PEDIATRIC PROTOCOLS
advertisement

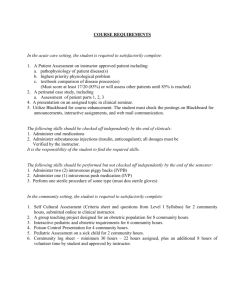
PEDIATRIC PROTOCOLS THE PEDIATRIC PATIENT Definitions: Newborn - birth to 30 days Infant - 30 days to one year Child - One year to 12 years or up to 75 pounds or 34 kilograms Focused history - The history and physical exam for pediatric patients differs in some areas from the adult. Areas that might get more emphasis are: PMH - allergies, medications, prematurity, prenatal care, birth weight Neuro - feeding well, level of activity, alertness Cardiac - palpations, chest pain Respiratory - retractive breathing, appearance of shortness of breath, previously on a ventilator, wheezing, barking noises GI - vomiting, diarrhea GU - urine volume, (wetting diapers); urine color, smell; crying on urination Skin - color, turgor, rash Extremities - movement, reflexes General - eye movement, strength, moist mucosa .INFUSIONS Epinephrine Infusion Dopamine Infusion 0.6 X body weight (kg) equals milligrams added To diluent to make 100 ml 0.6 X body weight (kg) equals milligrams added to diluent To make 100 ml Total 1 ml/h delivers 0.1 ug/kg per minute; titrate to effect 1 ml/h delivers 1.0 ug/kg per minute; titrate to effect CHART Age Newborn 1-6 6 Months 1 Year 3 Years 6 Years 10 Years Weight lbs kgs 7 3.5 7 3.5 15 7 22 10 33 15 40 18 60 28 Systolic BP Pulse Respiration 50-70 70-95 80-100 80-100 80-110 80-110 90-120 100-160 100-160 90-120 90-120 80-120 70-110 60-90 30-60 30-60 25-40 20-30 20-30 18-25 15-20 Pediatric hypotension is defined as: newborn to 30 days - systolic BP < or = 60; 1 month to 1 year - SBP < or = 70; over 1 year < or = 70 + ( 2 + age in years) Since it is difficult to measure blood pressures on children less than 1 year, other signs of shock should be assessed. These include delayed capillary refill; rapid heart rate; pale, cool, clammy skin; weak or absent peripheral pulses; altered level of consciousness. PEDIATRIC BRADYCARDIA Criteria For Use Pediatric patient with symptomatic bradycardia, i.e. hypotension, poor perfusion, respiratory difficulty and/or diminished level of consciousness. Pediatric bradycardia would be a heart rate of: <100 Newborn; <80 Infant; <60 Child; due to Sinus bradycardia, 1st. 0 , 2nd 0 or 3rd 0 heart block or ventricular escape beats. Pediatric hypotension is defined as: Newborn to 30 days systolic blood pressure < or =60; 1 month to 1 year systolic blood pressure <or =70; over 1 year systolic blood pressure of < or =70 +(2+age in years) ALS Provider Guidelines: 1. Perform initial survey - resuscitate as needed 2. Secure Airway; administer appropriate oxygen 3. Perform chest compressions if bradycardia continues despite oxygenation and ventilation. A. Heart rate < 60/minute for newborn, infant or child with associated poor systemic perfusion. B. Infant with heart rate 60-80 per minute that does not increase despite effective positive pressure ventilation with 100 % oxygen over 30 seconds. 4. Initiate cardiac monitoring 5. Initiate an appropriate IV 6. Utilize length based tape, Broselow tape, or other similar devices to calculate medication dosages or for estimated weight or use the current known accurate weight of the patient. 7. Administer epinephrine 0.01 mg/kg,(1:10,000, 0.1mL/kg) IV or IO. If administered via ET, 0.1mg/kg (1:1000, 0.1 mL/mg). Repeat q 3-5 minutes. ------Contact Medical Command-----Command Physician’s Actions Might Include: 1. Order IO access 2. Second and subsequent doses epinephrine IV or IO,0.01mg/kg, (1:10,000, 0.1mL/kg) or ET, 0.1 mg/kg (1:1,000,0.1mL/kg). Repeat q 3-5 minutes. 3. Order atropine 0.02 mg/kg minimum dose: 0.1 mg maximum single dose: 0.5 for child; 1 mg adolescent May be repeated x 1 4. Consider external pacing 5. Order Epinephrine infusion or Dopamine infusion to maintain blood pressure See chart. Expeditious transport after initial resuscitation efforts is recommended. PEDIATRIC PULSELESS ELECTRICAL ACTIVITY Criteria For Use Management of a pulseless pediatric patient with presence of some type of electrical activity on the monitor, including EMD, idioventricular rhythm, ventricular escape rhythms, bradysystolic rhythms, and tachycardic narrow complex rhythms. This does not include ventricular tachycardia without a pulse. Refer to protocol for pulseless ventricular tachycardia where appropriate. ALS Provider Guidelines: 1. Perform initial survey - resuscitate as needed 2. Secure airway; intubate 3. Hyperventilate with 100% oxygen 4. Confirm cardiac rhythm in more than 1 lead 5. Initiate appropriate IV; (limit: 2 attempts or 60 seconds. If unsuccessful, administer first dose of Epinephrine via endotracheal tube 6. If unable to intubate or initiate and IV, and the patient is four years old or less, initiate an intraosseous line, while enroute to the hospital. Use one leg only for attempt. 7. Utilize length-based, Broselow tape, or other similar devices to calculate medication dosages or to estimate weight or use current known accurate weight of pediatric patient. 8. Administer epinephrine, first dose IV or IO: 0.01 mg/kg (0.1 ml/kg 1:10,000) ET: 0.1 mg/kg (0.1 ml/kg 1:1000) 9. Prepare for transport ------Contact Medical Command-----Command Physician’s Actions Might Include: 1. Order Intraosseous (IO) access 2. Order fluid challenge of 20 cc/kg Newborn to 30 days - 10cc/kg 3. Consider earlier treatment for other causes; i.e. hypovolemia, cardiac tamponade, tension pneumothorax, hypoxia, acidosis, pulmonary embolus, profound hypothermia, poisoning by drug overdose 4. Second and subsequent doses of epinephrine IV, IO ET, 0.1 mg/kg,1:1,000, (0.1ml/kg). Repeat q 3-5 minutes maximum of 1mg. 5. Order atropine 0.02 mg/kg minimum dose: 0.1 mg maximum single dose: 0.5 for child; 1 mg adolescent May be repeated x 1 Expeditious transport after initial resuscitation efforts is recommended PEDIATRIC ASYSTOLE Criteria For Use Management of pulseless pediatric patient with straight line EKG confirmed in 2 leads ALS Provider Guidelines: 1. Perform initial survey - resuscitate as needed 2. Secure airway and hyperventilate 3. Initiate cardiac monitoring 4. Initiate appropriate IV; (limit: 2 attempts or 60 seconds. If unsuccessful, administer first dose of Epinephrine via endotracheal tube. 5. If unable to intubate or initiate IV, initiate an IO line if the patient is four years old or less, enroute to the hospital. Use one leg only for attempt. 6. Use length-based, Broselow tape or other similar devices to calculate medication dosages or for estimated weight or use current known accurate weight of the patient 7. Administer epinephrine, first dose IV: 0.01 mg/kg,1:10,000, (0.1 ml/kg ET: 0.1 mg/kg,1:1000, (0.1 ml/kg) 8. Prepare for transport ------Contact Medical Command-----Command Physician’s Actions Might Include: 1. Order IO access 2. Order transcutaneous pacing 3. Order second and subsequent doses of IV, IO or ET epinephrine, 0.1 mg/kg (1:1000) 0.1 ml/kg, maximum of 1 mg 4. Order continuation of resuscitation efforts according to current pediatric guidelines 5. Order termination of resuscitative efforts Expeditious transport after initial resuscitative efforts is recommended. PEDIATRIC RAPID PULSE NARROW COMPLEX TACHYARRHYTHMIAS (Sinus Tachycardia) Criteria For Use Pediatric patient with EKG documented evidence of narrow complex ST and is symptomatic. Heart rate of 160-220 bpm is probable ST; heart rate of > or = 220 bpm is probable SVT. Pediatric tachycardia would be a heart rate of: newborn > or = 240; infant $ 220; child > or =180. See related tachycardia protocol. ALS Provider Guidelines: 1. Perform initial survey - resuscitate as needed 2. Secure airway and administer appropriate oxygen 3. Initiate cardiac monitoring 4. Obtain vital signs and focused patient history. Pediatric hypotension is defined as: newborn to 30 days systolic BP < or = 60; 1 month - 1 year SBP < or = 70; over 1 year SBP < or =70 + (2 + age in years) . Pediatric symptomatic tachycardia, i.e. hypotension, poor perfusion, respiratory difficulty, and/or diminished level of consciousness. 5. Determine if pediatric patient is stable or unstable. Go to appropriate protocol ------Contact Medical Command-----Command Physician’s Actions Might Include: 1. Order fluid challenge 2. Appropriate drug therapy PEDIATRIC FAST PULSE UNSTABLE SUPRAVENTRICULAR TACHYCARDIA Narrow or Wide with Evidence of Cardiovascular Compromise SVT, VT, SVT with Aberrancy, Criteria For Use Pediatric patient with EKG documented evidence of narrow or wide complex tachycardia with evidence of cardiovascular compromise: pediatric patient with tachycardia with symptoms of hypotension (diaphoresis, pallor, cool mottled extremities), poor perfusion, respiratory difficulty and/or diminished level of consciousness. Heart rate of > or = 220 bpm with symptoms for narrow complex Heart rate of > or = 120bpm with symptoms for wide complex Pediatric hypotension is defined as: newborn to 30 days - systolic BP < or = 60; 1 month to 1 year - SBP < or = 70; over 1 year < or = 70 + ( 2 + age in years) ALS Provider Guidelines: 1 Perform initial survey - resuscitate as needed 2. Secure airway; administer appropriate oxygen 3. Initiate cardiac monitoring 4. Assess vital signs; obtain focused patient history 5. Initiate appropriate IV; (limit: 2 attempts or 60 seconds.) 6. Utilize length based tape, Broselow tape, or other similar devices to calculate medication dosages or for estimated weight or use the current known accurate weight of the patient. 7. If stable, perform vagal maneuver: Infant or cooperative child - stimulation of the diving reflex Apply ice or extra cold wash cloth quickly and firmly to the patient’s nose and mouth for five (5) seconds. ------Contact Medical Command------ Command Physician’s Actions Might Include: 1. Order Adenosine 0.1-0.2 mg/kg, maximum of 12 mg followed by 5-10 cc of fluid flush 2. Order synchronized cardioversion, 1 - 2 joules/kg. Second and subsequent cardioversion is doubled from initial cardioversion to a maximum of 4 j/kg. PEDIATRIC CARDIAC ARREST PULSELESS VENTRICULAR TACHYCARDIA VENTRICULAR FIBRILLATION Criteria For Use Management of a pulseless pediatric patient with cardiac monitor showing ventricular fibrillation or ventricular tachycardia. ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed. 2. Administer appropriate oxygen. Begin CPR and ventilate until defibrillator is charged. 3. Initiate cardiac monitoring. 4. Utilize length based tape, Broselow tape, or other similar devices to calculate medication dosages or to estimate weight or use current known accurate weight off patient. 5. If ventricular tachycardia or ventricular fibrillation are noted on monitor, Immediately defibrillate at 2 j/kg or 1 j/lb. 6. If no conversion, defibrillate at 4 j/kg or 2 j/lb. 7. If no conversion, defibrillate at 4 j/kg or 2 j/lb. 8. Intubate, if not already done. If not able to intubate, use BVM. 9. Initiate appropriate IV; (limit: 2 attempts or 60 seconds. If unsuccessful, administer first dose of Epinephrine via endotracheal tube and contact medical command. 10. If unable to intubate or initiate an IV, initiate an IO, if the patient is four years old or less, while enroute. Use one leg only for attempts 11. If vascular access is obtained, administer Epinephrine 0.01 mg/kg 1:10,000, (0.1 ml/kg). If administered via ET, 0.1 mg/kg 1:1000, (0.1 ml/kg). -----Contact Medical Command----Command Physician’s Actions Might Include: 1. Order intraosseous access 2. Defibrillate at 4 j/kg within 30-60 seconds if rhythm unchanged after each administration of medication. 3. Administer Lidocaine 1 mg/kg IV or IO, (maximum total dose 3 mg/kg) 4. Administer Epinephrine, second and subsequent doses IV, IO, ET at 0.1 mg/kg 1:1000, (0.1 ml/kg). Repeat every 3-5 minutes. 5. Administer Bretylium 5 mg/kg first dose. Expeditious transport after intubation and initiation of resuscitative efforts is recommended. STABLE SUPRAVENTRICULAR TACHYCARDIA IN THE PEDIATRIC PATIENT Criteria for use Management of the pediatric patient with ECG documentation of narrow or wide complex tachycardia who is stable. ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed 2. Administer appropriate oxygen. 3. Initiate cardiac monitoring. 4. Perform vagal maneuvers: Infant or co-operative child - stimulate the diving reflex by applying ice or extra cold wash cloth quickly and firmly to the patient’s nose and mouth for five (5) seconds. 5. Initiate appropriate IV. If unable to establish vascular access after 2 attempts or 60 seconds, contact medical command immediately. -----Contact Medical Command----Command Physician’s Actions Might Include: 1. Transport with close observation 2. Order additional IV attempts or intraosseous access. 3. Synchronized cardioversion at 1 j/kg may be ordered. 4. If no conversion, repeat synchronized cardioversion at 1 j/kg. 5. If vascular access is established, administer Adenosine 0.1-0.2 mg/kg rapid IV push, IO up to 6 mg. 6. Order repeat Adenosine at 0.2-0.4 mg/kg rapid IV push, IO up to 12 mg. (Maximum dose 12 mg.) 7. Order Lidocaine 1 mg/kg (Maximum total dose 3 mg/kg) Expeditious transport after initiation of resuscitation efforts is recommended. DYSPNEA/ASTHMA IN THE PEDIATRIC PATIENT Criteria For Use Management of the dyspneic pediatric patient with a suspected cause of bronchospasm. (Presence of wheezes or diminished lung sounds.) ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed. 2. Administer oxygen appropriate for the condition and history. 3. Initiate cardiac monitoring. 4. Utilize length based tape or Broselow tape for estimated weight or use the current known accurate weight of the patient. 5. Administer Albuterol (Proventil) 2.5 mg/3 cc saline aerosol inhalation, over 15 minutes for child over 12 months of age. Under 12 months, administer Albuterol (Proventil) 1.25 mg/3cc saline aerosol inhalation over 15 minutes. -----Contact Medical Command----Command Physician’s Actions Might Include: 1. Order initiation of appropriate IV if patient is not improving with Albuterol aerosol inhalation 2. Order repeat Albuterol 20 minutes after first dose, 2.5 mg/3cc saline aerosol inhalation. 3. Order Epinephrine 1:1000 0.01 mg/kg to be given subcutaneously, for severe respiratory distress to maximum dose of 0.3 mg (0.3 ml) Note: Severe respiratory distress in children is characterized by marked increase in respiratory effort; i.e. severe agitation, dyspnea, tripod position, intercostal and parasternal retractions, poor feeding in an infant, skin pallor, weakness, tachycardia. PEDIATRIC PATIENT WITH ALTERED MENTAL STATUS Criteria For Use Pediatric patients who are in a coma with evolving neurological deficit, or altered mental status of unknown etiology. Patients who are known diabetics who have an altered level of consciousness not thought to be secondary to trauma. Maintenance of normal respiratory and circulatory function is always the first priority. Pediatric patients with altered mental status and/or respiratory failure or arrest, shock, trauma, near drowning or other anoxic injury should be treated under other protocols. ALS Provider Guidelines: 1. Perform initial survey-resuscitate as needed 2. Administer appropriate oxygen 3. Initiate cardiac monitoring 4. Start an appropriate IV 5. Draw blood for sugar 6. Do a chemstrip 7. Utilize length based tape, Broselow tape, or other similar devices to calculate medication dosages or for estimated weight or use the current known accurate weight of the patient. 8. If the chem strip reading is 40 or below, administer D25, 0.5 g/kg; for newborns, D12.5, 0.5g/kg 9. If the patient is12 years old or over, and the chemstrip reading is less than 60, and no I.V. can be established, administer 1 mg Glucagon, IM. If the patient is less than 12 years old, call medical command. ------Contact Medical Command------ Command Physician's Actions Might Include: 1. Order IO line, to be performed during transport 2. Order additional 0.5 mg/kg IV or IO D25, D12.5 in newborns.) 3. If no IV access available, order Glucagon, 0.5 mg in 0.5 ml diluent, IM, for pediatric patients weighing less than 20 kg.(20-30 Fg/kg 4. Order Narcan 1 mg IV/IO in patients greater than two years old. 0.4 mg for patients less than 2 years old. If no IV or IO access can be established, may order 2mg Narcan IM for patients > 2 years old, 1 mg for patients < 2 years old. 5. Order transport Note: To make D12.5, take an amp of D25, spill ½ the volume and refill to original volume with sterile normal saline solution. PEDIATRIC ANAPHYLAXIS Criteria for use : Management of pediatric patients who are acutely symptomatic secondary to suspected exposure to an allergen and have impending true anaphylaxis. Acutely symptomatic is defined as : Systemic reaction: sudden onset of urticaria and/or any of the following signs - airway problems, wheezing, throat tightness, sudden difficulty swallowing. hypotension, associated altered level of consciousness. Urticaria by itself is not anaphylaxis but still should be closely monitored. However, urticaria may not always be present in anaphylaxis.. ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed. 2. Administer oxygen 3. Initiate cardiac monitoring. 4. Utilize length-based tape, Broselow tape, or other similar devices to calculate medication dosages or for estimated wt., or use the current known wt. of the pediatric pt. If acutely symptomatic, (a) if wheezing is present, immediately administer albuterol 2.5mg/3cc saline by aerosol inhalation. (b) if signs of shock or severe respiratory distress are present, initiate an appropriate I.V. and give Epinephrine 1:10,000, 0.01 mg/kg (0.1 cc/kg), up to 0.3 mg (3 ml) and give a 20 ml/kg bolus of NSS or lactated ringers. If no I.V. access is available, give epinephrine 1:1,000, 0.01 mg/kg (0.01 ml/kg) SQ up to 0.3 mg. (c) administer diphenhydramine 1 mg/kg, I.V. maximum of 50 mg. Give IM if no I.V. access is available. (d) maintain close monitoring even if symptoms resolve, as they may recur when Epi is metabolized. -----Contact Medical Command----Command Physician’s Actions Might Include: 1. In patients with less severe reactions, order initial IV of NSS via a large bore IV (18-22 gauge), or IO. 2. Order additional boluses of NSS as necessary. 3. Administer epinephrine 0.01 mg/kg (0.1cc/kg of a 1:10,000 solution) slowIV/IO bolus, or SQ. 4. Repeat IV/IO/SQ epinephrine as necessary using the same dose. 5. Administer additional Albuterol 2.5 mg. in 3 cc by aerosol inhalation. 6. Administer additional diphenhydramine1mg/kg, I.M. or I.V. NOTE: Examples Epi 1:1,000: 20 kg dose = 20(0.01cc) =0.2cc =0.2mg subcutaneously Epi 1:10,000: 20 kg dose = 20(0.1cc) = 2cc = 0.2mg intraveneously SEIZURES IN THE PEDIATRIC PATIENT Criteria For Use Pediatric patient with a history of seizures or who is in a seizure state. ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed. 2. Administer appropriate oxygen. 3. Initiate cardiac monitoring. 4. Initiate appropriate IV. 5. Utilize length based tape, Broselow tape, or other similar devices to calculate medication dosages or for estimated weight or use the current known accurate weight of the patient. 6. Check Chemstrip reading. If the patient is not a known seizure patient or if the patient is diabetic and the Chemstrip reading is <40, give Dextrose 25%, 0.5 - 1 g/kg IV bolus. For newborns use D12.5. -----Contact Medical Command----Command Physician’s Actions Might Include: 1. If the patient is known to have a seizure history and has had more than one generalized seizure and is in a seizure state upon the arrival of ALS or has been in a seizure for longer than 5 minutes, orders may be given for the administration of Valium, 0.1-0.3 mg/kg. If no IV access has been established, orders for rectal Valium @ 0.5 mg/kg may be given via lubricated 3 cc syringe. Be prepared to manage the airway 2. Order intraosseous access. 3. Order additional 25% or 12.5% Dextrose IV. Note: Bodily injury protection and airway maintenance with a nasopharyngeal airway and oxygen administration is usually sufficient initial treatment for most seizure. Seizures are usually self limiting. Call MedCom if unsure of aggressiveness of treatments needed. SHOCK - TRAUMATIC or HYPOVOLEMIC IN THE PEDIATRIC PATIENT Criteria For Use Management of the pediatric patient involved in a traumatic episode with hypovolemia. (Pediatric hypovolemia is defined as: Newborn to 30 days systolic BP < or = 60; 1 month to 1 year systolic BP < or = 70; over 1 year systolic BP of < or = 70 + 2 + age in years caused by suspected or evident blood loss resulting in adequate perfusion.) Because of the difficulty in measuring BP in children less than 1 year, other signs of shock should be assessed. ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed with spinal immobilization in place. 2. Administer appropriate oxygen, via BVM or E.T. if needed. 3. Make decision concerning hospital destination and method of transport as possible. 4. Utilize length base tape, Broselow tape or other similar devices to calculate medication dosages or to estimate weight or use current known accurate weight of patient 5. Initiate cardiac monitoring. 6. Without delaying transport, establish one I.V. Initiate fluid challenge at 20 cc/kg, 10 cc/kg for newborn. If unable to establish vascular access after 2 attempts, contact medical command immediately in anticipation of an order for intraosseous access. -----Contact Medical Command----Command Physician’s Action Might Include: 1. Alter patient destination or method of transfer. 2. Order intraosseous access. 3. Alter fluid administration. 4. Order ALS procedures as required for specific trauma assessment. Expeditious transport after initial resuscitation efforts is recommended. Note: Fluid boluses in children are best given by drawing up lactated ringers or normal saline solution in a 50 cc syringe and pushing via IV line port while closing off line above port, until 20 cc/kg have been infused. Gravity bolus takes too long in a child. TRAUMA - MECHANISM OF INJURY IN THE PEDIATRIC PATIENT Criteria For Use: Management of the pediatric patient involved in a traumatic episode with vital signs within normal range (Step I - Trauma Guidelines) but meets criteria of Step II - Anatomy/Mechanism of Injury requiring Trauma Center destination. ALS Provider Guidelines: 1. Perform initial survey, resuscitate as needed with spinal immobilization in place. 2. Administer appropriate oxygen and intubate if necessary. 3. Make decision concerning hospital destination and method of transport as soon as possible. 4. Initiate cardiac monitoring. 5. Without delaying transport or while arranging aeromedic transport as per #3, establish one IV. -----Contact Medical Command----Command Physician’s Actions Might Include: 1. 2. 3. 4. Alter patient destination or method of transfer. Alter fluid administration. Order MAST application and inflation pressure. Order ALS procedures as required for specific trauma assessment. Expeditious transport after initial resuscitation efforts is recommended PEDIATRIC BURNS Criteria for use : Management of pediatric burns characterized as moderate, and or critical in nature with or without associated trauma. ALS Provider Guidelines: 1. Perform initial survey. 2. Ensure airway and breathing 3. Administer oxygen appropriate for the condition and history. (Note: pay special attention for signs and symptoms of inhalation injury) 4. Decide hospital destination and mode of transport . Burn Center/ Trauma Center/closest hospital. 5. Without delaying transport, initiate IV appropriate for condition and infuse KVO until estimated weight or known accurate weight is established. After weight is established, infuse 10 cc/kg/hour. 6. Utilize length based tape or Broselow tape or other available devices for estimated weight or use the current known accurate weight of the patient. 7. Treat shock if present. Give a 20cc/kg bolus of NSS 8. Initiate cardiac monitor especially if burned by electricity. 9. Cover burns with dry sterile dressings or burn sheets. If the burn area is too large cover with regular cotton sheet. (Not flannel, use hospital sheets) --------Contact Medical Command-------Command Physician’s Actions Might Include: 1. Order additional airway control procedures, as necessary 2. Order additional IV’s or establish IO line if no IV established 3. Order morphine sulfate 0.1mg/kg titrated, IV 4. Order treatment for shock as per the pediatric shock protocol 5. Alter method of transport or destination facility.