One of today`s major public health crises, opioid overdose is a
advertisement

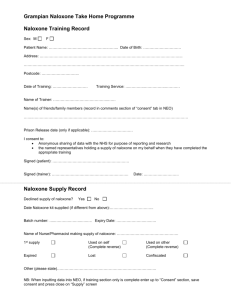
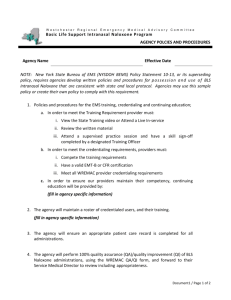
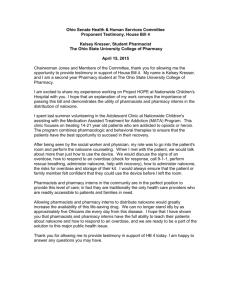
Policy Interventions to Address Fatal Opioid Overdose: A Regional Menu Leo Beletsky Introduction Despite its devastating impact in many communities and its emergent epidemic proportions, fatal opioid overdose (OOD) has gotten far too little attention from public health authorities, academics, and the media in many settings. The causes behind OOD are complex. They include fluctuations in drug quality and purity, lack of awareness among drug users and healthcare providers, and poor infrastructure for drug treatment and emergency response. Problems associated with the distribution, administration, and legal status of naloxone also form barriers to effective intervention to prevent overdose events from turning deadly. Stigmatization of drug use and users underlies many of these causes. It also helps to explain the general lack of attention or resources dedicated to combat OOD in many countries. Nonetheless, thanks to dedicated advocacy by community members and progressive healthcare providers, a number of countries, states or provinces, and cities have implemented policy reforms to address OOD. Shaped by the specific legal environment, resources, and other factors, these efforts focused on the following three major areas: 1. 2. 3. Improving the naloxone supply chain on national, regional, local, and institutional levels, Ensuring effective emergency response to OOD by governmental institutions and healthcare providers, Facilitating OOD prevention by NGOs and individuals. Although more scientific evaluation is needed to document the overall public health impact of these initiatives, it is clear that policy reforms can facilitate OOD prevention efforts. In this brief, we will summarize the various kinds of reforms that have been implemented (or could be implemented) in this realm, providing examples of existing efforts where appropriate. Each country, and each individual program, should consider this menu of options when determining its advocacy and other action priorities. The Landscape for Policy and Legal Interventions 1. Improving the Naloxone Supply Chain Naloxone is a cheap, effective opioid agent whose sole purpose is to block the effect of other opioids, like heroin. It is the standard of care for reversing opioidinduced respiratory depression in the emergency medical setting. It is available in liquid form, used for injection and intranasal administration, as well as sublingual administration reportedly available in China. The acceptance and availability of naloxone as the standard medical agent to reverse OOD is widespread, but not universal. As a prescription pharmaceutical medication that is not a controlled substance, the legal supply of naloxone is predicated on the official approval of the drug to that country. In others, the drug may be approved, but is not available for distribution. The flow of naloxone supply to the points of its sale, distribution, or utilization in emergencies may be a complicated process, fraught with legal, logistical, and economic problems. The following policy processes may be helpful in addressing these issues: A. Inclusion of naloxone into the national registry of medical drugs that are approved for use and sale in the country, B. Inclusion of naloxone into the national list of essential medicines for the country, NATIONAL FORMULARY OF REGISTERED C. Inclusion of naloxone among the DRUGS, KAZAKHSTAN (2002) standard formulary of drugs available LISTS INJECTIBLE FORMULATION OF at key institutions, including NALOXONE AS A DRUG THAT IS APPROVED pharmacies, outpatient medical clinics, FOR DISTRIBUTION, SALE, AND USE drug treatment (and methadone maintenance treatment) centers, ambulances, hospital emergency departments, and correctional settings, D. Long-term commercial contractual agreement or government mandate assuring steady and cheap supply from a reliable manufacturer and supported through a donor agency, foundation or government. Although it may be possible to conduct pilot OOD activities involving naloxone without undertaking the last four of these efforts, sustained and appropriately scaled operations require attention to supply chain management. Securing these policy shifts requires coordinated national-level or institutional-level advocacy, including members of the community, naloxone manufacturers, public health and medical professionals, and domestic and international legal experts. Drug manufacturers should be recruited to carry the brunt of the costs associated with improving supply chains. 2. Ensuring Effective Emergency Response by Healthcare Providers The deterioration and failure to reform the governance, financing, and supply chain management of healthcare systems has created serious problems in the delivery of emergency care in many regional settings. In the context of OOD reversal, this includes the provision of effective, timely aid to overdose victims in emergency rooms and by ambulance staff. Research suggests healthcare providers may have low knowledge of OOD and its treatment; their actions may also be shaped by poor attitudes toward drug using populations. Among the policy reforms that may be useful in addressing these problems are: A. Ensure effective overdose care by healthcare providers in emergency situations by improving knowledge and incentive structures: 2 o Amend formal medical “standards of care” and protocols for hospitals, ambulance workers, and other medical providers who may respond to OOD to include the provision of naloxone, o Change policies to ensure that procedures that are necessary to provide effective OOD PRIKAZ NO140, MOH, RUSSIA response are included among 1. DEFINES AND CLASSIFIES OOD FOR services billable (and actually MEDICAL PROFESSIONALS AND reimbursed) by the third party EMERGENCY RESPONDERS payers (national or other 2. DESCRIBES DIAGNOSTIC PROCEDURES health insurance schemes), AND PROTOCOLS o Change policies or curriculum 3. STIPULATES USE OF NALOXONE TO to recommend or mandate REVERSE OOD overdose prevention and response training for medical students, emergency medical technicians (EMTs) and active key medical personnel in areas with heightened population rates of OOD. B. Ensure the stocking of naloxone by key response institutions: o Change policies to require the inclusion of naloxone in the formulary of drugs that are stocked by the specific hospital, clinic, treatment organization, correctional institution, or ambulance service, o Change policies to monitor the actual inclusion of naloxone in key response settings. C. Facilitate timely emergency medical response: o Change policies to shield OOD victims and witnesses who call for help from criminal prosecution for drug possession or related charges, o Change policies to exclude police escorts from accompanying ambulances responding to OOD calls. o In some areas certain classes OOD PREVENTION LAW, of EMTs may not be authorized US STATE OF NEW MEXICO to administer naloxone (or other 1. LIMITS CRIMINAL LIABILITY FOR DRUG prescription medications), even POSESSION FOR VICTIM AND if it is available and legally WITNESSES OF OOD WHO CONTACT possessed by the victim; EMERGECY RESPONSE SERVICES allowing low-level EMTs to 2. LIMITS THE USE OF EVIDENCE THAT administer naloxone could be EMERGES FROM EMERGECY CALLS an additional policy directive. ABOUT OOD IN CRIMINAL CASES In addition to the above interventions, programs may also consider wider activities to facilitate the improvement of ambulance and other emergency services in the community, including working with governmental and donor organizations on training, infrastructure, and funding of these services. Efforts to boost general provider knowledge, attitudes, and practices related to drug user 3 health can facilitate more effective OOD response. Engaging medical providers and their organizations is key to the success of efforts in this realm. 3. Facilitating OOD Prevention by NGOs and Individuals In view of the supply chain and government PRESCRIPTION DRUG FORMULARY, response failures, harm reduction NGOs in the REPUBLIC OF GEORGIA region have responded to the crisis by instituting NALOXONE IS NOT INCLUDED training and naloxone distribution programs. This AMONG THE LIST OF PRESCRIPTION has included initiatives that distribute naloxone DRUGS, MAKING IT AVAILABLE directly to the users, those that provide OVER-THE-COUNTER prescriptions to outreach workers who, in turn, distribute the drug, and those that refer users to government clinics or pharmacies for purchase or dispensation of free doses of naloxone. The specific program design is often shaped by the legal and policy environment. Factors complicating efforts to improve peer access to naloxone includes naloxone’s prescription status, facility licensing for naloxone storage and dispensation, police interference, along with many others. The interventions listed below can help to improve the impact and facilitate the scale-up of these programs: A. Improve lay lifesaver access to naloxone: o Change professional or commercial policies to mandate the inclusion of naloxone in pharmacy inventory, including working with pharmacy chains, o Change in prescription status of naloxone by excluding it from the list of drugs available only by prescription (List B in most countries), o Provide for anonymous prescription or standing orders for prescription of naloxone, PRIKAZ NO327, MOH, RUSSIA (1999) reducing the need to involve 1. ALLOWS ANONYMOUS TREATMENT OF medical providers in naloxone DRUG USERS distribution. 2. SETS UP A FRAMEWORK FOR B. Facilitate NGO program operations: ANONYMOUS PRESCRIPTION OF o Procure licensing for NGO MEDICINES (NALOXONE) USING BLANK programs to purchase, store, and PRESCRIPTION CARDS TO BE FILLED dispense naloxone, OUT BY ALLIED MEDICAL STAFF o Change licensing laws to (OUTREACH WORKERS) eliminate or substantially lessen requirements for NGOs to obtain licensing to purchase, store, and dispense naloxone, o Change laws and operational police policies related to naloxone dispensation to reduce police interference with naloxone distribution programs, o Change policies to recommend or mandate police training on laws and operational procedures related to naloxone distribution. C. Encourage the use of naloxone by lay lifesavers in the community, 4 o Create or modify good Samaritan legislation (shielding from criminal and civil POLICE FIELD OPERATIONS MANUAL, NEW responsibility for any YORK CITY POLICE DEPARTMENT negative consequences), 1. DESCRIBES OOD PROGRAMS o Change institutional policies 2. DESCRIBES THE LAW RELATED TO to recommend or mandate NALXONE POSSESSION AND USE drug user training in 3. OUTLINES PROCEDURES RELATED TO naloxone use, first aid, and CONTACT WITH A TRAINEE OF OOD other OOD prevention PREVENTION PROGRAMS techniques, especially in key 4. DESIGNED TO ACCOMPANY TRAINING settings such as drug FOR CADETS AND OTHER OFFICERS ON treatment and corrections. OOD o Change laws or operational police policies related to naloxone possession or administration to reduce police interference with lay lifesaver activities. o Create policies recommending or mandating police training on policies and procedures related to lay lifesaver activities. o Incorporate overdose response in broader health education initiatives aimed at the general population. D. Encourage providers to participate in OOD prevention, including prescribing naloxone o Create legal protection to prescribers to facilitate participation in OOD prevention programs, including laws shielding them from criminal or civil responsibility from lay lifesaver activities, o Change reimbursement schemes to make screening for overdose risk, naloxone prescription, OOD education, and refills and followup care billable services, o Amend formal medical “standards of care” and protocols for hospitals, drug treatment clinics, MEDICAL BOARD POSITION STATEMENT, US correctional institutions, and other STATE OF NORTH CAROLINA key settings where naloxone 1. RECOGNIZES NALOXONE prescription and dispensation is PRESCRIPTION AS AN ACCEPTED feasible to cover these activities, MEDICAL SERVICE TO PREVENT OOD o Change professional licensing or 2. RECOMMENDS NALOXONE education policies to mandate or PRESCRIPTION TO KNOWN AND recommend provider training on SUSPECTED OPIOID USERS naloxone prescription as a way to prevent OOD. o Provide funding for development and dissemination of continuing medical education (CME) credits on naloxone-based overdose prevention for clinician accreditation. Prevention of OOD in the community requires a holistic approach, including improving medical infrastructure, supply chain for naloxone, and broader awareness and capacity in the community to respond to OOD events. National, regional, and institutional policy reform can help facilitate these efforts and 5 improve the impact of existing OOD prevention initiatives. Most importantly it has to be a key aspect of the strategic planning process in expanding and scaling-up pilot programs. 6