cp551-4
advertisement

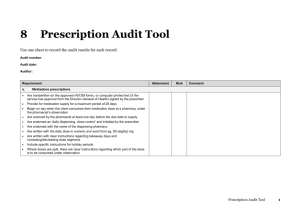
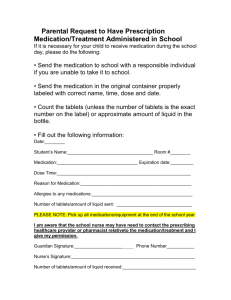
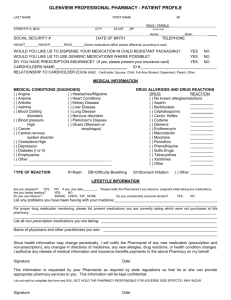
4. Medication Distribution Systems Background One of two methods of distribution was employed by pharmacy departments to deliver medications to patient care units (PCU): 1. Floorstock system: it was more commonly used method. In this system, the pharmacist dispensed bulk supplies of drug to the PCU, where nurses prepared all doses of medication (included the preparation of IV admixture) intended for administration to the patient. The medications sent were not labeled for a specific patient and the pharmacist saw only transcribed drug requisitions sent by nurses. 2. Patient prescription system: in this system, the physician wrote a prescription order, then, the nurse transcribed this order onto a medication administration profile and generated a drug order for pharmacy, the pharmacist dispensed a 2-5 day supply of medication and the nurse maintained the bottles in stock and used a reminder to determine doses’ time. In both systems the nursing personnel were responsible for most step of medication cycle. Thus, the pharmacist did not have the opportunity to effectively monitor drug therapy and influence optimal prescribing. The Unit Dose System It was designed and implemented in the middle 1960’s as a response to a perception that the pharmacist is educated and capable of providing professional services. The fundamental difference between the unit dose system (UD) and older, traditional distribution methods is the more active role of the pharmacist in the medication cycle with the patient reaping the benefits of a trained medication practitioner and return of the nurse to patient care responsibilities. This UD system enabled the pharmacist to review an actual copy of the physician medication order, oversee all medication preparation steps and maintain patient-specific drug profiles. Also, the pharmacist-physicians interactive role began to emerge as a direct result of this system. In addition, studies showed that the UD system is the most cost effective of all pharmacy distribution system. Unit Dose System Components The pharmacist reviews and edits an original copy of all medication orders written by the physician prior to dispensing medications. Next, a pharmacy technician prepares the medication needed during the forthcoming 24-hour period. Then, the pharmacist check each corresponding dose of medication prepared by the technician for accuracy and authorizes these medications to be delivered to PCU. After the physicians writes the chart order, all medication orders are transcribed by the nurse onto a 1 medication administration record (MAR). Before administering each dose, the nurse compares the medication label on the drug product with the appropriate MAR entry. The nurse then administers the dose to the patient and records the fulfillment of the order on the MAR. The physical concept of the unit dose distribution program is unit dose packaging, that is, the placement of each dose of medication into a separate package that bears a label listing drug name, strength or concentration, lot or batch number, and expiration date. The delivered medication to the PCU is securely stored on a unit dose medication administration cart (med cart). This lockable cart with its series of sliding drawers and removable trays can be accessed only by authorized personnel. It houses storage space for auxiliary supplies and a series of patient-labeled bins arranged in room and bed sequence. On a routine basis (usually once daily) at a predetermined time the replacement supply is taken to the PCU, the bins that held the previous day’s doses are returned to the pharmacy for new filling. Medication that are needed on demand or prior to the time of scheduled med cart must be delivered via different mechanism. They may be prompted via a newly written medication order or a written communication form. Unit dose distribution may be enhanced when selected stable medications are delivered to the PCU by placement of limited floorstock supplies. In addition, medications needed for code blue cases must be provided in preassembled emergency drug kits or trays to all PCU’s of the hospital. Unit Dose System Design The unit dose system is defined as one that includes clinical pharmacy services along with drug distribution activities; that is, the two components go hand in hand. If the scope is confined to drug distribution activities only, it may be classified as “a unit dose packaging and distribution program”. On the other hand, the unit dose system requires greater personnel resources, includes a higher level of job content for pharmacy staff, and has a greater impact upon the quality of medication therapy. Centralization Centralized unit dose services are generally provided from a single, self-contained location within the hospital. Centralization of services may be useful to hospitals with limited space, small size or vertical design with quick and easy access to all patient care areas. Centralization has the advantage of requiring a smaller technical and professional staff than that of decentralized services. Decentralization A decentralized unit dose distribution system operates from two or more dispensing locations commonly called “pharmacy satellites”. 2 Personnel Responsibilities Professional Staff The floorstock and patient prescription systems required nurses to perform many medication-related activities that are now the responsibility of pharmacists. The evolution of the unit dose system has dramatically changed the pharmacist’s responsibilities from simple, recurring mechanical duties to professional service responsibility for the hospital’s complete medication order cycle. As a result, the pharmacist has become a highly visible member of the healthcare team who is responsible for the quality of medication-related activities from the time of the drug is purchased to the time it is administered to patient, and to the assessment of outcomes of therapy. Pharmacy Technicians The technician performs most duties related to medication preparation and delivery, but the pharmacist supervises all work completed and ensures the integrity and safety of each dose dispensed. Because most of the time-consuming tasks of drug preparation have been delegated to technicians, the pharmacist has been freed to pursue the development and expansion of clinical pharmacy practice. Quality Assurance The activities performed in the course of medication preparations and distributions are routinely monitored using predetermined criteria to guarantee that assigned standards of performance are met. Quality assurance is used to evaluate the performance of several distributive activities, including: 1. unit dose med cart filling/checking 2. creating/updating patient medication profiles 3. prepackaging unit dose medication 4. compounding parenteral admixtures 5. reviewing medication administration records Routine monitoring of these activities identifies existing problems and allow pharmacist to take actions necessary to correct the problem. Productivity Monitoring It is a program to document all product and nonproduct contributions to patient care and monitor the total quantity of services that the pharmacy personnel provide. The data derived from these programs can be used to quantify the workforce necessary to serve each PCU and to reallocate resources to those areas of greatest need and subsequently enhance quality and efficiency. An example of such program is PharmaTrend® productivity monitoring system. 3