AN “AVOIDABILITY TEST” AS A POTENTIAL TEST FOR ELIGIBILITY
advertisement

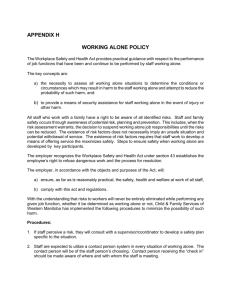
MRG Paper 24 MRG 7 Agenda Item 5 AN “AVOIDABILITY TEST” AS A POTENTIAL TEST FOR ELIGIBILITY TO COMPENSATION IN ‘NO-FAULT’ OR OTHER ADMINISTRATIVE SCHEMES Introduction The no-fault compensation working group has agreed to look at different eligibility criteria that could be used in a potential ‘no-fault’ compensation scheme, or other schemes as an alternative to medical negligence litigation when harm has resulted from medical treatment or failure to treat. We know from the research already carried out that such schemes, whilst referred to as ‘no-fault’ schemes apply certain qualifying criteria, even though there is not a need to prove legal liability. This short paper will discuss the potential merits or otherwise of the development of an “avoidability test” to establish eligibility for compensation in any potential scheme in Scotland, with reference to approaches adopted elsewhere. Action against Medical Accidents (AvMA), have considered alternatives over the years and in particular in response to the Chief Medical Officer for England’s, (Sir Liam Donaldson’s), request in Making Amends (2003) for suggestions for an alternative to the ‘Bolam test’ for negligence. The concept of an “avoidability test” is the charity’s preferred option. The ‘Avoidability Test’ There are different variations of an ‘avoidabilty test’ already being used in existing so-called ‘no-fault’ compensation schemes, or which are under discussion. For example, the schemes in Denmark, Finland and Sweden use a form of ‘avoidability rule ’ to determine eligibility for compensation under their schemes. (See researchers’ interim report). In the Nordic countries’ schemes the trend is to consider whether the harm would have been avoided by the use of ‘best’ practice. However, there are other criteria which also come into play when determining eligibility for the schemes which may significantly limit what would otherwise be very wide access to compensation. In the USA, there have been calls for a system of ‘health courts’ to determine which medical cases should be eligible for compensation, as an alternative to litigation. President Obama was recently reported as being in favour of such reforms. It has been proposed that the health courts would use an avoidability test to determine eligibility. See the attached article by Mello et al (Harvard Medical School, 2006) which provides a useful insight both into the arguments for use of a avoidability test and for health courts as an administrative alternative to litigation. Again, the definition of avoidability offered by the authors centres on avoidability if the ‘best practice’ was followed. AvMA have proposed another alternative to the ‘best practice’ kind of avoidability test. This test incorporates the concept of ‘patient safety incidents’. (Simply replace ‘patient safety incident’ with ‘adverse event’ if that remains the preferred terminology in Scotland). “Patient safety incidents” are defined by the National Patient Safety Agency (NPSA) as “any unintended or unexpected incident which could have, or did, lead to harm for one or more MRG Paper 24 MRG 7 Agenda Item 5 patients receiving NHS-funded healthcare”. In other words, they include ‘near misses’ as well as incidents which led to harm to a patient. For the purposes of this discussion, we are only concerned with where incidents have led to harm. The setting could also apply just as much to private treatment as NHS funded care. NPSA also define levels of harm as follows: ‘Low’: (Minimal harm - patient(s) required extra observation or minor treatment); ‘Moderate’: (Short term harm - patient(s) required further treatment, or procedure); ‘Severe’: (Permanent or long term harm);‘Death’: (Caused by the Patient Safety Incident). Under AvMA’s avoidability test cases where there has been a “patient safety incident” resulting in harm to the patient, the criterion to determine eligibility for compensation and/or other forms of redress would be: “A patient safety incident resulting in harm to the patient is compensable except where it is the result of an unavoidable complication which would have arisen regardless of treatment or non-treatment “ AvMA believes the use of an avoidability test to determine eligibility for compensation has significant advantages. For example: It encourages a culture of patient safety and learning from incidents so as to help avoid them. Every incident being considered for compensation would also be investigated asking the questions “Could we have avoided this, and if so how do we make sure we do in the future?” Whereas, the litigation system forces the healthcare provider to ask itself the question “Is there a credible defence that can be mounted to this claim”. It moves away from the blame culture/focus on pinning blame on individual health professionals which is considered a hindrance to improving patient safety and to openness and honesty when things go wrong It focuses on root causes and systems issues, meaning that one investigation should result in the answers needed to help improve patient safety as well as to whether or not someone deserves redress, avoiding multiple investigations with different aims. It is fairer. Most people would agree that someone who has suffered avoidable harm in healthcare should be entitled to redress, and that if something has gone wrong and harm is the result, the onus should be on the healthcare provider to prove that the harm was unavoidable (if that is what they believe). In litigation, all the burdon of proof, including ‘causation’, rests on the claimant. It would drive quality improvement by making the acceptable standard of practice the avoidance of avoidable harm rather than practice which is not so bad as to be categorised as ‘negligent’ MRG Paper 24 MRG 7 Agenda Item 5 AvMA’s version potentially has further advantages in that it uses phraseology / definitions (‘patient safety incident’ or ‘adverse event’) which are currently used in Scotland and other parts of the UK. This would make it simpler to identify cases which should be considered for compensation under any scheme and to align the scheme with existing work on patient safety. It is a matter for debate, should the concept of an avoidability test of some kind find favour at all, whether the ‘best practice’ and ‘experienced practitioner’ criteria in use in Nordic schemes or the AvMA model is most appropriate. Another issue is whether any additional qualifying criteria should apply, such as seriousness of harm caused. If this were to be the case, the levels of harm under the definition of ‘patient safety incident’ above might be used. Peter Walsh, March 2010.