Example of a Completed Plan
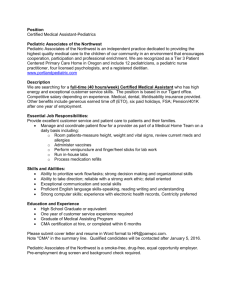
advertisement

Introduction On November 18, 2009, Pediatric ED staff (all attendings, 2 RNs) held a retreat to become trained in TeamSTEPPS and discuss innovations to improve patient care and safety in the Pediatric ED. Cheryl Jackson, Director of the Pediatric ED, invited Celeste Mayer, Patient Safety Officer, and the RTI TeamSTEPPS evaluation team to participate, and during this time, the group targeted areas for quality improvement and collaborated to develop a TeamSTEPPS Action Plan to address care and safety concerns. This report elaborates on each of the Action Planning steps. The change team selected improving staff situation monitoring and communication for their first project. Using the Strengths, Weaknesses, Opportunities, and Threats (SWOT) analysis conducted by an external consultant in 2007, they pinpointed the following threat: “inadequate system or practice for accurate cuing of patient status (especially on unit admission) or progress towards goal that allows entire ED team to maintain vigilance and situation awareness.” To ameliorate this concern, they opted to incorporate two specific activities into their regular activities: 1) conducting three scheduled huddles/briefings throughout the day (9AM, 6PM, and midnight) and 2) developing a white board system that tracks lab status (ordered, obtained, pending, completed) for each room. The change team intends to begin implementing these innovations on December 8, 2008 after speaking with the ED Nurse Manager, briefing incoming residents and other Pediatric ED staff, and discussing the changes at an upcoming ED nurse staff meeting. The RTI evaluation team and Celeste Mayer will document the implementation process and monitor program success using the metrics identified during the retreat. The performance measures and evaluation plan are outlined in more detail below, and staff hopes to see changes within a six month time frame. To make these interventions possible, Pediatric ED staff left the retreat with several tasks, listed in the table below. Change Team Next Steps Member Cheryl Jackson Meet with Sandy Pabers, ED Nurse Manager Brief incoming residents and HUCs Dan Macklin & Create checklist for huddles/briefings Jessica Katz-Nelson Robin Davis Make calendar with checkboxes for 9AM, 6PM, and midnight briefings Becky Wheeler & Develop white board/lab status system Paula Toney Celeste Mayer Contact Sergio Rabinovitz for Pediatric ED data Collect ongoing data (calendar, white board status, and clinical outcome measures) The following sections detail the Pediatric ED’s Action Plan. Step 1. Create a Change Team In developing the action plan, Pediatric ED staff identified the hospital, physician, nursing and frontline leaders (enumerated below). Of these team members, several have process improvement experience. Celeste Mayer has IHI Process for Improvement experience, and Alan Stiles, Jessica Katznelson, and Cheryl Jackson are Six-Sigma yellow belts. Change Team Member Senior Leader -“Executive Sponsor” Clinical or Technical Expert – “The Champion” Front-Line Leader Other Change Team Members Name (Staff Position) Brian Goldstein, MD (Chief of Staff, UNC Hospitals) Alan Stiles, MD (Chair of Pediatrics) Mary Tonges, RN (Vice-President, Nursing) Cheryl Jackson, MD (Director of Pediatric ED) Jeff Strickler, RN (Clinical Nursing Director) Celeste Mayer, RN PhD (Patient Safety Officer) Kelly Revels, RN Al Bonifacio, RN Jennifer Haynes, RN Becky Wheeler, RN Jessica Katznelson, MD Pediatric ED faculty Paula Toney, RN Step 2. Define the Problem, Challenge or Opportunity for Improvement An analysis of strengths, weaknesses, opportunities, and threats (SWOT analysis) revealed several processes that would benefit from improved teamwork and communication. During the November 2008 faculty retreat, the Pediatric ED staff selected one area for process improvement from the “Threats” section of the SWOT analysis: inadequate system or practice for accurate cuing of patient status (especially on unit admission) or progress towards goal that allows entire ED team to maintain vigilance and situation awareness. The team determined that inconsistent follow-up on lab status could benefit from situation monitoring and from creating an environment of mutual support. They will initiate a new white board system, indicating lab status for each room (e.g., labs ordered, obtained, pending, and completed). This should improve their ability to disposition patients in a timelier manner. All staff will share the responsibility for updating the board and there will be primary responsibilities based on roles (e.g., RNs who draw the blood for a lab would indicate that the lab was obtained). The change team also discussed involving the HUCs in this process because they can check A2K/SMS to follow lab status, even though they cannot see the results. Becky Wheeler and Paula Toney agreed to collaboratively create the first version of the white board. In addition, the staff decided to institutionalize three huddles/briefings during shift changes and prior to the Pediatric ED’s closure at night based on near misses due to breakdowns in team skills and staff member concerns of possible adverse events. These huddles/briefings will occur at 9AM, 6PM and at midnight. Attending physicians will lead the huddles/briefings. Drs. Dan Macklin and Jessica Katznelson agreed to create a checklist of important topics to cover during these concise huddles/briefings. The change team anticipates commencing these improvements on December 8, 2008 after Dr. Cheryl Jackson meets with the ED nurse manager and the ED nursing staff meets. Step 3. Define the Aims of Your TeamSTEPPS Intervention In this step, the change team outlined their process and outcome aims and identified several clinical outcomes. The table below summarizes the team’s plan: Planning Question TeamSTEPPS Process Aim What do we want to achieve? Who will be involved in the change? When will the improvement occur? Outcome Aim What do we want to achieve? Who will be involved in the change? When will the improvement occur? Clinical Outcome Aims Plan Scheduled huddles/briefings occur 80% of the time (based on calendar with checkbox indicating whether huddle occurred) White board up-to-date 85% of the time (based on self-report or observations made by Celeste Mayer) Consistent use of practices meant to improve situation awareness, mutual support, communication and efficiency. All Pediatric ED staff The huddles and white board system will be implemented in early December. Adherence to implementation goals is expected to be met by the end of January 2009. Improve Pediatric ED staff perceptions of teamwork, situation awareness, mutual support, communication, and efficiency, based on interviews within 6 months of TeamSTEPPS Intervention implementation Improve staff perceptions of situation awareness, mutual support, communication, and efficiency All Pediatric ED staff Official start date will be December 8, 2008 Expect to see changes within 6 months Decrease in length of stay (as compared to same six months of previous year) What do we want to achieve? Who will be involved in the change? When will the improvement occur? Decrease in time to triage Decrease in time to see the doctor Decrease in time to disposition Decrease in time from disposition to discharge Improve efficiency Improve patient care and satisfaction Improve staff satisfaction All Pediatric ED staff Expect to see changes within 6 months Step 4. Design a TeamSTEPPS Intervention As a first step, all of the Pediatric ED attendings as well as several nurse leaders were trained on TeamSTEPPS. As described above, the change team decided to emphasize communication and situation monitoring for their intervention. Specifically, they plan to implement three scheduled briefings during shift changes and prior to the nightly closure of the Pediatric Emergency Department (i.e., 9AM, 6PM, and midnight). To maintain consistency and ensure coverage of important topics (e.g., bed availability, patient status), Drs. Katznelson and Macklin will develop a list of key topics for discussion. Both noted that they regularly use the same mental list, but this will codify their mental lists, support a shared mental model and promote resident professional socialization. In addition to the scheduled huddles/briefings, they decided to implement a white board system to update a room’s lab status (ordered, obtained, pending, and complete). Paula Toney, RN and Becky Wheeler, RN will develop the first version of the white board and will involve other staff in the decisions about where to hang it and exactly how it should be updated. The change team also hopes to use this new system as an opportunity to integrate HUCs and volunteers into the team. HUCs can look up lab status, not results, in the A2K/SMS systems, and volunteers can report lab status to families when patients inquire (rather than trying to search for a physician). All Pediatric ED staff are responsible for updating this board, but the change team felt that clear responsibilities need to be assigned based on roles (e.g., a nurse may be responsible for updating the status as “obtained” once s/he draws blood). In addition to these two specific new practices, the change team will model the TeamSTEPPS strategies and behaviors in their team interactions, making use of all of the tools as appropriate and explaining them to other staff (e.g., checkbacks, call-outs, good leadership practices, two-challenge rule, CUS words, etc.). Since not all of the Pediatric ED staff will have received TeamSTEPPS training at the time the intervention is implemented, it will be especially critical for the change team to explain the benefits of the two new practices, and to consistently demonstrate situational awareness and good communication skills in their department interactions. The change team will initiate these new practices on December 8, 2008 and will discuss what revisions they should consider to the innovation during their February 2009 retreat (unless an immediate need for a revision seems important). Step 5. Develop a Plan for Testing the Effectiveness of your TeamSTEPPS Intervention To accomplish Step 5, the change team agreed upon several measures and data collection strategies to determine whether their intervention was successful. Planning Question Plan TeamSTEPPS Scheduled huddles/briefings occur 80% of the time (based on Process Aim calendar with checkboxes indicating whether huddle occurred) White board up-to-date 85% of the time (based on self-report or observations made by Celeste Mayer) Staff responsible for Robin Davis will create a calendar, with checkboxes for each collecting data designated briefing time, indicating whether huddle occurred Celeste Mayer will obtain a copy of the monthly calendar Celeste Mayer will collect data on white board usage through phone calls and observations (white board should be up-todate during 85% of phone calls and visits) Measures/target Scheduled huddles/briefings occur 80% of the time ranges for the data White board up-to-date 85% of the time Study Design Pre-post intervention study Data Sources, Huddle/briefing calendar collected throughout implementation collection methods, period and collection White board status checked by Celeste Mayer throughout timeline implementation period TBD observations by Wei-Ting Lin at baseline and postintervention Analysis, Calendar and white board data assembled in Excel file and interpretation, and presented in graphical form (e.g., time by % of huddles presentation achieved) TBD, report summarizing findings of observations Team Outcome Aim Improve Pediatric ED staff’s situation awareness, mutual support, communication and efficiency Staff responsible for RTI evaluation team collecting data TBD, Wei-Ting Li, nurse observer, may conduct observations (baseline and post-implementation) Measures/target Staff perceptions of changes in situation awareness, mutual ranges for the data support, communication, and efficiency Study Design Post-test only (given the quick start time of the implementation it was not possible to collect baseline interviews). Staff will be asked to recall their earlier perceptions, as well as their current perceptions. Data Sources, collection methods, and collection timeline Analysis, interpretation, and presentation Clinical Outcome Aims Staff responsible for collecting data Measures/target ranges for the data Study Design Data Sources, collection methods, and collection timeline Analysis, interpretation, and presentation Key informant interviews conducted 6 months postimplementation with Pediatric ED staff Observational data using the TENTS tool to assess use of TeamSTEPPS tools and behaviors RTI evaluation team will transcribe and code interviews. Key codes will be organized in an analytic matrix and summarized across themes. Wei-Ting Lin will summarize and analyze her observational data and RTI will incorporate it into their reports. RTI will present findings in a descriptive report. Decrease in length of stay (as compared to same six months of previous year) Decrease in time to triage Decrease in time to see the doctor Decrease in time to disposition Decrease in time from disposition to discharge Celeste Mayer will contact Sergio Rabinovitz for data (hospital currently collects this data) Decreases in each measure Pre- and post-intervention Hospital collected data Celeste Mayer will get the data from the hospital throughout the implementation period Findings presented in most appropriate graphical form Step 6. Develop an Implementation Plan All Pediatric ED attendings and two ED nurses who work with the Pediatric ED received training on November 18, 2008. Other ED nurses will receive training as the ED nursing staff roll out TeamSTEPPS over the next two to three months. The Pediatric ED will implement their innovations beginning December 8, 2008. Prior to their intended start date, Cheryl Jackson will discuss the change team’s plans with Sandy Pabers, Nurse Manager of the ED. Cheryl will also update the incoming residents and HUCs on this practice. Nurses, present at the change team meeting, Wade Daniels, Becky Wheeler, Chris Clarke, and Paula Toney, will describe the planned intervention at an upcoming staff meeting and will encourage other nurses to visit the LMS TeamSTEPPS module. Step 7. Develop a Plan for Sustained Continuous Improvement In addition to documenting and measuring outcomes throughout the implementation, the huddle/briefing calendar and white board, should they prove effective, will likely become permanent fixtures. Staff can use their experience with the two innovations to consider program revisions (e.g., if huddles do not routinely occur at 9AM, they can analyze the reasons underlying that and change the time) and potential additions. To keep all staff apprised of the department’s progress, the change team is considered hanging conspicuous posters charting their rates of “compliance” with the two new practices (e.g., percentage of times the huddles were conducted). These timely updates may serve as a reminder and motivator. Celeste Mayer will share examples of the recognition cards that have been successfully used to reinforce TeamSTEPPS behaviors in the PICU and SICU. The change team will also discuss the program at faculty retreats (as well as consider future innovations, such as implementing strategies to ensure consistent use of standing orders). Step 8. Develop a Communication Plan Celeste Mayer and Cheryl Jackson have communicated with Drs. Goldstein and Stiles and Ms. Mary Tonges, RN about the program in the past. These stakeholders have knowledge of the program through its earlier implementation in the Pediatric Intensive Care Unit and Surgical Intensive Care Unit. They will continue to share information with these stakeholders by sending short reports on a quarterly basis. As mentioned above, Cheryl Jackson will speak with Sandy Pabers, Nurse Manger of the ED, and will advise incoming residents and HUCs of the innovation. All change team members will wear their TeamSTEPPS badges and strive to model TeamSTEPPS practices.