Applicable Clinical Laboratory Safety Regulations
advertisement
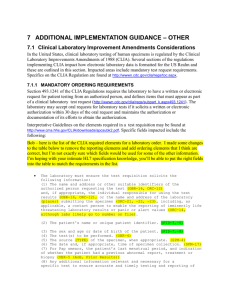
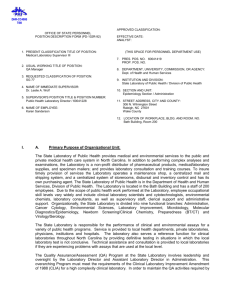
BMET Course Development IUPUI Applicable Clinical Laboratory Safety Regulations PART II Clinical Laboratory Improvement Amendments of 1988 (CLIA ‘88) This unit will present information regarding the clinical laboratory’s compliance with the safety related standards required by the Clinical Laboratory Improvement Amendments of 1988 (CLIA ’88). Section 1: What is CLIA? Section 2: CLIA’s Safety Regulations. Section 3: How does CLIA affect BME ? Section 4: Compliance Tips Section 5: The most common CLIA deficiencies related to BME. Section 6: Resources PART II, Section 1: What is CLIA? Actually, CLIA is an acronym for two separate federal documents. CLIA was enacted by the U.S. Congress in 1967 as “The Clinical Laboratory Improvement Act of 1967.” This was called CLIA ’67 and served as the basic quality assurance guidance document to clinical laboratories for over 20 years. In the mid 1980’s, due to changes in medical technology and growing concern for the quality of testing in labs, Congress amended the original document. With these approved changes, the federal statute became “The Clinical Laboratory Improvement Amendments of 1988. So the original CLIA ’67 became CLIA ’88. The focus of CLIA has always been to improve the quality of clinical laboratory testing. Quality has many definitions, but it is generally agreed that quality work cannot occur in an environment that is hazardous or unsafe to the workers or patients. If one reads the CLIA ’88 document, you will find only a few sections devoted to safety. But those few words clearly emphasize that safety is an essential to a quality organization. June 2000 1 BMET Course Development IUPUI PART II, Section 2: CLIA’s Safety Regulations. As previously mentioned, CLIA addresses safety in general terms only a few times in the entire document. But those few words effectively convey the federal government’s concern about working in a safe environment. The four key CLIA safety standards are: 1. Standard 493.1204(a). The laboratory must provide and ensure maintenance of the utilities necessary for all phases of testing, including pre-analytic (specimen preparation, reagent preparation and analytical instrument preparation), analytic (testing), and post-analytic (posttesting data processing) as appropriate. 2. Standard 493.1204(b). Safety precautions must be established, posted, and observed to ensure protection from physical hazards and biohazardous materials. 3. Standard 493.1205(c) – (1) – (iv). The laboratory must define criteria for…protection of equipment and instrumentation from fluctuations and interruptions in electrical current that adversely affect patient test results and test reports. 4. Standard 493.1445(e)-(2). The laboratory director must ensure that the physical plant and environmental conditions are appropriate for the testing performed and provide a safe environment in which employees are protected from physical, chemical and biological hazards. PART II, Section 3: How does CLIA Affect Biomedical Engineering? The pathologists, technologists, technicians and other scientists working in the clinical laboratory cannot meet the above stated standards without the expertise of biomedical engineering personnel. Laboratory workers do not have the proper education or training to achieve what the government requires of a good quality safety program. Therefore, the BME Department bears a considerable responsibility by helping the laboratory maintain its CLIA certification. BME assurance that electrical and safety systems are properly working is the keystone to successful operations in the clinical laboratory. Without sufficient and “clean” power and proper maintenance to the lab’s instruments and analyzers, the clinical laboratory simply cannot function. A partnership between the clinical lab and biomedical engineering is necessary to provide good quality patient care. Remember, CLIA is first and foremost a quality document. The Biomedical Engineering Department’s expertise is essential to maintaining the laboratory’s ability to provide quality results, therefore, it becomes inherent upon the BME Department to accept CLIA regulations are a part of their job responsibilities. Equally, it is inherent upon the laboratory or the administration of the healthcare facility to provide BME with the essential information and training to ensure the CLIA quality standards are met by both departments. June 2000 2 BMET Course Development IUPUI PART II, Section 4: Compliance Tips Let’s first begin this section by mentioning why we have safety regulations in the first place. Too often, safety standard compliance is pursued by healthcare workers in order to avoid deficiencies and possible fines and penalties by OSHA or other accrediting agencies. Safety regulations are really there to protect you, the worker. The OSHA General Duty regulations, including electrical safety, and other specific OSHA rules on matters such as Bloodborne Pathogens, Tuberculosis, Hazardous Materials in the Workplace, etc. have defined methods of protecting workers. Employers have the responsibility to provide you with the necessary training to protect yourself when your job duties require you to come in contact with dangerous materials or work in some other hazardous environment. As you are trained in these precautions, pay close attention on how to protect yourself in situations that may cause you to be exposed to hazardous conditions or substances. Following the safety rules you learn in training is the best way to protect yourself from harm in the workplace. Your responsibility as an employee is to follow the established safety rules. This often requires documentation in some manner. Your training should be documented. Various tasks you perform in the name of safety, such as checking laboratory analyzers for proper function, will require that you properly document your actions. This ensures safety for you as well as the laboratory worker who will operate the analyzer. Laboratory instruments or analyzers that develop problems require some documentation of the problem. This is followed by BME’s documentation of repairs. This will be followed by the laboratory’s documentation that the instrument or analyzer has returned to normal function. Regulatory inspectors follow this rule: If it isn’t written down, it didn’t happen. Follow your employer’s rules on documenting repairs. It really does contribute to ensuring a safe work environment for you and the laboratory workers. It also serves as a record of your commitment to safety. In 1990, OSHA’s Occupational Exposure to Bloodborne Pathogens Rule became effective. This rule is intended to require employers to protect workers from harmful bloodborne diseases such as Hepatitis A , Hepatitis B, Hepatitis C, and Acquired Immune Disorder Syndrome (AIDS). BME personnel need to be keenly aware of the danger that lies concealed in laboratory instruments and analyzers. Spatters or blood, body fluids or other potentially infectious materials can be present on or in these devices. It is essential to protect yourself from exposure to these dangerous materials when working on laboratory instruments. The laboratory should provide you with masks, eye protection, protective gloves, gowns or lab coats, and any other personal protective equipment to enable you to work safely on laboratory devices. June 2000 3 BMET Course Development IUPUI The laboratory instruments and analyzers generally have a some portion of it in contact with blood or other body fluid that may be potentially infectious. Please always remember this when working on these instruments. Protect yourself first. The benefit of using personal protective devices is that it protects you and those with whom you come in close contact and also maintains compliance with federal regulations. Obviously, the more important reason is that it protects you and the patients who are served by your healthcare facility. PART II, Section 5: The Most Common Lab Regulatory Deficiencies that Affect BME. Regulatory deficiencies can be narrowed to three general classes: 1) Failure to provide something essential; or 2) Failure to properly document something, like verifying the function of devices, the repair of devices, participation in training or education programs, etc.; and 3) Failure to correct a problem once it has been identified. Here are some common failures cited in laboratory inspections: 1. Failure to provide electrical power devices that prevent fluctuations and interruptions in electrical current. Where such devices do exist, failure to document proper function of these devices by regular testing. If problems are documented, failure to repair or replace the devices used to provide clean and steady power to lab instruments and analyzers. 2. Failure to provide adequate education and training programs to the workers who come in contact with known hazards in the workplace. Where such education and training occurs, failure to document the contents of the training and the dates the training occurred. Where training is provided, corrective actions must be established to retrain those individuals who fail to meet the criteria of the safety education program. 3. Some laboratory equipment is temperature controlled. In some analyzers, even temperature fluctuations of +/- 1 or 2 degrees can affect the accuracy of test results. A common deficiency is to document that proper operating temperature criteria are met. Further, if an onboard temperature monitor or thermometer is present, it must at least annually be checked against a known thermometer for accuracy. Failure to correct a known problem with temperature controlling equipment may also be cited as a deficiency. 4. Any observance of unsafe condition or behavior may be reported to the appropriate federal agency by a CLIA inspector. As representatives of the federal government, they are required by their job description to relay any violation or potential violation to OSHA, the EPA, State agencies, etc. This represents a broad spectrum of possible deficiencies and is a compliance tool that can be used by the inspectors. They have, and will report unsafe conditions they observe while evaluating laboratories. June 2000 4 BMET Course Development IUPUI PART II, Section 6: Resources 1) The Clinical Laboratory Improvement Amendments of 1988 (CLIA ’88); Title 42 (Public Health) of the Code of Federal Regulations (CFR) Part 493. 2) Appendix C: Survey Procedures and Interpretive Guidelines for Laboratories and Laboratory Services. Federal Document Number : PB-146174. 3) Web Site: http://www.cdc.gov/phppo/dls/42cfr493.htm 4) Healthcare Hazard Control and Safety Management. Tweedy, J.T., Lewis Publishers, 1997. June 2000 5