Enteral Workshop – suggested answers
advertisement

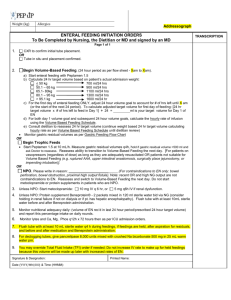
Enteral Workshop – suggested answers Group 1 –Case study #1 Convenor: Equipment required: 1) 55 copies of case study #1 2) White board/ white board marker 3) Calculator/pen Related Learning Outcome: - be able to plan an appropriate enteral feeding regimen - understand the management of NGT feeding regimen - be able to calculate the nutritional requirements for differing medical conditions - understand the nutrition management of refeeding syndrome Case: Alice is an 80-year-old female admitted from a nursing home a right sided stroke. She has been assessed by the Speech Pathologist as not appropriate for oral intake and to be NBM. 1) Where will you get details regarding her anthropometry? Nursing home, family, estimate You establish that her weight is 45kg, and her height is 5ft 4” 2) Calculate her estimated energy and protein requirements (include all working out) Height 163cm Weight 45kg BMI 16.9kg/m2 (underweight++) IBW 58kg! Comment on BMI, use of actual vs ideal body weight and when each might be used. Energy Harris benedict: 2741 + 1800 + 1255 – 1568 = 4228kJ/1010kcal X AF + IF= 1.4 = 1414kcal/day (31kcal/kg) Schofield: 1.71 + 2.755 = 4.465MJ/1067kcal X AF + IF = 1.4 = 1495kcal/day (33kcal/kg) Protein: 1.0-1.2g/kg= 45-54g/day 3) Calculate an appropriate enteral feeding regimen including starting regimen, water flush, and plan for progression to goal rate. NB: Consider intake hx, especially given weight ?refeeding risk - - - - - Refeeding risk: Depending upon recent diet hx, assuming no information commence thiamine supplement prior to commencing enteral formula, baseline EUC/CMP and supplement if required. Once position of tube confirmed by medical officer and documented ok to start: 20mL/hr 1kcal/mL with fibre formula x 24/24, 50mL water flush 4/24 plus IVT. Organise daily bloods for EUC/CMP. Check bloods, if normal increase by ~250kcal per day (10mL/hr). If not, keep formula at same rate and supplement where required. Continue this daily until goal 55-60mL/hour x 24/24. If NUMF @ 55ml/hr = 1320ml, 1320kcal, 53g protein (1.2g/kg), 57mmol Na/50mmol K+, 20g fibre or if NUMF @ 60mL/hr = 1440kcal/6025kJ (32kcal/kg) , 58g protein (1.3g/kg), 62mmol Na/55mmol K+, 22g fibre. If patient was definitely not at risk of refeeding: Once position of tube confirmed by medical officer and documented ok to start: commence 1kcal/mL fibre formula at 30-40mL/hr x 4/24, if tolerated increase by 10mL ever 4/24 until goal rate reached (as above) Suggest 50mL water flush 4/24 = 1680mL total fluid/1450mL free water (32mL/kg), may need to slightly increase upon review. 4) Upon review: i) What are you checking? Initial assessment/nutrition care plan remains appropriate, has clinical condition changed etc. ii) What do you need to look at (include chart names)? Med chart, fluid balance chart, bowel chart, BGL chart (if appropriate), biochem, weight (if done) iii) Who do you need to speak with? Nurse, patient (if able)/family, doctor (if new issues) Enteral Workshop Group 2 –Case study #2 Convenor: Equipment required: 1) 55 copies of case study #2 2) White board/ white board marker 3) Calculator/pen 4) 55 copies of enteral formula composition (either chart or photocopy of company info for one company eg Nutricia) Related Learning Outcome: - be able to plan an appropriate enteral feeding regimen - understand the management of NJT/PEJ feeding regimen - be able to calculate the nutritional requirements for differing medical conditions - be able to describe the types of enteral nutrition formulae and plan an appropriate feeding regimen - have an appreciation of the issues with home enteral feeding Case: 1) List some clinical circumstances where postpyloric/jejunal enteral tube feeding may be required? Recurrent aspiration, persistent reflux/vomiting, pancreatitis, persistent large gastric aspirated in ICU despite prokinetics 2) What needs to be considered relating to the selection of an enteral formula when commencing a postpyloric/jejunal feeding? Osmolality: (a measure of the number of particles present in solution and is independent of the size or weight of the particles) and compare with plasma osmolality (normal osmolality in plasma is about 280 - 303 milliosmoles per kilogram) Volume: emphasis location of delivery Delivery method: commence with continuous feeding, may be able to grade over to bolus with time. Lucy is a 74-year-old female who is admitted with recurrent aspiration pneumonia due to Parkinson’s disease. She has a PEG and has been established on enteral tube feeding for approximately 12 months. The PEG is now going to have a jejunal extension due to the recurrent aspiration. Lucy usually mobilises with a stick and lives with her daughter and her family. Her weight is 54kg and height is 153cm. 3) Calculate her estimated energy and protein requirements (include all working out) Check previous enteral feeding regimen and weight hx (ie if stable potentially aim for same). BMI = 23.1kg/m2 Harris Benedict: 2738 + 40W + 7.5H – 20A = 2738 + 2160 + 1148 – 1480 = 4566kJ (1100kCal) X AF (1.3-1.4) + IF (1.1) = 1.4-1.5 = 6392-6849kJ (1540-1650kCal) Schofield: 38W + 2755 = 4807kJ (1145kCal) X AF + IF = 1.4-1.5 = 6730-7211kJ (1603-1718kCal) Protein: 59.4g (1.1g/kg) Fluid: 1603-1718ml (1ml/kCal) OR 1620ml (30ml/kg) 4) Calculate an appropriate enteral feeding regimen including starting regimen, water flush, and plan for progression to goal rate. Assume no refeeding risk: - Follow post-jejunal extension insertion instructions from gastroenterologist - Commence 1kcal/mL with fibre formula at 30mL/hr x 4/24, increase by 10mL/hr every 4/24 until goal rate 70mL/hr (may need to be slower). Water flush 50mL 4/24. - Discuss goal rate and potential issues re high volume, PEJ will not necessarily prevent aspiration pneumonia etc. - Need to discuss with medical team, and consider local protocol re feeding overnight. - Consider options re 1.5kcal/ml, 2.0kcal.ml formula but balance with osmolality. ? Nutrison Concentrated (470mOsm/kg H20) then goal only 35ml/hour x 24/24 or if 16/24 feeds 50-55mL/hr - Given this is Lucy’s sole source of nutrition long-term, particularly need to check against RDI and supplement micronutrient where required. 5) What will you need to do in order to organise Lucy for discharge? Check discharge destination, has the feeding regimen changed from prior to admission, organise education if required, contact daughter to advise of feeding regimen, organise follow-up (outpatient clinic or if for placement recommend NH organises dietitian consultation) Enteral Workshop Group 3 – Practical Aspects of Enteral feeding Convenor: Equipment required: 1) Enteral company names (Company Names Enteral & Parenteral doc in 2008 folder) 2) Enteral formula from each of four enteral companies to display (basic products eg 1kcal, 1.5kcal, 2.0kcal/mL with and without fibre, not specialised formula) 3) 5 x feeding pumps plus sets to fit formula (from Tyco) 4) Enteral formula for students ‘hands-on’ with pumps (5 x a ready-to-hang formula from each company) Related Learning Outcome: - be able to describe the types of enteral nutrition formulae - understand the management of feeding regimens Practical: - Enteral feeding company displays of enteral nutrition formulae (on table, set-up). Brief explanation re 4 companies and basic formula types/names. - Convenor to demonstrate set-up of enteral feeding pump (including formula, giving-set, priming line, setting rate) - Students to be in groups of 2-3 (total 5 pumps) for ‘handson’ experience of setting up enteral feeding pump Enteral Workshop Group 4 – Considerations and practical aspects of Home Enteral Nutrition tube feeding Related Learning Outcome: - have an appreciation of the issues with home enteral feeding See workshop 4 document handout.