- humans ingest more proteins than needed for replacement of
advertisement

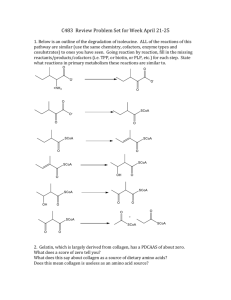
- humans ingest more proteins than needed for replacement of endogenous proteins; excess amino acids can’t be stored catabolized; - figure 1, 18-2 - any amino acid that can be degraded to pyruvate or citric acid cycle intermediate can serve as precursor in liver for synthesis of glucose (glycogenic or gluconeogenic) - some amino acids (try, phe) only part of their carbon skeleton can be used to synthesize glucose because the remainder is converted to acetyl CoA that cannot be used in synthesis of glucose - leucine is solely ketogenic its only endproduct is acetyl CoA - asparagines deaminated aspartate; proline ring opened to glutamate Alanine – most important amino acid precursor for synthesis of glucose; catabolized in a single step by transamination to yield pyruvate (reversible); ala is product of glycine and serine degradation Arginine- formed in urea cycle split into urea and ornithine; complete catabolism yield alphaKG via glutamate Aspartate – converted to oxaloacetate in single step via transamination; formed from asparagine; formed from oxaloacetate Glutamate – converted to and from alpha-KG via transamination or glutamate dehydrogenase Glutamine – deaminated to glutamate via glutaminase; produced from glutamate via glutamine synthetase Glycine- interconverted with serine through donation/acceptance of carbon via N5N10-methylene tetrahydrofolate (THF); serine/glycine converted to pyruvate via alanine; glycine formed from and degraded to NH3 and CO2 with N5N10-methylene tetrahydrofolate (THF) providing 2nd carbon 1. Metabolism of phenylalanine and tyrosine and associated disorders Metabolism of phenylalanine and tyrosine - phe is an essential amino acid; undergoes catabolism via tyrosine via phenylalanine hydroxylase (O2 H2O) - feature common to amino acid catabolism 1. production of organic acid intermediates 2. requirement of a cofactor for pathway function 3. inborn errors of metabolism at multiple steps - tetrahydrobiopterin (BH4), cofactor, is regenerated from dihydrobiopterin (BH2) that is reduced with NADPH (goes to NADP+) via dihydropteridine reductase; BH4 also cofactor in hydroxylation of tyrosine to L-dopa (via tyrosine hydroxylase) in synthesis of catecholamines or pigment 2. - most cell tyrosine transaminated to p-hydroxyphenylpyruvate (via tyrosine aminotransferase) homogentisate maleylacetotacetate (via homogentisate oxidase) fumarylacetoacetate Phenylketonuria (PKU) - most common inborn error of amino acid metabolism (1:10000 individuals) - defective phenylalanine hydroxylase elevation of phenylalanine in blood permanent neurologic damage - accumulation of phe production of phenylpyruvate (formed via transamination of phe), phenyllactate (reduction of phenylpyruvate), and phenylacetate (formed via oxidative decarboxylation of phenylpyruvate); these show up in urine - blood phe levels can be reduced with dietary restriction; newborns screened - toxic effects of phe may be caused by reduced uptake and metabolism by the brain of other aromatic amino acids reduction in protein synthesis - tyrosine deficiency hypopigmentation (light skin/eyes) - diminished phenylalanine hydroxylase activity can also be caused by defect in tetrahydrobiopterin synthesis more serious than just PKU because BH4 is also a cofactor two enzymes in NT synthesis, serotonin and dopamine Tyrosinemia type II/Richner-Hanhart syndrome - defect in tyrosine aminotransferase blood tyrosine elevation - tyrosine crystals in tissue due to exceeding solubility; in cornea, plasma, and soles Alkaptonuria - defect in homogentisate maleylacetotacetate (via homogentisate oxidase) - large amounts of homogentisate in urine; deposited in cartilage polymerization black ears; produces arthritis Albinism - defective tyrosine hydroxylase (tyrosine L-Dopa); doesn’t alter catecholamine synthesis because tyrosine hydroxylase in that pathway is an isoenzyme product of different gene 3. METABOLISM OF METHIONINE AND CYSTEIN, AND DISORDERS Methionine and cysteine metabolism - first step is condensation of met with ATP S-adenosylmethionine (SAM) via methionine adenosyltransferase - SAM donates methyl group for creatine, epinephrine, polayamines, phosphatidylcholine (found in neural membranes), and sphingomyelin (myelin sheath component) synthesis - SAM donates methyl group production of S-adenosylhomocysteine cleaved to homocysteine and adenosine 4. - homocysteine can be converted back to met via cobalamin (vitamin B12) containing enzyme methionine synthase - active form of cobalamin (methylcobalamin) donates methyl group to homocysteine met; methylcobalamin (methyl-B12) regenerated from hydroxycobalamin (hydroxy-B12) by accepting methyl group from N5-methylTHF (goes to THF); vitamin B12 and folate participate; takes place in cytoplasm - homocysteine can also be metabolized to cystathione by action of cystathione-beta-synthase (requires pyridoxal phosphate as prosthetic group cofactor, which also acts in glycogen phosphorylase and transaminases) - cystathione cleaved to form cysteine, NH3, and alpha-ketobutyrate by action of cystathionase - cysteine from cystathionase converted to pyruvate and sulfate (SO4, which is the majority of sulfate excreted in urine) -alpha-ketobutyrate proprionyl CoA via oxidative decarboxylation requiring NAD (CO2 also produced); propionyl CoA succinyl CoA (endproduct of met metabolism); succinyl CoA can also come from isoleucine and valine 5. Disorders of methionine and cysteine metabolism Homocystinuria - defect in cystathione-beta-synthase; can be caused by pyridoxine deficiency; leads to increased blood levels and urinary excretion of homocystine - homocysteine accumulates in blood and excreted in urine where it forms disulfide bond with another homocysteine homocystine; homocysteine’s reactive sulfur group allows it to form disulfide bond with many proteins - tall patients, dislocation of ocular lenses, retardation - folate or vitamin B12 deficiency results in homocystinuria due to reduced activity of methionine synthase (to result in met) - arteriosclerosis patients have high plasma [homocysteine] - B vitamins decrease plasma homocysteine concentration; people with low plasma B vitamin levels and low intake of B vitamins have increased heart disease risk; folate/B12 deficiencies common in populations at high risk for heart disease (smokers, alcoholics) - may involved oxidative damage to lipoproteins and endothelia (impaired platelet function) 4.,5. METABOLISM OF COBALMIN, AND DISORDERS - in mitochondria conversion of methylmalonyl CoA succinyl CoA via methylmalonyl CoA mutase; uses adenosylcobalamin (adenosyl-B12); - methylmalonyl CoA provided by proprionyl CoA via proprionyl CoA carboxylase (biotin is cofactor); succinyl CoA enters citric acid cycle in mitochondria - methyl group of SAM used in many synthetic reaction (mentioned above); homocysteine can receive a methyl group from methylcobalamin met; source of methyl group for methylcobalamin is N5-methylTHF, which is generated from folate intermediates that get methyl groups from other sources - vitamin B12 deficiency accumulation of N5-methylTHF methyl groups trapped (affects DNA synthesis); deficiency also reduces availability of adenosylcobalamin for methylmalonyl CoA mutase methylmalonic aciduria (can also be caused by defect in methylmalonyl CoA mutase, defective binding of adenosylB12) and homocystinuria - appearance of homocystine and methylmalonic acid in urine secondary deficiency of vitamin B12 - methylmalonic aciduria proprionyl CoA accumulates with methylmalonyl CoA 6. METABOLISM OF BRANCHED-CHAIN AMINO ACIDS, AND DISORDERS Branched-chain amino acid metabolic pathways - branched-chain amino acids leucine, isoleucine, and valine (essential amino acids) - first step in their catabolism is reversible transamination amino group transferred to alphaKG to form glutamate - second reaction irreversible oxidative decarboxylation (similar to pyruvate dehydrogenase) catalyzed by branched-chain dehydrogenases for each of branched-chain alpha-ketoacids CoA derivatives of each branched-chain ketoacid; irreversible reaction humans can’t form branched-chain amino acids from basic starting materials; amino acids can be produced from ingested alpha-ketoacid - ultimately, leucine is converted to three molecules of acetyl CoA; one reaction requires biotin 3-methylcrotony-CoA carboxylase (needs biotin and ATP) - isoleucine and valine form succinyl CoA; isoleucine proprionyl CoA methylmalonyl CoA via carboxylation by proprionyl CoA carboxylase (requires biotin and ATP, like all carboxylases); defect in proprionyl CoA carboxylase accumulation of proprionyl CoA which reacts with citrate synthase to from methylcitrate (inhibitor of citric acid cycle) -when biotinidase is defective biotin cannot be feed and biocytin is excreted in urine; dysfunction of carboxylase enzymes; can result in neurological impairment Maple syrup urine disease - also branched-chain ketonuria - defect in branched-chain alpha-ketoacid dehydrogenase complex (like PDH) - most common is defect in ketoacid decarboxylase (2nd reaction); requires thiamine diphosphate; thiamine deficiency can cause maple syrup urine disease - name from odor of branched-chain ketoacids - branched-chain ketoacids also elevated in blood because transamination is irreversible - infant lethargic, mentally retarded