research Seminar on Friday mornings and the Visiting Professor Seminar at noon. In addition, the faculty meets in small group sessions when research findings of fellows are discussed and critique is provided (such as the frequent meetings of the Thesis Advisory Committee, for the predoctoral fellows supported by the training program). All faculty members are active participants in these weekly seminars and at the various research sessions such as Ph.D. Student Advisory Committees. These meetings are essential in providing input concerning each trainee’s research and assessing their general progress in the development as an investigator. The faculty also has the opportunity of influencing the program through the Internal Training Advisory Committee as described below. Finally, the faculty members also meet once a year with the trainees at the retreat to discuss research and to coordinate the various training issues. (iii) Roles of Advisory Committees (I) Internal Training Program Committee The Internal Training Program Committee functions to (1) screen finalist Ph.D. and postdoctoral trainees for admission into program (2) evaluate progress of fellows, (3) discuss any changes in direction of program, and (4) discuss issues relating to organization and management of training program. The members of this committee are Drs. Richard Green, Heidi Hamm, Lester Lau, Peter Gettins, and Asrar Malik (II) External Advisory Committee PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. The External Advisory Committee will consist of Dr. Michael Shasby, Professor of Medicine, University of Iowa, Dr. Michael Matthay, Professor Medicine, University of California at San Francisco, and Dr. Joe (Skip) Garcia, Professor of Medicine, and Head Pulmonary and Critical Care Division, Johns Hopkins University. This committee will provide a regular review of activities of the training program, deal with concerns of the training faculty, and help to identify potential trainees. They will also provide a measure of the trainees in this program relative to the research trainees at their home institutions. Other issues to be dealt with by this committee in conjunction with Program Director include trainee performance as carried out by annual evaluation of the progress of trainees in the program. Each of these individuals has visited the training program and consulted with the Program Director in the previous cycle. (iv) Basic Science and Clinical Integrations An important strength of the program is the strong linkage between the clinical and basic science training faculty members. These basic science and clinical interactions are an integral component of the training program. They are facilitated by having as members of the training faculty, individuals whose primary appointments are in clinical departments: Drs. Dean Schraufnagel, Richard Benya, Donovan Yeates, Jacob Sznajder, and John Varga. Moreover, both Dr. Benya and Dr. Sznajder have cross-appointments in the Department of Pharmacology. In addition, Dr. Benya directs the Confocal Core facility at the Veterans Administration Hospital available to training program fellows. There are also several members in the basic science faculty with either M.D./Ph.D. or M.D. degrees: Drs. Oscar Colamonici, Ervin Erdös, Xiaoping Du, Tatyana VoynoYasenetskaya, and Shigehiro Nakajima. Thus, there are ample opportunities for basic scienceclinical integration through the daily interactions of physician-scientists and basic science training faculty members. These individuals not only serve as role models, but also provide a clinical prospective to the basic science trainees. As the trainees are exposed to training faculty members with an integrated perspective of their research areas, this further points to the training approach as being truly multidisciplinary. We believe that these clinical interactions are of fundamental benefit to the predoctoral and postdoctoral trainees. For example, trainees may not easily recognize the relevance of a particular research question; however, because they are exposed to issues first-hand through their contacts and discussions with the physician-scientist members of the training faculty, the trainees are able to integrate their bench research observations to the physiological and clinical relevance of their research question. This continuous dialogue has been an integral aspect of the training process. Although the research questions of the trainees are focused and targeted, these interactions are essential in providing the trainees with a broader and well-rounded perspective of the problem; thus they go beyond viewing the question only at the reductionist level. (v) Coordination in Selection of Research Projects (I) For Postdoctoral Fellows Postdoctoral fellows inducted into the program apply to a particular individual in the training program, or are attracted to the program itself, and thus they have preconceived notions of the specific research area they intend to pursue. However, if the selection of the research advisor has not been made during the first two months in the program, a committee consisting of the Program Director and Internal Training Program Committee assists in this process. The intent is to match optimally the research training experience desired by the fellow to the research interests of the faculty. Also during the first two months, all postdoctoral trainees are required to present their proposed research program under headings of specific aims, background, rationale, and methods of their proposed research. They are guided in this exercise by their selected advisor and other training program faculty convened on the basis of the closeness of their research areas to the research interests PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. of the trainee. This allows for a more focused definition of the hypothesis and experimental design. In addition, we ask all our incoming postdoctoral trainees, within a 2 to 3 month period of having selected an advisor, to present at the Lung Research Seminar the ideas that will form the basis of their work and preliminary supporting data. The intent of this exercise is to outline the hypothesis and present preliminary data in support of the hypothesis. Our experience indicates that this period of “acclimatization” assists the trainees in developing a more focused and directed approach to their future studies. During this initial period, the fellows are advised about the planned experimental approaches and methodologies available to them within the program as well as the necessary equipment and other resources needed to conduct their studies. (II) For Predoctoral Fellows After their selection into the training program, the Ph.D. students meet with the Internal Training Program Committee to discuss research areas and interests. The committee advises them about the particular training faculty members with matching interests. The predoctoral students then rotate through the laboratories (usually 4-5 laboratories) of these training faculty for 6 months after admission into the program. They make their choice of an advisor at the end of this period on the basis of research interests and the particular interactions that they have had during the laboratory rotation period. The selection of the research project and preceptor is made with the approval of the Internal Training Program Committee. Following this selection period, the Thesis Advisory Committee members are chosen by the Ph.D. student in consultation with the Ph.D. advisor. The Ph.D. Advisory Committee then meets at intervals of 2-3 months during the entire training period of the Ph.D. student. A year to 18 months prior to the anticipated graduation date, the Ph.D. student is required to submit the Preliminary Ph.D. Thesis which outlines the hypothesis, presents the detailed supporting data, and outlines the series of experiments to be carried out for completion of the thesis, and subsequently for the defense of the thesis in an in viva examination. (vi) Coordination in Selection of Preceptors Most prospective postdoctoral trainees entering the program are aware of the research areas that they wish to pursue, and thus have already directed their attention to their primary advisor. In those instances where a postdoctoral trainee has not made a choice, a period of laboratory rotations (usually to several laboratories) is allowed to obtain a better sense of the available training opportunities. Usually, 2 months are allowed for rotation; thereafter, it is expected that the advisor be identified. In some instances, the postdoctoral trainee has the option of selecting more than one preceptor. This has been a valuable modus operandi in this program because it allows more than one way of viewing a particular research problem and provides opportunities for the trainees to address research questions with wider array of experimental strategies and methodologies than would be otherwise possible. This flexibility enhances the quality of the program because it enables the fellows to cross disciplines and to receive cross-training on the basis of research questions being addressed rather than there being departmental or laboratory barriers to training. This goal of interdisciplinary research training is realized within this program because of the many close collaborations amongst the training faculty members and the cooperative attitudes fostered within the program. The selection of the preceptor for the Ph.D. student varies from that of the postdoctoral trainee. The Ph.D. students have a distinct and well-defined 6-month period of laboratory rotations after which they are required to select their primary research advisor. The Internal Training Program Committee along with the Program Director approves the advisor and the laboratory as the primary site of Ph.D. training. The Ph.D. student also has the opportunity to interact with other members of the training faculty through the Ph.D. Advisory Committee; within 6 months of selecting a primary advisor, the Ph.D. student selects the Ph.D. Advisory Committee which incorporates members of the training faculty into the overall training structure of the Ph.D. student. Members of the Ph.D. Advisory Committee of the student (who are also members of the training faculty) have a critical role PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. in advising the Ph.D. student along with the primary advisor during the student’s entire training period. Individuals comprising the Ph.D. Advisory Committee are selected on the basis of their research interests, which enables them to participate effectively in the research training of the Ph.D. student. (vii) Research Performance and Evaluation: Quality Control Measures (I) Research Presentations at Weekly Meetings The Lung Research Seminar on Fridays at 8:30 A.M. in which trainees present their findings and which are interspersed with seminars given by training faculty and visiting professors provide an important opportunity to evaluate trainee progress. A trainee is afforded typically opportunities for three seminars during the academic year; thus, this enables an ongoing and continuous review of the research progress being made by the trainee. In addition to these research-in-progress seminars, there are the formal noon seminars in which leaders in the field are invited to the institution (Table 8c list the individuals who have participated as visiting professors and consultants). (II) External Consultants/Visiting Professors The training program organizes a series of Visiting Professorships and Consultant sessions during the academic year (Table 8c). These individuals are invited to review the research and serve in an advisory capacity to the Program Director and program. The consultants’ visits are usually for one and a half days during which the fellows present their work often on a one-to-one basis. Sufficient time is allocated for the fellows’ presentations and for feedback and critique. Important benefits accrue to both trainees and we believe to the training faculty from these visits. The consultants/ visiting professors are important in enhancing the training process as they critically and objectively review the research of the trainees and provide insightful feedback from an objective perspective. Their evaluations are also relayed to the Program Director who then shares them with trainees and the Internal Training Program Committee. (III) Presentation of Other Weekly Seminars In addition to the weekly Lung Research Seminar and the regularly scheduled visits by external consultants/visiting professors, there are also weekly Trainee Research Colloquia held in the basic science departments participating in the program. Ph.D. students and post-doctoral fellows present their research at these meetings. These are more generally attended, and thus provide a broader exposure of the trainees’ research findings. Although these seminars are more structured than Lung Research Seminar, they serve as important means for monitoring progress of the trainees in the program. (IV) Presentations at National Meetings and Preparation of Manuscripts An important goal of the training program is to guide trainees in presenting their research findings at national meetings (e.g., Experimental Biology Meetings, American Thoracic Society Meetings, or Gordon Conference, etc.). This involves members of the training faculty providing critiques of oral presentations and poster presentations for content and style (e.g., quality of graphics). This is done at the Friday morning Lung Research Seminar one to two weeks before the national meeting. Although the primary responsibility for publication and critiquing lies with the preceptors, other members of the training faculty, with particular interests in the research project also participate in the process. The various faculty members are also often asked to review manuscripts by trainees. It is our experience that these critiques invariably lead to improvements in the trainees’ communication and writing skills. (V) Presentations at Annual Retreat All trainees are also asked to present their research at the annual retreat held at Lake Geneva, Wisconsin in mid-September, near the beginning of the academic year. This provides an PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. opportunity for the trainees to be evaluated and also for the trainees to learn about the research activities of the faculty. (VI) Role of Advisory Committees The Internal Training Program Committee is significantly involved in monitoring trainee performance during the various presentations given by the trainees at the research seminars described above. In addition, the committee is kept apprised of the trainee’s progress by regular contacts with the trainee and by the frequent meetings organized by the Program Director. The basic question addressed by the Internal Training Program Committee with respect to trainee evaluation is whether the fellows are achieving their goals under the guidance of their advisors. Feedback by this committee is provided to the Program Director during the meetings held with the Internal Training Program Committee. Any decision to terminate a fellow is made by the Internal Training Program Committee and Program Director. Specific and persistent concerns will result in such an issue being discussed and a letter being written by the Program Director to the concerned individual. Although this policy is in effect, there have been no such issues raised about any of our trainees. (VII) Role of Program Director The Program Director has a critical role in evaluating the research performance of trainees during the multiple opportunities available to him. These include the Friday morning Lung Research Seminar and the graduate student colloquia, held on Wednesdays at noon, as well as evaluations by external consultants/visiting professors. The Program Director also directly consults with the preceptors concerning developments being made by the trainees in the program. The Program Director provides the feedback whenever appropriate and deemed necessary. The close working relationships between members of the training faculty and Program Director are key to the director playing an essential role in evaluation of the trainees’ progress. D. Trainee Candidates (a) Overall Qualifications of Prospective Trainees It is the policy of the program to recruit those candidates with high academic performance and significant potential for a research career. The predoctoral trainees are required to have undergraduate degrees in biology, chemistry and biophysics, molecular biology, or related disciplines. All postdoctoral candidates are required to present a seminar of their previous research work (this does not apply to the M.D. candidates without prior research experience). Academic grades from graduate school and medical school are requested from all candidates. The prospective Ph.D. trainees are required to submit scores from their college and the Graduate Record Examination (GRE). All predoctoral and postdoctoral candidates are asked to submit letters of reference or provide a list of references. (b) Specific Criteria and Procedures for Selection of Trainees The training positions are advertised in widely distributed scientific journals. Postdoctoral candidates are also identified at annual meetings of scientific societies such as Experimental Biology and American Society of Cell Biology. Postdoctoral candidates are also considered on the basis of recommendations from colleagues at other institutions. Predoctoral candidates apply to The University of Illinois and to the basic departments participating in the training program. They are informed about the program, if they are not already aware of it. They are recommended for admission by the Graduate Committee of the participating departments on the basis of the criteria established by the departments. The names of those candidates expressing an interest in the program are then forwarded to the Internal Training Program Committee of the program, which has 3 Graduate Program Directors (Drs. Lau, Gettins, and Green) as well as Drs. Hamm and Malik. This committee then does the final screening in admitting the Ph.D. candidate into this program. The PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. decision to admit is based on the candidates research interests and aptitude, scholarly activity, recommendations, and interview with members of the training faculty. Table 9 lists the predoctoral trainee recruitment data of the basic science departments participating in the training program. As is evident from this list, all departments connected with the program have a large applicant pool, and only a small fraction of the outstanding applicants are considered for admission into the department Ph.D. programs, and after further screening the number entering the Ph.D. programs is yet smaller. Thus, the Ph.D. programs of all departments involved with the training program are highly selective. Table 9a provides further details about the applicants who were eligible for the program. These individuals received their undergraduate education from a spectrum of institutions reflecting the national visibility of the predoctoral training programs of the University of Illinois College of Medicine. The criteria for admission into the program are described below. They are based not only on grades and GRE scores but also on personal interviews, letters of recommendation, previous research experience, future goals, and aptitude for research. We have been successful in recruiting a highly qualified group of candidates into the training program without regard to race, color, creed, or sex. Our experience to date is that we have a substantially larger pool of both qualified predoctoral and postdoctoral candidates (Table 9b and 9c) than the available positions. Tables 9b and 9c list the pre-doctoral and post-doctoral candidates expressing interest in the lung research training program. Regrettably, many of the interested and potentially acceptable outstanding candidates cannot be accepted. In 1998-1999, there were 29 finalist predoctoral Ph.D. trainee candidates; that is, those individuals with expressed interest in lung research training who were recommended by the Departmental Graduate Committees for possible admission into the training program (Table 9b). In 1998-1999, there were 65 postdoctoral candidates (Table 9c) for the available positions in the training program. The Internal Training Program Committee further narrowed down the list of postdoctoral candidates to the 16 individuals listed in Table 9d. Prior to inviting predoctoral or postdoctoral candidates for interview, members of the Internal Training Program Committee as well as the Program Director screen all applicants and select those to be invited. All travel and accommodation expenses for the short-listed candidates are covered. The selection criteria are: (1) strong academic background reflected in grades and previous research experience, if the candidate has a Ph.D. or M.D. degree; (2) strong motivation for and commitment to a research career; (3) strong references from individuals knowledgeable about the candidate (e.g., departmental chairperson, previous mentor, and other faculty members from the candidate’s institution); and (4) future goals and commitment to devote full-time effort to research training in this program. If any of the prospective trainees have had previous research experience, they are asked to present their research findings at a seminar. The interviews are scheduled so that the candidates have an opportunity to meet many members of the training faculty, establish a sense of our expectations, and for the faculty to evaluate the candidates at first-hand prior to admission into the program. (c) Sources of Availability of Trainees The training faculty as a group has a wide network of colleagues, an essential component of a successful recruitment process. The training program also publicizes itself by advertisements in scientific journals as well as through placement services of scientific organizations such as Experimental Biology and American Society of Cell Biology. Postdoctoral trainees are often attracted to the program because of the research being carried by a faculty member, the quality and reputation of the training faculty members as a whole, and the growing visibility of the training program itself. The Ph.D. students are attracted to the program because of the training faculty and the visibility of the graduate programs of the University of Illinois academic departments represented in the training program. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. In the coming year, we will further address this issue by establishing outreach programs to various outstanding undergraduate institutions in the Great Lakes area and the upper Mid-west. The Program Director and members of the training faculty will make presentations in Departments of Biology of these institutions with hope of further increasing our applicant pool, and attracting some of these students into the program. 3. Recruitment of Under-Represented Minorities A. Goals and Programs The training program remains actively committed to providing opportunities for training of candidates of under-represented minorities. We actively participate in programs designed by The University of Illinois Graduate College to attract undergraduate minority students to graduate programs. Members of the Graduate College and the Office of Vice Chancellor for Research have established direct contacts with a number of minority institutions. These include Xavier University, Morgan State University, Jackson State University, and Prairie View University all of which have excellent academic programs. In addition, senior members of the faculty at The University of Illinois College of Medicine such as Dr. Richard Davidson, Professor and Head of Molecular Genetics, has visited Howard University, Morgan State University, and Xavier University to establish good working relationships that we believe will be important in recruiting their best students. A summer internship program has also been established to provide research opportunities for undergraduate students from Howard University and Morgan State University. This ten-week summer program has allowed 14 students to work in various laboratories at The University of Illinois College of Medicine. The Committee on Institutional Cooperation (CIC), the academic consortium of the Big Ten Universities and The University of Chicago, has designed a Summer Research Opportunity Program (SROP). The goal of SROP is to introduce talented minority sophomores and juniors, early in their undergraduate education, to research and rewards of graduate study. Working with faculty members, some of whom also are on the training faculty, we hope to attract minority trainees on this basis. The goal of this project is to identify potential graduate school applicants within the consortium and share their names with member institutions, and ultimately influence their eventual graduate and academic career choices. Another program involves students from community colleges. The Graduate College of the University of Illinois has received funding from the U.S. Department of Education through a grant application to the Minority Participation in Graduate Education Programs to provide research experience for talented students from community colleges. These students are selected to participate in an 8-week program under the supervision of University of Illinois faculty members the summer prior to transferring from their associate degree program at the community college to the baccalaureate program at The University of Illinois. The intent of this program is to enable some of the top students to apply eventually to graduate programs leading to the doctorate degree. The institution also participates in an outreach program to bring minority high school students into the laboratory with the hope that they become interested in a research career following their graduation. An example of such a program for high school students is that from the Illinois Mathematics and Science Academy (IMSA), a public residential high school for talented science and mathematics students. Students from institutions such as IMSA and others in the area have demonstrated high academic abilities and potential. Students under this mentorship program participate in research during the summer months with investigators in the training program. These students are assigned mentors during the summer and they participate in seminars and research discussions of the lung biology training program. Although no grade is assigned, students receive an appropriate note in their transcripts indicating their participation in this research program. Many of these students have returned to their mentor’s laboratory in successive summers prior to enrolling in an undergraduate degree-granting institution. We hope in the future to be able recruit back some of these outstanding students into the training programs under the auspices of this training grant. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. In addition to the strategies indicated above, in the future, the program intends to play a more active role in advertising at specific minority undergraduate institutions (as described below under the heading “Direct Involvement of Program Director in Minority Recruitment”). We will also continue to advertise this program on the GRE Minority Placement Service, Minority Access to Research Careers training programs, and Deans of Honors Programs in the National Collegiate Council. We have been successful in recruiting two minority trainees in lung research through contacts with colleagues at other institutions and within the institution. Two trainees, Dr. Theresa John and Mr. Raudel Sandoval, are receiving training in lung research as other the other trainees in the in the program. Because of the cutbacks in the original recommended budget of the program from 4 postdoctoral fellows and 4 predoctoral trainees to 3 in each category, Dr. John and Mr. Sandoval are being supported by supplements to ongoing NIH grants in lung research (these trainees are described below.) B. Fellowship Opportunities Supported by The University of Illinois The Graduate College of The University of Illinois is committed to increasing the racial diversity of the graduate student population. We are well aware of the dramatic decrease in the number of African-American and Hispanic graduate science students (greater than 20% drop between 1996 and 1997 according to a report released by the American Association for Advancement of Science, “Losing Ground: Science and Engineering Graduate Education of Black and Hispanic Americans”, AAAS publications, Washington D.C.). The University of Illinois by its University Fellowship Stipend program provides stipends as well as waives tuition for many eligible underrepresented minority students entering the Ph.D. program. C. Retention of Minority Trainees It is the intent of the training program, and indeed that of the institution, to improve the retention of minority students. The Graduate College along with relevant academic departments regularly monitors the academic progress of all students. The minority students experiencing academic difficulty are invited to meet the Graduate College staff to review and assess their progress, and subsequent referrals are made to appropriate support services. Continuation of fellowship awards is contingent upon the fellow’s academic progress towards the completion of the degree. The Graduate College regularly verifies the satisfactory academic progress of externally supported fellows and formulates reports to the appropriate funding agencies. These reviews are held in concert with the student’s academic unit. A minority graduate student organization at The University of Illinois, Helping Other People Excel (HOPE), also provides academic and non-academic support for minority graduate students. HOPE focuses on the promotion of intellectual growth and fellowship among students, faculty, and university administrators. To this end, HOPE sponsors regular events, such as orientation and brown bag lunches where speakers discuss topics important to professional and academic development, and social events are held for potential minority graduate students. In addition, the Urban Health Program at the University of Illinois at Chicago was established to increase the number of minorities in health professions. Although a main goal of this program is recruitment, the program also emphasizes retention, financial aid assistance, academic and personal counseling, and early outreach. The program functions in seven different colleges of the University, including the College of Medicine. D. Direct Involvement of Program Director in Minority Recruitment The Program Director will be directly involved in minority student recruitment. He will organize meetings with (i) minority students majoring in biology, chemistry, and physics in the Colleges of Liberal Arts and Sciences at both at the Chicago and Urbana campuses, (ii) minority students enrolled in medicine at the Chicago campus (approximately 15% of our medical school class PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. in the first year enrolled under the auspices of the Urban Health Program are minority students), and (iii) minority students in biomedical engineering programs at both the Chicago and Urbana campuses. Any student expressing an interest in the program with be invited for meetings and interviews with members of the training faculty as well as trainees in the program. The Program Director will also seek out and visit undergraduate advisors and students at the traditionally African-American institutions of higher learning (such as the ones mentioned above) as well as institutions with large Hispanic undergraduate populations. It is our hope both of the above strategies to be spear-headed by the Program Director as well as the other aforementioned will increase the minority applicant pool. Table 10 list the minority predoctoral and postdoctoral fellowship recruitment data for the Department of Pharmacology; this table reflects the general experience of all other academic departments connected with the training program. Our experience has been that all minority candidates accepted to the various predoctoral and postdoctoral positions are outstanding and they are eligible to receive support from via a variety of mechanisms including University Fellowships, and NIH grants. We hope to increase the number of applicants using the strategies described above and to enroll them into this training program. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. E. Successes in Recruitment of Under-Represented Minority Trainees in Lung Research We have been successful thus far in recruiting a minority graduate student and a postdoctoral fellow in lung research, Mr. Raudel Sandoval and Dr. Theresa John, respectively. Both are outstanding trainees and are full and integral members of the training program. They participate in all training activities as described in this proposal, although they derive their stipend support from supplement awards from ongoing R01s because of the reduction in the number of trainee positions at the time of funding by 1 predoctoral and 1 post-doctoral position. Raudel Sandoval is a Ph.D. student. He received his undergraduate degree at The University of Illinois at Chicago. His work deals with the endothelial contractile protein, myosin light chain kinase, and regulation of endothelial barrier function. He works in Dr. Tiruppathi’s laboratory and collaborates with Dr. Malik. Mr. Sandoval is in the fourth year of his Ph.D. program. He has published 2 papers as a co-author (Time Course of Recovery of Endothelial Cell Surface Thrombin Receptor (PAR-1) Expression, C.A. Ellis, C. Tiruppathi, R. Sandoval, W. D. Niles and A. B. Malik, Am. J. Physiol., 276:C38-C49, 1999) and (Thrombin Induces Proteinase-activated Receptor-1 Gene Expression in Endothelial Cells via Activation of Gi-linked Ras/Mitogen-activated Protein Kinase Pathway, C.A. Ellis, A.B. Malik, A. Gilchrist, H. Hamm, R. Sandoval, T. Voyno-Yasenetskaya, and C. Tiruppathi, J. Biol. Chem. 274:13718-13727, 1999. He has also just submitted a paper as first author (Intracellular Calcium Stores Regulate Thrombin-Induced Increase in Endothelial Permeability, R. Sandoval, A. B. Malik, C. A. Ellis, L. Kiedrowsky, and C. Tiruppathi, Am J. Physiol.) Dr. Theresa John is a post-doctoral fellow in lung research. She is an U.S. citizen, who received her doctorate at the University of Lagos in Nigeria, and subsequently received research training at the University of Manchester in England. She came to Dr. Malik’s laboratory in the summer of 1998 to study mechanisms of clearance of albumin across alveolar epithelial cells. She has recently presented a paper (Faseb J. 13(A), 219.8, 1999) at the 1999 Experimental Biology Meetings (John, et. al., Transalveolar Albumin Transport: Evidence for a Saturable Albumin Binding Site). Dr. Cordus Easington is a medical student enrolled in The University of Illinois College of Medicine. Through the effort of the program, he receives an institutional stipend because of his future interest in entering lung research training program. He completed his B.Sc. at Georgetown University in Washington, D.C. and Ph.D. in Pharmacology at Rush-Presbyterian-St. Luke’s Medical Center, and has subsequently enrolled as a medical student at the University of Illinois College of Medicine. Although Dr. Easington is not a research trainee in the program as yet, his intent is to pursue advanced training in lung research after having completed his medical degree. Thus, he spends all of his available time in research with the presumption that he will enter the training program upon completion of his medical training. We have developed this novel approach to nurture Dr. Easington’s interests in lung research during his medical program. F. Recruitment of Women in the Training Program Table 11 lists the number of women in the training program from its inception. It is clear that we have been committed to recruiting women at both the predoctoral and postdoctoral levels. 4. Responsible Conduct of Research All trainees are required to take the course entitled “Scientific Integrity and Responsible Conduct” given by Professor Robert Kelly (outline is in Table 8b). This is a lecture-based course interspersed with in-depth discussions and case studies of the key topics in the outline. The specific PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. details of the course, its contents, involvement of the faculty and trainees, and how the course is given is described in Table 8b. 5. Progress Report (7-1-95 to 5-1-99) A. General Attributes of the Program and its Developments There have been several important accomplishments of the Lung Biology and Pathobiology Training Program in its initial cycle. The first is that the training program has now been systematized and integrated along interdisciplinary lines at The University of Illinois College of Medicine. Multiple productive linkages based on research interests and the common goal of providing multidisciplinary lung research training have developed amongst the training faculty members to the ultimate benefit of the trainees. In addition, the training program has become an integral component of the institution as evident by the well-attended weekly research seminars in lung biology (Lung Research Seminar) that are supplemented by presentations from visiting scientists and consultants. In other words, the training program has now become a distinct institutional entity. Because of the recruitment of the specialized and outstanding training faculty, which is the “heart and soul” of the program, the trainees have access to a variety of research opportunities and strategies ranging from molecular approaches to lung physiology. The training program has been essential in bringing together such a talented and diverse faculty along a thematic line. The trainees themselves have also aided in building linkages amongst the training faculty because of the strengths such as the inquisitive spirit that they have brought to the program. A major aspect of the program is that it has enabled these trainees access to the various training faculty members solely on the basis of the particular research questions being addressed and their own intellectual curiosity. This level of integration could not have occurred without the program. The Ph.D. students supported by the training program (who were uninitiated in research when they joined the program) have benefitted from the many layers of research interactions and different ways of addressing questions as well as the availability of specialized courses (e.g., Lung and Vascular Biology) that cross departmental lines. Moreover, all trainees have benefitted from the intellectually stimulating environment created and fostered by the program. An important spin-off of the program has been the improvement in the overall quality of the training efforts of several components of the College of Medicine. Another major accomplishment has been our ability even in a short time since the program’s inception to compete successfully for outstanding Ph.D. students and postdoctoral fellows for admission into the program. We believe that the interdisciplinary research training environment has been a major reason for our successes in recruitment. Table 12 lists the positions awarded and committed since the inception of the program. Table 13 identifies these individuals, their research areas, current positions, and other training support received by them. Tables 14 and 14a list the trainees’ publications and their achievements. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Seven postdoctoral and six predoctoral trainees have been recruited into the program since its inception (Table 12). All were recruited on the basis of intense competition and their outstanding potential. Because this is our first funding period, these individuals are still early in their career development (Table 13). Nevertheless of the four postdoctoral fellows who completed their training, Dr. David Beno is an Assistant Professor in the Department of Pediatrics at RushPresbyterian-St. Luke’s Medical Center in Chicago, IL., Dr. Walter Niles is a Group Leader/Principal Investigator at Aurora Biosciences in La Jolla, CA, Dr. Karen Buchkovich-Sass is a Senior Scientist at Cephalon Laboratories in Philadelphia, PA, and Dr. Annette Gilchrist has accepted a position as Assistant Professor in the Department of Pharmacology and Molecular Biology at Northwestern University School of Medicine. Of the predoctoral trainees who have completed their training, Dr. Chad Ellis is in postdoctoral training with Dr. Geoffrey L. Clark at National Institutes of Health; Dr. Andrea True has accepted a postdoctoral training appointment at the Department of Medicine, University of Michigan under Dr. Elizabeth G. Nabel. Dr. True will move with Dr. Nabel to NIH upon completion of her laboratories. One of the trainees (Dr. Buchkovich-Sass) was the recipient of the competitive Parker B. Francis Award, thus freeing up a position for another trainee to be appointed. Three out of the six postdoctoral trainees and one out of the six predoctoral trainees have been women. In addition, one Hispanic-American (Raudel Sandoval) pre-doctoral trainee and one African-American post-doctoral trainee (Dr. Theresa John) are both integral members of the lung research training program as described above. Thus, it is evident that our trainees are on a successful track, and future evidence of their successes will accumulate as they establish their research careers. Trainee publications, an indication of their accomplishments and their other achievements, are listed in Table 14 and Table 14a, respectively. Another significant accomplishment has been the development of a graduate level course in Lung and Vascular Biology. This course is directed by Drs. R. Skidgel and C. Tiruppathi (both members of the training faculty) and has significant involvement from all members of the training faculty, including the Program Director. The establishment of this specialized required course as well as other graduate level courses directed by other training faculty members (such as the course on Platelet Activation Mechanisms directed by Drs. LeBreton and Lam and the course on Receptors and Signaling developed by Drs. Mark Rasenick and Richard Green) greatly benefit the trainees not only in the program but also a variety of other trainees at The University of Illinois. In summary, although we are nearing the end of the first cycle (Year 04), the training program has matured progressively during this period. It has created a productive and intellectually stimulating training environment by assembling a group of highly qualified interdisciplinary faculty members who provide research training opportunities for predoctoral students and postdoctoral fellows. The trainees recruited on the basis of their credentials, research interests, and potential have been outstanding and the training environment created under the umbrella of the training program has clearly benefitted them. Even at the early stages of their development, it is apparent that our postdoctoral trainees have accepted fulfilling research and academic positions and the graduate students who have completed their Ph.D. training have accepted outstanding postdoctoral fellowships. B. Research Conducted by Trainees Supported by the Program The specific research carried out by the trainees supported by the program is indicated in Table 14b. This table provides the abstracts of their research studies. 6. HUMAN SUBJECTS See Table 15 7. VERTEBRATE ANIMALS See Table 16 PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. ATTACHMENT #3 PCOL 530 PHARMACOLOGY AND VASCULAR BIOLOGY Fridays, 2:00 – 4:00 PM, 419 CMW Course Directors: Dr. Randal A. Skidgel, 412 CSN; Phone: 996-9179; Email: rskidgel@uic.edu Dr. Chinnaswamy Tiruppathi, 1006A CME; Phone: 355-0249; Email:tiruc@uic.edu Date Topic Jan 16 Introduction to the Course Overview of Vascular Biology Jan 23 Endothelial cell cytoskeleton, signaling and barrier function Jan 30 The plasminogen system in cardiovascular disease Feb 6 Endothelial cell adhesion molecules Feb13 Endothelial cell adhesion and leukocyte trafficking Feb 20 Vascular Inflammation, oxidant signaling and gene expression Feb 27 Nitric Oxide and the regulation of nitric oxide synthases Mar 5 Novel functions of myeloperoxidase Smooth muscle cell proliferation Mar 12 Cadherins in cellular adhesion and signaling Mar 19 Thrombin receptor activation and signaling in endothelial cells Mar 26 Spring Break, No Class Apr 2 Angiotensin converting enzyme, angiotensin and bradykinin Apr 9 Hypertension Measurement of barrier function in vivo Apr 16 Transcellular permeability pathway in endothelial cells Apr 23 Student Presentations Apr 30 Angiogenesis May 7 Final Exam Grading: Grades will be based on the following formula: Attendance: 10% Student Presentation: 15% Student Paper: 25% Final Exam: 50% PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Instructor Randal Skidgel D. Mehta Randal Skidgel Xiaoping Du Richard Ye Asrar Malik Randal Skidgel C. Tiruppathi Richard Minshall Michael Broman C. Tiruppathi Ervin Erdös Steve Vogel Richard Minshall Karen Snapp Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. ATTACHMENT #4 (2 United States Patent Sutton , et al. of 3) 6,204,054 March 20, 2001 Transcytosis vehicles and enchancers for drug delivery Abstract Transcytosis of a physiologically-active agent that exerts its action following passage across endothelia, epithelia or mesothelia containing the GP60 receptor is enhanced by formulation with or conjugation to a transcytosis enhancer or vehicle selected from albumin and fragments thereof, antiGP60 antibody and fragments thereof, GP60 peptide fragments, and PDI (protein disulphide isomerase) and fragments thereof. Inventors: Sutton; Andrew Derek (Grantham, GB); Malik; Asrar Bari (Chicago, IL); Tiruppathi; Chinnaswamy (Chicago, IL); Johnson; Richard Alan (Nottingham, GB) Assignee: Andaris Limited (GB) Appl. No.: 043412 Filed: June 25, 1998 PCT Filed: September 20, 1996 PCT NO: PCT/GB96/02326 371 Date: June 25, 1998 102(e) Date: June 25, 1998 PCT PUB.NO.: WO97/10850 PCT PUB. Date: March 27, 1997 Foreign Application Priority Data Mar 26, 1996[GB] Current U.S. Class: 9606315 435/334; 424/143.1; 424/158.1; 424/447; 435/371 PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Intern'l Class: Field of Search: Malik, Asrar B. C12N 005/06; C12N 005/08; A61K 039/395; A61L 015/16 435/334,371 424/447,143.1,158.1 References Cited [Referenced By] 5254342 WO 88/00834 WO 93/20834 U.S. Patent Documents Oct., 1993 Shen et al. Foreign Patent Documents Feb., 1988 WO. Oct., 1993 WO. Other References Ghitescu, L. et al., "Specific Binding Sites for Albumin Restricted to Plasmalemmal Vesicles of Continuous Capillary Endothelium: Receptor-mediated Transcytosis," J. Cell. Biol. 102:1304-1311 (1986). Schnitzer, J. E., "gp60 is an albumin-binding glycoprotein expressed by continuous endothelium involved in albumin transcytosis," Am. J. Physiol. 262 (Heart Circ. Physiol. 31):H246-H254 (1992). Schnitzer, J. E. and Oh, P., "Antibodies to SPARC inhibit albumin binding to SPARC, gp60, and microvascular endothelium," Am. J. Physiol. 263 (Heart Circ. Physiol. 32):H1872-H1879 (1992). Schnitzer, J. E. and Oh, P., "Albondin-mediated capillary permeability to albumin. Differential role of receptors in endothelial transcytosis and endocytosis of native and modified albumins,"J. Biol. Chem. 269:6072-6082 (Feb. 1994). Database Medline, Accession No. 94164970 (Abstract). Primary Examiner: Park; Hankyel T. Attorney, Agent or Firm: Saliwanchik, Lloyd & Saliwanchik Parent Case Text CROSS-REFERENCE TO RELATED APPLICATION This application is a U.S. national phase application corresponding to International Patent Application No. PCT/GB96/02326, filed Sep. 20, 1996 (pending). This application claim benefit to provisional application Ser. No. 60/004,097 Sep. 21, 1995. Claims PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. 424/401. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. What is claimed is: 1. A composition comprising, or conjugate of, a physiologically-active agent that exerts its action following passage across endothelia, epithelia or mesothelia containing the GP60 receptor, and a transcytosis enhancer or vehicle selected from albumin and fragments thereof, anti-GP60 antibody and fragments thereof, GP60 peptide fragments, and PDI (protein disulphide isomerase) and fragments thereof; wherein said composition or conjugate is a dry powder suitable for inhalation. 2. The composition or conjugate according to claim 1, wherein the transcytosis enhancer or vehicle includes the CGMC motif. 3. The composition or conjugate according to claim 1, wherein the transcytosis enhancer or vehicle comprises albumin or an albumin fragment. 4. The composition or conjugate according to claim 1, wherein the transcytosis enhancer or vehicle comprises anti-GP60 antibody or an anti-GP60 antibody fragment. 5. The composition or conjugate according to claim 1, wherein the transcytosis enhancer or vehicle comprises a GP60 peptide fragment. 6. The composition or conjugate according to claim 1, wherein the transcytosis vehicle comprises albumin or an albumin fragment in combination with a GP60 peptide fragment. 7. The composition or conjugate according to claim 5 or claim 6, wherein the GP60 peptide fragment is or comprises SEQ ID No. 1. 8. The composition or conjugate according to claim 1, wherein the physiologically-active agent is selected from the group consisting of Luteinizing hormone (LH), chorionic gonadotropin, atrial peptides, interferon, lymphokines I, lymphokine II, lymphokine III, lymphokine IV, lymphokine V, lymphokine VI, lymphokine VII, a colony-stimulating factor, growth hormone-releasing factor, corticotropin-releasing factor, luteinizing hormone-releasing hormone (LHRH), somatostatin, calcitonin, thyrotropin-releasing hormone, calcitonin gene-related peptide (CGRP), transferases, hydrolases, isomerases, proteases, ligases, oxidoreductases, esterases, phosphatases, nerve growth factor (NGF), ciliary neurotrophic factor (CNTF), brain-derived neurotrophic factor (BDNF), glialderived neurotrophic factor (GDNF), epidermal growth factor (EGF), fibroblast growth factor (FGF), insulin-like growth factor, tumour necrosis factor (TNF), transforming growth factor (TGF), encephalins, endorphins, gonadoliberin, melanostatin, melonoliberin, somatostatin, thyroliberin, substance P, neurotensin, corticotropin, lipotropin, melanotropin, lutropin, thyrotropin, prolactin, somatotropin, neurohypophyseal hormones, parathyrin, calcitonin, thymosin, thymopoietin, circulating thymic factor, thymic humoral factor, insulin, glucagon, somatostatin, gastrin, cholecystokinin, secretin, gastric inhibitory polypeptide, vasointestinal peptide, motillin, relaxin, angiotensin, bradykinin, somatomedins, epidermal growth factors, urogastrone, deferoxamine, buserelin, deslorelin, gonadorelin, goserelin, histrelin, leuprorelin, nafarelin, and triptorelin. 9. In a method for administering a physiologically-active agent to a mammal, the improvement PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. comprising: administering said active agent either conjugated to or in admixture with a transcytosis vehicle or enhancer as defined in claim 1, wherein said transcytosis vehicle or enhancer delivers or enhances passage of said physiologically-active agent across epithelia, endothelia, or mesothelia containing the GP60 receptor. 10. The method of claim 9, wherein said physiologically-active agent is selected from the group consisting of Luteinizing hormone (LH), chorionic gonadotropin, atrial peptides, interferon, lymphokine I, lymphokine II, lymphokine III, lymphokine IV, lymphokine V, lymphokine VI, lymphokine VII, a colony-stimulating factor, growth hormone-releasing factor, corticotropinreleasing factor, luteinizing hormone-releasing factor (LHRH), somatostatin, calcitonin, thyrotropinreleasing hormone, calcitonin gene-related peptide (CGRP), transferases, hydrolases, isomerases, proteases, ligases, oxidoreductases, esterases, phosphatases, nerve growth factor (NGF), ciliary neurotrophic factor (CNTF), brain-derived neurotrophic factor (BDNF), glial-derived neurotrophic factor (GDNF), epidermal growth factor (EGF), fibroblast growth factor (FGF), insulin-like growth factor, tumor necrosis factor (TNF), transforming growth factor (TGF), encephalins, endorphins, gonadoliberin, melanostatin, melonoliberin, somatostatin, thyroliberin, substance P, neurostensin, corticotropin, lipotropin, melanotropin, lutropin, thyrotropin, prolactin, somatotropin, neurohypophyseal hormones, parathyrin, calcitonin, thymosin, thymopoietin, circulating thymic factor, thymic humoral factor, insulin, glucagon, somatostatin, gastrin, cholecystokinin, secretin, gastric inhibitory polypeptide, vasointestinal peptide, motillin, relaxin, angiotensin, bradykinin, somatomedins, epidermal growth factors, urogastrone, deferoxamine, buserelin, deslorelin, gonadorelin, goserelin, histrelin leuprorelin, nafarelin, and triptorelin. 11. The method of claim 9, wherein said physiologically-active agent is conjugated to said transcytosis vehicle by a method selected from the group consisting of glutaraldehyde conjugation using Schiff base formation, carbodiimide reaction between proteins and carboxylic acids, acid anhydride activation of amine containing drugs followed by carbodiimide linkage, activation of primary amine containing drugs with 3-(2-pyridyldithio)proprionate-N-succinimidyl anhydride followed by coupling to cysteine groups of proteins, coupling of sugar alcohols to proteins utilizing cyanuric chloride, and conjugation between amines and hydroxyl groups via bisperoxidation. 12. The method of claim 9, wherein said mammal is human. 13. The composition or conjugate, according to claim 1, which further comprises an excipient. 14. The composition or conjugate, according to claim 1, which comprises microparticles of the active agent which are from 2 to 5 .mu.m in size. 15. An inhaler device which comprises a composition comprising, or conjugate of, a physiologicallyactive agent that exerts its action following passage across endothelia, epithelia or mesothelia containing the GP60 receptor, and a transcytosis enhancer or vehicle selected from albumin and fragments thereof, anti-GP60 antibody and fragments thereof, GP60 peptide fragments, and PDI (protein disulphide isomerase) and fragments thereof; wherein said composition or conjugate is a dry powder suitable for inhalation. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Description FIELD OF THE INVENTION The invention relates to drug delivery. In particular, the invention relates to transcytosis vehicles and enhancers capable of delivering and enhancing passage of drugs across endothelia, epithelia and mesothelia containing the GP60 receptor. BACKGROUND OF THE INVENTION For most therapeutic drugs administered by intra-arterial or intravenous routes the intended site of molecular activity lies outside the vasculature. For drugs administered via the airways, the intended site of activity normally is beyond the first cellular barrier of alveolar, bronchiolar or tracheal epithelia. In both cases, there is an endothelial or epithelial barrier which must be crossed before the drug can mediate its effect. For small lipophilic drugs, there appears to be a paracellular route between the tight junctions of the barrier cells. However, for hydrophilic drugs and larger macromolecular active agents, such as peptides, proteins, genes or anti-sense nucleotides, the only route across the barrier is through the cells. This poses a particular problem for drugs administered intravenously which have exceedingly short half-lives due to rapid degradation or first pass clearance by the liver. In order to maintain therapeutic levels in balance with such excretion and degradation, large doses or infusions are often necessary. Thus, there is clearly a need in the art for more rapid mechanisms for delivering drugs across cellular barriers. There have been numerous reports of specific receptors which mediate endocytotic events, where a ligand binds to the receptor and is then internalized, complexed to the receptor, by a process similar to pinocytosis. This involves invagination of the cell membrane in the region of the ligand receptor complex and then release of the ligand into the cell by a process which is not fully understood. Numerous endocytotic receptor systems have been reported including LDL, insulin, epidermal growth factor, insulin-like growth factor and tPA-PAI-I (hybrid molecule). Transcytosis entails invagination and vesicle formation around a ligand receptor complex, followed by transcytotic passage with release by a reverse invagination process at the basolateral membrane. Monoclonal antibodies to the transferrin receptor have been conjugated with toxins, so that they can undergo transcytosis, across blood-brain endothelia. However, there is a continuing need in the art for agents capable of delivering or enhancing passage of drugs by receptor-mediated transcytosis across cellular barriers other than blood-brain endothelia, such as endothelia of the vasculature, alveolar epithelia, and peritoneal mesothelia. The GP60 receptor, also referred to as albondin, is one of several albumin-binding proteins reported in the literature (Schnitzer and Oh, J. Biol. Chem. 269(8):6072-6082 (1994)). Others include SPARC (serum protein, acidic, rich in cysteine), oesteonectin or basement membrane protein 40, GP30, GP18 and GP60. SPARC and oesteonectin are extra-cellular proteins. GP60 shares some homology with SPARC as determined using anti-SPARC antibodies (Schnitzer and Oh, Am. J. Physiol. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. 263:H1872-H1879 (1992)). GP18 and GP30 are membrane glycoproteins found in a variety of cell types but are particularly prevalent in the macrophage (Schnitzer et al, J. Biol. Chem. 267: 24544-24553 (1992)). GP18 and GP30 are the so-called "scavenger receptors" responsible for mediating removal of oxidized, glycated or adduced forms of albumin by endocytosis and are thus believed to play a role in albumin catabolism for a wide variety of organs (Schnitzer and Bravo, J. Biol. Chem. 268(10):7562-7570 (1993)). In contrast to GP18 and GP30, the GP60 receptor has found to be expressed exclusively in continuous endothelia of the vasculature (Schnitzer, Am. J. Physiol. 262:H246-H254 (1992)), in alveolar epithelia (Kim et al, Am. J. Resp. and Crit. Care Med. 151:A190, (1994) and inferentially in peritoneal mesothelia (Gotloib and Shostak, Kidney International. 47:1274-1284 (1995)). GP60 is particularly abundant in the microvessel endothelia and is, interestingly, absent from the blood-brain barrier, where little albumin flux is observed (Rousseaux et al, Methods in Enzymology 121:163 (1986)). It has been shown that polyclonal antibodies to endothelial GP60 also bind alveolar epithelial GP60 (Kim et al, supra). The GP60 receptor has been implicated in receptor-mediated transcytosis of albumin across epithelia and endothelial cell barriers (Kim et al, supra; Tirrupathi et al, Molecular Biology of the Cell 4 (Supp):338a, Abstract No. 1964 (1993)). The GP60 amino acid sequence is known in the art (Yamauchi et al, Biochem. Biophys. Res. Comm. 146:1485 (1987)). SUMMARY OF THE INVENTION The present invention provides transcytosis vehicles and enhancers capable of transporting physiologically-active agents across epithelia, endothelia and mesothelia containing the GP60 receptor. The GP60 receptor has been implicated in receptor-mediated transcytosis of albumin across cell barriers. By means of the invention, GP60 receptor-mediated transcytosis can be exploited for the transport of not only albumin, but also physiologically-active agents which do not naturally pass through epithelia, endothelia and mesothelia via the GP60 system. Transcytosis vehicles and enhancers of the invention include albumin, albumin fragments, anti-GP60 polyclonal and monoclonal antibodies, anti-GP60 polyclonal and monoclonal antibody fragments, and GP60 peptide fragments. Further, they include PDI (protein disulphide isomerase) and fragments thereof (any subsequent reference to GP60 fragments may be interpreted as referring also to PDI fragments). A common factor may be a CGMC motif found in PDI and at least the T.sub.1-44 fragment of GP60. If the transcytosis vehicle or enhancer is a GP60 peptide fragment, it is preferably co-administered with other transcytosis vehicles or enhancers of the present invention such as albumin or an albumin fragment. Suitable albumin fragments of 14, 20 and 32 kDa can be generated by cleavage at methionine residues using cyanogen bromide and can be further reduced in size by reduction of disulfide bridges. Anti-GP60 polyclonal and monoclonal antibody fragments useful as transcytosis vehicles and enhancers according to the present invention include Fab, Fab', F(ab').sub.2, and Fv fragments. Preferred GP60 peptide fragments include the T3118 peptide which corresponds to the N-terminal 18 amino acids of the GP60 protein. In accordance with the invention, when the above compounds are conjugated to a physiologicallyPHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. active agent, they are referred to herein as "transcytosis vehicles". When co-administered with but not conjugated to a physiologically-active agent, the above compounds are referred to herein as "transcytosis enhancers". In preferred embodiments, the transcytosis vehicles and enhancers of the present invention are useful for delivering or enhancing passage of physiologically-active agents across endothelia of the vasculature, alveolar epithelia and peritoneal mesothelia. DETAILED DESCRIPTION OF THE INVENTION As its name indicates, the GP60 protein has been reported in the art as having a molecular weight of about 60 kDa. After a more careful analysis, it has been discovered that the "true" molecular weight for this protein is more probably about 57 kDa. This discrepancy in molecular weight is thought to be due to differences in protein preparation and gel conditions. However, to be consistent with the art, this protein is referred to herein (with the exception of Example 1 below) as the GP60 receptor. It has been discovered that GP60 receptor-mediated transcytosis can be exploited for the transport of not only albumin, but also for a vast number of therapeutically-important physiologically-active agents which do not naturally pass through epithelia, endothelia and mesothelia via the GP60 system. Thus, the present invention provides an improved method for transporting physiologicallyactive e.g. those having relatively high molecular weights, e.g. 50, 100, 150 kDa or more, across the cellular barriers of the endothelia of the vasculature, alveolar, bronchiolar, and tracheal epithelia, and the peritoneal mesothelia. Transcytosis vehicles and enhancers capable of delivering or enhancing passage of physiologically-active agents across GP60-containing endothelia, epithelia and mesothelia include albumin, albumin fragments, anti-GP60 polyclonal and monoclonal antibodies, anti-GP60 polyclonal and monoclonal antibody fragments, and GP60 peptide fragments. If the transcytosis vehicle or enhancer is a GP60 peptide fragment, it will preferably be co-administered with other transcytosis vehicles or enhancers of the present invention such as albumin or an albumin fragment. Mammalian albumin is well known in the art and readily available. Preferably, the albumin used will be from the same mammalian species as the patient. For example, if the patient is human, human serum albumin will preferably be used as the transcytosis vehicle or enhancer. Similarly, if the patient is equine or bovine, equine or bovine serum albumin is preferably used, respectively. Methods for generating albumin fragments are well known in the art. For example, cleavage of albumin at methionine residues by cyanogen bromide yields three particularly suitable peptides of 14, 20 and 32 kDa which can be further reduced in size by reduction of the disulfide bridges, to peptides ranging in size from 3.3-20 kDa. Alternatively, protease digestion can be used to generate albumin peptide fragments. Whether any particular albumin fragment is useful as a transcytosis vehicle or enhancer according to the present invention can be determined according to the routine screening assay described below. As indicated in the Examples below, it has now been demonstrated that both bovine and human serum albumin, acting as transcytosis enhancers, stimulate uptake of a physiologically-active agent 2.5-4 fold over the control. Anti-GP60 polyclonal and monoclonal antibodies can be generated from the GP60 receptor purified from endothelia, epithelia or mesothelia. As discussed above, endothelial, epithelial and mesothelial PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. cells which express the GP60 receptor include endothelia of the vasculature (including capillary endothelia (Ghinea et al, J. Cell Biol. 107:231-239 (1988)); arterial endothelia (Silflinger-Birnboim et al, J. Cellular Physiology 149:575-584 (1991); aortic and vein endothelia (Schnitzer and Oh, Am. J. Physiol. (1992), supra); epithelia of alveolar tissue (Kim et al, supra); and mesothelia of the peritoneum (Gotloib and Shostak, supra). GP60 can be purified from epithelia, endothelia and mesothelia according to art-known methods (see, for example, Schnitzer and Oh, J. Biol. Chem. (1994), supra) and as described in Example 1 below. Producing polyclonal antibodies against purified GP60 or a GP60 peptide fragment (such as the T3118 peptide discussed below) can occur in mice, rabbits, or goats according to art-known techniques. In Example 1 below, the GP60 receptor was eluted from preparative SDS-PAGE to immunize rabbits. Approximately 50 .mu.g protein per rabbit was injected intramuscularly after mixing with equal volume of Freund's complete adjuvant. A second injection was given after two weeks. Rabbits were bled at 4 to 6 weeks after the second injection, and the immune response was tested. The antiserum IgG was then purified using a Protein A-Sepharose column. Monoclonal antibody preparation can also occur according to known techniques (Goding, J. Immunol. Methods 39:285 (1980); Oi and Herzenberg, Selected Methods in Cellular Immunology, p. 352, Freeman, San Francisco, 1979)). For example, Balb/c mice are injected intraperitoneally with 50-150 .mu.g of GP60 or a GP60 peptide fragment. Three to five days before the fusion, positive mice receive a booster injection of antigen (50-150 .mu.g of GP60 or GP60 fragment), and then 10 .mu.g (intravenous and intraperitoneal route) every day until spleen removal. The spleen cells are fused with Sp2/0-Ag14 myeloma cells essentially according to St. Groth et al, J. Immunology Methods 35:1-21 (1980). Culture supernatants are screened by ELISA using unconjugated GP60 or GP60 fragment as antigen. Positive cultures are then tested by immunofluorescence and Western blotting on cDNA-transfected COS-1 cells as described in Lutz et al, Experimental Cell Research 175:109-124 (1988). Hybridomas secreting specific antibodies are cloned twice on soft agar. Each hybridoma can be adapted in serum-free medium SFRI-4. For ascites fluid production, approximately 2.times.106 cells are injected in pristine-primed Balb/c mice. Class and subclass determination is performed using an Isotyping Kit. Both SFRI culture supernatants and ascites fluids can be used as monoclonal antibody sources. As discussed, the anti-GP60 polyclonal and monoclonal antibodies and antibody fragments of the present invention are useful as transcytosis vehicles and enhancers capable of delivering or enhancing passage of physiologically-active agents across endothelia, epithelia and mesothelia containing the GP60 receptor. Anti-GP60 antibody fragments useful as transcytosis vehicles or enhancers of the present invention include fragments containing single (Fab) antigen binding domains produced by papain digestion; or F(ab').sub.2 fragments produced by limited pepsin digestion (Olsson and Kaplan, Methods in Enzymology 92:3 (1983)). Other suitable fragments include Fab' and Fv. Whether any particular antibody fragment is useful as a transcytosis vehicle or enhancer can be determined according to the routine screening assay described below. In Example 3 below, it is demonstrated that administering anti-GP60 polyclonal antibodies at 37.degree. C. results in a 1.6-2 fold increase in uptake of a physiologically-active agent over the level of a pre-immune serum control. According to the invention, anti-GP60 antibodies raised in animals other than humans such as mice and rats are suitable for short-term administration only (i.e., non-chronic dosage) due to the wellPHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. known adverse immune response to foreign antibodies. However, art-described methods can be used to produce human monoclonal antibodies to the GP60 receptor, to overcome the problems of administering murine monoclonals to humans (Olsson and Kaplan supra), thereby rendering the antibodies suitable for long-term or chronic administration. Moreover, the murine antibodies of the present invention can be "humanized" by chimeric or CDR grafting. The recognition region of the murine antibody is grafted into the appropriate region of a human antibody, in order to avoid or limit an adverse immune response in a patient. GP60 peptide fragments are also useful as transcytosis vehicles and enhancers according to the present invention. Particularly suitable GP60 peptide fragments include the first 18 amino acids from the N-terminus of GP60; it has been discovered that this is at least 80% homologous to a stretch of the bovine, membrane-bound thyroid hormone (T3) binding protein. Such GP60 peptide fragments can be produced according to any known enzymatic or physical technique, including proteolytic degradation. Alternatively, GP60 peptide fragments can be produced synthetically. As indicated in Example 5 below, a synthetic N-terminal peptide (T3118) of GP60 corresponding to the first 18 residues may be produced by solid-phase synthesis. This peptide, acting as an agonist of transcytosis, stimulated uptake of human albumin 5-fold over the control. Methods for conjugating the transcytosis vehicles of the present invention to a physiologically-active agent will be readily apparent to the skilled artisan and include, but are not limited to, glutaraldehyde conjugation involving Schiff base formation; carbodiimide reaction between proteins and carboxylic acids; acid anhydride activation of amine-containing drugs followed by carbodiimide linkage; activation of primary amine-containing drugs with 3-(2-pyridyldithio)propionate-N-succinimidyl anhydride followed by coupling to cysteine groups of proteins; coupling of sugar alcohols to proteins utilizing cyanuric chloride; and conjugation between amines and hydroxyl groups via bisperoxidation. For example, the amino sugar moiety of a physiologically-active agent can be oxidized by sodium periodate treatment and directly attached to lysine residues on a transcytosis vehicle of the present invention via Schiff base formation according to the method described in Hurwitz et al, Cancer Res. 35:1175-1181 (1975). Alternatively, a physiologically-active agent can be linked to a transcytosis vehicle of the present invention through carbodiimide-mediated linkage of the amino group of the active to carbonyl groups on the vehicle or to an aminoalkyl group according to the method described in Hurwitz et al, Int. J. Cancer 21:747-755 (1978). The physiologically-active agent can also be linked to a transcytosis vehicle of the present invention by cross-linking the amino sugar of the active and amino groups of the vehicle with glutaraldehyde according to the method described in Belles-Isles et al, Br. J. Cancer 41:841-842 (1980). Other suitable conjugation sites for conjugating physiologically-active agents to one of the transcytosis vehicles of the present invention can be routinely determined empirically. For example, a transcytosis vehicle of the present invention can be labelled with fluorescein or .sup.125 I either before or after conjugation to a physiologically-active agent such as insulin. After conjugation and labelling, a screening assay such as that described in the Examples below can be used to determine the endothelial cell uptake, the epithelial cell flux, or the mesothelial cell flux of any candidate vehicle/active conjugate. Such a routine screening assay allows the skilled artisan to determine which transcytosis vehicles of the present invention retain the ability to undergo transcytosis after being conjugated at a particular site to a physiologically-active agent. Such an assay is also useful PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. for routine screening of candidate albumin fragments, anti-GP60 antibody fragments and GP60 peptide fragments to determine which are suitable (for use as transcytosis vehicles and enhancers according to the present invention. The conjugation of physiologically-active agents to a transcytosis vehicle of the present invention is particularly suited for intravenous delivery of low molecular weight drugs which otherwise have exceedingly short serum half-lives, or of peptide drugs that are rapidly degraded in the blood stream or removed by first pass excretion in the liver. Of course, where the physiologically-active agent is covalently conjugated to one of the transcytosis vehicles of the present invention, the residual activity of the therapeutic agent must be assessed after conjugation. Techniques for assaying a therapeutic agent's activity are well established in the art, and many therapeutics have successfully been conjugated and retained substantial activity. For example, the literature describes conjugates between receptor ligands, or fragments thereof, and drugs to promote transcytosis across the blood brain barriers. Fukta et al, Pharm. Research 11(12):1681 (1994), describe conjugation of horse radish peroxidase (HRP) to insulin which enabled HRP to cross the blood, brain barrier. The investigators went on to produce fragments of insulin which were screened for their ability to bind to the insulin receptor on bovine brain microvessel endothelial cells in culture. Similarly, other transcytosis systems allow the passage of antibodies linked with active drugs including, among others, antibodymethotrexate targeted to the transferrin receptor (Friden et al, Proc. Natl. Acad. Sci. USA 88:4771 (1991)), and antibody-polylysine targeted to the epidermal growth factor receptor (Chen et al, FEBS Lett. 338:167 (1994)). By contrast to the transcytosis vehicles, transcytosis enhancers of the invention are not conjugated to the physiologically-active agent. It has been discovered that co-residence on epithelia, endothelia and mesothelia containing the GP60 receptor of one of the transcytosis enhancers of the present invention and a physiologically-active agent is sufficient to enhance uptake and passage of the agent across the cell barrier. Without wishing to be bound by theory, the transcytosis enhancers of the present invention apparently "trigger" the GP60-mediated transcytosis mechanism, thereby stimulating the enhanced uptake of co-resident macromolecules, including therapeutic agents. Uptake or passage of physiologically-active agents by or across epithelia, endothelia and mesothelia can be induced or enhanced with any of the transcytosis enhancers of the present invention either alone or in combination. For example, the experiments below demonstrate that, acting as an agonist of transcytosis, the GP60 peptide T3118 enhanced human albumin uptake 5-fold over the control. In a further embodiment of the present invention, delivery of active agents can be achieved when one of the transcytosis vehicle conjugates discussed above is administered together with one or more of the transcytosis enhancers of the present invention. The transcytosis vehicle conjugates and the transcytosis enhancer compositions (including an active agent) of the present invention can be administered with a pharmaceutically-acceptable carrier or excipient, i.e., pharmaceutically-acceptable organic or inorganic substances suitable for application which do not deleteriously react with the conjugate or composition. Suitable pharmaceuticallyacceptable substances include but are not limited to water, salt solutions, alcohol, vegetable oils, polyethylene glycols, gelatin, lactose, amylose, magnesium stearate, talc, silicic acid, viscous paraffin, perfume oil, fatty acid monoglycerides and diglycerides, petroethral fatty acid esters, hydroxymethylcellulose, polyvinylpyrrolidone, etc. The pharmaceutical preparations can be sterilized and, if desired, mixed with auxiliary agents, e.g., lubricants, preservatives, stabilizers, PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. wetting agents, emulsifiers, salts for influencing osmotic pressure, buffers, colourings, flavouring and/or aromatic substances, which do not deleteriously react with the conjugates. For parenteral application, particularly suitable preparations are solutions, preferably oily or aqueous solutions, as well as suspensions, emulsions, or implants, including suppositories. Ampoules are convenient unit dosages. For enteral application, particularly suitable preparations are tablets, dragees or capsules having a carrier binder such as talc and/or a carbohydrate, the carrier preferably being lactose and/or corn starch and/or potato starch. A syrup, elixir or the like can be used wherein a sweetened vehicle is employed. Sustained release compositions can be formulated including those wherein the active component is protected with differentially degradable coatings, e.g., by microencapsulation, multiple coatings, etc. Administration of a conjugate or composition comprising one or more physiologically-active agents and one or more of the transcytosis vehicles or enhancers of the present invention can occur according to any art-known technique including injection or via the pulmonary airways. Injection is particularly suitable for administration to the vasculature and the peritoneum, whereas the pulmonary airways are particularly suitable for administration to the alveoli. Suitable formulations for pulmonary administration include one or more of the transcytosis enhancers of the present invention admixed with a physiologically-active agent. Alternative suitable formulations for pulmonary administration include a transcytosis vehicle conjugated to the agent. For example, formulations may be made from a nebulizer device such as an Acorn or DeVilbiss jet nebulizer, wherein the agent and transcytosis enhancer or vehicle are presented as an aqueous solution in the nebulizer reservoir. Alternatively, in a preferred embodiment for pulmonary administration, the formulation is discharged from a dry powder inhaler (DPI) device. DPI devices are described by Sutton et al in U.S. patent application Ser. No. 08/487,420 and in WO-9609814. They require spraydrying the formulation into microparticles of 2-5 .mu.m which are preferred for alveolar penetration. In particular, a transcytosis enhancer or vehicle of the present invention or a mixture thereof, preferably at a concentration of about 20% w/v, is used for spray-drying. The preparation to be sprayed may contain substances other than the transcytosis enhancers or vehicles and solvent or carrier liquid. For example, the aqueous phase may contain 1-20% by weight of water-soluble hydrophilic compounds such as sugars and polymers as stabilizers, e.g., polyvinyl alcohol (PVA), polyvinyl pyrrolidone (PVP), polyethylene glycol (PEG), gelatin, polyglutamic acid and polysaccharides such as starch, dextran, agar, xanthin and the like. Similar aqueous phases can be used as the carrier liquid in which the final microsphere product is suspended before use. Emulsifiers may be used (0.1-5% by weight), including most physiologically-acceptable emulsifiers, for instance egg lecithin or soya bean lecithin, or synthetic lecithins such as saturated synthetic lecithins, for example, dimyristoyl phosphatidylcholine, dipalmitoyl phosphatidylcholine, or distearoyl phosphatidylcholine or unsaturated synthetic lecithins, such as dioleyl phosphatidylcholine or dilinoleyl phosphatidylcholine. Emulsifiers also include surfactants such as free fatty acids, esters of fatty acids with polyoxyalkylene compounds, e.g. polyoxypropylene glycol and polyoxyethylene glycol; ethers of fatty alcohols with polyoxyalkylene glycols; esters of fatty acids with polyoxyalkylated sorbitan; soaps; glycerol-polyoxyethylene ricinoleate; homo-and copolymers of polyalkylene glycols; polyethoxylated soya-oil and castor oil as well as hydrogenated derivative; ethers and esters of sucrose or other carbohydrates with fatty acids, fatty alcohols, these being optionally polyoxyalkylated; mono-, di- and triglycerides of saturated or unsaturated fatty acids, glycerides or soya-oil and sucrose. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Additives can be incorporated into the wall of the microspheres to modify the physical properties such as dispersibility, elasticity and water permeability. Among the useful additives include compounds which can "hydrophobize" the wall in order to decrease water permeability, such as fats, waxes and high molecular weight hydrocarbons. Additives which improve dispersibility of the microspheres in the injectable liquid-carrier are amphipathic compounds such as phospholipids; they also increase water permeability and rate of biodegradability. Additives which increase wall elasticity include plasticizers such as isopropyl myristate and the like. The quantity of additives to be incorporated in the wall is extremely variable and depends on the needs. In some applications, no additive is used at all; in other cases, amounts of additives which may reach about 20% by weight of the wall are possible. A solution containing one or more transcytosis enhancers or vehicles of the present invention and additive, if any, is atomized and spray-dried by any suitable technique which results in discrete microspheres or microcapsules of 2 to 5 .mu.m as discussed above. As used herein, "microcapsules" refers to hollow particles enclosing a space, which space is filled with a gas or vapour but not with any solid materials. The atomization forms an aerosol of the transcytosis vehicle or enhancer formulation, for example by forcing the formulation through at least one orifice under pressure, or by using a centrifugal atomizer in a chamber of warm air or other inert gas. The chamber should be big enough for the largest ejected drops not to strike the walls before drying. The gas or vapour in the chamber is clean (preferably sterile and pyrogen-free) and non-toxic when administered to the bloodstream in amounts concomitant with administration of the microcapsules in use. The rate of evaporation of the liquid from the preparation should be sufficiently high to form hollow microcapsules but not so high as to burst the microcapsules. The rate of evaporation may be controlled by varying the gas flow rate, concentration of transcytosis vehicle or enhancer in the formulation, nature of liquid carrier, feed rate of the solution and, more importantly, the temperature of the gas encountered by the aerosol. For example, an albumin or albumin fragment concentration of 15-25% in water, and an inlet gas temperature of at least about 100.degree. C., preferably at least 110.degree. C., is sufficient to ensure hollowness and the temperature may be as high as 250.degree. C. without the capsule bursting. About 180-240.degree. C., preferably about 210-230.degree. C. and most preferably about 220.degree. C., is optimal. Since the temperature of the gas encountered by the aerosol will depend also on the rate at which the aerosol is delivered and on the liquid content of the preparation, the outlet temperature may be monitored to ensure an adequate temperature in the chamber. An outlet temperature of 40-150.degree. C. is suitable. Controlling the flow rate is useful in controlling other parameters such as the number of intact hollow particles. The microparticles may comprise at least 50%, more preferably 70% or 80%, and most preferably 90%, by weight transcytosis enhancer. For use in an inhaler device, the microparticles may be formulated with a conventional excipient such as lactose or glucose. The amount of the physiologically-active agent will be chosen with regard to its nature and activity, to the mode of administration and other factors known to those of skill in the art. By way of example, the number of particles administered may be such as to deliver 100 mg/day .alpha.-1 anti-trypsin, or 0.1 mg/day of an active agent such as beclomethasone. Other possible physiologically-active agents that can be administered via microparticles are given below. A further embodiment of the present invention is the co-spray-drying of the physiologically-active PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. agent with the transcytosis enhancer in order to facilitate stabilization of the active agent during formulation, packing, and most importantly, during residence on the alveolar lining. In this environment, there can be intense proteolytic activity. In this or another embodiment, the active agent may be covalently linked to the transcytosis vehicle via cleavable linkages prior to spraydrying. This embodiment represents a method of carrying the active agent all the way from the device to the bloodstream, and possibly to targets within the body. The formation of particles with optimal aerodynamic size means that the "physical" vehicle delivers the active agent to the site of absorption. Once deposited upon the alveoli, the "molecular" vehicle then protects and facilitates passage into the bloodstream via the GP60-mediated transcytosis system and, once in the bloodstream, can further enhance circulatory half-life and even direct the active agent to certain sites which are found to contain the GP60 receptor. Suitable linking technologies are discussed above; further, WO-A-9317713 describes esterase-sensitive polyhydroxy acid linkers. Such technology, used in the derivatization of the transcytosis vehicle prior to spray-drying, enables the production of a covalent carrier system for delivery of active agents to the systemic vasculature. This utilizes the potential of the transcytosis vehicles to cross the alveoli and to carry active agents over a prolonged period while protecting potentially unstable entities. Although the physiologically-active agent used in the present invention my be imbibed into or otherwise associated with the microparticles after their formulation, it is preferably formulated with the transcytosis vehicle or enhancer. The microparticles may be at least partly coated with a hydrophobic or water-insoluble material such as a fatty acid, in order to delay their rate of dissolution and to protect against hydroscopic growth. Methods and equipment for spray-drying and generating the microparticles, e.g. for use in a dry powder inhaler device are described in more detail in WO-A-9609814 and in U.S. patent application Ser. No. 08/487,420, the contents of which are incorporated herein by reference. The optimal proportions of drug to transcytosis enhancer in a formulation for pulmonary delivery can be determined according to any suitable method. An in vitro optimization of the formulation entails using epithelial monolayers of primary human or immortalized human epithelial cells grown as monolayers on porous filters, as described in the Examples below. Combinations of drug and enhancer may then be applied to the upper chamber of a transwell flux system also as described below. Using either labelled tracer or an immunoassay, flux rates of the drug or gene to the lower layer are determined. The optimal formulation is defined as the one showing maximal rate and extent of passage through the restrictive monolayer. An alternative way of optimizing the formulation entails performing an in vivo determination of lung to blood passage of the drug under investigation. There are well-reported studies in rat, pig and sheep (Patton et al, Journal of Controlled Release 28:79 (1994), Folkesson et al, Acta. Physiol. Scand. 147:73 (1993); Schreier et al, Pharm. Res. 11:1056 (1994)); these studies describe methods of instilling or aerosolizing drug formulations into the trachea and bronchioles and assessing the appearance in blood of the drug by immunoassay or pharmacological activity. Optimization would entail a series of animal preparations using differing proportions of the drug and enhancer, the optimal formulation being defined by the most beneficial area under the curve that matched the desired pharmacological profile for the drug. For instance, the drug may simply be required to show the maximal bioavailability or alternatively to show a protracted or sustained release profile. For each case, it is likely that there would be differing requirements for the level of enhancer PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Malik, Asrar B. Principal Investigator/Program Director (Last, first, middle): incorporated in the formulation. For drugs requiring maximal availability, it would be desirable to utilize the maximal level of enhancer and/or the enhancer showing the highest activating effect upon the GP60 receptor. For drugs requiring a longer period of presentation across the lung, it would be desirable to utilize lower levels of enhancer and/or enhancers showing lower activation potential on the transcytosis GP60 receptor. The "strength" of the enhancer or vehicle can be defined, by the extent to which transcytosis of a given tracer can be enhanced, by the presence of the GP60 receptor-binding ligand, antibody or mimetic, over the level of transcytosis in the absence of the ligand. The "strength" of the enhancing agent may be somewhat drug-dependent also. Enhancement of marker uptake can vary dependent upon the nature of the marker and the transcytosis enhancer. Tabulated below is a synopsis of the markers, enhancers, cell system and extent of enhancement over the control achieved for differing markers cell systems and experimental type. Abbreviations used: .sup.125 I-BSA bovine albumin .sup.125 I-IgG HSA BSA FITC-Insulin GP60 Ab T3118 .sup.125 Iodine-labelled Marker Enhancer .sup.125 I-BSA GP60 Ab .sup.125 I-BSA GP60 Ab anti-BSA BSA .sup.125 I-IgG FITCHSA Insulin FITCBSA Insulin .sup.125 I-BSA BSA/T3118 .sup.125 Iodine-labelled Immunoglobulin G Human albumin Bovine albumin fluorescein-labelled insulin Anti-GP60 polyclonal antibody Synthetic peptide derived from N terminal 18 residues of GP60 Fold Cell Type Enhancement Bovine/Endothelia/ 1.6 flux Bovine/Endothelia/ 2.0 flux Bovine/Endothelia/ 1.5 flux Human 2.5 Endothelia/flux Rat Epithelia/flux 4 Bovine Endothelia/uptake 5 By "physiologically-active agent" is intended drugs which include nucleic acid molecules and medicinal peptides and proteins. "Physiologically-active agent" is used interchangeably herein with "drug", "active", "active agent" and "therapeutic". Drugs that would benefit from a more rapid transcytosis across the endothelia and epithelia include Luteinizing hormone (LH), chorionic gonadotropin, atrial peptides, interferon, the various lymphokines such as the interleukins (I, II, III, IV, V, VI, and VII), and colony-stimulating factors. Other drugs suitable for use in the present invention include: Growth hormone-releasing factor, corticotropin-releasing factor, luteinizing hormone-releasing hormone (LHRH), somatostatin, calcitonin, thyrotropin-releasing hormone, calcitonin gene-related peptide (CGRP), proteins such as PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. enzymes, including transferases, hydrolases, isomerases, proteases, ligases, oxidoreductases, esterases and phosphatases, and various growth and neurotrophic factors, such as somatomedins, epidermal growth factors, urogastrone, nerve growth factor (NGF), ciliary neurotrophic factor (CNTF), brain-derived neurotrophic factor (BDNF), glial-derived neurotrophic factor (GDNF), epidermal growth factor (EGF), fibroblast growth factor (FGF), insulin-like growth factor, tumour necrosis factor (TNF) and transforming growth factor (TGF). Further drugs include endogenous opioid agonists, such as encephalins and endorphins; hypothalamic hormones, such as gonadoliberin, melanostatin, melonoliberin, somatostatin, thyroliberin, substance P, and neurotensin; adenohypophyseal hormones, such as corticotropin, lipotropin, melanotropin, lutropin, thyrotropin, prolactin, and somatotropin; neurohypophyseal hormones; calcitrapic (thyroid) hormones, such as parathyrin and calcitonin; thymic factors, such as thymosin, thymopoietin, circulating thymic factor, and thymic humoral factor; pancreatic hormones, such as insulin, glucagon and somatostatin; gastrointestinal hormones, such as gastrin, cholecystokinin, secretin, gastric inhibitory polypeptide, vasointestinal peptide, and motillin; ovarian hormones, such as relaxin; vasoactive tissue hormones, such as angiotensin and bradykinin; and artificial or pseudo peptides, such as deferoxamine; and LHRH analogs such as buserelin, deslorelin, gonadorelin, goserelin, histrelin, leuprorelin, nafarelin, or triptorelin. Having generally described the invention, the same will be more readily understood through reference to the following Examples which are provided by way of illustration but are not intended to be limiting. EXAMPLE 1 Growth of Endothelial and Epithelial Monolayers Bovine pulmonary microvessel endothelial cells (BPMVEC) and (BPAEC) bovine pulmonary artery endothelial cells were isolated and cultured according to described methods (Del Vecchio et al, In Vitro. Cell. Dev. Biol. 28A:711-715 (1992)). Endothelial cells were routinely cultured with DMEM containing 20% FBS. For isolating plasma membranes, the endothelial cells were cultured in 850 cm.sup.3 roller bottles. To each roller bottle, 75 ml culture medium was added. An air-CO.sub.2 mixture was introduced. The cells were then transferred to a roller bottle incubator at 37.degree. C., and were allowed to grow for 10-12 days. Primary rat alveolar epithelial cells (AEC) were isolated by methods described in Uhal et al, Am. J. Physiol. 257:C528-C536 (1989). Cells were cultured in DMEM containing 10% FBS for either 2 or 4 days, at which times they exhibited a type II or type I cell-like phenotype respectively. Phenotype was verified by methods described by Uhal et al, Am. J. Physiol. Suppl. 261:110-117 (1991). Endothelial Cell Membrane Isolation Endothelial cells grown in roller bottles were washed 2.times. with phosphate buffered saline. The cells were scraped from roller bottles and suspended in Buffer-A (20 mM HEPES/Tris, 0.15 M NaCl, 0.1 mM PMSF at pH 7.4) and washed 2.times. by centrifuging at 700.times.g for 10 minutes. The cells obtained from 6-8 roller bottles were suspended in 75 ml of buffer-A and homogenized using a Polytron homogenizer for 1 minute at full speed. The homogenate was centrifuged at 3000.times.g for 10 minutes. The supernatant was collected and centrifuged at 40,000.times.g for 60 PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. minutes. The pellet obtained was then suspended in buffer-A and recentrifuged at 40,000.times.g for 60 minutes. The final membrane pellet was suspended in a small volume of buffer-A containing 0.2 mM EDTA and the protein concentration was determined (Lowry et al, J. Biol. Chem. 193:265-275 (1951)). The plasma membrane marker enzyme activities were determined and the sample stored at 70.degree. C. until further use. Ligand Blotting Endothelial cell membranes were preincubated with 1 mM PMSF and 0.5 mM EDTA for 20 minutes at 22.degree. C., and then solubilized by mixing with 1.5 volume of solubilizing buffer (9M urea, 2% SDS, 2% .beta.-mercaptoethanol, 0.1 M Tris, 0.02% bromophenol blue pH 6.8). The mixture was incubated at 22.degree. C. for 30 minutes. The solubilized proteins were separated by SDS-PAGE (Laemmli, Nature (London) 227:680-685 (1970)) using a slab-gel electrophoretic system with 3% acrylamide in the stacking gel and 10% acrylamide in the separating gel. After electrophoresis, the proteins were transferred to either PVDF or nitrocellulose membrane. The transfer was carried out for 2 hours at 150 volts using 25 mM Tris, 192 mM glycine, and 20% methanol as transfer buffer. The non-specific binding was blocked by incubating the membrane with 5 mM CaCl.sub.2 in TBS (20 mM Tris, 0.5 M NaCl at pH 7.5) for 10 minutes and then with 0.5% Tween-20 in TBS overnight. After this step, the membrane was washed and cut into two strips. One strip was incubated with 0.6 mg/ml globulin-free BSA in TBS containing 1.5% gelatin for 2 hours and the other strip was incubated without BSA. The strips were washed and incubated with anti-bovine BSA for 60 minutes in TBS containing 1.5% gelatin. The membranes were then washed 2.times. and incubated with second antibody (goat anti-rabbit IgG) conjugated with alkaline phosphatase. The protein bands were localized after adding 5-bromo-4-chloro-3-indolylphosphate and nitroblue tetrazolium salt. Protein Purification BPMVEC membranes were used to isolate a 57 kDa albumin-binding protein. The ligand blotting was carried out to assess the presence of this protein in each step. BPMVEC membranes (100 mg) were preincubated with 1 mM PMSF and 0.5 mM EDTA for 30 minutes at 22.degree. C. The membranes were solubilized using a final concentration of 2.5% sodium cholate and 4 M urea, at 4.degree. C. for 3 hours, with gentle stirring. The protein concentration was adjusted to 4 mg/ml during solubilization. After this treatment, the suspension was centrifuged at 100,000.times.g for 60 minutes. The supernatant was collected and dialyzed against 5 mM HEPES/Tris (pH 7.2). More than 80% of membrane proteins were recovered in the supernatant. The dialysed suspension was concentrated by 60% ethanol precipitation at 4.degree. C. The ethanol precipitate was collected by centrifugation at 10,000.times.g for 30 minutes at 4.degree. C. and suspended in Buffer-A. This precipitate was solubilized with 2.5% Triton X-100 overnight at 4.degree. C. with gentle stirring. The suspension was centrifuged at 100,000.times.g for 60 minutes. The supernatant was collected and dialysed against 4 l of 50 mM Tris-HCl, 0.2 mM EDTA, 0.15% Triton X-100 and 0.1 mM PMSF, pH 8.0 (Buffer-B). The dialysed extract was applied on a DEAE-52 column (10.times.13 cm). The column was previously equilibrated with Buffer-B. The column was washed with 50 ml of Buffer-B after applying the sample. The bound proteins were eluted from the column with 80 ml of 0-500 mM linear NaCl gradient in Buffer-B at a flow rate of 15 ml/hr. The fractions from individual peaks were pooled separately and concentrated by 50% acetone precipitation. The acetone precipitate was used for ligand blotting. Only peak-I showed albumin-binding activity. The proteins present in peak-I were further separated by using preparative SDS-PAGE (16 cm.times.16 cm, 3 mm PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. thick slab-gel), and a 57 kDa protein eluted from the gel was used for further studies. Antibody Production and Purification The 57 kDa albumin-binding protein eluted from preparative SDS-PAGE was used to immunize rabbits. Approximately 50 .mu.g protein (per rabbit) was injected intramuscularly after mixing with equal volume of Freund's complete adjuvant. A second injection was given after two weeks. Rabbits were bled at 4 to 6 weeks after the second injection and the immune response was checked. The preimmune serum IgG and the antiserum IgG were purified using protein A-sepharose column. Immunoblotting Endothelial cell membranes were subjected to SDS-PAGE (Laemmli, supra) , and electrophoretically transferred to nitrocellulose or PVDF membrane. Non-specific binding was blocked with 3% gelatin in TBS for 5 hours at 22.degree. C. The membrane was washed 2.times. with 0.5% Tween-20 in TBS and incubated with antiserum diluted in TBS containing 1% gelatin. The incubation was carried out for 4-6 hours, washed 2.times., and then incubated for 60 minutes with the second antibody (goat anti-rabbit IgG coupled to alkaline phosphatase). After incubation, the membranes were washed 2.times. and the protein bands were localized as described under "Ligand Blotting". Molecular weights of the proteins were determined using known marker proteins. Monolayer Binding Studies BPMVEC were seeded (3.times.105 cells/well) in six well Corning tissue culture plates and grown to confluence. The monolayers were washed 2.times. with serum-free medium (20 mM HEPE/DMEM pH 7.4) and incubated with serum-free medium for 15-20 hours in a tissue culture incubator. After this incubation, the monolayers were washed 2.times. with binding buffer (20 mM HEPES/Tris HBSS pH 7.4) and the binding was initiated by adding 1 ml of 1 .mu.M .sup.125 I-BSA in binding buffer. The incubation was carried out at 4.degree. C. for 60 minutes. The binding was terminated by washing the monolayer 3.times. with the binding buffer. The radioactivity associated with the monolayer was determined after lysing the cells with 1 N NaOH (Tiruppathi et al, Am. J. Physiol. (Lung. Cell. Mol. Physiol.) L595-L601 (1992)). Non-specific binding was determined by the inclusion of unlabelled BSA (40 mg/ml) during the binding procedure. The test components, preimmune serum-IgG and the anti-57 kDa-IgG were preincubated for 30 minutes with the monolayer prior to the addition of .sup.125 I-BSA. Trans-cellular Flux Experiments Transendothelial .sup.125 I-albumin flux rates in cultured endothelial monoloyers were used to assess transendothelial albumin transport. The system used for this study has previously been described (Cooper et al, J. Appl. Physiol. 62:1076-1083 (1987); Garcia, et al, J. Cell. Physiol. 128:96-104 (1986); Del Vecchio, et al, Vitro. Cell. Dev. Biol. 28A:711-715 (1992) and SiflingerBirnboirn et al, J. Cell. Physiol. 132:111-117 (1987)). The system measures the transendothelial movement of tracer macromolecules in the absence of hydrostatic and oncotic pressure gradients. It consists of luminal and albuminal compartments separated compartments separated by a polycarbonate microporous filter (0.8 .mu.m pore diameter). BPMVEC were seeded at 105 cells/filter and grown for 3-4 days to attain confluency. Both compartments contained the same PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. medium (20 mM HEPES-DMEM, pH 7.4) at volumes of 600 ml and 25 ml, respectively. The luminal compartment was fitted with a Styrofoam outer ring, and "floated" in the abluminal medium so that fluid levels remained equal after repeated samplings from the abluminal compartment. The abluminal compartment was stirred continuously and the entire system was kept at 37.degree. C. by a thermostatically regulated water bath. Transendothelial clearance of .sup.125 I-albumin was determined as the volume of luminal chamber radioactivity cleared into the abluminal chamber. The change in volume over time provided the .sup.125 I-albumin clearance rate in .mu.l/min as determined by weighted least-squares non-linear regression analysis (BMDP Statistical Software, Berkeley, Calif.). At the beginning of the experiment, the luminal compartment was floated in the abluminal medium, and filled with medium containing about 6 .mu.Ci/ml .sup.125 I-albumin. Albuminal samples, 400 .mu.l, were collected at 10 minute intervals for up to 60 minutes and the radioactivity was measured using a gamma counter. At the end of the experiment, free .sup.125 I in the luminal and abluminal compartments was determined using 12% TCA precipitation and the transendothelial .sup.125 Ialbumin flux rates were corrected for free .sup.125 I. The day before the experiment, the BPMVEC monolayers were washed 2.times. with 20 mM HEPES-DMEM pH 7.4 (serum-free medium) and incubated at 37.degree. C. in cell culture incubator with serum-free medium for 12-15 hours. After this incubation period, the test components (preimmune serum-IgG and the anti-57 kDA-IgG) were diluted in serum-free medium and incubated with the monolayers for the desired periods. These monolayers were then used for transendothelial albumin transport measurement. Trans-epithelial flux rates were measured with slight modification to the method described for endothelial cells. Flux rates were determined on primary AEC or the A549 human lung carcinoma cell line cultured as described on Transwell filters (Costar) (Evans et al, Exper. Cell Res. 18:375-387 (1989)). Monolayer integrity is defined by transepithelial electrical resistance being greater than 500 ohms/cm.sub.2. Filters with intact monolayers were placed in a 24 well culture plate containing 1 ml serum-free DMEM per well (abluminal chamber). The luminal chamber was filled with 200 .mu.l serum-free DMEM containing the tracer molecule of interest (FITC-Insulin). The fluid levels in the two compartments were the same, eliminating hydrostatic pressure. The filter system was preincubated (30 mins) and then maintained at 37.degree. C. in a CO.sub.2 incubator throughout the flux experiment. At one and two hours, 300 .mu.l samples were withdrawn from the abluminal chamber and immediately replaced with serum-free DMEM. The fluorescence of the transcytosed material was recorded on a plate reader, and the ratio of bound vs. free FITC determined by gel filtration chromatography of the abluminal samples. Actin Filament Distribution The actin filament distribution and cytoskeletal changes in endothelial monolayers grown on the filters were studied under the conditions identical to those used for the measurement of .sup.125 Ialbumin clearance rates. After the required pretreatment period with the test components, the monolayers on the filter were fixed in 10% buffered formalin (Pallescences Inc., Warrington, Pa.), permeabilized with 1% Nonidet P40 (Sigma), and stained with rhodamine phalloidin (Molecular Probes, Inc., Eugene, Oreg.) as described by Phillips and Tsan, J. Histochem. Cytochem. 36:551-554 (1988). The intact filters containing the monolayers were removed from the wells and mounted on PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. coverslips, covered with a 1:1 solution of glycerine in phosphate-buffered saline, and then covered with a round coverslip and sealed. The slides were analyzed using a Nikon Lab Diaphot fluorescent microscope (NiKon Inc., Melville, N.Y.) and photographed using TRI X Pan 400 ASA Kodak film). Identification of Albumin-Binding Proteins Plasma membranes were first isolated from BPMVEC by differential centrifugation and the albumin-binding proteins present in this membrane fraction were identified using ligand blotting (see above). A simple method was developed, to identify native albumin-binding proteins in endothelial cell membranes. The membrane proteins were separated using SDS-PAGE and then transferred to PVDF or nitrocellulose. Non-specific binding was blocked by incubating the membrane strips with Tween-20, and then treated with globulin-free monomeric native BSA. The BSA-binding regions were identified using polyclonal antibody raised against native BSA. In the absence of exposure of the membrane strip to native BSA, the anti-BSA recognized only a 67 kDa polypeptide, indicating the presence of a significant amount of BSA bound to endothelial cell membranes. However, when the strip was treated with BSA, the anti-BSA antibody reacted with 3 additional polypeptides (110 kDa, 57 kDa and 18 kDa). Of these polypeptides, the antibody reacted most intensely with 57 kDa, indicating the 57 kDa polypeptide to be the major native albumin-binding protein. Total endothelial cell membrane fractions (100,000.times.g particulate fraction from BPMVEC and BPAEC) were also prepared and used for ligand blotting. These particulate fractions also showed a primary interaction of BSA with the 57 kDa polypeptide. Isolation of the 57 kDa Albumin-Binding Protein Since binding of native albumin was seen primarily with the 57 kDa protein, a method was developed for the isolation of this protein from BPMVEC membranes. Ligand blotting was employed to assess the presence of this protein during purification. BPMVEC membranes were initially solubilized with 2.5% sodium cholate and 4M urea, and the extract was dialyzed and concentrated by 60% ethanol precipitation. This precipitate was re-extracted with Triton x-100 (see above). The Triton x-100 solubilized extract was chromatographed on the DEAE column, and the bound proteins were eluted with linear gradient (0-500 mM NaCl). The proteins were eluted as 3 peaks. The fractions from each peak were pooled and screened for albumin-binding using the ligand blotting assay. Only one peak (I) showed albumin-binding with the 57 kDa protein region. SDS electrophoresis was conducted, using proteins from native BPMVEC membrane and DEAE column peak I after staining with Coomassie brilliant blue R-250. The presence of 57 kDa protein corresponding to albumin-binding was observed with ligand blotting in both native membranes as well as in DEAE peak I. SDS-PAGE was also performed under non-reducing conditions (in absence of .beta.ME), and the albumin-binding was observed only with 57 kDa region, suggesting the absence of sulfide link in this protein. This protein was further purified using preparative SDSPAGE, and the protein eluted from gel was used for the antibody preparation. Immunoblotting BPMVEC and BPAEC membrane proteins were separated by using SDS-PAGE and transferred to nitrocellulose strips. The strips were immunoblotted with the 57 kDa antiserum. The preimmune serum did not recognize any proteins from BPMVEC and BPAEC membranes. The antiserum PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. recognized two major proteins (57 kDa and 36 kDa) and one minor protein (43 kDa) in both membrane preparations. The particulate fractions from BPMVEC and BPAEC were also used for immunoblotting. The antibody recognized only these three proteins in the particulate fractions. This suggests that the albumin-binding protein was purified to an apparent homogeneity. To study the proposed structural relationship between the endothelial membrane-associated and secreted (SPARC) albumin-binding proteins, immunoblotting of BPMVEC membranes was carried out with the antibodies raised against purified bovine SPARC. The antiserum raised against purified bovine SPARC recognized 67 kDa, 61 kDa, 57 kDa, 43 kDa and 36 kDa polypeptides in BPMVEC membranes. The anti-SPARC-NH2 terminal peptide antiserum reacted strongly with a 36 kDa polypeptide and weakly with a 43 kDa polypeptide. This suggests that scavenger receptors are quite different from native albumin receptors. Effect of Anti-57 kDa-IgG on Binding of .sup.125 I-BSA to BPMVEC Monolayers Preimmune serum-IgG and the anti-57 kDa-IgG were affinity-purified using Protein-A Sepharose column. The influence of IgG fractions on binding of .sup.125 I-BSA to BPMVEC monolayers at 4.degree. C. was investigated: non-specific binding ranged from 40-50%. The preimmune serumIgG did not significantly affect the specific binding of .sup.125 I-BSA to the BPMVEC monolayers. In contrast, the anti-57 kDa-IgG reduced the specific binding of .sup.125 I-BSA to BPMVEC monolayers in a dose-dependent manner. The reduction was maximum (40-50%) at 200 .mu.g/ml concentration in anti-57 kDa-IgG, and remained unchanged up to 1000 .mu.g/ml. These results demonstrate that the antibody developed against the 57 kDa protein does not fully recognize the albumin-binding domain in the receptor, or that the native albumin may interact with other binding sites on endothelial cell surface. Activation of Transendothelial Albumin Flux by Anti-57 kDa-IRG in the Absence of Endothelial Cell Shape Change To study the effects of the anti-57 kDa-IgG on transendothelial transport of albumin, the transendothelial .sup.125 I-BSA clearance rates in BPMVEC monolayers was measured. The monolayers were preincubated with preimmune serum-IgG and anti-57 kDa-IgG for 15 minutes, 30 minutes and 60 minutes, and then the transendothelial .sup.125 I-BSA clearance rates were measured up to 60 minutes. The anti-57 kDa-IgG-induced increase in permeability was time-dependent. A 30minute period of preincubation of anti-57 kDa-IgG resulted in a 2-fold increase in .sup.125 I-BSA clearance rate over preimmune IgG. No significant increase in permeability was seen with 15 min. preincubation, and a 40-50% change was noticed when anti-57 kDa-IgG was pre-incubated with the monolayer up to 60 min. The preimmune serum-IgG had no influence on transendothelial albumin transport at all preincubation periods tested. The anti-57 kDa-IgG effect on the permeability of .sup.125 I-albumin reverted at 4.degree. C. The shape change of endothelial cells after treating with preimmune serum-IgG and anti-57 kDa-IgG was studied, using a technique described previously (Phillips and Tsan, supra; Siflinger-Birnboim et al, Lab Invest. 67:24-30 (1992)). BPMVEC grown on nucleopore filters were preincubated with preimmune serum-IgG and anti-57 kDa IgG for 30 min., and the monolayers were stained with rhodamine phalloidin (see above). No cell "rounding" or formation of interendothelial gaps was PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. observed in either case. These results suggest that anti-57kD albumin-binding protein antibody activates albumin transport. There is another possibility, i.e. that this antibody may non-specifically increase the pericellular transport of albumin, by widening the interendothelial junctional gaps. To delineate this, the effect of anti-receptor IgG and preimmune serum IgG on endothelial cell morphology was studied. Pretreatment of BPMVEC monolayers with either preimmune serum-IgG or anti-receptor-IgG had no influence on interendothelial junctional gaps. This antibody to the 57 kDa albumin-binding protein may activate the transcytosis of albumin. The permeability increasing effect of this antibody did not occur at 4.degree. C., supporting the conclusion that the antibody activated albumin transcytosis via formation of vesicles, which have been shown to be temperature-sensitive (Lo et al, J. Cell. Physiol. 151:63-70 (1992)). EXAMPLE 2 Antibodies Raised Against GP60 Antibody raised against GP60 from endothelial cells was used to probe epithelial membrane extracts as described in Example 1. The anti-GP60 antibodies recognized a 60 kDa protein found in the epithelial extracts. This clearly shows that an immunologically-related protein is present in this system. Epithelial and endothelial cells were grown as monolayers, as described in Example 1, to produce confluent monolayers showing the appropriate reactivity to solute flux. Anti-GP60 antibody (200500 .mu.g/ml) was incubated with the monolayers at 4.degree. C. to bind antibody to the receptor, in the absence of metabolic activity that might result in internalization of the GP60. Binding of antiGP60 antibody under these conditions resulted in a 80-90% decrease in .sup.125 I-BSA binding by the endothelial monolayers. The epithelial monolayers were further incubated with a second antibody to the primary rabbit anti-GP60 antibody, to cross-link the receptors. Both monolayers were washed and then incubated with .sup.125 I-BSA for the epithelial cells or .sup.125 I anti-BSA immunoglobulin for the endothelial monolayers at 37.degree. C., to allow internalization of the receptor-antibody complex and co-transcytosis of the .sup.125 I-labelled tracer. Incubation with antiGP60 antibody resulted in a 1.6-2 fold increase in uptake over the level of a pre-immune serum control. Thus, binding the GP60 receptor by an anti-GP60 antibody results in activation of the transcytosis mechanism, thereby enhancing uptake of a macromolecule in the vicinity of the invaginating membrane. EXAMPLE 3 Use of Albumin with Macromolecules Endothelial monolayers were incubated at 4.degree. C. in the presence of BSA, to initiate the binding of BSA to GP60 but to prevent the internalization of the ligand receptor complex. After extensive washing to remove unbound BSA, the cells were incubated with .sup.125 I-labelled antiBSA immunoglobulin at 37.degree. C., as the macromolecular tracer. Pre-treatment with BSA enhanced transcytosis of the immunoglobulin tracer by 1.5 fold over the control cells pre-incubated with unlabelled anti-BSA immunoglobulin. Further, when the cells incubated at 37.degree. C. were PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. washed and immediately taken through the same protocol, no macromolecular flux was observed; this shows that, once internalized, the GP60 receptor is unavailable for ligand binding. Thus, large (150 kDa) molecules can be co-transcytosed in concert with HSA using the GP60 system. EXAMPLE 4 Use of Albumin with Peptides Human and rat epithelial monolayers were grown to confluence, as described in Example 1. The cells were then incubated with FITC-insulin (1 mg/ml) or FITC-insulin and BSA (each 1 mg/ml) at 37.degree. C. in the transcellular flux system described above. For human and rat epithelial monolayers, there was a 2.5 or 4 fold increase in FITC-insulin flux over the control of FITC-insulin alone. Thus, albumin also stimulates co-transcytosis of small molecular weight peptides across epithelial cells containing the GP60 receptor. EXAMPLE 5 Use of N-Terminal Peptide 1-18 of GP60 A synthetic N-terminal peptide (T3118) of GP60 corresponding to the first 18 residues was produced by solid-phase peptide synthesis. The sequence (SEQ ID No. 1) shows at least 80% homology with the bovine, membrane-bound thyroid hormone (T3)-binding protein (Yamauchi et al, Biochem. Biophys. Res. Comm. 146:1485 (1987)). It has 97% homology with PDI. Antibodies were raised in rabbits against T3118, and used to probe endothelial membrane extracts, to determine cross-reactivity with proteins recognized by anti-GP60 antibodies as described below. BPMVEC membrane proteins (100 .mu.g) were separated on SDS-PAGE and transferred to nitroulose membrane strips. Non-specific binding was blocked with 5% non-fat dry milk in Trisbuffered saline. The antisera were diluted in blocking solution, incubated for 4-5 hrs at 4.degree. C., washed and treated with goat-anti-rabbit-IgG conjugated with alkaline phosphatase. The protein bands were identified using known molecular weight marker proteins. The anti-T3118 antibodies showed only reactivity towards the GP60 protein and not towards the SPARC peptides recognized by the anti-GP60 antibody. The T3118 peptide was then used in an endothelial uptake experiment to determine if it would act as an antagonist of albumin recognition and uptake. Endothelial monolayers were incubated at 4.degree. C. in the presence of .sup.125 I-BSA or .sup.125 I-BSA plus the T3118 peptide. After incubation, the cells were washed extensively, lysed and counted for tracer uptake. Surprisingly, rather than acting as an antagonist, the T3118 peptide actually stimulated uptake of albumin 5-fold over the albumin alone control. The enhancement was saturable at a concentration of 500 .mu.m of T3118 peptide. These data suggest that the T3118 peptide, acting as an agonist, may induce a conformational change in albumin, which enhances recognition by GP60, or is the signal for uptake by the endothelial cells. It will be appreciated by those skilled in the art that the invention can be performed within a wide range of equivalent parameters of composition, concentrations, modes of administration, and conditions without departing from the spirit or scope of the invention or any embodiment thereof. PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Principal Investigator/Program Director (Last, first, middle): ***** PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Malik, Asrar B. Principal Investigator/Program Director (Last, first, middle): Malik, Asrar B. Reporting Structure Attachment #7 Dean COM Standing Committee Associate Director Center Director Center Faculty Trainees PHS 398 (Rev. 5/95) Page Number pages consecutively at the bottom throughout the application. Do not use suffixes as 3a, 3b. Internal and External Advisory Committee Department Heads