3. THE CASE AGAINST IgG AND FOOD SENSITIVITY IN CHRONIC
advertisement

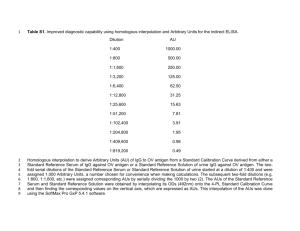
1 10. The Role of IgG and Food Sensitivity in Chronic Disease © 1999 - Do Not Reproduce Without Authorized Permission This independent literature review was carried out between the dates of 01/09/99 and 09/10/99 by Alison Mathery B.Sc. (Hons) Biochemistry, Ph.D. Immunology (submission in process). CONTENTS SECTION 1. SUMMARY PAGE . . . . . . . . . . . . . . . 1 . . . . . . . . . . . . . . 2 3. THE CASE AGAINST IgG AND FOOD SENSITIVITY IN CHRONIC DISEASE . . 3 4. THE CASE FOR IgG AND FOOD SENSITIVITY IN CHRONIC DISEASE . . . 4 2. INTRODUCTION 4.1 INDEPENDENT BEHAVIOUR OF FOOD SPECIFIC IgG . . . . . 4 4.2 COW’S MILK SENSITIVITY . . . . . . . . . . . 5 4.3 ECZEMA . . . . . . . . . . . 6 4.4 FOOD SENSITIVITY IN ATOPY . . . . . . . . . . 7 4.5 INFLAMMATORY BOWEL DISEASE . . . . . . . . . 8 4.6 IRRITABLE BOWEL SYNDROME . . . . . . . . . . 9 4.7 MIGRAINE . . . . . . . . . . . . . . . . 10 4.8 RHEUMATOID ARTHRITIS . . . . . . . . . . . 11 5 CONCLUSIONS . . . . . . . . . . . . 11 6 APPENDIX I (search strategy) . . . . . . . . . . . . 13 7 REFERENCES . . . . . . . .. . . . . 14 . . . . . . . . 2 1. SUMMARY YNL have developed an ELISA to detect food specific IgG in the serum of individuals with suspected food sensitivity. They have good testimonial evidence that shows that the dietary modifications suggested by the ELISA results are very successful in providing symptomatic relief from a variety of chronic conditions. The scientific literature world-wide was reviewed to find evidence for and against the role of IgG in food sensitivity. The review revealed evidence to support the view that food specific IgG may indeed serve as a useful diagnostic marker for food sensitivity related to chronic disease. However its role in the pathogenesis of these disease conditions is less clear. The occurrence of raised levels of IgG in food sensitive individuals, and their decrease when the offending food is removed from the diet, provides strong circumstantial evidence for the involvement of IgG in food sensitivities. This view is further supported when the elimination of offending foods also results in symptomatic improvement. Well designed clinical trials will be necessary to provide more convincing evidence for the role of food specific IgG in chronic disease. YNL is currently undertaking such studies. 2. INTRODUCTION Over the past 2 years YNL Ltd have been conducting tests to detect raised IgG antibodies for food sensitivities. The test is an enzyme linked immunoassay or ELISA method consisting of a panel of food antigens, the pattern of serum IgG reactivities against these antigens is used to identify an individual programme of dietary modifications. They have evidence that the dietary modifications suggested are successful in providing symptomatic relief from a wide range of chronic illnesses. The identification of food 3 sensitivities via this method is much easier and far more convenient for both patient and clinician than challenge/elimination diets. Until recently, a medically extracted blood sample was required for testing, now method for all parties involved as the laboratory not only returns the results of the clinical test, but also individual dietary modifications for each patient. The role of IgE in adverse reactions to food is much more clearly defined than non-IgE responses, so the associated diagnostic testing traditionally involves the detection of IgE antibodies by skin prick tests and food challenge/elimination diets, (Salkie 1994). The skin tests are not well correlated with food allergens and are only diagnostic of IgE-mediated responses. The challenge/elimination diets are time consuming and rely heavily on the patient for both motivation and compliance, (Miller 1998). The theory behind testing for elevated levels of food specific IgG in the diagnosis of food sensitivities comes from the evidence that reports raised IgG titres in the serum of atopic individuals. Early studies show that IgE is not always detected in the sera of individuals who give an inflammatory response after skin pricking tests, however in many of these sera, IgG is observed, (Parish 1970 and Berry 1977). Significantly elevated levels of IgG have also been observed in the serum of individuals with certain food sensitivities (Shiner et al 1975, Dannaeus et al 1977, Berrens et al 1981, Dannaeus & Inganas 1981, Daul et al 1987, Burks et al 1988, Lilja et al 1991, Host et al 1992 and Germano et al 1993). Adverse reactions to food can cause a range of symptoms throughout the body, which are thought to be immunologically or non-immunologically mediated. The two immunologically related responses differ in that food allergy (IgE mediated) usually occurs within 1 hour of ingestion and results in a variety of symptoms involving the skin, gastrointestinal tract (GIT) and lungs. Food sensitivity (elevated food specific IgG levels often observed) involves a delayed reaction, usually occurring between 24 to 120 hours after eating and is more of a recurrent/ongoing response. The symptoms are more generalised and may include bloatedness, cramps, nausea, rashes, migraine and general malaise. 4 The GIT contains the largest surface area of mucosal lymphoid tissue of any organ in the body; therefore it is the obvious choice for major antigen sensing and antibody production. The food antigens are sampled from the contents of the GIT by immune mediators, which are capable of recognising most of the food antigens; thus an individual is routinely sensitised to many of the foods ingested. An immune reaction in the GIT will induce an inflammatory response, leading to increased GIT permeability and demonstration of the associated symptoms of heartburn, nausea and vomiting. The increased permeability of the GIT allows incompletely digested food to enter the bloodstream and is then treated as a pathogen to be recognised by circulating antibodies, leading to the symptoms of other organs mentioned. This continual stress will eventually cause the immune system to weaken, leaving the individual much more susceptible to illness. Functional experiments have provided evidence of a pathogenic role for IgG as well as IgE in food sensitivities. IgE mediated histamine release is well documented, but other studies have shown that IgG may also be involved, (Hindocha & Wood 1985 and Beauvais et al 1990). A study looking at the passive transfer of milk sensitivity to non-sensitised guinea pig epithelium demonstrated an involvement of IgG and not IgE, (Baird et al 1987). One study has shown that IgG directed antibody dependent cell mediated cytotoxicity (mechanism where antibodies interact with cytotoxic cells) may be of pathogenic importance in certain diseases associated with adverse GIT symptoms in cow’s milk protein sensitive individuals. Sera from children with GIT symptoms as oppose to coeliacs patients was shown to efficiently mediate ADCC to cells coated with -lactoglobulin. capacity. Deliberate depletion of IgG 1, 3 and 4 caused a marked decrease in ADCC mediating Thus IgG is of pathogenic importance in cow’s milk protein sensitive patients with GIT symptoms, (Saalman 1995). As the theory behind testing is unclear and the reliability and validity of the test has not been fully evaluated, this methodology is still argued against in terms of diagnostic value. Therefore, it is the aim of this review to present evidence and key arguments in support of a role for IgG in food sensitivity. 3. THE CASE AGAINST IgG AND FOOD SENSITIVITY IN CHRONIC DISEASE Many studies have reported food specific IgG in the serum of normal subjects, this review cites a few 5 examples. Food specific IgG containing immune complexes were observed in adult and children non-atopics, (Haddad et al 1983, Paganelli et al 1983, and Lessof & Kemeny 1991). in healthy subjects (Husby et al 1985 and Kruszewski et al 1994). Food specific IgG has been observed It has been demonstrated by ELISA that the levels of food specific IgG in control subjects and food sensitive patients were not significantly different, (Portnoy et al 1988 and Burks et al 1989 and 1990). Specific IgG was significantly raised in shrimp sensitive individuals, but the IgG response was not significantly predictive of an adverse reaction to food challenge (Morgan et al 1990). It has been demonstrated that food specific IgG levels don’t seem to be predictive of certain diseases such as inflammatory bowel disease and eczema, (Zvetckenbaum 1988 and Sloper et al 1991). 4. THE CASE FOR IgG AND FOOD SENSITIVITY IN CHRONIC DISEASE Although elevated levels of food specific IgG seems to be a good marker of food sensitivities, the exact role played by IgG remains unclear. There is however considerable evidence that argues in favour of the involvement of food specific IgG in individuals who suffer from adverse reactions to foods. This includes the demonstration of an independent behaviour of food specific IgG compared to IgE in food sensitive individuals and the observation of elevated levels of food specific IgG in various diseases. A search of the relevant literature associated with food sensitivity reveals evidence supporting a role for food specific IgG in the pathogenesis of various diseases and ailments. Probably the most common is a general sensitivity to cow’s milk producing various symptoms including those associated with the GIT, respiratory tract and the skin. 4.1 INDEPENDENT BEHAVIOUR OF FOOD SPECIFIC IgG In many individuals who suffer from an immunologically related adverse reaction to food, the food specific IgG behaves independently of the IgE, suggesting that there is more than one immunopathogenic mechanism involved, (Brighton 1980). In orally challenged food sensitive individuals two components of the complement pathway were utilised in the specific immune response, the IgE levels were unchanged from normal, suggesting IgG may have triggered complement leading to inflammation, and the adverse effects, (Trevino et al 1981). Sera from eczema patients contained high levels of milk specific IgG, A and E whereas cow’s milk allergy patients had high levels of 6 IgE only, indicating two possible different pathogenic mechanisms, IgE mediated mast cell degranulation and the eczema skin lesions were probably the result of chronic antigen exposure, leading to immune complex deposition and local inflammatory response in the skin, (Firer et al 1982). In egg allergic individuals, elevated ovalbumin specific IgG showed no relationship with IgE and in some patients IgG was observed in the absence of IgE, (Nakagawa 1986). Individuals with late onset food allergies of the skin, respiratory tract and GIT mostly had elevated IgG compared with IgE and in some a food induced IgE response was absent altogether, (el Rafei et al 1989). In food allergic children, 77% had elevated IgG and only 37% had IgE, in non-allergic individuals there was no response. Elimination and re-introduction of offending food lead to remission and relapse of symptoms respectively, (Hoffman 1995). These particular studies emphasise that elevated food specific IgE is not always involved in adverse reactions to food, as there is evidence of a high occurrence of elevated IgG in association with symptomology this suggests that there are at least two immunological mechanisms involved in the pathogenesis of food sensitivity. 4.2 COW’S MILK SENSITIVITY An infant with anaemia and chronic bronchitis associated with cow’s milk showed elevated levels of cow’s milk specific IgG measured by ELISA. When milk was removed from the diet there was symptomatic improvement and a decrease in cow’s milk IgG was observed in the absence of IgE. The investigators hypothesised that the initial formula feeding sensitised the infant to cow’s milk protein, which caused a slight intestinal illness leading to increased gut permeability and when whole cow’s milk was introduced into the diet a marked immune response involving IgG occurred, (Cohen et al 1985). It has been demonstrated that anti- -lactoglobulin IgG correlates well with delayed onset cow’s milk sensitivity and that antibodies against -lactoglobulin may be useful in the diagnosis of cow’s milk protein sensitivity, (Fallstrom et al 1986 and Shakib et al 1986). Significantly higher -lactoglobulin IgG were observed in infants with persistent cow’s milk allergy, (Host et al 1992). In children from atopic families, elevated levels of cow’s milk specific IgG was detected by enzyme 7 immunoassay. The ingestion of milk caused significant increases in milk specific IgG in the patients with sensitivity to cow’s milk, (Hamburger et al 1987). In a later study an ELISA designed to detect cow’s milk protein specific IgG revealed the presence of milk specific IgG in the serum of cow’s milk protein sensitive children. The levels of IgG were significantly higher than those found in control individuals, which consisted of those with ‘toddler diarrhoea’, atopic individuals and normal healthy subjects. The ELISA was highly sensitive and specific for the diagnosis of cow’s milk protein sensitivity when differentiating between that and general infant diarrhoea, (Taylor et al 1988). When anti- -lactoglobulin IgG levels were measured by an enzyme immunoassay, marked differences in IgG levels were apparent in cow’s milk protein sensitive individuals compared with healthy controls and those with GIT symptoms not associated with food sensitivity. The investigators stated that the enzyme immunoassay test could be used to confirm the diagnosis of cow’s milk protein sensitivity, (Iacona et al 1995). Patients with gastroesophageal reflux (GER) plus cow’s milk sensitivity were significantly positive for anti- -lactoglobulin IgG compared with those with GER only, suggesting that tests that detect elevated anti- -lactoglobulin IgG are specific and sensitive methods for the diagnosis of GER with cow’s milk sensitivity, (Cavataio et al 1996). It has been shown that preferential recognition of some epitopes of an antigen can be observed for IgG in children with cow’s milk sensitivity. Specific anti- -lactoglobulin IgG specificity to native and pepsin -lactoglobulin was measured by ELISA. In cow’s milk sensitive individuals there was significant -lactoglobulin, in the controls there was no difference in -lactoglobulin was significantly higher in the sensitives -lactoglobulin specific IgG declined with elimination of milk from the diet, this was not the case for the healthy controls where the low-level IgG was independent of milk consumption. The direct relationship between levels of anti- -lactoglobulin IgG and the success of elimination of milk demonstrated that milk specific IgG is a useful indicator of food sensitivities, which may be used in dietary modifications, (Duchateau et al 1998). 8 4.3 ECZEMA Eczema is a group of skin conditions in which the severity of the disease can vary, in mild forms the skin is dry, hot and itchy, whilst in more severe forms the skin can become broken, raw and bleeding. With treatment the inflammation of eczema can be reduced, though the skin will always be sensitive to flare-ups and need extra care. The causes of eczema are many and varied, and depend on the particular type of eczema that a person has. Atopic eczema is thought to be a hereditary condition, being genetically linked. It is proposed that people with atopic eczema are sensitive to allergens in the environment which are harmless to others. In atopy there is an excessive reaction by the immune system producing inflamed, irritated and sore skin. Associated atopic conditions include asthma and hayfever. Other types of eczema are caused by irritants such as chemicals and detergents, allergens such as nickel, and yeast growths. In later years eczema can be caused by a blood circulatory problems in the legs. The causes of certain types of eczema remain to be explained, though links with environmental factors and stress are being explored. It has been demonstrated that milk specific IgG is elevated in some children with milk inducing eczema and some milk sensitive children without eczema have no IgG response. This points towards the fact that in milk related eczema the milk specific IgG may be involved in the pathogenic mechanism of the disease via immune complex deposition, (Firer 1982). Milk specific IgG was found in much higher levels in patients with food inducing eczema compared with controls. However, this phenomenon was not observed with egg specific IgG, but the controls used in this study included just two healthy adults and the rest were children who had been referred to the hospital for apparently non-atopic disorders, (Shakib et al 1984). protein sensitive eczema patients, an ELISA showed elevated IgG to - In cow’s milk -lactalbumin, and -casein for all subclasses in these patients compared with the control subjects, (Shakib et al 1986). -lactoglobulin in atopic eczema patients compared with healthy subjects, (Husby et al 1989). In patients with atopic eczema, significant increases in IgG levels were observed with milk ingestion and the investigators concluded that IgG should be considered when eliminating offending foods, (Iikura et al 1989). IgG against egg white, egg yolk and Significantly elevated levels of -lactoglobulin were reported in the sera of atopic eczema patients 9 compared with controls, (Garcia et al 1990). In children with atopic eczema and GIT symptoms associated with food ingestion, IgG for casein was significantly elevated, the investigators concluded that IgG is useful in the diagnostic work-up, particularly in children with GIT symptoms, (Lucarelli et al 1998). From these studies it seems that elevated milk specific IgG plays an important role in the development of some forms of eczema/dermatitis and in some cases a diagnosis can be made by elevated IgG subclasses to cow’s milk proteins. 4.4 FOOD SENITIVITY IN ATOPY Elevated levels of IgG have also been described in other atopic and allergic individuals. In patients with various allergic related symptoms, elimination of food that gave a positive IgG RAST test, resulted in a 70% reduction of symptoms. This suggests that detection of elevated food specific IgG may be helpful in the diagnosis of food sensitivity related diseases, (Dockhorn 1987). In patients with food induced allergies manifested in the skin, respiratory tract and GIT, late onset allergies showed a greater IgG response compared with IgE and in some patients the IgE response was completely absent. histories matched the IgG4response, (el Rafei et al 1989). In most of these patients, the clinical In bakers with adverse reactions to wheat flour, levels of specific IgG by enzyme immunoassay were significantly higher than those with no adverse reactions, (Tiikkainen & Klockars 1990). In patients with general food sensitivities, the IgG titres by enzyme immunoassay, which far exceeded the IgE levels measured by RAST tended to correlate well with patient history and symptomology, (Berrens & Homedes 1991). In atopic individuals with egg allergy over 5 years old, elevated levels of ovalbumin specific IgG were observed compared with non-egg allergic atopic patients, (Nakagawa et al 1986). In a study that monitored patients whilst on an elimination diet based on previous food specific IgG positivity, there was a significant correlation in decrease of food specific IgG levels. The patients were also much improved in their clinical symptoms, supporting the value of IgG determination to foods as a helpful tool to reduce illness, ( Marinkovich 1996). In soybean intolerants, most of the proteins giving a high IgG response differed from the proteins giving an IgE response in the same ailments, again suggesting that another immune mechanism involving IgG is 10 occurring. The frequency of soybean specific IgG was high in infants and in the latter stages of infancy it was low, suggesting that IgG is suppressed in normal individuals and if this mechanism is altered it may have an adverse effect, thus suggesting a role for IgG in the pathogenesis of food sensitivity in these individuals, (Awazuhara et al 1997). 4.5 INFLAMMATORY BOWEL DISEASE Inflammatory bowel disease is a chronic disorder causing inflammation or ulceration in the small and large intestines, the cause is unknown. and ulcerative colitis. There are two main types of inflammatory bowel disease: Crohn's disease In Crohn's disease, the wall of the intestine becomes sore, inflamed, and swollen. Ulcerative colitis is a condition that causes tiny sores to form in the inner lining of the colon and rectum. Crohn's disease and ulcerative colitis have similar symptoms: abdominal pain and cramps, diarrhoea, and rectal bleeding and/or bloody stools. Also common are pain in the joints, lack of appetite, weight loss, and fever. There is no test to identify the disease and diagnosis is usually based on a medical history, a physical exam, and blood tests. In addition, patients often undergo barium X-rays of the upper and lower gastrointestinal tract, as well as endoscopic procedures allowing examination of the colon and rectum through a lighted instrument inserted through the anus. Treatment involves minor adjustments to the diet (for example, a decrease in fat, fiber, and lactose) sometimes help in decreasing symptoms, but a specially tailored diet plan may be necessary. A number of medications are used to treat inflammatory bowel disease, including anti-inflammatory drugs and antibiotics for local infections. The responses to dietary antigens have been implicated as playing a role in inflammatory bowel disease (IBD). In patients with food induced enterocolitis, the antigen specific IgG response to soy and eggs was at least 10 times higher than in control subjects, (McDonald et al 1984). Monozygotic twins with IBD including Crohn’s disease and ulcerative colitis were studies for their IgG, IgA and IgM responses to egg, milk, gliadin, yeast and mannan (component of yeast cell wall). The only difference between the ulcerative colitis patients and the controls was in the response to gliadin. The Crohn’s disease patients, however gave significantly high titres for antibodies against mannan and whole yeast. This suggested that in Crohn’s disease, the immune system is selectively activated by an antigen in the yeast cell wall, (Lindberg et al 1992). 11 4.6 IRRITABLE BOWEL SYNDROME Food sensitivity has been implicated as playing a role in irritable bowel syndrome (IBS). Patients with IBS have chronic symptoms of abdominal pain, bloating, and disordered bowel habits (e.g. diarrhoea, constipation or wind) for at least 3 months per year (Thompson et al 1999). These symptoms of functional disorder of the bowel are commonly associated with non-bowel symptoms of other disorders such as fibromyalgia, chronic fatigue syndrome, as well as symptoms arising from pelvic organs such as dysmenorrhoea and urinary symptoms, (Camilleri & Choi 1997). These patients have usually been fully investigated and other pathology excluded on endoscopy and barium studies. After being diagnosed IBS they are offered a range of treatments often aimed at suppressing symptoms such as anti-inflammatory or anti-cholinergic agents. For many patients these are only partially successful and only temporarily, (Camilleri & Choi 1997). IBS is associated with considerable medical costs, (Talley et al, 1995), accounting for approximately 10% of the workload of general practitioners, (Jones 1996). The cause of IBS is unknown, indeed it is not clear whether it is in fact a single clinical entity or a convenient label for patient with chronic functional bowel disorder of varying origin, (Shaw et al 1998). The role of food in the aetiology of IBS is controversial e.g. a common recommendation for patients with IBS is to increase bran consumption, (Harvey et al 1987). caused by lack of fibre in the diet, (Painter 1972). this disorder, (Lynn & Freidman 1993). This advice is based on the theory that IBS is Minimal evidence exists that bran has therapeutic value in However, a recent trial has shown that bran supplementation is of no value in relieving the symptoms of IBS, (Snook & Shepherd 1994). It has also been shown that bran may increase these symptoms and is possibly responsible for exacerbating mild, non-complaining cases, thereby creating more IBS patients, (Francis & Whorwell 1994). There is evidence that IBS may (at least in some patients) be the result of food sensitivity, (Alun-Jones et al 1992, Fell et al 1991 and Bischoff et al 1996). Recently, a systematic review of the literature using Medline (1980-1996), targeting IBS and adverse reactions to food was conducted. Out of 32 publications located, a total of 7 fulfilled the inclusion criteria, (written in English, adult subjects, no letters/abstracts). The studies 12 included were Jones et al 1982, Bentley et al 1983, Farah et al 1985, Petitpierre et al 1985, McKee et al 1987, Zwetckenbaum & Burakoff 1988 and Nanda et al 1989. Of these studies, the positive response to an elimination diet ranged from 15-71% and double-blind placebo-controlled food challenges identified problem foods in 6-58% of cases. However, all selected studies had major limitations in their trial designs including inadequate patient selection, appropriateness and duration of elimination diets, and methods of food challenge. Carefully designed controlled clinical trials are necessary to test the role of adverse reactions to food in patients with IBS, (Niec et al 1998). Food specific IgG has been observed in patients with GIT symptoms (Iacona et al 1995, Cavataio et al 1996) and in patients with more clinically defined gastrointestinal diseases. In gluten-sensitive enteropathy both IgG and IgA antibodies to gliadin, as well as other dietary antigens have been well documented in relation to coeliac disease, (Unsworth et al 1983 and O’Farrelly et al 1983). Recently, a disease like antibody pattern was also found in approximately one third of IBS patients, indicating a potential coeliac-like disease in a subgroup of IBS patients, (Wahnschaffe et al 1998). 4.7 MIGRAINE Patients with migraine have chronic symptoms of headache lasting from 4 to 72 hours with transient sensory and/or gastrointestinal disturbances, (Soloman & Price 1997). Migraine is not associated with considerable medical costs, which is largely due to low rates of consultation by sufferers and poor of recognition of the disorder by physicians. Population-based studies have demonstrated that 19 to 44% of the patients never consult a doctor, furthermore, most sufferers who initially consult a GP rarely go back, ( Stang et al 1994, Lipton et al 1995). The low rate of consultation may be due to poor initial diagnosis and that most migraine sufferers rely on over-the-counter medication rather than being treated with prescription drugs, thus, may not be receiving effective treatment. Although migraine isn’t associated with high medical costs, its impact on quality of life is considerable and has economic implications in terms of productivity losses due to disrupted work. The overall cost attributable to migraine is unknown, but it is established that the indirect costs outweigh the direct medical costs and represent an obvious target for intervention aimed at reducing the impact of this chronic condition. 13 The cause of migraine is still largely unknown, however, there is evidence that it may result from food sensitivity, about 25% of migraine patients report that their symptoms can be initiated by certain foods, ( van den Bergh et al 1987). A double blind study on 40 migraine affected children, reported a decrease of attacks with the avoidance of some foods. Associated symptoms also improved including abdominal pain, fits, asthma and eczema (Egger et al 1983). Other studies have observed a decrease in number of attacks in 80% of patients on avoidance diets, (Hughes et al 1985 and Mansfield et al 1985). A role for IgG in the induction of migraine has been proposed but not confirmed, (Lord & Duckworth 1977 and Jerzmanovski & Klimek 1983). 4.8 RHEUMATOID ARTHRITIS Rheumatoid arthritis is an inflammatory disease that causes pain, swelling, stiffness, and loss of function in the joints. It can also affect other parts of the body besides the joints and people with the disease may have fatigue, occasional fever, and a general sense of malaise. The severity of the disease ranges from mild or moderate to severe disease that is active most of the time, lasts for many years, and leads to serious joint damage and disability. There is no treatment that can cure or reverse rheumatoid arthritis, however, there are medications that can relieve its symptoms and slow or halt its progression. They include nonsteroidal anti-inflammatory drugs (help relieve pain and inflammation), corticosteroids (reduce inflammation and slow joint damage), disease-modifying antirheumatic drugs (slow or halt the progression of rheumatoid arthritis). Each of these treatments produce side effects including stomach upset/bleeding, easy bruising, thinning of bones, cataracts, weight gain, diabetes, high blood pressure, blurry vision and increased susceptibility to infection. There have been reports that suggest adverse reactions to food may influence the disease progression of rheumatoid arthritis in certain individuals. 9% of a group of RA patients showed a favourable response to diet restriction and a marked exacerbation on re-challenge, six of these patients were studied via placebo controlled re-challenges and food intolerance was observed in four of them. This suggests a subgroup of RA in which food intolerance influences disease activity, (van der Laar & der Korst 1992 and van der Laar et al 1992). 14 5. CONCLUSION It was the aim of this review to present evidence and key arguments supporting the role of IgG in food sensitivity. The main reason for this is the fact that the theory behind testing is unclear and the reliability and validity of the food specific IgG test has not been fully evaluated. For these reasons, the diagnostic value of the methodology has been argued against. The key argument against the role of IgG in food sensitivity is the various reports of the presence of food specific IgG in normal healthy individuals. There are more publications opposing the role of IgG in food sensitivity, but these studies are based on the presence of food specific IgG in health as well as disease and not on IgG in chronic disease. In some of these studies either there is no mention of the number of subjects used, or a low number was used so it is difficult to say how significant the results are. Some of the studies did not reflect a sufficiently large sample of the population. For example, infants as normal individuals may not be accurate as it has been demonstrated that there is an age trend increase in food specific IgG in 5-12 month old infants, which declines to negligible levels in adults, (Ahmed et al 1997). In other studies it is unclear whether the controls were healthy or merely non-atopic/food-challenge negative patients. studies, different assay techniques are used and could easily give different results. In many of the Even in the same assay technique, such as ELISA, there are many variables involved, which can produce contrasting results. This review has been successful in providing some evidence that food specific IgG may indeed have a role to play as a useful diagnostic marker in food sensitivity influenced chronic disease. From the evidence, it seems that although the pathogenic mechanism of food sensitivity is unclear, IgG is involved in some way. Its occurrence in raised levels in food sensitive individuals, and its decrease when the offending food is removed from the diet provides strong evidence of its involvement. This is especially true when the elimination of offending food results in symptomatic improvement. However, the lack of studies looking at the mechanism of IgG in food sensitivity and clinical trials involving a disease group such as irritable bowel syndrome, migraine and eczema make it impossible to say for certain that the food specific IgG is the cause of some of the chronic diseases discussed. 15 At the present time the evidence suggests that the testing for food specific IgG by the reliable and reproducible ELISA technique may be of use as a diagnostic tool, which can be utilised to reduce or remove the adverse symptoms of many individuals who suffer from food sensitivity. Clinical trials involving disease groups and healthy individuals, along with double blind placebo controlled elimination diets in conjunction with the food specific IgG test, will be helpful in providing more convincing evidence that IgG has a role to play in the pathogenesis of certain diseases associated with food sensitivity. APPENDIX I - Search strategy The scientific literature databases searched were MEDLINE (1966-1999), BIDS (1981-1999) and AGRICOLA (1979-1999). Variations on these Key words used were food sensitivity, food intolerance and food allergy. searches included one of immunopathogenesis/pathogenesis or diagnostic tests. the above plus IgG, immunoassay/ELISA, The search results were incorporated and merged in Endnotes reference management software to give over 7000 references some of which were not related to this study and were deleted to give about 6000 references. IgG was then used as the key word to give 231 references, the abstracts of each were read if available and 88 relevant papers were chosen to be included in this review.