DNA sequencing advances usher in the era of personalized
advertisement

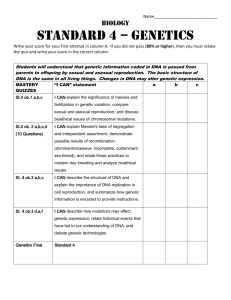
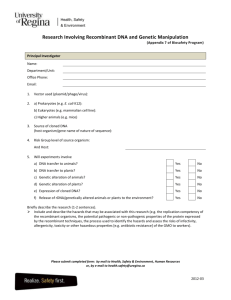
DNA sequencing advances usher in the era of personalized medicine by Dr. David L. (“Woody”) Woodland (as published in the Summit Daily News of September 2, 2013) It’s been 60 years since James Watson and Frances Crick determined the structure of DNA. The now-famous structure revealed that the DNA molecule is comprised of two intertwined strings of paired bases that form a double helix. Each string is composed of four different bases – Adenosine, Guanine, Thymidine, and Cytosine (A, G, T, and C) arranged to form a code that an individual cell can interpret and translate into the proteins that form the cell’s structure and regulate its metabolism. The DNA sequence and its relationship to the proteins it encodes represent the foundation of modern genomics. In years past, researchers sequenced short stretches of DNA by running gels that enabled them to determine the order of bases along the DNA strings. Although timeconsuming, the process allowed researchers to understand the structure of genes and identify the parts of the sequence that coded for the protein and the parts that regulated whether the protein was produced or not (i.e., regulatory sequences). This explained conundrums, such as why skin cells express lots of the skin protein keratin whereas neuronal cells generally do not. It also provided a genetic basis for our understanding of many diseases such as cancer. Deleterious changes (mutations) in the sequence of a gene can alter the pattern of protein expression or result in damaged proteins which either lack function or have altered function. Importantly, damaged or over-expressed proteins have been linked to specific disorders. For example, a mutation in the p53 gene which regulates cell division results in uncontrolled cell growth and is key in the development of some cancers. The first automated DNA sequencers appeared in 1987 and were expensive to operate. However, sequencing cost has fallen dramatically. When the challenge to sequence the first human genome was announced in 1988, it took approximately 15 years and $2.7 billion in 1991 dollars to produce and annotate the first complete sequence. Today, the cost of sequencing all three billion bases of DNA in the human genome has plunged to less than $4,000 (an approximately one million-fold decline). Scientists anticipate being able to sequence an entire human genome for less than $100 within a few years. Your future visits to the doctor’s office may involve taking a genome sequence along with your blood pressure. Our ability to sequence DNA rapidly and cheaply is spawning the era of “personalized medicine” in which disease treatments are tailored to the individual’s genetic makeup. One benefit is that more medicines may become available. Currently, new medicines are tested on large populations of individuals and are discarded if they show benefit for only a fraction of the population or produce side effects in a few individuals. Much of this variability is due to individuals’ genetic makeup; we may be throwing out many medicines very effective for a subset of patients. Genetic testing means we can identify patients who would respond to a specific medicine, thereby utilizing medicines that would not otherwise have made it to market. Indeed, in the not-to-distant future, your doctor prescribes a medicine selected to be the most effective and with fewest side effects for your genetic makeup. Examples of personalized medicines are already present in the clinic, especially in the cancer field. Cancer is really a variety of diseases, many linked to a number of distinct genetic defects. Even within a class of cancers, such as breast cancer, there are different forms of the disease. Genetic testing allows physicians to identify the specific defect involved and select the most appropriate drug. For example, about one-third of breast cancer patients over-express a protein called HER2 and respond poorly to standard therapies. These patients can be identified and treated with a drug that selectively targets HER2-positive tumors. Another important aspect of personalized medicine is prevention. Knowledge of specific disease risks will allow us to focus on prevention or earlier intervention. We already do this to some extent – for example, by acting on our predicted risk for cardiovascular disease based on family history and clinical measurements of blood chemistry and pressure. But, in future, preventative medicines may become much more refined and based on genetic sequence analysis. These advances do not come without challenges. Genetic information could potentially impact medical insurance, and there are individuals who might not wish to know their high risk of developing certain diseases, especially diseases with no cures. However, the overall impact of personalized medicine is likely to be positive. Our access to the sequence of individual genomes will allow physicians to better diagnose diseases and implement more effective treatments, potentially reducing healthcare costs in the future. David L. “Woody” Woodland, Ph.D. is the Chief Scientific Officer of Silverthorne-based Keystone Symposia on Molecular and Cellular Biology, a nonprofit dedicated to accelerating life science discovery by convening internationally renowned research conferences in Summit County and worldwide. Woody can be reached at 970-262-1230 ext. 131 or woody@keystonesymposia.org. To view more (Petri) Dish articles, please visit “News” on the Keystone Symposia website.