Word Doc
advertisement

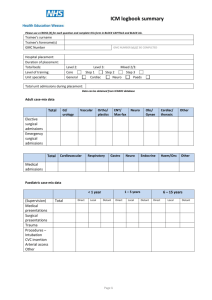
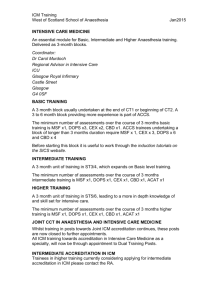
Intensive Care Medicine training The start of a journey Dr CM Oliver, CT2 Anaesthetic trainee. Princess Alexandra Hospital NHS Trust. Dr R Saha, Consultant Anaesthetist and Intensivist. Princess Alexandra Hospital NHS Trust. Correspondence: rajnish.saha1@pah.nhs.uk Introduction The creation of the Faculty of Intensive Care Medicine (FICM) last year was hailed as a “starting point …not a destination” [1]. However whilst it remains to be seen whether the Faculty will evolve into a College of Intensive Care Medicine, what is certain is that the foundation of the FICM signifies the introduction of sweeping changes to the way individuals will train in Intensive Care Medicine (ICM) in the UK. The current structure of ICM training Since 1999 it has only been possible to be awarded a Certificate of Completion of Training (CCT) in ICM when jointly undertaken alongside training in a parent specialty (Anaesthesia, Emergency Medicine, General Internal Medicine or Acute Surgery). Despite Anaesthesia being the commonest parent specialty historically, increasing numbers of medical trainees are entering ICM training. The competency-based joint CCT in ICM consists of: Training in ICM Training in the complementary acute specialties of Anaesthesia and/or GIM such that all trainees have at least six months experience in each. Obtaining a CCT in one of the four primary specialties. The minimum duration for CCT in ICM is five years once at ST3 which, in addition to primary specialty training typically comprises six months of dedicated ICM training (Step One) and a single block of twelve months ICM training within the final two years of specialist training (Step Two). The future of ICM training The General and Specialist Medical Practice Order 2003 founded the Post Medical Education Training Board (PMETB) [2]. The Order recognises ICM as a single separate specialty requiring a single standalone CCT Programme. This is to be implemented in August 2011. The GMC has agreed that dual CCT training with a parent specialty will remain acceptable, but with the creation of a standalone CCT it is likely that dual accreditation will result in the temporal extension of training. Entry to Higher Training ICM trainees will enter ICM higher training through one of the three core training routes; Acute Care Common Stem (ACCS), Core Anaesthetic Training (CAT), or Core Medical Training (CMT). Entry into higher training will occur at ST3 level by a competitive process and will require successful completion of a relevant primary examination: FFICM (Fellowship of the Faculty of Intensive Care Medicine) Part I FRCA (Fellowship of the Royal College of Anaesthetists) Part I MRCP (UK) (Membership of Royal College of Physicians) MCEM (Membership of the College of Emergency Medicine) Part A However once the FFICM examination becomes established it is likely to become an essential requirement for entry into higher training. Future CCT ICM Curriculum A four part curriculum comprising a handbook, assessment system, syllabus and competencies has been drafted by the FICM [3]. The competency based curriculum is derived from the CoBaTrICE (Competency Based Training programme in Intensive Care Medicine for Europe) syllabus of the European Society of Intensive Care Medicine (ESICM). During the seven year CCT programme trainees will progressively build a portfolio of evidence to demonstrate that they have mastered ninety seven competencies in the twelve following domains: Resuscitation and management of the acutely ill patient Diagnosis, Assessment, Investigation, Monitoring and Data Interpretation Disease Management Therapeutic interventions/ Organ support in single or multiple organ failure Practical procedures Peri-operative care Comfort and recovery End of life care Paediatric care Transport Patient safety and health systems management Professionalism Competencies will be assessed using Work Place Based Assessment (WPBA) tools and mapped to the four domains of good medical practice: Knowledge, skills and performance Safety and quality Communication, partnership and teamwork Maintaining trust Assessment The Annual Review of Competence Progression (ARCP) will be a formal assessment of a trainee’s progress. The FICM is developing an e-Portfolio to assist trainees to record their progress. Table 1 sets out the evidence a trainee may need to provide at an ARCP for Stage One Training. Log book procedures A total of more than 15 to reflect choice of DOPS. Evidence of progression/successful completion. Log book cases Unit Admission data allows yearly leaning outcomes to be fulfilled Individual cases provide suitable case mix to achieve yearly learning outcome. Log book Airway skills A total of more than 15 cases with evidence of progression of skill. Exam Possession of one of the designated core exams is needed for entry to ST3. Educational Supervisor report Satisfactory report. Audit At least 1 audit completed during each stage of training. Expanded Case summaries 2 cases (at least Level 2 standard). WPBA At least 5 general ‘Top 30’ cases as CBDs, CEX or both. Up to 5 CoBaTrICE competencies can be covered in each assessment. DOPS: chosen to reflect agreed CoBaTrICE competency assessments. MSF: 1 per year. Morbidity and Mortality meetings Journal clubs Attend at least 4 and evidence of reflection from 1 meeting. External meetings as approved in Personal Development Plan Reflection on content. Management meetings No mandatory requirement but attendance encouraged. Present at least once. Table 1 Assessments at ARCP Examinations Presently trainees have the option of sitting the UK Diploma in Intensive Care Medicine (DICM) or the European Diploma in Intensive Care Medicine (EDIC), the examination of the European Society of Intensive Care Medicine (ESICM). Although these qualifications are not currently compulsory for attainment of CCT in ICM, there has been an exponential rise in the number of candidates sitting both examinations in recent years and job descriptions for consultant appointments increasingly cite them as desirable or essential requirements. An inevitable development in the evolution of ICM training is the creation of examinations for trainees to become Fellows of the Faculty of Intensive Care Medicine (FFICM). Becoming a FFICM will become a compulsory requirement to obtain a CCT in ICM, effectively replacing the DICM and it is likely to impact on the number of UK candidates sitting the EDIC. The FFICM will be a two part examination with the Part 1 Primary examination being developed during 2012 – 2014. This is expected to comprise a total of ninety questions to be attempted over three hours. Forty questions will be in multiple choice format and twenty-five questions each in single best answer and extended answer formats. The examination will be taken at any stage of training before ST3. The Final examination will be taken after ST4 and is expected to comprise three sections- MCQs, Objective Structured Clinical Examination (OSCE) and Structured Oral Examination (SOE). The Final FFICM MCQ will follow the format of the Primary FFICM exam and it will be possible to carry over a pass in the MCQ component of the examination for three subsequent sittings of the OSCE and SOE. Conclusion Despite its historical ties with anaesthesia, a successful training programme affording non-anaesthetists improved access to ICM training has been established. A cultural shift has now paved the way for a move to a separate stand alone ICM CCT. Whilst the possible decrease in trainees with airway skills is viewed by some as a route fraught with danger, it is hard to dispute the benefits of a broadened skills mix in the multi-disciplinary environment of the Intensive Care Unit. That ICM should not remain a subspecialty is increasingly gaining support in the UK and Europe and it remains to be seen if the foundation of the FICM represents the starting point of a journey towards the creation of a College of ICM. What is certain is that for trainees embarking on their ICM careers, it is the start of an exciting and challenging journey. References [1] Bion J. News from the FICM. RCoA Bulletin 2011; 65; 15. [2] The General and Specialist Medical Practice (Education, Training and Qualifications) Order 2003. [3] Curriculum for a CCT in Intensive Care Medicine. 3rd. Edition. The Faculty of Intensive Care Medicine. 2011.