Chapter-47-Pruritus
advertisement

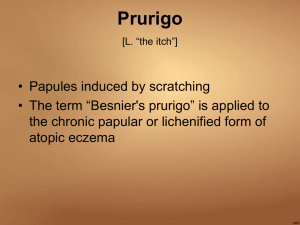
Section 9: The skin and internal disease Chapter 47: Pruritus Introduction Pruritus (itching) is the predominant symptom of kin disease and a frequent manifestation of systemic disease. Itch can be defined as an unpleasant sensation in the skin which elicits a desire to scratch. Itch is classified into 4 types: cutaneous (e.g. scabies, lichen planus), neuropathic (due to lesions of afferent pathways of the nervous system e.g. peripheral neuritis, brain tumours), neurogenic (due to centrally acting mediators which do not damage the CNS e.g. opioid peptides in cholestasis) and psychogenic itching. The quality of itching varies, ranging from burning, through pricking, to sensation of insects crawling over the skin. Pruritus may occur with or without skin disease and may be caused by systemic disease. Pathways of itching The neurophysiological pathways of itching start by the itch receptors in the skin. These are non-specific non-specialized unmyelinated free nerve endings located close to the dermal-epidermal junction. Itch is transmitted from the receptors to unmyelinated C fibers which enter the dorsal horn of the grey matter of the spinal cord, synapse there with secondary neurons, which cross over to the contralateral spinothalamic tract, and ascend to the thalamus. There, tertiary neurones relay itch to the level of conscious perception in the cerebral cortex. Table 47.1 Causes of pruritus. Systemic causes Chronic uraemia Cholestasis (primary biliary cirrhosis, obstructive jaundice, HCV pregnancy infection) Polycythemia vera Iron deficiency anaemia Malignancy (internal, Hodgkin’s disease, leukaemia) Anorexia nervosa Thyrotoxicosis Psychogenic The anterior cingulate cortex is involved in the recognition of itch sensation at conscious levels, whilst the premotor cortical areas participate in intention to scratch, which go to the skin through descending pathways. The receptors of itching are also sensitive to temperature, and this explains the worsening of itching in a warm environment. Scratching is a reflex functioning at a spinal level, modified by higher centers. Scratching relieves itching for several minutes after scratching has ceased. This may be due to suppression of the facilitating circuits that reinforce itching sensation, or the itching may damage temporarily the sensory nerve endings which take several minutes for repair. Causes of itching Itching has causes and is accomplished through mediators. The causes of itching include skin disease (e.g. scabies, lichen planus, atopic eczema, psoriasis), systemic diseases (e.g. chronic renal failure, hepatic cholestasis, iron deficiency, polycythemia vera, systemic drugs, thyrotoxicosis, myxoedema, diabetes mellitus, malignant diseases and anorexia nervosa), and itching in clinically normal skin (e.g. aquagenic pruritus, pruritus of senescence, psychogenic pruritus, postmenopausal pruritus, notalgia paraesthetica, and brachioradial pruritus). The causes of pruritus are presented in table 47.1 Skin causes Urticaria Eczema (atopic, asteatotic, stasis, contact) Prurigo (nodularis, pigmentosa, chronic of adults, of pregnancy, dermographic, actinic, Besnier’s, of HIV infection) Lichen simplex chronicus Drug hypersensitivity Bullous diseases e.g. DH, BP, pregnancy (PUPPP) Senile pruritus Neoplastic (mycosis fungoides) Infestations (scabies, pediculosis, papular urticaria, schistosomal cercarial dermatitis) Inflammations (extensive plaque psoriasis, LP, mastocytosis, eosinophilic pustular folliculitis) Localized pruritus: ani, scroti, vulvae, nostalgia paraesthetica Aquagenic pruritus -515- Mediators of itching Mediators of itching are central and peripheral. Central mediators are released in the CNS and include opioid peptides (e.g. in cholestasis). They have a peripheral augmenting action on histamine itch, in addition to their pruritic central action. Peripheral mediators are released in the skin and include mainly histamine, but other mediators are also implicated e.g. substance P, proteases (e.g. kallikrein and chymotrypsin), cytokines (e.g. IL-2), prostaglandin E2 and acetyl choline. Histamine is released by degranulation of dermal mast cells. There are 3 subclasses of histamine receptors. H3 receptors occur in the brain, and H1 and H2, receptors are present in the skin. H1 but not H2 receptors, are implicated in histamine-induced itching. Thus, there is no theoretical basis for use of H2 antagonists (cimetidine, ranitidine) in the suppression of itching caused by histamine. Substance P is a neuropeptide usually present in the skin which increases in itchy inflammatory dermatoses. It acts by enhancement of histamine release from mast cells but not other mast cell mediators. Substance P is synthesized in the dorsal root ganglion of nociceptor C fibres and transmitted peripherally in granules. A role for IL-2 in the itching of atopic eczema is proposed: T lymphocytes, an important source of IL-2, are a feature of the dermal infiltrate, and ciclosporin, a potent inhibitor of IL-2 production by T lymphocytes, causes relief of itching in atopic eczema. Also, IL-31 is involved in the pruritus of atopic dermatitis. Prostaglandin E2 enhances itching caused by histamine and other mediators. Acetylcholine is thought to be the mediator in aquagenic pruritus and possibly atopic dermatitis. Important mediators and their function in itching are illustrated in table 47.2. Itching in systemic disease Chronic uraemia: Itching occurs in chronic, but not acute, renal failure, in the majority of patients, and is severe in only a few. Itching may be persistent and extensive or transitory and localized. Dialysis usually does not improve itching. Factors suggested for the pathogenesis include abnormal sprouting of unmyelinated nerve fibres in skin of uraemic patients, and presence of raised serum parathyroid hormone levels, due to secondary hyperparathyroidism. Parathormone is known to increase tissue mast cells. T-cell derived lymphokines (IL-2) and opioid peptides are possible mediators for the itching of uraemic pruritus, and histamine is improbable because of absence of relief with the use of antihistamines. The best treatment for uraemic pruritus is renal transplantation. Other effective measures include UVB phototherapy (narrow band), activated charcoal, and gabapentin. Emollients are used for the dry skin. Topical capsaicin 0.025% is effective in localized uraemic pruritus. It acts by depletion of substance P from sensory nerve endings. Cholestasis: Pruritus, which may be generalized or localized (e.g. to the hands and feet), is a frequent and distressing symptom of cholestasis and may precede the onset of jaundice of any cause. It may be caused by primary biliary cirrhosis, obstructive jaundice, HCV infection or pruritus of pregnancy. Hepatitis C is an important cause of intense cholestatic pruritus, and should be considered as a part of the work-up of patients with severe pruritus. The pathogenesis of cholestatic pruritus may be the increased plasma levels of bile salts, or those of opioid peptides. Naloxone is effective in the treatment of cholestatic pruritus. Other therapies that may be effective include cholestyramine (ionexchange resin), phenobarbital combined with rifampicin, UVB phototherapy, and plasmapheresis. Table 47.2 Important mediators and their function in itching. Mediator Function in itch Histamine Pruritus of urticaria Acetylcholine Possibly pruritus of atopic dermatitis Substance P Prime mast cells for release of histamine CGRP Sensitization of itch receptive neurone terminals Opioid peptides Cause central itch, especially in cholestasis Neurotrophins (nerve growth Sensitize itch receptive neurons, possible role in atopic dermatitis factors) Prostaglandin E Sensitize itch receptors to histamine Cytokines Possible role of IL-2, IL-31 in itch of atopic dermatitis -516- Polycythemia vera: The itching of polycythemia vera occurs in 50% of patients. These develop a severe, prickly and distressing discomfort after water contact lasting for 15-60 minutes. As it frequently occurs after the patients emerge from bathing, it is referred to as ‘bath itch’. Platelet aggregation has been suggested as a possible mechanism and source of pruritogenic factors, including histamine. However, antihistamines are generally ineffective and treatment with PUVA or NB-UVB may be effective. Thyroid disease: The cause of intractable itching of thyrotoxicosis is cutaneous vasodilatation which leads to increased skin surface temperature, which lowers the itch threshold. The itching of myxoedema is due to excessive dryness of the skin, and responds to application of moisturizing creams. Diabetes mellitus: Contrary to popular belief, generalized pruritus is not a feature of diabetes mellitus. However intractable anogenital itching may occur due to candidiasis. Localized pruritus of the scalp is also a recognizable feature of diabetes. Other diseases: Generalized pruritus may be caused by malignant diseases and itching may be migratory. The generalized itching that occurs in patients with anorexia nervosa is associated with low body weight and resolves with weight restoration. Generalized pruritus may occur in patients having iron deficiency anaemia. Itching in normal skin The skin is apparently normal, apart from scratch marks. Pruritus may be localized (e.g. aquagenic pruritus, psychogenic itching, notalgia paraesthetica, and brachioradial pruritus) or generalized (e.g. pruritus of senescence, psychogenic itching, and postmenopausal pruritus). Aquagenic pruritus: Contact with water at any temperature leads to an intense pricking itch in the exposed skin, without visible change in the appearance of the skin. Acetylcholine is the probable mediator. The condition responds poorly to antihistamines and may respond to UVB phototherapy or PUVA. Psychogenic itching: Itching, either localized or generalized, can be a manifestation of psychological disturbance. Perianal and, in women, vulval itching are the commonest manifestations of localized psychogenic pruritus. Parasitophobia (delusions of parasitic infestation of the skin) is a generalized psychogenic pruritus that can be diagnosed from the patient’s description of itching due to insects in the skin. It is treated by antidepressant and anxiolytic drugs (e.g. doxepin and hydroxyzine), and pimozide (a phenothiazine) has been advocated for the treatment of delusion of parasitosis. Notalgia paraesthetica: This is a common cause of localized persistent pruritus. Characteristically, patients complain of persistent burning pruritus localized to the mid-scapular area, but may extend to the scalp. Mild lichenification and pigmentation may be seen. The current view is that it is a type of sensory neuropathy. Capsaicin cream may be effective. Brachioradial pruritus: This is a common sunlight-induced chronic pruritus, localized to the outer aspects of the elbow, and adjacent lower and upper arms. Oral gabapentin and topical capsaicin cream may be effective. Pruritus of senescence: Generalized pruritus, associated with extensive excoriation, occurs in 50% of those in the seventh decade or beyond. Itching results from excessive dryness (xerosis of the skin) caused by decreased sebum production and failure to retain water by the ageing skin. Treatment is with emollients, that should be applied at least 4 times daily. Antihistamines are not indicated in itching due to xerosis. postmenopausal itching: The generalized itching of postmenopausal women, which is troublesome at night, characteristically evokes rubbing rather than scratching and is controlled by ethinyl oestradiol replacement therapy, which is also effective in the treatment of localized genital pruritus resulting from oestrogen deficiency. Itching in atopic dermatitis The itching of atopic eczema is aggravated by scratch damage, which causes enhanced inflammation (itch-scratch cycle). Itching is usually worse at night, and is aggravated by contact with wool, sweat, spicy foods and alcohol. Paroxysms of itching may be experienced by patients in response to sudden changes of temperature, humidity, undressing or dressing. The itching of atopic eczema is multifactorial being due to dryness, inflammation and probably to disturbed regulation of itch traffic in the CNS. Mediators of itching are both peripheral -517- (histamine, mast cell mediators other than histamine, IL-2 from T-lymphocytes), and central (opioid peptides). Topical treatment of atopic eczema includes emollients for dryness, topical corticosteroids and tacrolimus (a topical T-cell immunosuppressant). Systemic treatment includes sedative antihistamines, UVB phototherapy, PUVA, and oral immunosuppressive drugs (azathioprine, ciclosporin). All these topical and systemic agents are highly effective in relieving the pruritus of atopic dermatitis, except sedative antihistamines which have a medium effect. Investigation of generalized pruritus This includes blood picture, renal, hepatic and thyroid function tests, stools for occult blood, and inquiry about a history of drug intake. Treatment of pruritus It is important to identify and treat the cause of itching, whether it is primarily in the skin or of a systemic origin. At the same time, patients require symptomatic relief. Pruritus is temperature-dependent and the patient should be advised to wear light clothes and keep his environment as cool as possible. Pruritus due to dry skin, especially prevalent in elderly people, may respond to emollients as aqueous cream. H1 antihistamines and topical corticosteroids should not be used in the absence of visible inflammatory changes in the skin. Low-sedation antihistamines are the treatment of choice for urticaria, while sedating antihistamines are better used for atopic eczema. Topical capsaicin is effective in localized pruritus e.g. post-herpetic neuralgia, prurigo nodularis, notalgia paraesthetica and brachioradial pruritus. Intractable itching may be treated with naloxone or doxepin, a tricyclic antidepressant. Paroxetine, a selective serotonin reuptake inhibitor, may have a place in the treatment of intractable itching, including that of advanced cancer. Naloxone is effective in pruritus of cholestasis. Gabapentin is effective in uraemic pruritus. Tables 47.3, 47.4 illustrate the mode of action of topical and systemic antipruritics, respectively. Table 47.3 Topical antipruritic medications. Topical antipruritic Mode of action Calamine Cooling Menthol Activation of cold-sensitive channels on afferent nerve terminals Capsaicin Depletes neuropeptides of afferent nerve terminals Doxepin Tricyclic, also potent H1 antihistamine Corticosteroids Calcineurin inhibitors Local anesthetics Anti-inflammatory, indirectly antipruritic Down-regulate activated T cells in skin Cause temporary loss of all skin sensation at site of application Table 47.4 Systemic antipruritic medications. Drug Mode of action H1 antihistamines Inverse agonist at the H1 receptor Doxepin Tricyclic, and potent H1 antihistamine Naltrexone Paroxetine Opioid receptor antagonist SSRI Mirtazapine Serotonergic and noradrenergic antidepressant Prevents release of neurotransmitters from nerve terminals Gabapentin -518- Comment on usage Short lived relief Short lived relief Burning sensation in early stages of treatment Effective in itching of atopic eczema, causes drowsiness Ineffective in itching of clinically normal skin Relieve itching of atopic dermatitis Risk of contact allergic sensitization Comment on usage Effective in urticaria, controversial in atopic dermatitis and other pruritic dermatoses May be effective in pruritus of atopic dermatitis Effective in pruritus of cholestasis Effective in pruritus of internal malignancy For intractable nocturnal pruritus Effective in uraemic pruritus