Notes - Austin Community College
advertisement

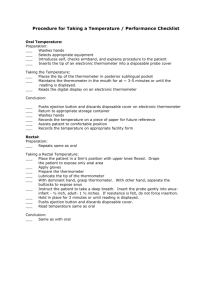
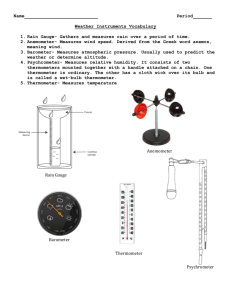
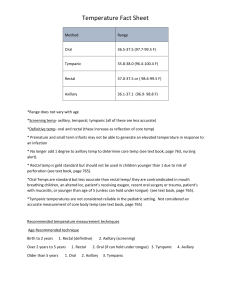
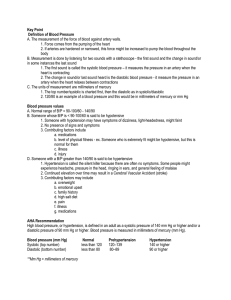
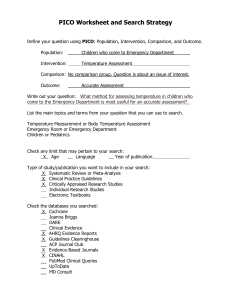
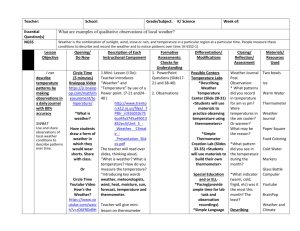
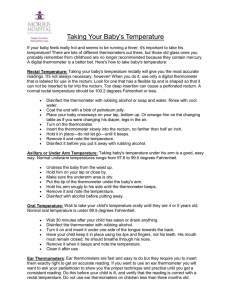
Learning Supplement Vital Signs – Body Temperature Definition Body temperature is the balance between heat produced in the body and heat loss from the body. Temperature-Regulating System The balance between heat produced in the body and heat loss from the body is maintained by the process of thermoregulation. Thermoregulation is psychological or physiological. Psychological Psychological regulation occurs when an individual perceives he is hot or cold. If a person perceives he is cold, he then puts on a sweater. Physiological The main physiological system regulating temperature is the autonomic nervous system. Receptors in the skin, abdomen, and spinal cord send messages to the autonomic nervous system that then sends it to the hypothalamus. The hypothalamus acts as a central thermostat, receiving input from sensors that detect hot or cold temperatures. When an individual’s set-point temperature (temperature that thermoregulatory mechanisms attempt to maintain) increases, a message is relayed to the hypothalamus, which initiates body responses that decrease heat production and increase heat loss. Heat Loss The four main avenues of heat loss are: Radiation, Conduction, Evaporation, and Convection. 1. Radiation Transfer of heat from the surface of one object to the surface of another without contact. Blood flows from the core internal organs carrying heat to skin and surface blood vessels. Amount of heat carried to the surface depends on the extent of vasoconstriction and vasodilation regulated by the hypothalamus. About 85% of the bodies’ heat is loss via radiation to the environment when heat leaves the body going to a cooler surface in the environment. 2. Conduction Transfer of heat from one object to another with direct contact. When the warm skin touches a cooler object, the heat leaves the body to the cooler surface. The amount of heat conducted from the body can be increased by applying an ice pack or bathing with cool water. The opposite can take place, a person can decrease the amount of heat loss by applying warm blankets and not allow the body to come into direct contact with a cooler surface. The body can actually gain heat via conduction when contact is made with a warmer object. 3. Evaporation Transfer of heat when a liquid is changed to a gas. When the body temperature rises, hypothalamus signals the sweat glands to release sweat. Sweat evaporates from the skin, resulting in heat loss. Same principle applies with bathing. Heat is loss with water on the skin. 4. Convection Transfer of heat away by air movements. Heat leaves the body to cooler air currents that carry away the heat. An electric fan promotes heat loss through convection. Heat Conservation The body conserves heat via Vasoconstriction. If there is a decrease in the amount of blood that reaches the surface of the body, then there is not as much heat that can be released or lost. Heat Production Heat is produced in the body by: a. Increase Basal Metabolism Rate b. Muscle contraction c. Shivering Average Ranges Normal values of body temperature differ with age groups. Children, adults, and older adults all have average ranges for each of these groups. Children: 98.6 – 99.6 degrees F, oral Adults: 98.6 +/- 1 degree F, oral Older Adults: 97.6 +/- 1 degree F, oral Normal values for rectal body temperature is usually 1 degree higher than the oral and an axillary body temperature is 1 degree lower than the oral temperature. Terms Related to Temperature An elevation in body temperature is known a pyrexia, hyperthermia, or fever. A very high fever (105.8 F) is called hyperprexia. The patient who has a fever is referred to as febrile; the one without a fever is afebrile. A decreased body temperature below normal ranges is known as hypothermia. Interpreting the Temperature After taking the temperature, the nurse needs to analyze the data and make a nursing decision. The decision does not come from a single value. Rather, the nurse needs to look at the relationship of the vital signs to each other, to previous findings, and to other assessment findings. If the temperature is above or below the normal range, the nurse should notify the physician. They should also reassess the temperature more often than ordered. Usually a patient has orders that specify the frequency to measure temperature and parameters in which to notify the physician. If a patient’s temperature changes, you may need to reassess more often than the order requires. This is a nursing intervention. Factors that Affect an Individual’s Temperature 1. Age 2. Activity / Exercise/ Sleep 3. Hormones 4. Stress 5. Environment 6. Medication 7. Illness Sites / Method for Measuring Body Temperature There are a number of sites for measuring body temperature. The four most common methods are oral, rectal, axillary, and tympanic. Oral – it is the most common and convenient site with large vascular supply. The sublingual pocket under the tongue responds very quickly to changes in core temperature. A disadvantage is the temperature can be inaccurate if the patient has just ingested hot or cold food, is smoking, chewing gum, or if the patient breathes through the mouth. Oral thermometers are not considered safe for infants, children, elderly, disoriented, epileptic, or unconscious patients. Rectal – is the most reliable measurement. The major disadvantages are it is more unpleasant for the patient and inconvenient to gain access to the site. Rectal temperatures do not respond to body temperature changes quickly, it cannot be used with rectal surgery, and stool in the rectum can interfere with thermometer placement that can lead to an inaccurate temperate reading. Axillary – is the safest, most noninvasive, and easily accessible. The major disadvantage is that a glass thermometer must be left in place for a long time to obtain an accurate measurement. Does not always give a true reading of core temperature. It is used for infants, children, patients, with oral problems, patients breathing through their mouths, and irrational patients. Tympanic – is readily accessible, minimal discomfort, and reflects the core temperature. Major disadvantage is the cost of the equipment and inaccurate reading related to incorrect positioning of the instrument. Types of Thermometers There is a wide variety of thermometers available today. The most commonly used in the clinical setting is the electronic probe. Electronic probe – battery operated unit with an attached heat sensitive probe and disposable probe cover. This thermometer has a more rapid reading of the body temperature. Can be used in all methods of assessing temperature. Tympanic Thermometer – infrared light reflectance thermometer determines the temperature of the tympanic membrane by measuring heat radiated as infrared energy from that site. Because the hypothalamus and the tympanic membrane share the same vasculature, the temperature measured reflects the core temperature. Accuracy depends on placement of the probe in the ear. Temperature sensitive tape – provides a generalization of body temperature and is not an accurate measurement of the body temperature. If a temperature elevation is noted, a more accurate measurement can then be obtained. Should be placed on dry skin, the forehead is the most common site. A color change on the tape is used to indicate the approximate body temperature. Chemical in glass thermometer - measures the temperature by the movement of chemical through the calibrated glass. This type of thermometer is no longer in general use, but may still be found in some health care settings. IV. Student Activity in the Lab 1. Practice taking a temperature with electronic thermometer on classmates following correct procedure. Refer to the procedure in your textbook. 2. Chart the temperature on a graphic record and in the descriptive notes. 3. Participate in simulated experiences.