PCOS (POLYCYSTIC OVARY SYNDROME):
advertisement
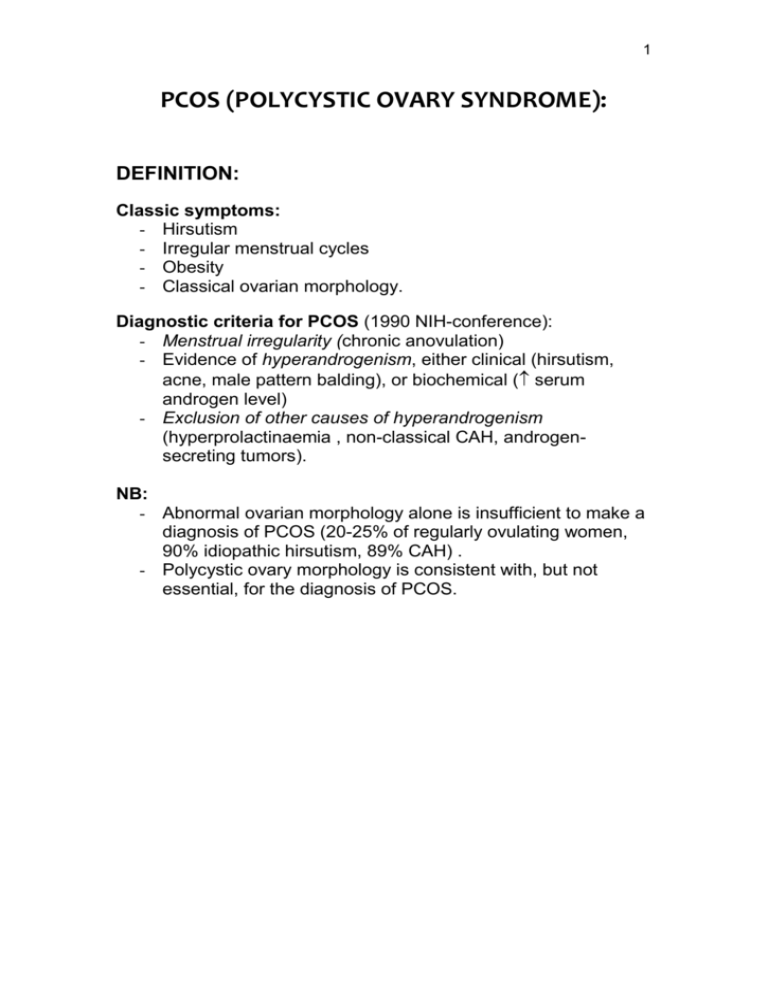
1 PCOS (POLYCYSTIC OVARY SYNDROME): DEFINITION: Classic symptoms: - Hirsutism - Irregular menstrual cycles - Obesity - Classical ovarian morphology. Diagnostic criteria for PCOS (1990 NIH-conference): - Menstrual irregularity (chronic anovulation) - Evidence of hyperandrogenism, either clinical (hirsutism, acne, male pattern balding), or biochemical ( serum androgen level) - Exclusion of other causes of hyperandrogenism (hyperprolactinaemia , non-classical CAH, androgensecreting tumors). NB: - Abnormal ovarian morphology alone is insufficient to make a diagnosis of PCOS (20-25% of regularly ovulating women, 90% idiopathic hirsutism, 89% CAH) . - Polycystic ovary morphology is consistent with, but not essential, for the diagnosis of PCOS. 2 PATHOPHYSIOLOGY: 3 major hypotheses: - LH hypothesis: Primary neuroendocrine defect leading to exaggerated LH pulse frequency and amplitude resulting in ovarian hyperandrogenism. - Ovarian hypothesis: A primary defect of sex steroid synthesis or metabolism results in exaggerated ovarian (adrenal) androgen secretion and anovulation. - Insulin hypothesis: A unique defect in insulin action leading to hyperinsulinemia resulting in excess androgen secretion (augmentation of LH stimulation of ovarian androgen production) and anovulation. Interrelationship between abnormalities: - Multiple pathophysiologic defects described as a selfamplifying circle. - Still impossible to determine primary etiologic factor. 3 LH hypothesis (Neuroendocrine aspects of PCOS): Observations: LH (baseline/post-GnRH stimulation), normal FSH, LH/FSH ratio (> 2.5) (75% of PCOS) Rapid GnRH pulse frequency favouring acyclic LH release: possible mechanisms ( sensitivity of GnRH secretion to inhibition by ovarian steroids): - Neurotransmitters: Dopamine and endorphins are inhibitory to GnRH release. - Estrogens: o Early “estrone hypothesis”: peripheral aromatisation of androstenedione estrone pituitary LH secretion. o Current evidence does not support a role for persistent elevations of estrone in enhancing GnRH pulsatile secretion, although a role in reducing FSH responses to GnRH has been established. - Androgens: o Although not conclusive, several studies suggest that excess androgen exposure (prenatal/ prepubertal) may modify subsequent regulation of hypothalamic GnRH release. - Insulin: o Although not conclusive, several studies suggest that hyperinsulinemia could enhance GnRH secretion or pituitary responses to GnRH or both. o Supported by reduction in LH after metformin or troglitazone. - Estrogen-progesterone feedback: o Anovulation and absence of luteinization progesterone levels negative feedback (hypothalamic/pituitary). 4 Ovarian hypothesis (Defective steroid synthesis/ metabolism): Figure 1: Steroid biosynthesis in adrenal cortex. Figure 2: Two-cell model of ovarian steroidogenesis. 5 Generalised dysregulation (ovarian and adrenal) of steroid biosynthesis and metabolism. - Dysregulation of 17-hydroxylase and 17,20-lyase activities, both properties of P450c17 (rate-limiting enzyme in androgen biosynthesis) activity. - Results in functional ovarian hyperandrogenism (70% of PCOS) and/or adrenal hyperandrogenism (50% of PCOS). - P450c17 gene expression is normally dependent on the concentration of the respective trophic hormones (LH in the ovary, ACTH in the adrenal cortex). - The steroidogenic response to trophic hormones is modulated by a multitude of intrinsic (autocrine/paracrine) / extrinsic (eg insulin, IGFs) regulatory mechanisms – more important in women. - Functional ovarian hyperandrogenism: o Characterised by: 17-OH progesterone secretion in response to GnRH agonist/HCG stimulation and failure of dexamethasone suppression of free testosterone (in presence of normal adrenocortical suppression). o Ovarian hyperresponsiveness to LH - escape of thecal cells from normal downregulation in response to increasing LH (? Insulin excess) o Intensified by LH excess. - Functional adrenal hyperandrogenism: o Characterised by: moderately increased secretion of 17-ketosteroid DHEA in response to ACTH (glucocorticoid-suppressible). o Possible role for insulin excess. - Disturbed peripheral steroid metabolism: o Accelerated cortisol turnover ACTH secretion adrenocortical activity Dysregulation of 11-hydroxysteroid dehydrogenase ( cortisol cortisone, urinary excretion of cortisol metabolites, ratio of 11-keto/11-hydroxy metabolites). Enhanced activity of 5-reductase (in liver) ( hepatic cortisol metabolism, total urinary cortisol metabolites, ratio of 5/5metabolites). 6 o Enhanced activity of 5-reductase (in skin) results in DHT levels (active/more androgenic). o Obesity contributes to androgen excess by formation of estrogen and testosterone from inactive precursors. Figure 3: Some principal pathways for cortisol metabolism. Figure 4: Model of factors causing functional hyperandrogenism. 7 Insulin hypothesis: First report of association of hyperinsulinemia / insulin resistance and PCOS in 1980. Figure 5: Molecular mechanisms of insulin action. Figure 6:Molecular mechanisms of insulin resistance in PCOS. 8 Hypotheses explaining the association of insulin resistance and PCOS: Causal association: - Do androgens cause insulin resistance? o Androgens may produce mild insulin resistance ( less insulin-sensitive type IIb skeletal muscle fibres, muscle glycogen synthase). o Modest hyperandrogenism of PCOS may contribute to insulin resistance, but additional factors are necessary to explain the insulin resistance because suppressing androgen levels does not completely restore normal insulin sensitivity. - Does hyperinsuliemia cause hyperandrogenism? o Hyperinsulinemia augments androgen production in PCOS: Dysregulation of P450c17 Decreased hepatic production of SHBG. o Intrinsic abnormalities in steroidogenesis seem necessary for this insulin action to be manifested ( insulin levels: no affect on circulating androgen levels in normal women, ameliorates but does not abolish hyperandrogenism in PCOS). o Insulin has specific actions on steroidogenesis acting through the insulin receptor. These actions seem to be preserved when there is resistance to insulin action on carbohydrate metabolism – selective defects in signalling pathways regulating carbohydrate metabolism. Possible genetic association of PCOS and insulin resistance: - Serine phosphorylation of P450c17 increases its 17,20lyase activity. - Insulin resistance in PCOS appears to be secondary to serine phosphorylation of the insulin receptor. - Protein kinase A has been shown to serine phosphorylate both in vitro. - It is postulated that one or several genetic defects may cause both the insulin resistance and reproductive abnormalities of PCOS. 9 BIOCHEMICAL ABNORMALITIES/ LABORATORY DIAGNOSIS: Laboratory diagnosis of PCOS is one of exclusion. HORMONE PROFILE: In PCOS: - Estrogen: N follicular levels (> 150 pmol/l) (mainly from peripheral conversion) - Progesterone: - LH: - FSH: disproportionally N/ - LH/FSH ratio > 2.5 (75% of PCOS) (* also CAH) ANDROGENS: DHEAS: Adrenal origin Testosterone: Ovarian/adrenal origin In PCOS: - S-Total testosterone: modestly (< 5.2 nmol/l)/ normal (due to SHBG). - Free testosterone: - higher diagnostic yield - DHEAS: N/slightly . Exclusion of androgen-producing tumors: Consider if: - Total testosterone > 200 ng/dl (6.9 nmol/l) - DHEAS > 700ug/dl (19 umol/l) 17-OH PROGESTERONE (follicular phase): Exclusion of non-classical/late onset CAH: - < 6 nmol/l: Excludes CAH - > 30 nmol/l: Confirms CAH - 6.9-45 nmol/l: ACTH stimulation test (follicular phase): o CAH: 60 min > 30 nmol/l o * PCOS: basal and stimulated 17-OHP, but normal incremental change (17-OHP 30-0). URINE STEROID PROFILE (follicular phase): Distinguish between CAH and PCOS: PCOS: - total urinary cortisol metabolites - 5/5-metabolites CAH: - urinary cortisol metabolites - cortisol precursors eg pregnanetriol. 10 PROLACTIN/TSH: - Exclusion of prolactinoma (Prolactin > 200 ug/l). - 35% of PCOS patients have slightly prolactin (lactotroph stimulation by chronic estrogen). - Coexistence of prolactinoma + PCOS uncommon. - Abnormal thyroid function (/) associated with menstrual irregularities. ASSOCIATED BIOCHEMICAL ABNORMALITIES: HYPERINSULINEMIA / INSULIN RESISTANCE: Important to diagnose for institution of preventive strategies (diet, exercise, insulin-sensitizing agents): - Mild form: slightly fasting insulin - Ratio of fasting glucose/insulin (G in mg/dl, Insulin in mIU/l) < 4.5: sensitive/specific marker in obese PCOS IGT / DM: All PCOS (obese/non-obese) have risk (3x) for IGT/DM. Screening with OGTT: - Obese women before pregnancy is attempted. - All PCOS after 40 y of age. ALTERED SERUM LIPID PROFILE AND IMPAIRED FIBRINOLYSIS: Lipid abnormalities: - Total Chol - LDL-Chol - TGS - HDL-Chol / Apo A-I (most characteristic) Impaired fibrinolytic activity: - PAI-1 Screening with fasting lipogram: - All PCOS at 35 y of age - If normal: repeat every 3-5 years Women with PCOS have an estimated 7x increased risk for MI. 11 DIFFERENTIAL DIAGNOSIS: Table 1: Differential diagnosis of hyperandrogenism and menstrual irregularity. 12 PCOS PATHOPHYSIOLOGY: Combination of abnormal ovarian steroidogenesis / LH / hyperinsulinemia CLINICAL: Irregular menses (anovulation) Gradual onset of mild hirsutism Onset at/soon after puberty Obesity BIOCHEMICAL: Test (< 5.2 nmol/l) N/slight DHEAS LH/FSH ratio (> 2.5) N Estrogen Progesterone Ovarian hyperthecosis Non-classical CAH Cushing’s syndrome Androgenproducing neoplasms Abnormal proliferation of luteineised theca cells, hypersensitive to gonadotropin stimulation 21-hydroxylase deficiency (90%) Cortisol overproduction (ACTH-dependent/ independent) Ovarian or adrenal tumors Enlarged firm ovaries Severe hirsutism of gradual onset Virilisation(clitoromegaly) Obesity Acanthosis nigricans Resistant to contraceptive therapy Regular menses Mild -severe hirsutism of early onset Premature adrenarche Virilisation (clitoromegaly) Short stature Familial tendency Hirsutism Obesity Menstrual irregularity Moonlike facies Buffalo hump Hypertension Abdominal striae Osteoporosis/muscle wasting Severe hirsutism of rapid onset (within months) Virilisation(clitoromegaly) Male body habitus Palpable pelvic/abdominal mass Test / DHEAS LH/FSH low N / Estrone Insulin resist ( Ins) 17-OH progesterone DHEAS/ DHEAS (>700ug/dl/ (> 45 nmol/l) DHEAS / androstenedione Test N/ LH/FSH ratio 19 umol/l) Testosterone (> 200 ng/dl/6.9 nmol/l) May be associated with Progesterone/cortisol androstenedione Test (> 5.2 nmol/l) U-Free cortisol N/ ACTH 13 PCOS Ovarian hyperthecosis PELVIC ULTRASOUND: Polycystic ovaries (8-10 Bilateral noncystic peripheral <8mm enlargement follicles, stroma) (80-100%) Endometrial hyperplasia OTHER IMAGING STUDIES: Non-classical CAH Cushing’s syndrome Androgenproducing neoplasms Polycystic ovaries (80%) Normal ovaries Suspected ovarian tumor Abdominal CT/MR for suspected adrenal tumor Abdominal CT/MR if suspected adrenal tumor ( DHEAS) REFERENCES: 1. Taylor AE. Polycystic ovary syndrome. Endocrinology and Metabolism Clinics of North America 1998 Dec; 27(4): 877-902. 2. Logo RA, Carmina E. The importance of diagnosing the polycystic ovary syndrome. Ann Intern Med 2000 June; 132(12): 989-993.