id_37_patricia_coward_sub
advertisement

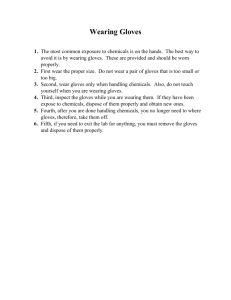
COMMENTS TO THE CONSULTATION DRAFT OF STAYING HEALTHY IN EARLY CHILDHOOD EDUCATION AND CARE Page 4 5 5 Issue The person with the infection spreads the germ into the environment Germs can spread in a number of ways: coughing and sneezing, touching infectious body fluids or secretions, touching contaminated surfaces, animals, food. A sneeze can spread droplets as far as two metres away. The droplets may be breathed in directly by another person, or another person may touch a surface contaminated with the droplets, then touch their mouth, eyes or nose. Comment This description of the chain of infection works well for diseases that are spread by contact with a contaminated environment (e.g. gastrointestinal infections) but does not work so well for diseases that are spread directly from one person to another without passing through the environment (eg scabies, head lice, respiratory droplets deposited directly onto another person’s mucous membranes). This section should be re-written to reflect established modes of transmission, i.e. contact, droplet, airborne, vector borne and food borne modes of transmission. This section should distinguish between infectious diseases that are spread by droplet transmission (e.g. influenza) and those spread by airborne transmission (e.g. measles and chickenpox). 1 5 8 9 10 10 11 20 Germs can spread …. if a person touches infectious body fluid, then puts their hands in their mouth, or if they prepare and eat food without first washing their hands. Main ways to prevent infection Germs can be present on the skin, hair, feathers and scales of animals and in their faeces and urine Antibacterial soaps Cloth towels cannot be used without prior laundering due to the risk of recontaminating or cross-contaminating hands Factors that may contribute to dermatitis include….: Pertussis Include, ‘through non-intact skin’. This section should include information on design features at the childcare facility that promote infection prevention and control, e.g. appropriate number and placement of hand washing basins (including in outdoor play areas and at nappy changing stations), use of impervious surfaces and materials that readily cleaned, well ventilated spaces, etc. This should include ‘mouth and saliva’. It may be useful to state that these soaps can cause skin irritation in some people. This statement should clarify that cloth towels are not to be shared between people. Add, ‘using some types of disposable gloves, particularly by susceptible people’. This should include that pertussis is a serious risk to infants and can cause life threatening illness in this age group 2 20 Measles This should include that encephalitis and subacute sclerosing panencephalitis are serious complications of measles 20 Mumps 2122 23 Measles/varicella spreads by droplets Wearing gloves does not replace the need to wash your hands, and you should ensure you wash your hands before putting gloves on and after taking them off. Latex gloves are preferable2 This should include that orchitis can occur in post-pubertal males (because of the increasing number of males working in childcare) ‘Droplets’ should read ‘airborne droplets’ to distinguish between droplet transmission and airborne transmission 23 This should refer to hand hygiene rather than hand washing. Latex gloves provide a high level of protection in healthcare settings, however there are concerns about the use of latex gloves and associated latex allergy in childcare settings, as latex allergy has been reported in children other than those with recognised risk factors such as spina bifida ( Ref: Shield S et al 1992, ‘Prevalence of latex sensitivity in children evaluated for inhalant allergy’, Allergy Proc, 13(3):129-131). Children attending childcare settings may be at significant risk of exposure to latex and acquiring latex allergy because: childcare services are more likely to use cheaper, powdered supermarket brands of latex gloves rather than the more expensive low protein, powder free medical grade examination gloves used in healthcare children may be regularly exposed to latex, including via their mucous membranes (e.g. when staff wear powered latex gloves to prepare and handle food and to change a child’s nappy, from inhaling latex powder when staff remove powdered gloves near children, and from touching surfaces that are contaminated with latex powder such as nappy change mats). Some authorities are suggesting that latex gloves should not be used in childcare because of latex allergy risks to 3 children (and staff) (Ref: University of NSW 2003 section 16.4 http://www.sphcm.med.unsw.edu.au/SPHCMWeb.nsf/resources/CCModelPolicies.pdf/$file/CCModelPolicies.pdf) 23 Vinyl gloves are not recommended Vinyl gloves provide a lower level of protection than latex gloves for healthcare workers in healthcare settings, however childcare care workers are at lower risk of contact with blood and body substances (including frequency, duration and volume of contact), and therefore appropriate vinyl gloves may be adequate in this setting and prevent the risk of latex allergy among staff and children from the use of non-medical examination grade powdered latex gloves. This section should include that polyethylene gloves are not recommended for contact with blood and body fluids, i.e. plastic food handling gloves. 23 23 Powder-free gloves are preferable, because powdered gloves may contribute to latex allergies When changing a nappy, it is important to wash your hands before you put on gloves, so that when you have finished changing the child, you can remove the dirty gloves and dress the child with your clean hands, without needing to wash your This statement should stress that powdered latex gloves must not be used because of the increased risk of latex allergy for both staff and children. This section should be amended to state that workers are to perform hand hygiene using alcohol based hand rub after removing gloves and before dressing the child, because hands may be accidentally contaminated during glove removal or due to a breach of the glove’s integrity (PPE failure). 4 24 32 34 hands in between. This also means that bottles are cleaned less often and there is a higher risk of germs growing in the stale detergent. Panadol High-risk groups include elderly people, people who are diabetic, and people who are alcoholic This statement should include the following points: Germs can be dispersed into the environment by the spray mechanism The trigger mechanism on the spray bottle cannot be cleaned and dried properly thereby encouraging bacterial growth The use of chemicals in spray bottles can cause health and safety issues such as respiratory irritation and sensitisation. Brand names of medications (i.e. Panadol) should not be used. This statement should also include pregnant women, given the predominance of women of reproductive age working in childcare. 35 Measles—highly infectious virus spread by droplets ‘Droplets’ should read ‘airborne droplets’ to distinguish between airborne transmission and droplet transmission. 39 If cloth towels are used they must be laundered before they are reused due to the risk of contaminating clean hands. How to wash hands with soap and water This statement should clarify that cloth towels are not to be shared between people. 39 39 How to clean hands with hand rub This section should include a statement about how rings can prevent proper hand hygiene and harbour bacteria, and should be removed or kept to a minimum. (Ref: Trick et al (2003), ‘Impact of Ring Wearing on Hand Contamination and Comparison of Hand Hygiene Agents in a Hospital’, Clin Infect Dis, 36 (11): 1383-1390. This should specify the minimum percentage of ethanol of the ABHR (some brands available on the market have < 70v/v ethanol). 5 41 When there is a chance you may come in contact with body fluids, including faeces, vomit or blood’; ‘when cleaning faeces, blood or vomit, including when it is on clothes’; and ‘If there is a chance that you may come in contact with faeces, vomit or blood, you should wear disposable gloves.’ When preparing bleach solutions for cleaning These statements should include urine, because childcare workers are at high risk of exposure to cytomegalovirus, and this is of particular concern given the predominance of women of reproductive age working in childcare (Ref: Billette de Villemeur et al 2011, ‘Occupational risk for cytomegalovirus but not parvovirus B19 in childcare personnel on France’, Journal of Infection, 63:457-467). 41 Disposable gloves 42 An area should be specifically set aside for changing nappies. Table 8 Nappy changing procedure If faeces spill onto the change surface, clean This section should stress that disposable gloves are not to be re-used, for example by washing gloved hands in between nappy changes, or by laundering gloves for re-use. Add, ‘This area should have ready access to a hand washing basin’. 41 42 43 Bleach is not a cleaning agent. This statement should read, ‘When preparing bleach or other chemical solutions for cleaning and disinfection’. This section should recommend that hand hygiene using alcohol based hand rub should be included between removing gloves and dressing the child. Include urine because of the risk of exposure to cytomegalovirus. 6 44 45 52 52 53 58 the surface with detergent and warm water and leave it to dry. Wear gloves when handling and preparing bleach. Dispose of dirty tissues immediately. Staff clothing or overclothing should be washed daily in hot water. Include, ‘use safety eyewear if there is a risk of splashes of bleach to the face, for example if decanting bleach from concentrated solutions in primary containers’. Include, ‘into an appropriate receptacle such as a lined rubbish bin’. Most staff will wash their work clothes at home, and unless they are provided with a uniform then this clothing will be their personal clothing. Recommending a hot wash means that staff will experience additional expense and time associated with washing these clothes as this will require a separate was to other clothes washed in cold water. A hot wash uses significantly more energy and may damage some fabrics over time. The dilution effect of a machine wash combined with detergent should be sufficient to remove any infectious agents. Unless there is good evidence to support a hot wash, this recommendation should be removed. Include a statement recommending that hand hygiene should be performed using alcohol based hand rub between removing gloves and dressing the child. Remove your gloves. Dress the child and wash the child’s hands and your hands Start a ‘Toys to wash’ Include, ‘or if a toy has been placed in a child’s mouth’. box and place toys in it during the day if you see a child sneeze on a toy, or if the toy has been used by a child who is unwell. Adults and children Replace with, ‘Adults and children must perform hand hygiene by washing their hands with soap and water or must wash their hands applying hand rub after playing in the sandpit’. with soap and water or 7 a hand rub after playing in the sandpit. 59 Animals 63 Workplace health and safety Acts in Australian states and territories place a duty of care on employers to ensure workplace health and safety Every education and care service needs to ensure it has effective infection control policies and procedures in place, including strategies to prevent exposure to infectious diseases and minimise risks from chemicals, and processes to ensure that infection control measures are carried out. Employers of educators and other staff have an obligation to minimise the risk to all staff from exposure to diseases that are preventable by 63 64 Include a sentence about ensuring the hygienic cleaning of fish tanks (to prevent exposure to fish zoonoses such as M. marinum). This should reflect the wording of the new harmonised WHS legislation that is being enacted by the states/territories. For example state, ‘Work health and safety Acts in Australian states and territories place a duty of care on persons conducting a business or undertaking to ensure the health and safety of workers and others so far as is reasonably practicable’. Replace with, ‘Every education and care service needs to ensure that infection risks are prevented or minimised so far as is reasonably practicable, including strategies to prevent or minimise exposure to infectious diseases and chemicals used to manage infection risks, and processes to ensure that infection control measures are implemented and maintained’. Include, ‘Infections acquired by staff that are reliably attributable to their work must be notified to the workplace health and safety regulator in their state or territory’. Replace with, ‘Persons conducting a business or undertaking in education and childcare services have a duty of care to ensure, so far as reasonably practicable, the work health and safety of educators and other staff at risk of exposure to diseases that are preventable by vaccination’. 8 64 64 64 65 65 65 vaccination. being restricted to working with children over 12 months old not being able to work at all during outbreaks of bacterial diseases Employers should: Recommended vaccinations for educators and other staff pertussis—this is especially important for educators and other staff caring for the youngest children who are not fully vaccinated Some vaccinations are not recommended during pregnancy, or if a person has a disease or is undergoing treatment that affects Include, ‘if they have not received an adult pertussis booster (dTpa)’. Remove ‘bacterial’ because staff may also be removed or have work restrictions placed on them if they are nonimmune and there are outbreaks of viral diseases such as measles, varicella and hepatitis A. Include, ‘manage the work health and safety risks of workers who refuse vaccination, who cannot be vaccinated due to medical contraindications or who do not respond to vaccination (e.g. following rubella vaccination). These workers remain at risk and their risk should be managed in other ways including by pre-exposure strategies such as safe work practices and appropriate work placement (e.g. don’t place workers who have not had an adult pertussis booster(dTpa) to care for infants), and post-exposure strategies such as work adjustments/restrictions/placements (eg restricting a non-immune worker during a measles outbreak) and post-exposure prophylaxis/chemoprophylaxis(e.g. post-exposure hepatitis A immunoglobulin/vaccine). If the guidance is to be used by facilities providing care for older children (e.g. school-based services), then it should clarify that hepatitis A vaccination is only required for childcare workers and not those caring for older children unless other risk factors exist (e.g. working in a remote Indigenous community). This sentence needs to clarify that staff require an adult pertussis booster (dTpa) in addition to their childhood vaccination/infection because immunity from childhood immunisation/infection wanes over time. This statement should clarify that influenza vaccination is recommended for pregnant women in who are going to be in their second and third trimester of pregnancy during the influenza season. 9 67 their immune system. For example, an educator who usually works in the babies room becomes pregnant, and she is not immune to CMV. 68 Chickenpox 81 The disease is more severe in adults and in people of any age who have impaired immunity. Responsibilities of educators and other staff 81 82 8182 82 This statement incorrectly implies that women become immune to CMV from previous infection, and that only seronegative women should be relocated to a lower risk area. Pre-conceptual CMV immunity reduces the risk of congenital infection but the protection is incomplete. Intrauterine transmission and symptomatic congenital infection from re-infection can occur in women who are seropositive prior to pregnancy. Because congenital infection can result from maternal re-infection, avoiding exposure to CMV through behavioural changes and work adjustments should be beneficial for seropositive as well as seronegative women. (Ref: Ross et al. (2010), ‘Cytomegalovirus reinfections in healthy seroimmune women’, JID, 201(1 Feb): 386-389; Boppana et al (2001), ‘Intrauterine transmission of cytomegalovirus to infants of women with pre-conceptual immunity’, N Eng J Med, 344(18):13661371; Wang et al (2011), ‘Attribution of congenital cytomegalovirus infection to primary versus non-primary maternal infection’, CID, 52(15 Jan):e11-e15). Include in this section, ‘Anyone who works with children and who has not previously been infected with chickenpox should be immunised, or be certain that they are immune to chickenpox by having a blood test’. Include in this section ‘and can cause serious complications such as pneumonia and encephalitis’. Include in this section, ‘Ensure non-immune staff are vaccinated. Protect non-immune staff if cases of chickenpox occur at the facility, for example by arranging vaccination or immunoglobulin if advised by a medical practitioner, or removing non-immune staff from child contact during the outbreak if advised by the public health unit’. Controlling the spread of infection Chickenpox Include in this section, ‘Discuss with the public health staff who in the education and care service might need preventive treatment and who should be excluded from care’. The fact sheet should also discuss the management of staff with shingles (and children with childhood shingles). Vaccination after exposure can usually prevent a person getting symptoms of Include ‘Non-immune exposed staff should be referred promptly to their doctor for advice about vaccination. Parents who are non-immune or whose children are non-immune should be advised to seek medical advice’. 10 91 chickenpox if the vaccine is given within 3 days of exposure, and may prevent symptoms when given up to five days after exposure. Avoid contact between the person who is ill, and children or frail and elderly people, until the person is feeling well. Cytomegalovirus 91 Description 91 This risk is highest during the first half of the pregnancy and in women who have not been infected before. During initial infection or reactivation Responsibilities of educators and other staff 82 92 92 Include, ‘and pregnant women’. If the guidance is to be used by facilities providing care for older children (e.g. school-based services), then it should clarify that CMV is primarily an occupational risk for those caring for pre-school aged children but that exposure may occur in some at-risk settings involving older children such as special needs. This section should include a statement that CMV re-infection with a different strain of CMV can occur in a previously infected person (note: a prevailing misconception exists that primary CMV infection provides complete protection against re-infection). Add, ‘However re-infection with intrauterine transmission and congenital infection can occur in a woman who has had previous CMV infection’. (Ref: Ross et al. (2010), ‘Cytomegalovirus re-infections in healthy seroimmune women’, JID, 201(1 Feb): 386-389; Boppana et al (2001), ‘Intrauterine transmission of cytomegalovirus to infants of women with pre-conceptual immunity’, N Eng J Med, 344(18):1366-1371; Wang et al (2011), ‘Attribution of congenital cytomegalovirus infection to primary versus non-primary maternal infection’, CID, 52(15 Jan):e11-e15). Replace with, ‘During initial infection, re-infection or reactivation’. Include, ‘Ensure that staff wear disposable gloves for activities involving contact with urine, such as changing nappies’. Include, ‘Where practicable, relocate pregnant women to work with older children to reduce the level of contact with urine and saliva’. (Ref: Pass et al (1990), ‘Increased risk of cytomegalovirus infection among day care centre workers’, Paed Infect Dis J, 9:465-470; Adler, S (1989), ‘Cytomegalovirus and child day care’, New Eng J Med, 321(19):1290-1296). 11 92 106 111 Pregnant women or women considering pregnancy who work with young children should pay particular attention to good hand hygiene after contact with body secretions, especially after changing nappies or assisting in toilet care. Description Responsibilities of educators and other staff Include, ‘Inform staff who are pregnant or considering pregnancy about CMV risks and how to protect against infection’. Include, ‘and wear disposable gloves for tasks involving contact with urine’. Include, ‘and should consider working with older children where practicable to reduce to reduce the level of contact with urine and saliva’. Include, ‘There is some evidence that acquiring hand, foot and mouth disease during pregnancy may result in congenital infection in rare cases’. (Ref: Monif GRG & Baker DA eds (2004), Infectious diseases in obstetrics and gynecology, 5th edn, Parthenon Publishing, Boca Raton. Include, ‘‘Ensure non-immune staff are vaccinated. Protect non-immune staff if cases of hepatitis A occur at the facility, for example by referring for vaccination as per medical advice, or removing staff from contact with children in affected areas of the centre or from contact with children requiring nappy changes or assistance with toileting’. Include, ‘Ensure staff wear disposable gloves for nappy changes and contact with faeces’. 113 113 Hepatitis B spreads when infectious body fluids … Responsibilities of educators and other staff Replace with ‘Hepatitis B spreads when infectious blood and body fluids …’. Include, ‘If inappropriately discarded sharps (needles and syringes) are an identified hazard at the facility, ensure procedures for the safe handling and disposal of sharps and provide training to staff’. Include, ‘Ensure hepatitis B vaccination for educators and other staff who care for children with intellectual disabilities. Although the risk is low, seek advice about hepatitis B immunisation if the children are not immunised’. 12 114 115 116 118 121 122 131 & 132 145 & Controlling the spread of infection Responsibilities of educators and other staff Controlling the spread of infection Responsibilities of educators and other staff & Controlling the spread of infection Children with measles should be excluded for at least 4 days after the appearance of the rash. Ensure that all staff have received two doses of MMR if they were born after 1966. Include, ‘Ensure a protocol for managing accidental blood and body fluid exposures and needlestick injuries’. Include, ‘Ensure good hand hygiene and wear disposable gloves when handling blood and body fluids’. Include, ‘Ensure a protocol for managing accidental blood and body fluid exposures and needlestick injuries’. Include, ‘Ensure good hand hygiene and wear disposable gloves when handling blood and body fluids’. Include, ‘Wear disposable gloves when handling blood and body fluids’ As per comments for hepatitis B and C, include information about ensuring good hand hygiene and wearing disposable gloves when handling blood and body fluids’ This should state ‘Staff and children with measles…’. Replace with ‘Ensure that all staff have received two doses of MMR if they were born during or since 1966.’ (Ref: The Australian Immunisation Handbook, 9th edn (2008) http://www.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-measles) Include, ‘Manage the risk to staff who are not immune, for example by restricting them from the facility during an outbreak if advised by the public health unit’. Include, ‘Ensure that all staff have received two doses of MMR if they were born during or since 1966.’ (Ref: The Responsibilities of Australian Immunisation Handbook, 9th edn (2008) educators and other staff & Controlling the http://www.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-measles)’. spread of infection Responsibilities of educators and other Include, ‘Ensure that all staff have received two doses of MMR if they were born during or since 1966.’ (Ref: The Australian Immunisation Handbook, 9th edn (2008) 13 146 165166 189 staff & Controlling the spread of infection Responsibilities of educators and other staff & Controlling the spread of infection Staff vaccination table http://www.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-measles)’. Include, ‘Ensure that staff have received an adult pertussis booster vaccine (dTpa). Manage the risk where staff have not received a booster, for example by not placing these persons to care for infants. Measles: This should clarify that the person requires 2 doses of MMR if born during or since 1966. Pertussis: This should clarify that the person requires an adult pertussis booster (dTpa), because childhood infection or immunisation alone will not provide adequate protection because of waning immunity. Patricia Coward [Personal information removed by NHMRC] [Personal information removed by NHMRC] [Personal information removed by NHMRC] 10.01.12 14