Psyc 383: 3/20/07
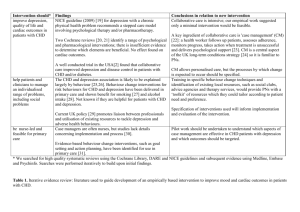
advertisement
PSYC 383 NOTES 4/24/07Thurs Review Session: Bring your question. Answer keys are posted in glass case on east side of third floor hallway in the Psyc building. Strong recommendation: Go through all 60 questions. On the final, there will be 10 questions from Unit 1, 10 from Unit 2, and 40 from Unit 3. Position opening: Assisting in course study guide revisions. My new book is now in print. There will be a book release party at UA Bookstore on Thursday, September 14, starting at 5:30pm. AIDS-Prevalence of AIDS is approximately 1 out of 100 adults. Human Immunodeficiency Virus (HIV) attacks helper T cells and macrophages. HIV is transmitted through the exchange of cell-containing bodily fluids (blood, semen). Early symptoms of HIV infection are mild, can look like cold or flu symptoms. This is followed by an asymptomic period. Later symptoms can include pneumonia, cancer (sarcoma, lymphoma), diarrhea, wasting, joint pain, blindness, CNS damage (dementia, confusion, coma) protease inhibitors, highly active antiretroviral therapy (HAAVT)--a cocktail of protease inhibitors. Effectiveness--in some cases, patients using these medications will no longer have detectable levels of HIV; patients must take the drugs daily; these drugs make it possible for some people with AIDS to live fairly normal lives. The primary populations that were initially at risk for HIV infection were homosexuals and iv drug users. Although these populations are still at risk, the highest rates of infection are among low-income minority populations, especially women, and adolescents and young adults. AIDS is associated with helper T cell levels below 200. The psychological effects of testing HIV+: Most people react with stress, sometimes anxiety and depression, which get moderated over time. A small subset of people become so depressed that they show suicidal ideation or behavior. Can lead to changes in liefestyle that include more exercise, quitting smoking, better diet, eliminating drug use, and safer sexual practices. Those people with HIV who disclose their status show improved immunocompetence. Teaching and developing safe practices: Gay men and adolescents who are high in self-efficacy with respect to condom use are more likely to use condoms. Those high in self-esteem are less likely to engage in anonymous sex. The kinds of preventive interventions that are most effective focus both on technical and communication skills. Motivational training, like goal-setting and monitoring of behavior. With iv drug users, the ways to reduce risky injection behavior are: 1. offer info on AIDS transmission 2. needle exchange programs 3. instruction on how to sterilize needles What doesn't seem to work is peer-based interventions with adolescents (e.g., bringing in other teens who either have AIDS or are HIV+). One of the defenses that adolescents use is to distance themselves from emotional threats, including peers who are infected with HIV. Internet has been effective mostly in providing info to those already infected with HIV. There is a correlation among HIV+ individuals between Internet use, social support, and positive coping skills. Stress increase the rate of development of AIDS symptoms, as do negative selfconcept and pessimism. Among gay men who conceal their homosexual identity, the rate of progression of the disease is higher. Bereavement can compound the effects of stress, as can depression. CANCER Cancer is linked to a malfunction in DNA that causes excessively rapid cell growth. Risk factors for cancer include: family history, ethnicity (Hispanics: high rate of cervical cancer; African Americans: prostate cancer; Japanese Americans: stomach cancer; Chinese Americans: liver cancer), diet, infections (HPV is linked to cervical cancer, H. pylori is linked to stomach cancer), SES, marital status "The Corporation" --Cancer rates have been linked to advances in industrial chemistry Stress affects both the incidence of cancer and the rate of progression of the disease SUMMARY: Stress makes you sick. Don't get stressed. Chemotherapy--nausea and vomiting, "anticipatory nausea" With child patients, distraction is very effective at controlling nausea and anxiety. This has been shown with research using video games. With cancer patients, one of the common complaints includes a decline in sexual activity, which is due to a number of factors, including body image concerns (mastectomy), sexual dysfunction due to the disease (prostate and gynecological cancers) or due to the treatment (chemo) Those patients who cope most effectively with cancer are those that use coping styles that involve seeking social support and focusing on the positive. Some patients with chronic diseases such as cancer discover new meaning and sources of joy in their lives as a result of having the disease. Patients with avoidant coping styles (engage in escape behavior to distract themselves or cognitive avoidance) are least effecticve at coping with the disease. Pharmacological interventions that are most likely to be used with cancer patients to manage symptoms focus on: 1 nausea and vomiting--medical marijuana, valium 2. anorexia and other eating difficulties--dietary supplements that stimulate appetite 3. emotional disorders such as depression and anxiety, which are treated with antidepressants and anxiolytics 4. pain,which is treated with morphine, methadone, and other opiates mindfulness-based stress reduction techniques have been effective at slowing the course of cancer and improving the quality of life among cancer patients; also can improve immune functioning individual and family therapy: patients seeking individual therapy are generally looking for help dealing with fear of recurrence, pain, or death; fear of organ loss; the interference of the disease with their quality of life and valued activities; job discrimination, relationship and dating problems patients seeking family therapy are looking for help dealing with communication problems in their relationship and their family life; changes in roles as a result of the disease (e.g., becoming more dependent on loved ones for care); sexual dysfunction. Support groups-- Are especially helpful for women, for patients who have more problems in their lives related to the disease (e.g., financial loss), fewer resources, less overall support from friends and family. Support group members live an average of 1.5 years longer with cancer than non-members. ARTHRITIS Rheumatoid arthritis (RA)-Cause: The immune system attacks the membranes surrounding the joints, leading to pain, inflammation, and stiffness (2million people) Symptoms--Pain and stiffness in the small joints of the hands and feets, wrists, ankles and neck. Treatment--aspirin (relieves pain/inflammation), rest, supervised exercise, stress management, pain management, social skills training Osteoarthritis-- (20 million) Cause: Wear and tear of the cartilage in the joints, which begin to crack and wear away over time. Symptoms include pain, stiffness and inflammation in the hips, knees and spine primarily Treatment- shark cartilage, weight loss, aspirin, exercise, anti-inflammatory drugs (steroids: cortisone), surgery (hip and knee replacements) Gout (1 million)-- more prevalent in men by about a 9-to-1 ratio Cause: Buildup of uric acid in the body due to the kidneys' inability to filter it out. The uric acid forms crystals which lodged in the joints and internal organs Symptoms: pain and inflammation in the joints, most commonly in the big toe Treatment: limit intake of alcohol and certain foods, increase in exercise, weight loss, and increased intake of WATER. 4/19/07Review questions on the final, taken from Units 1 and 2, will draw upon the exact same objectives that were tested on the two midterms. If an objective from Units 1 and 2 was not included on the midterms, it won't appear for the first time on the final. DIABETES Health risks associated with diabetes: Thickening of arteries, increased risk for CHD, blindness, nervous system damage, loss of limbs (amputation), sexual dysfunction, depression, increased risk for heart attack and stroke. Stress compounds the problem-- Cortisol inteferes with insulin function. The role of cortisol is to keep glucose in the bloodstream. Cortisol release causes the pancreas to secrete more insulin, which raises bp and heart rate and can also increase fat storage. Managing diabetes: Type I-- monitor glucose levels, and inject insulin Type II-- dietary control, weight loss, exercise, stress management, reducing carbs Adherence to management programs is poor among diabetics. Why? 1. Many of the most severe symptoms and complications associated with diabetes may take 15-20 years to show up ("invisible") 2. Diabetics often fail to monitor glucose levels, because it's inconvenient and because many believe that they can "feel" their glucose levels. 3. Injecting insulin is tricky and many Type I diabetics don't do it correctly. 4. With children: Parents are often more concerned about hypogycemia in their children then hyperglycemia. PreventionType II diabetics--Intensive lifestyle interventions, which support people in the process of changing their diet, exercise routines, and other aspects of lifestyle. These interventions can decrease the incidence of Type II diabetes by 58%. Type I diabetes-- The kinds of interventions that are used tend to be cognitivebehavioral: 1. Helping diabetics engage in appropriate self-injection procedures. 2. Building the habit of monitoring blood glucose levels. 3. Managing stress 4. Social skills training 5. Dealing with depression CH.14Psychoneuroimmunology-- The interaction of psychosocial factors with immune function. Immune SystemNatural immunity--immediate response to an infection, mediated by three different kinds of lymphocytes (lymphocytes are a type of white blood cell, or leukocyte, that is found primary in the lymphatic system): macrophages-- engage in phagocytosis (eat other organism), found mostly in the tissues of the various organ systems neutrophils--also engage in phagocytosis, but they mostly circulate in the bloodstream natural killer cells- They "lyse" foreign cells Non-specific, immediate, and cell-mediated Specific immunity-- Takes a few days to mobilize after an infection, mediated primarily by two types of lymphocytes: B cells- Humoral immunity (floating around in the bloodstream and the lymph), broadcase throughout the body T cells- Produce specific antibodies also but deliver those antibodies directly to the invader they're destroying immunocompetence-- immune function is healthy and normal immunocompromise-- immune function is suppressed Immunocompetence can be measured in one of two ways: 1. By measuring the number of certain types of lymphocytes (B, T, or NK cells). 2. By measuring specific aspects of immune function ( the ability of lymphocytes to kill invading cells, to reproduce, to engage in phagocytosis) How does the immune system respond to stress? It depends on the kind of stress: 1. Short-term stressors- Natural immunity begins to get mobilized, in anticipation of possible injury and/or infection 2. brief naturalistic stressors (stressors that last a few days: studying for a health psychology final)-- specific immunity may start to get mobilized as well; cytokine production increase (lead to inflammation); emphasis is on humoral immunity 3. long-term stressors-- Immune function gets depleted. Long-term exposure to stress depletes the body' fight-or-flight system, including the adrenals. What kinds of stressors have been studies in terms of their effect on the immune system? Space travel, exposure to hurricane (Hurricane Andrew), writing about traumatic experiences (fill you with guilt and shame), Three Mile Island, depression, anxiety, marital arguments, separation and divorce, caregiving of difficult patients ALL produce immunocompromise Symptoms of stress in both adults and children include vulnerability to all kinds of infection, including colds, viruses such as herpes, flu People with high self-efficacy and a sense of control show less immunocompromise in response to stress. Tons of evidence that relaxation training improves immune function: Melanoma patients show higher NK cell counts and higher NK activity, and are less likely to have a recurrence of melanoma, after undergoing relaxation training. 4/17/07 Hypertension- High blood pressure. Systolic (heart is contracting and pumping blood to the rest of the body) Hypertension is defined in terms of systolic ranges: 140-159 Mild 160-179 Moderate 180 or above Severe Ideal: Below 120 RISK FACTORS Above age 55, the risk for hypertension is 90% for men and women in our society. Hypertension increases the risk for CHD, kidney disease, and cognitive impairment. Prior to age 50, women are at a reduced risk for hypertension. Highest risk is among men, minorities, those with a genetic predisposition, those with high emotional reactivity to stress, negative affectivity, and anger; high in cynicism; those who strive against long odds ("John Henryism"--someone who works themselves to death) TREATMENT of hypertension: Low-sodium diet, reducing alcohol intake, weight reduction, exercise, caffeine restriction, the use of diuretics, which lower blood volume and sodium levels; adrenergic inhibitors-- block some type of adrenal gland activity central a.i.s-- block signals coming from the central nervous system to the adrenals peripheral a.i.s-- deplete catecholamine levels mind-body approaches: biofeedback, PMR, hypnosis and meditation, all can reduce b.p and have been shown to have modest but significant beneficial effects in treating hypertension Non-adherence to treatment is a problem for hypertension patients: Why? 1) Hypertension is largely symptomless; 2) People think that they can "feel" when their blood pressure and modulate it that way; correlations between perceived and actual bp are low. STROKE Two types of stroke: 1. ischemia--blood clot or other other blockage in the brain (drought); 80% 2. hemorrhage--rupture of a blood vessel in the brain (flood) Risk factors: Similar to CHD, including CHD, high bp, smoking, age, ethnicity (African American males over the age of 45 are at highest risk), prior stroke, family history of stroke, depression and anxiety, a history of transient ischemic attacks (minor strokes that produce temporary faigue, weakness, clumsiless, loss of feeling, loss of vision, speech difficulty) Effects of stroke: 1. Motor problems- Loss of movement of body parts on one side of the body. Strokes tend to be unilateral, with left hemisphere strokes affecting the right side of the body and right hemisphere strokes affecting the left side (right hem strokes are more common) 2. Cognitive problems-- Left hem strokes can affect speech (aphasia), short- term memory, learning new tasks; rt hem strokes can affect visual processing, judging distances, reading (dyslexia), awareness of impairment (anosognosia). 3. Emotional problems-- Left hem stroke can lead to anxiety and depression; right hem stroke can produce flat affect (indifference) Treatment: 1. Psychotherapy--including treatment of anexiety, depression and other psychological symptoms. 2. Cognitive remedial training-- restore intellectual/cognitive functioning Neurorehabilitation-- cognitive rehab based on the notion of plasticity, which is that the brain can rewire itself so that new areas take over for damaged ones 3. Training in specific skills- teaching stroke patients how to walk, drive a car, etc. 4. Use of structured, stimulating environments-- Computer simulations to help patients with hemineglect (patients with right hemisphere strokes will neglect the left side of space); objects appear on the neglected side and the patient has to learn how to attend to them, usually by turning their head to compensate Blood thinners-- prevent coagulation. One of the most effective blood thinner on the market for treating stroke patients is aspirin; with patients who have already had a stroke, daily dosages of aspirin can reduce risk of recurrence by 1/3. DIABETES Due to either insufficient insulin production by the pancreas (Type I diabetes) or insulin resistance (Type II diabetes), in which the cells of the body develop a tolerance to insulin. In both cases, glucose stays in the blood stream instead of entering cells, putting stress on kidneys while starving the cells of nutrients. Foods have a glycemic index, which is a measure of how much they increase blood glucose levels over a two-hour period following consumption. The standard by which glycemic index is calibrated is glucose, which has a value of 100. Sucrose-- g.i. ranges from 87-110 Honey-- 80's Agave nectar-- 11 Stevia-- herb that is used as a sweetener, gi is under 10 Fruits and vegetables have the lowest g.i., processed starches (white bread, white rice, mashed potatoes) have the highest; high-protein foods such as lean meat have a fairly high g.i. Insulin index-- measure of how much of an insulin response a food produces Type I- Abrupt onset before age 13, usually following a viral infection. It appears to be an autoimmune reaction in which the body's immune system attacks the cells of the pancreas that produce insulin. Early symptoms that lead to diagnosis: frequent urination, unusual thirst, uncontrollable food craving, fainting. Type I accounts for 10% of all cases of diabetes. Type II-- Onset occurs in middle age and late adulthood; linked to obesity; results from too much glucose in the bloodstream at one time, which causes cells in the body to become resistant to insulin; eventually, insulin production declines because there is more than the body can use. Symptoms: frequent urination, dryness in the mouth, loss of sensation in certain parts of the body, infections of skin, gums, urinary system; painful cramps in legs, feet, and fingers; slow healing of wounds; itching; drowsiness. 4/12/07CH.13: Heart Disease, Hypetension, Stroke, & Diabetes Heart DiseaseCoronary Heart Disease (CHD) seems to be linked to low-grade inflammation in the body. During inflammation, certain proteins are released, such as cytokine and c-reactive proteins (CRP) that isolate the area of inflammation and promote clotting. Those proteins have also been linked to the formation of fatty deposits in coronary arteries, and the resulting damage to arterial walls. Risk factors for CHD--smoking, obesity, high serum cholesterol, low levels of physical activity, metabolic syndrome Serum cholesterol is carried by at least two types of lipoproteins: Low-density lipoproteins (LDL) and high-density (HDL). LDLs deliver cholesterol from the liver to the other tissues in the blood stream and produce more deposits of cholesterol in arterial walls; HDLs carry cholesterol to the liver where it can be excreted from the body. cholesterol is a type of lipid or fat substance that is actually necessary in the formation of cell membranes in other physiological processes. metabolic syndrome--the occurrence of three or more of the following: obesity centered around the waist (the "apple" configuration), high blood pressure, low levels of HDL, difficulty metabolizing blood sugar (pre-diabetic condition), and high LDL levels. cardiovascular reactivity--is when your heart increase blood pressure and heart rate in response to a stressor relately easily. Cardiovascular reactivity is linked to the depositing of fats/lipids ion arterial walls, to increased inflammation, and to the narrowing of coronary arteries. Fluctuations in bp associated with cardiovascular reactivity also put wear and tear on the arteries. Psychological/social factors associated with CHD: Job-related stresses- Job strain (high demand/low contrl), working at a job that isn't rewarding or challenging, having low job security and little social support in the workplace. Social instability- People who are more mobile in their lifestyle are at higher risk for coronary heart disease: including those who live in industrialized countries, migrants, anyone else who is geographically unstable. Type A behavior-- Pattern of behavior characterized by: 1) high levels of hostility; 2) competitiveness; and 3) a sense of time urgency. Type A behavior is weakly correlated with CHD, but it predicts the risk of heart attack in those with CHD. The significant component of Type A behavior, in terms of its relationship to CHD, is hostility, which is linked to high levels of cytokines (pro-inflammatory proteins). People who are high in both hostility and defensiveness show the greatest correlation between cardiovascular reactivity and CHD. What are developmental factors associated with hostility. People high in hostility are more likely to be raised by parents who are punitive, who interfere and are controlling, and in households taht are high in conflict and abuse while being low in acceptance. Having hostility is NOT predictive of CHD to any significant degree, but expressing hostility is predictive. Some of the most effective therapeutic techniques for CHD patients who express a great deal of hostility is to train them in new speech patterns (learn to speak more slowly and softly). Gender and CHD-- Women tend to have higher HDL levels than men until menopause, which is believed to be linked to estrogen levels. Estrogen levels are known to also lower sympathetic nervous system arousal, blood pressure, and cortisol levels in response to stress. As a result, women have a lower risk of CHD than men of the same age. For menopausal women, hormone replacement therapy (HRT), and specifically estrogen replacement, has been tried as a means of reducing the risk of CHD, but at this point, research data don't support a positive effect of HRT on CHD. Gender differences in the way CHD patients get treated: CHD is diagnosed earlier in men and treated more aggressively (more likely to get prescription drugs or other interventions); women are less likely to receive counseling, education, preventive health measures, or to be placeed in stress management programs; they are less likely to receive beta blockers, aspirin, and lipid-lowering agents. Depression and CHD- The correlation between depression and CHD is HIGHER than that between smoking and CHD. Depression stimulates inflammatory processes in the body, including the release of c-reactive proteins. Treatment of CHDExercise programs-- Research with Type A men assigned them to one of two conditions: 1) aerobic exercise training; 2) strength and flexibility training. Both groups showed reduced cardiovascular reactivity, but the men in the aerobic condition also showed lower heart rates, bp, and oxygen consumption, both during a challenge task (doing some type of exercise such as running on a treadmill) and also while recovering from that challenge. Relaxation training- Relaxation does not reduce cardiovascular reactivity during stress but produces faster recovery. Those high in hostility can be retrained in terms of their speech patterns and their use of language. Cardiac rehabilitation-- For those who have had a heart attack, the goals of rehab are: 1) produce relief from symptoms such as chest pain; 2) reduce the severity of the disease; and 3) limit the further progression of the disease. When a person has a heart attack, certain factors improve the likelihood of recovery: 1) self-efficacy--believing that you have some control over your health status, and mastery of whatever self-treatment you've been prescribed; 2) coping style-- in the short term, repressive coping styles (not dealing with the emotions) can be beneficial; in the long-term, positive, problem-focused styles are most effective. Those higher in optimism and self-esteem are likely to recover from a heart attack most quickly. Types of drugs prescribed to CHD patients: 1. Beta-blockers-- These drugs block sympathetic nervous system activity, reducing catecholamine levels and therefore symptoms such as increases in heart rate and bp. Side effects: fatigue, impotence. 2. Aspirin- Blood thinner; it helps prevent blood clots by blocking the aggregation of platelets. 3. Statins--Target LDL cholesterol, reducies the risk of repeat heart attacks Most likely to be at risk for stress after receiving a diagnosis of CHD: 1. younger patients; 2. female patients; 3. patients with poor social support, high social conflict and negative coping styles Stress management programs are used effectively with CHD patients, focusing on the following: 1) recognizing stressful situations; 2) learn to avoid those situations; and 3) develop coping strategies for those situations when you can't avoid them. These programs produce a 34% reduction in mortality among CHD patients and a 29% reduction in the risk of an additional heart attack. Stress management has also been linked to improvements in body weight, smoking cessation, exercise, eating habists, blood pressure. How important is serum cholesterol in relation to CHD? For every 1% drop in blood cholesterol levels, you show a 2% drop in risk for CHD. 4/10/07Audio CDs are only available at Arizona Bookstore (821 N. Park). Hospice CareHospice movement really caught on with the work of Elizabeth Kubler-Ross. She was the first physician to consider the specific health care issues associated with the dying. Her five stages of dying: 1) Denial; 2) Anger; 3) Bargaining; 4) Depression; and 5) Acceptance. Strengths--She was the first to document the range of emotional reactions to dying; her research also pointed out the specific counseling/psychotherapeutic needs of dying patients; and broke through the taboos that the medical establishment had around death. The Tibetan Book of Living and Dying by Sogyal Rinpoche Weaknesses-- How the research has been interpreted by the medical community. Medical staff who work with dying patients take K-R's work too literally, assuming that it's "unhealthy" to not go through these five stages. This research paid too little attention to other emotional reactions, such as Anxiety, as well as the role of pain. K-R's work started the field of "Clinical Thanatology," psychotherapy/mental health care for dying patients; also started the movement towards "palliative care," which emphasizes the physical and psychological comfort of the patient. Curative care--curing illness Palliative care--easing pain Hospice--a movement to provide appropriate care to dying patients; the emphasis on the movement is on relief of suffering, and on creating an environment that is accepting of death, supportive of patients and their families, and that can be offered either at home, in a stand-alone facility, or in a hospital unit. Sogyal Rinpoche started a hospice program called Rigpa. Home hospice care--Has the following advantages: Far less expensive, the care can be as good (as long as there is training and supervision by medical staff), has a high degree of psychological comfort for the patient (control, familiarity, and social support). Challenges facing survivors--Flurry of activity, both in the days preceding death and following it: funeral arrangements, contacting friends and family, provide housing for out-of-town visitors; financial burdens; new responsibilities; grief According to the book, the most adaptive coping styles with grief are emotional avoidance and positive appraisals (reframing). Grief is a function of time. Why? Some process must happen over time that makes it possible for people for let go, for them to reframe what has happened, and to literally have a change in perspective. Least adaptive--ruminating about your loss; Focus is on the loss. What if you reframed it in terms of what you had, appreciation, gratitude? Impermanence-- Not taking for granted that things and people are going to last. Grief is a function of entitlement. Descriptive theory--presents human behavior, thought, and experience as "it is" Normative theory-- presents human behavior, thought, and experience as it "could be" Love = attachment Attachment styles-One type of attachment is the bond of affection formed between two people. The other type of attachment comes from feeling you have an entitlement/expectation of something from that other person. Dependence. Can you love without dependence? 4/5/07The grades in this course are determined ONLY by the cutoffs below: Grade A B C D F Score___ 115-140 95-114 75-94 55-74 below 55 Take your two midterm scores, add them, add 20 points to that, and subtract that sum from whatever cutoff you're aiming for. That will tell you how many points you will need on the final to get that grade. WARNING: Those 20 points are not a given. You CAN screw them up. As long as the journal entries are turned in: a) on time; b) complete (in terms of length); and c) addressing the topics listed in the syllabus, you will get 20 points. Hypothetical: 40 points on the two midterms, 20 for the journal (not guaranteed), equaling 60. If you're shooting for an A, which is 115, then you need 115 -60 = 55/60 on the final. The answer keys are posted on the third floor hallway of the Psyc building. My strong suggestion is to make sure that you can answer every question on both midterms. The same questions will not necessarily reappear on the final, but the review questions from Units 1 and 2 will address the same objectives and key terms. Of the 60 questions of the final, 20 are review. Finishing off CH.11: Chronic Illness How does chronic illness affect career and workplace? There is substantial research evidence showing that discrimination against people with chronic illnes is fairly common in the workplace. Employees with cancer are fired or laid off five times as often as other workers. If they keep their jobs, they are often given less demanding positions and are overlooked for promotions. This compounds the financial strain that is already produced by chronic illness: 1. The patient may lose some or all of his/her income. 2. May lose health benefits. 3. If the patients keeps health benefits, s/he may find that they're underinsured. What are trends in caregiving for the chronically ill? Typical caregiver is a woman in her sixties, caring for an elderly spouse. What types of caregiving are there? 1. intermittent/supplementary--for patients who can manage their disease with periods of relapse 2. short periods of high intensity--e.g., stroke patients recovering and regaining lost cognitive and physical functioning. 3. increasing responsibility--for progressive diseases, such as Alzheimer's Risks to the caregiver: stress, depression, declining physical health, lowered immune function, and strained relationships. Gender differences in terms of the kinds of caregiving received: Chronically ill women may experience less social support, lower incomes, higher levels of disability, and are more likely to be institutionalized. CH.12: Death and Dying Average life expectancy: 77.4 years That statistic takes into account infant mortality rates, which in the US are among the highest of any developed/industrialized nation (~7 per 1000). Why is infant mortality so high in the US? Maternal and prenatal are not covered by a national medical program, unlike in most developed nations. Causes of death: Differ by point in the life cycleInfancy--the main causes are congenital abnormalities and sudden infant death syndrome (SIDS). What is SIDS? The only really known symptom is that the infant stops breathing suddenly. SIDS is correlated with SES, mothers' smoking during pregnancy, and with the position in which a child is put to sleep (infants who sleep on their stomach are more likely to die of SIDS). Childhood--the main causes of death are accidents (40%), including accidental poisoning, falls, automobile accidents, drowning; cancer is second (childhood leukemia) Adolescence-- The main causes are automobile accidents, followed by homicide, suicide, cancer, AIDS Older adults--degenerative diseases (cancer, CHD, stroke, organ failure), and accompanying infectious diseases (pneumonia, influenza) In older adults, health and mortality rates are predicted by the following psychosocial factors: 1. Life satisfaction2. Mood/mental state-- Depression is a factor that increases mortality significantly among older adults. 3. Relationships-- Stronger social support network is associated with lower mortality, better health, and better quality of life. RIGHT TO DIE Many chronically ill patients, such as those with renal failures, refuse life-saving treatment, such as kidney dialysis, because of the severe pain involved. Medical technology has advanced enough to have many different kinds of measures to sustain and extend life under "extraordinary" circumstances. Final Exit, a bestseller that gave people specific instructions for how to commit suicide. US Patient Self-Determination Act (1990)-- Hospitals an other medical facilities that receive either Medicare or Medicaid funding must have written policies in place concerning patients' wishes regarding life-sustaining measures. Do Not Resuscitate (DNR) order-- Requires medical personnel NOT to intervene when a patient stops breathing. Oregon Death with Dignity Act (1997)-- Allows physician-assisted suicides in very specific cases 4/3/07- Chronic Illness Chronic illnesses are illnesses that last more than six months; they can be recurring, stable, or progressive. Diabetes, cancer, CHD, paralysis (paraplegia, quadraplegia) How does chronic illness affect quality of life? 1. Physical functioning--Limits mobility, sensory perception, use of arms and hands. 2. Social functioning--Family life, work life, recreational activities, friendships. 3. Psychological state-- Depression, anxiety, stress 4. Disease-related or treatment-related symptoms--pain, nausea, insomnia Psychological state Anxiety--Anxiety is highest among those patients awaiting test results, awaiting invasive procedures, anticipating or experiencing negative side effects of treatment, experiencing major life changes related to the illness, feeling dependent on others--especially medical staff, or lacking information. Ramifications of anxiety in chronically ill patients: Anxious patients cope more poorly with treatments such as chemo and radiation; in the diabetics, there are more fluctuations in blood glucose levels, increase the severity and the frequency of symptoms, and can dleay recovery. Depression-- There are the following ramifications: increased risk for severe chronic illness, speeds up the onset of symptoms, reduces adherence, increases mortality, promotes passivity, and affects medical decision-making. Diathesis-stress model-- There is a predisposition that may even be genetic to experience certain conditions (e.g., depression), and that predisposition interacts with environmental stressors to compound the effects of the condition. Problems with diagnosing depression in chronic illness: The physical signs of depression (e.g., fatigue, weight loss, sleeplessness) also happen to be symptoms of the disease in some cases or side effects of treatment. Coping with chronic illness-- There are different coping styles for any stressor, including chronic illness, and they vary on at least two dimensions: active vs. passive problem-centered vs. emotion-centered avoidant vs. confrontative The coping styles that are most common among chronically ill patients are: 1. Social support/direct problem-solving-- Looking for practical solutions to one's problems, including help from others. 2. Distancing-- Neutral coping style that neither confronts nor avoids the problem but puts emotional distance from it, as if it were occurring to someone else ("Let's not worry about that") 3. Positive focus--About 1/3 of chronically ill patients claim that the quality of their lives has IMPROVED since the onset of their illness; some people find meaning as a result of their illness, and respond to it with joy, optimism, appreciation. 4. Cognitive escape/avoidance--Wishing the situation would go away, Distracting oneself, Denial. 5. Behavioral escape/avoidance--Distracting oneself actively with drugs and alcohol, or other forms of "escapism." Denial isn't always maladaptive. Immediately after a diagnosis, denial can protect the person from depression, anxiety and stress. People with high initial denial actually spend fewer days in intensive care, and fewer side effects of treatment. BUT denial takes its toll in the long-term, and it's not an effective strategy in terms of long-term survival, adherence, and severity of symptoms. How does coping differ in chronically ill patients compared to individuals dealing with other stressors? Chronically ill patients report using fewer active coping strategies (e.g., planning, problem solving, confrontative) and more passive coping (escape/avoidance, positive focus). What about patients who respond with self-blame? Adaptive- That it can lead a person to feel a sense of control over their situation (perceived control and self-efficacy have enormous beneficial effects in coping with stress) Maladaptive- It can create feelings of guilt, depression, and self-recrimination. TREATMENT Physical therapy/rehabilitation Goals of rehab with chronically ill patients are: 1. To learn how to use one's body as much as possible. 2. To learn how to sense changes in the environment and to react appropriately. Orientation and mobility-- Hearing and visually impaired individuals are trained to maneuver in their environment (e.g., cross a street, catch a bus) 3. To learn new physical management skills (personal hygiene, dressing oneself). 4. Learn how to administer a specific treatment regimen (do specific exercises). 5. To learn how to control the expenditure of energy. Psychotherapy How does this psychotherapy differ from that other types of patients? 1. Therapy tends to be episodic rather than continuous (work around their treatment schedule). 2. Therapy requires more respect for the patient's psychological defenses (e.g., defenses such as denial may be adaptive for them in some cases). 3. Therapy requires cooperation with medical personnel and family members. 4. Therapist must understand the illness, including symptoms and treatment. Relaxation training has been used successfully with chronically ill patients to: 1. Lower anxiety and nausea from chemotherapy. 2. Lower the likelihood and severity of asthma attacks in asthmatic patients. 3. Reduce pain. Support groups serve a variety of functions: 1. To discuss issues of mutual concern about the illness. 2. Provide information about the disease, coping, treatment alternatives, etc. 3. Offer opportunities to share emotional experiences (cathartic) Support groups are effective in increasing adherence to treatment regiments for the following reasons: 1. When people commit publicly to doing something (e.g., such as changing a behavior), they are more likely to do it. 2. People in support groups learn from their peers which modes of treatment are most effective. 3. Emotional support and encouragement facilitate adherence. 3/27/07: Review Session II-13c) Patient dissatisfaction with HMOs 1. Providers do not seem too concerned with patient satisfaction. 2. Cost-cutting has resulted in shortened stays and also a reluctance to perform expensive tests. 3. Long waits and short visits (12-15 minutes). 4. DRG are poor predictors of patient needs. DRG's are diagnostic related groups; patients are classified based on diagnosis, and that determines the kind of care and length of hospital stay. II-3e) Discuss the findings of research using the "hassle scale." Daily hassles--minor strains of our everyday life (e.g, traffic jams, noise, chores/obligations). These minor hassles turn out to be BETTER predictors of health outcomes than stress. II-2a) Describe the methods commonly used as indicators of stress. 1. self-reports of perceived stress and life change SLE (stressful life events) questionnaires 2. physiological measures (heart rate, bp, catecholamine levels, cortisol levels) 3 behavioral measures (performance under stress) II-7h) Compare the health benefits of marriage for men and women MEN--Health benefits are dramatic (life expectancy, various measures of physical health, all improve) WOMEN-- Health benefits are minor II-7d) Identify two potential costs of social support Costs of RECEIVING social support: 1. Guilt associated with placing demands on someone else's time/resources 2. Threats to self-esteem and independence II-2b) List the methodological problems associated with stress indicators. 1. self-report--subject to bias and inaccuracy; SLE questionnaires have methodological limitations such as treating positive and negative events equally, not taking into account individual differences in responding to SLEs, and not taking into account the duration of SLEs. 2. physiological measures--increases in measures such as bp and heart rate are not necessarily caused by stress but can be caused by other factors such as physical activity or sexual excitement. 3. behavioral measures--decreases in performance on cognitive or physical tasks are not necessarily due to stress but may be caused by other factors such as fatigue and boredom. II-2c) The following find positive events more stressful than negative ones: People with low self-esteem Those with a pessimistic explanatory style II-4a) Summarize the findings on the effects of early SLEs Children from families that are high in CONFLICT/ABUSE and low in NURTURANCE may develop increased sympathetic nervous system reactivity (the sympathetic n.s becomes aroused at the slightest arousal), exaggerated cortisol response, and may be more susceptible to a variety of chronic illnesses, including diabetes, depression, CHD, and lung disease. Even modest family stress in childhood can have some of these effects. II-4d) Describe the demand-control-support model Focuses primarily on workplace stress: when high demand is combined with low control and little social support, the risk for CHD is highest. II-4 f) List seven ways to reduce occupational stress: 1. 2. 3. 4. 5. 6. 7. Reduce physical stressors such as noise. Minimize job ambiguity and unpredictability. Involve workers in decision-making. Make jobs more interesting. Encourage social relationships. Focus on rewards rather than punishment. Look for early signs of stress (suggestion for supervisors). II-6c) Discuss the effects of disclosure on stress and illness Individuals who write about traumatic events in their lives show better health outcomes six months later. Widows/widowers who have an opportunity to talk with an objective third-party about the death of their spouse show a reduced susceptibility to illness, suggesting that immune function improves. II-13 Difference between nurse practitioner and physicians' assistant--Nurse practitioners have gone through nursing school; they have nursing degrees (RN) and then advanced training beyond that. PAs go through an entirely different training program. II-8b) The illnesses that stress management programs have been effective in treating: migraines and tension headaches, MS symptoms, high bp, CHD II-7a) Discuss the effects of external resources on health time, money, education, a good career, children, family, a high standard of living People with greater resources typically cope better with stressful events; People with high SES have fewer health problems overall and lower mortality II-16f) Describe the pathway followed by nociceptors Nociception--pain perception (NOTE: that's different than pain sensation) Perception = sensation + interpretation Two main pathways: A-delta fibers- Small, myelinated fibers that transmit sharp pain quickly (40 mph). A-delta fibers are more closely linked to mechanical and thermal pain, acute vs. chronic pain, and they project onto the thalamus and the sensory areas of the brain. C-fibers- large, myelinated fibers that transmit dull, throbbing pain slowly (~5mph). These fibers are more involved in chronic, polymodal pain (combination of thermal, chemical and mechanical pain), they project onto frontal areas of the cortex that are more associated with motivational and affective components of pain. II-11b) Nosocomial infection--infections caused by receving medical care or being exposed to infectious microbes in a hospital setting 1999 statistics-- Of 10 million hospitalized patients in the US, 2 million contracted infections there, and 90,000 died of those infections (~1%). II-11c) Two cost-containment strategies that affect hospital care: Diagnostic-related groups (DRGs)--The diagnosis that a patient receives falls into a certain category that determines hospital stay. Preferred provider organizations (PPOs)-- A network of affiliated practitioners that has agreed to charge a fixed rate for particular medical services. II-13d) List three components of holistic health care holistic health care--is a form of health care that is based on the assumption that health is a positive state and not just the absence of disease patient education, self-help, and self-healing The emphasis is preventive and it has a do-it-yourself orientation (The premise that all healing is self-healing). II-15b) Patient-centered communication (based on humanistic principles that were first outlined by Carl Rogers)--involving the patient directly in decision-making, respect the patient, and treat the indvidual with empathy, greeting the patient, addressing the patient by name, and explaining the purpose of every procedure The primary benefit is that it improves patient-provider communication and works especially well for "difficult" patients. Love, Medicine, and Miracles by Bernie Siegel II-15c) Communication courses for physicians should include: 1. Supervised contact with patients. 2. Immediate feedback on the nature of the interaction. 3. Videotaping of interactions. II-14d Non-adherent patients tend to cite the following: 1. Lack of time. 2. Lack of money. 3. Lack of support at home. II-15d Two institutional interventions that can foster adherence: 1. Postcard reminders or phone calls--Minimizes the likelihood that people will miss an appointment because they forgot or scheduled something else in its place. 2. Reduce wait times betweeen appointments II-15e Adherence to a medication regimen is a function of understanding. To increase understanding: 1. Medication info sheet that includes a description of the medication, dosage, and possible side effects. 2. Take-home pill calendars 3. Special pill packing such as pill boxes with compartments for each day of the week. II-15h 55% of nonhospitalized patients have taken some kind of drug in the last 24 hours; 40% of adult Americans use some medication on a regular basis Hospitalized patients receive an average of 14 drugs a day, which are taken simultaneously. II-16c Factors that affect the experience of pain: 1. Interpretation 2. Context in which the pain occurs. 3. Culture--in some cultures, pain is reported sooner and people react more strongly to pain. II-16d Dimensions of pain that are measured by pain questionnaires: QUALITY (dull, throbbing, stabbing, aching, burning) and INTENSITY (on a scale of 1-10) II-16e 1. mechanical pain--results from mechanical damage (e.g., tearing or squishing) to tissue 2. thermal pain-- exposure to extreme temperatures 3. polymodal pain--a combination of different types of pain (more associated with chronic vs acute pain) II-16h Substance P--distributed throughout the peripheral nervous system and in some internal organs, and it's released by nociceptors. The effects of substance P can be blocked or reduced by methods such as counterirritation (stimulates different types of sensory receptors in adjacent areas of the body) and glutamate--modulating neurotransmitter; it delivers pain signals to the brain II-15f Example of placebo effect in active treatment: Morphine loses 25% of its effectivess when people don't know that they're being given a painkiller (25% of the effect of morphine is due to patient expectations/beliefs). II-14e) 1. find out what happened 2. get an apology 3. know that the mistake will not recur Chronic pain, unlike acute pain, is linked to personality correlates: There are subscales of the MMPI that are correlated with chronic pain (hypochondriasis, hysteria, and depression) II-16j Evidence that endogenous opioids are involved in stress-induced analgesia Endogenous opioids (such as beta-endorphins) are found in adrenal glands, pituitary glands and the hypothalamus (HPA axis). The release of these opioids is triggered by autonomic arousal due to stress or physical exertion. II-13g Stereotypes based on age, sex, race, and mental illness 3/22/07: Treating Chronic Pain http://vas.web.arizona.edu, click on the Psyc 383 Notes link (within 24 hours, more or less, of a lecture, I will post notes) Nisbett & Schachter (not on the exam)-- The researchers gave a subjects a placebo and told them to expect certain symptoms such as jitteriness and heart palpitations, which happen to be symptoms of receiving an electric shock. Those who took the placebo endured more shock. Surgical techniques-- Two types: 1) structural-- back pain is often treated by fusing or removing discs in the back; 2) pain blocking-- ablation (cutting or severing) nerve tissue, surgical damaging of nerve endings, fibers, or ganglia. The disadvantages of this kind of surgery: 1. 2. 3. 4. 5. The effects of surgery are temporary. Risky. Painful side effects. Expensive. Can worsen the problem by damaging pain fibers. Neuropathic pain is pain caused by nerve damage. This surgery involves damaging nerves. Therefore... The primary advantage is that this type of surgery works for some people some of the time. If cutting nerves could stop pain, then there would be no phantom limb syndrome. How does phantom limb work? Is it the result of severed nerves leading to the limb? The assumption is that those nerves atrophy over time. Areas of the amputated or lost limb get remapped onto other areas of the body, such as the face. Buddhists make the distinction between pain and suffering. Pain is an inevitable part of life; it comes with being in a body. But suffering is a cognitive process, and to some degree under our control. Suffering is a combination of the cognitive, emotional, motivational and interpersonal components of pain. Pain management techniques: BIOFEEDBACK-Consists of four different phases: 1. Baseline phase--The patient is wired up to a device/instrument that measures a physiological process (e.g., heart rate, bp, muscle tension, skin conductance). The pre-treatment levels of that process are then recorded. 2. Shaping/reinforcement phase-- Here, the patient learns to alter this physiological process with the aid of the instrument. 3. Test phase-- In this phase, the patient tries to alter the process WITHOUT the use of any instruments. 4. Follow-up-- After a few weeks, the patient is hooked up to the instrument again to make sure that s/he is still successful at altering the process. Biofeedback is especially effective with tension headaches and certain kinds of muscular pain. These types of pain are directly linked to muscle tension, which can be controlled or altered through biofeedback. Less effective for other types of chronic pain that are more complex in their mechanism. The disadvantages of biofeedback are that it requires instrumentation, which is expensive and inconvenient. (Note: In the biofeedback exercise on the audio CDs for this course, YOU are the heart rate monitor) RELAXATION-The standard method, developed by Edmund Jacobson in the 1930's, is called progressive muscle relaxation (PMR). Why does PMR work in relaxing muscles? The current thinking is that it works through an opponent-process mechanism. If you initiate a process such as tensing a muscle, your body will automatically initiate a counterbalancing, compensating, or opponent intended to counteract the effects of that first process. For every muscle tension process, there is a muscle relaxing process that compensates for it. When the initial tensing stops, the muscle relaxation continues. PMR is moderately effective at pain control, but certainly no less than biofeedback, and it's much easier to do. HYPNOSIS-- One of the primary applications of hypnosis is pain relief, but mostly it's used with acute pain: dentistry, childbirth, burn victims, and other surgical anesthesia. What is hypnosis? At the core of hypnosis is something called the "classic suggestion effect." This is when a person responds to a suggestion with a sense of involuntariness. They carry out the suggestion voluntarily but have the sensation of something happening on its own. Usually hypnosis is used in conjunction with other pain control methods, such as chemical anesthesia, distraction. DISTRACTION-- You draw attention away from the pain. Studies in which dental patients are either given music (that's enjoyable) to listen to or nothing, the patients in the music condition experience much less pain and distress. VISUALIZATION/IMAGERY- There are two kinds of imagery that can be used with chronic pain: 1) Relaxing imagery--soothing, calming images and scenes; 2) aggressive imagery--this type of imagery is used more to address the cause of the pain rather than the pain itself (you envision your body's immune system as soldiers battling an infection). Both are reasonably effective at controlling pain, suggesting that they work because they provide distraction from the pain. COGNITIVE-BEHAVIORAL TECHNIQUES--These techniques are effective to the extent that they address the patient's self-efficacy in terms of being able to manage their own pain. How do these techniques improve self-efficacy? 1. Having patients reconceptualiz their pain as something manageable. 2. Having patients believe that they either have the skills or can the skills needed to manage that pain. 3. Having patients redefine themselves as being active players in their own pain management as opposed to passive recipients. 4. Having patients monitor their thoughts to avoid non-productive thought patterns (e.g., not using terms like "my pain"). 5. Patients learn to attribute their improvement in health to their own effectiveness. 6. Learning to cope with situations that are more likely to give rise to pain. INTERDISCIPLINARY TEAM APPROACH TO PAIN MANAGEMENT These programs involve a team that includes physicians, physical therapists, psychologists, and occupational therapists. The programs tend to consist of four components: 1. Patient education--Teaching patients about the nature of their condition or disorder. 2. Training in pain reduction techniques--Biofeedback, hypnosis, PMR, guided imagery, etc. 3. Group therapy to deal with the emotional and psychological effects of chronic pain. 4. Cognitive-behavioral therapy to deal with non-productive thought patterns. Psyc 383: 3/20/07 http://www.actonwisdom.com (Act on Wisdom) CH.10: Pain and Its Management Pain- For patients, pain is the central issue. For providers, it's just a byproduct of disease or injury. "extraneous variable" The chance of a chronically or terminally ill patient becoming addicted to morphine who doesn't already have a drug addiction is .03%. Pain management is not a topic that is addressed to any extent in most medical schools. Physiological mechanisms of painThere are two types of nerve fibers that carry pain signals to the brain: 1. A-delta fibers--Small, myelinated fibers that carry information about acute, sharp pain, such as mechanical/thermal pain. The rate of transmission in these fibers is 40 mph. 2. C-fibers--Unmyelinated, involved in polymodal pain transmission, carry information about dull, aching pain such as chronic pain. Types of pain1. mechanical pain- pain associated with stretching, tearing, or compressing of tissue. 2. thermal pain- pain associated with extreme heat and cold. 3. polymodal pain- pain that is due to a combination of factors, including mechanical, thermal, and chemical (e.g., skin irritation) Distinguish pain in terms of duration: acute (short-term) vs. chronic (lasts more than 6 months) Types of chronic pain- 30-50 million Americans suffer from some kind of chronic pain. 1. Benign chronic pain-- Pain that lasts more than 6 months but that doesn't get worse, and is not life-threatening (e.g., chronic back pain). 2. Recurrent acute pain-- Pain episodes don't last more than a few hours or days, but the pain episodes recur on a regular basis (e.g., migraines). continual (happens steadily) vs. continuous (recurs) 3. Chronic progressive pain-- Pain that increases in severity (e.g., degenerative disorders, cancer). How does the brain process pain information? All pain signals project onto the reticular formation first. 1. A-delta fibers- Project onto thalamus, which relays the signal to the somatosensory cortex (sensory areas of the brain) A-delta fibers provide mostly SENSORY information. 2. C-fibers- Project onto different thalamic and cortical areas. These fibers provide EMOTIONAL and MOTIVATIONAL information. Two aspects of pain: The sensation, and the cognitive-emotional experience. Gate control theory-- There are "gates" in the spinal cord that determine how much pain information reaches the brain. The gates are probably nerve bundles in the spinal cord. Whether the gates open or close is determined by a number of factors: 1. intensity of the stimulus that gives rise to the pain signal. People are VERY good at rating the intensity of their pain (accurate and precise). Typical pain intensity scale is 1-10 (1= lowest; 10= highest) 2. interpretation of the events 3, pain thresholds-- A function of individual differences, including gender and cultural differences. 4. level of physiological arousal-- Endogenous opioids are neurotransmitters that the opiate drugs mimic. Endorphins are a type of endogenous opioid found in the limbic system and brain stem. There are two other types of opioidsProenkephalins (endocrine and nervous system) and the prodynorphins (intestines, pituitary glands). In general, endogenous opioids are found in the hypothalamus, pituitary and adrenal glands (the HPA axis). Under certain conditions of physiological arousal, the HPA axis triggers the release of opioids that moderate pain. This may be why athletes can endure higher levels of pain and still function during competition. When the arousal is due to psychological stress and the SAM system kicks in, producing cortisol, opioid production can be blocked and pain levels can actually increase. Pain can be categorized as follows: 1. Nociceptive pain-- The experience of pain coming from signals delivered by pain receptors receptors (nociception = pain reception). Nociceptive pain is a by-product of injury or disease. It's a signal of something happening at a chemical, thermal or mechanical level. 2. Neuropathic pain- Pain associated with damage to the nervous system. If a nerve is damaged so that it does not deliver a clear signal, the brain interpret that damage as pain. (neuropathy = "sick nerves") In neuropathic pain, the pain IS the disease. Chronic pain can be considered a disorder of the nervous system. Gate control theory would say that gates in the spinal cord have been kept open by signals from the brain, so that the nervous system is hyper-sensitized to whatever stimuli there are in the damaged or injured area. Who suffers from chronic pain? Are there psychological predictors of chronic pain? In studies of personality, chronic pain patients have shown higher than average scores on three MMPI subscales: 1. Hypochondriasis-- Preoccupation with bodily functions, tendency to interpret normal sensations or minor problems as serious ones. 2. Hysteria-- Patterns characterized by dissociation (sudden, temporary alteration in identity, memory, or consciousness) and the tendency to convert psychological distress into physical symptoms (conversion disorders). 3. Depresson Chronic pain is a combination of physiological and psychological factors, including social, behavioral, cultural and emotional/motivational components. Chronic pain disrupts virtualy all aspects of the person's life, including: work, leisure, family life, friendships, sleep, income, self-esteem, sex life. CHRONIC PAIN CAN BE CONSIDERED A PSYCHOLOGICAL DISORDER (It does not yet have its own diagnostic category in the DSM) Chronic pain can be somatogenic (originates in the body) or psychogenic (originates in the mind). 3/8/07: Patient-Provider Communication Beckman & Frankel (1984)- On a first visit to a physician, patients get interrupted 18-22 seconds into their description/explanation of their symptoms. In the first 20 seconds, the physician has already made a diagnosis. Complaints about physicians: 1. They're not good listeners. 2. They either use jargon, on the one hand, or baby talk, on the other. Why jargon? a) That's the language that physicians have learned to use in their careers. b) To keep patients from asking too many questions or from discovering what the physician doesn't know or is unsure of. c) Inability to gauge the level of understanding of their patients. 3. Subtle prejudices and stereotypes that affect physicians' performance. a) Caucasian physicians sometimes feel less comfortable with patients who are from various minority groups (African-American, Hispanic); this discomfort can affect the physician's proficiency in terms of diagnosis and treatment. b) negative perception of the elderly- Older patients are resuscitated less often in ERs, or less time is devoted to life-saving measures in their cases. c) Sexism-- Women's complaints or health issues are more likely to be dismissed by male physicians. An increasing number of female patients are seeking out female physicians. 4. Diagnostic skills are often lost because medical school training emphasizes the use of instrumentation (MRI, CT scans). 5. The quality of treatment associated with HMO's is considered inadequate by many patients. a) Providers don't seem to be too concerned about patient satisfaction. b) Cost-cutting procedures used by HMOs have resulted in an unwillingness by physicians to perform costly tests and procedures. DRG's (Diagnostic-Related Groups)- The kind of care, the expense, and the length of hospital stays is determined by the diagnostic classification or category in which the patient's illness is placed. DRGs do not account for individual differences in terms of the intensity and duration of symptoms, as well as response to treatment. c) Long waits and short visits (The average doctor's visit lasts 12-15 minutes) How does the patient contribute to poor patient-provider communication? 1. Patient's mental state--Patients with anxiety are more likely to exaggerate their symptoms or not to focus clearly on physicians' instructions. 2. Patient's knowledge--Differences in level of understanding dure to social class, sociolinguistic factors (English may not be a patient's first language), education level. 3. Patient's attitude- a) Attitudes towards their symptoms, focusing more on pain than on other symptoms; b) Fear of asking questions--concerns about embarrasment; c) Embarrassment about socialy inappropriate behavior (e.g., patient with an STD is often not too thrilled to discuss the events leading to that diagnosis). Non-adherence or non-compliance-- Sometimes, the communications breakdown between providers and patients causes patients to disregard the physicians' instructions. Most non-adherence is intentional, especially in older patients. What kinds of instructions or treatments are more likely to result in non- adherence? Lowest adherence levels are for vocational advice (e.g., "Take time off work") Highest adherence levels are for advice that seems "medical" (a prescription for a medication) Some illnesses produce better adherence than others: High levels-- HIV, arthritis, cancer Low levels--diabetes, sleep disorders These disorders require behavior change. If you have to change a behavior such as your sleeping or eating patterns, you're less likely to adhere to the course of treatment. Behavior change programs for smoking/obesity have an 80% dropout level. Why do patients not adhere to medical advice in some situations? If you ask patients, they will tell you: a) lack of time; b) lack of money; or c) conflicts with their personal/home life. Some patients don't understand the instructions. Adherence can be increased by: 1. Asking patients to repeat instructions. 2. Writing down the instructions. 3. Offering to clarify unclear instructions. 4. Repeating the instructions. Institutional procedures to increase adherence: 1. Postcard reminders or phone calls before an appointment. 2. Reduce wait times (both from the time that an appointment is scheduled until the appointment date; wait times in physicians' waiting rooms). Medication-related adherence: 1. Medication info sheets that include a description of the side effects and standard dosage level. 2. Take -home pill calendars that let patients see when they're scheduled to take certain medications. 3. Pill packaging--Organized by date and time of day. What can be done to improve patient-provider communication? We need to understand what patients are looking for in their providers. They rate physicians more positively and as more competent who are: warm, empathic, and confident. EMPATHY and RESPECT The best predictor of physician sensitivity is the phycian's report interest in the welfare of people. In other words, sensitivity and good communication skills are less about ability and more about motivation. Some training programs are being developed to improve physician communication: 1. Supervised contact with patients. 2. Feedback from instructors. 3. Physician-patient interactions are videotaped. Physicians are also encouraged to: 1. Greet patients 2. Address them by their name 3. Listen without interrupting 4. Explain the purpose of a procedure before doing it 5. Consulting with the patient about medical decisions Placebo Effects People in the U.S. love taking medication. Over 40% of adult Americans take some medication daily or regularly. Hospitalized patients take an average of 14 different drugs a day. A big part of the effect of these drugs is a placebo effect. To some degree, the drugs work because of patients' expectations and beliefs. When painkillers such as morphine are compared to placebos, the placebo is effective in relieving pain in 35% of cases (rule of thumb: placebo effects work for about 1/3 of the people who are given a placebo). Placebos are most effective when they look and taste like "real" medicine. The placebo effect is a big part of the beneficial effect of standard drugs. If a pain patient is given morphine without knowing what s/he is being given, the effectiveness of the morphine goes down 25%. Latin--"I will please;" the implication is that the patient is in some way pleasing the physician by accommodating the request to get better. What are the qualities of a patient for whom the placebo effect is likely to be strongest? 1. High need for approval 2. Low self-esteem 3. External locus of control 4. High suggestibility 5. High levels of anxiety Most likely, placebo effect are related to the same two personality characteristics as hypnotizability: imaginative involvement and absorption. These people can focus their focus their attention on something to the point of filtering out all else, and they tend to get involved in their imaginations and fantasy life.