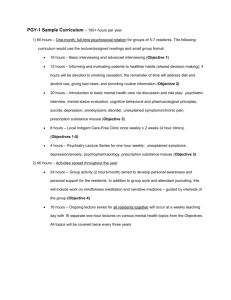
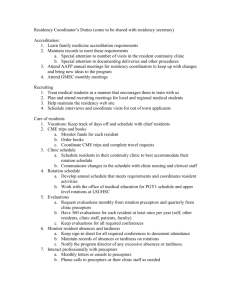
Role of Resident - School of Medicine
advertisement

Department of Medicine 2008-2009 Curriculum 2 A. General Information 1. Organization and Structure a. The Department of Medicine at the University of North Carolina at Chapel Hill provides an integrated, progressive experience for residents in their 36month training period. The goal of our curriculum is to prepare residents to be well-trained general internists. We believe this type of training not only prepares our residents for careers in General Internal Medicine but also provides the necessary foundations for further training as a subspecialist. The curriculum in the Department of Medicine changes greatly from the PGY-1 year to the PGY-3 year. The PGY-1 year consists of 9 months of inpatient rotations and 3 months of ambulatory medicine. During the second and third years, residents spend an increasing amount of time in the outpatient setting, so that by the time a resident is in the PGY-3 year, a majority of rotations occur in ambulatory medicine. The curriculum will be specifically described for each of the 3 years of training. The PGY-1 Year Competency- based Goals and Objectives The PGY-1 curriculum is taught in a series of monthly rotations linked with a number of Departmental teaching conferences. On all rotations the role of the PGY-1 resident is to serve as the primary physician for all of his/her patients. In this role the PGY-1 resident: 1. 2. 3. 4. 5. 6. Performs a history and physical examination on each new patient Enters all orders Communicates with the patient and ward team regarding daily progress Enters a history and physical and daily progress notes into the patient record Develops a diagnostic and therapeutic plan for each patient Enters a discharge summary into the patient record The monthly rotations for each PGY-1 resident are as follows: Cardiology/MICU - 2 months Inpatient General Medicine Ward - 2 months Inpatient Subspecialty Wards - 5 months Emergency Room - 1 month Same-Day Clinic - 1 month Ambulatory Elective-1 month Cardiology - consists of 30 beds covered by four teams. Each team is made up of 1 upper level resident and 1 PGY-1 resident. One faculty member and one subspecialty resident are assigned to each team to assist in patient management and to conduct teaching rounds. Didactic teaching rounds and bedside teaching occur daily. Also, there is a weekly core curriculum lecture series that is case-based. 2 3 A copy of the Cardiology Curriculum is included in Section 2. Common diagnoses of patients admitted to the cardiology service include myocardial infarction, arrhythmias, and chronic heart failure. Residents follow patients in the CCU (12 beds) and the general floor (20 beds). Residents on service place central lines including Swan Ganz catheters and perform arterial blood gases and thoracenteses. ICU - consists of 19 beds in a MICU. There are 4 teams, each team consisting of 1 upperlevel resident and 1 PGY-1 resident. One faculty member serves as attending in the MICU, another in the RICU. There is also a Critical Care Fellow. Teaching rounds include didactic presentations (30 min/day, 6 days/week), bedside teaching (2 hours/day, 7 days/week), and x-ray teaching (30 minutes/day, 6 days/week). There is a designated curriculum (Section 2). Patients admitted commonly have the following diagnoses: GI bleeding, septic shock, drug overdose, s/p cardiopulmonary arrest, DIC, COPD exacerbation, cystic fibrosis, rejection s/p lung transplant, and acute renal failure. Residents perform all procedures. Inpatient General Medicine - consists of 2 general medicine services. For each service, there is 1 attending, 1 upper level resident, and 2 PGY-1 residents. Teaching rounds occur for 1 hour, 5 times per week covering a number of topics described in the Inpatient General Medicine curriculum (see Section 2). Patients admitted have a variety of problems including: community -acquired pneumonia, COPD exacerbation, diabetic complications, and lupus complications. Residents perform all procedures. Also, residents rotate at Wake Hospital, a community hospital in Raleigh, NC. There are four teams consisting of 1 attending, 1 upper level resident and 1 resident. Teaching rounds occur for 1 hour five times per week covering topics in General Internal Medicine. Residents perform all procedures. Inpatient Subspecialty Wards Medicine Medicine Medicine Medicine Medicine Service A - Geriatrics B - Nephrology E - Hematology/Oncology G - Pulmonary K - Infectious Diseases # Beds 24 24 48 24 24 For each service there is one attending, one upper level resident, and two PGY-1 residents. Each of these services has daily work rounds and attending rounds. Each service has designated teaching time occurring at a minimum of 5 hours per week. During teaching time a series of topics pertinent to each service are reviewed. A copy of each curriculum is included in Section 2. Residents perform all procedures on these services. Emergency Room - faculty from the Department of emergency medicine supervise PGY-1 residents. PGY-1 residents have a generic experience seeing medical, surgical, and obstetrics/gynecology patients. There are four hours of didactic teaching per week, which cover a wide variety of topics. Examples of monthly topics are included in Section 3. 3 4 Same-Day Clinic - faculty in the Division of General Internal Medicine supervise PGY-1-3 residents. A variety of outpatient problems are encountered. Didactic teaching takes place daily for 30 minutes to 1 hour. Subjects covered in the curriculum are included in Section 3. This is a walk-in clinic for the established IM patients. Ambulatory Elective – PGY-1 residents spend one month on a subspecialty service of the Department of Medicine. Consultations are done on inpatients and outpatients and patients are also seen in subspecialty clinics. Division faculty provides faculty supervision. Curricula for each rotation are included in Section 3 Teaching Conferences - PGY-1 residents attend a series of Departmental Conferences. The daily work schedule is set up to allow PGY-1 residents to attend the conferences (Table 1). TABLE 1 UNC Department of Medicine - Schedule of Daily Activities Time 0700 0730 1000 1000 1100 1200 Monday Pre-Rounds Work Rounds Tuesday Pre-Rounds Work Rounds Wednesday Pre-Rounds Work Rounds Thursday Pre-Rounds Work Rounds Friday Pre-Rounds Work Rounds Residents Report Attending Rounds Core Curriculum Residents Report Attending Rounds Core Curriculum Residents Report Attending Rounds Intern Conference Residents Report Attending Rounds Grand Rounds/ Morbidity and Mortality Conference Residents Report Attending Rounds EBM Conference 4 5 Residents are expected to attend all conferences. The conferences are as follows: Monday – Residents Core Curriculum Conference - 1 hour Tuesday – Residents Core Curriculum Conference - 1 hour Wednesday - Interns Conference - 1 hour Thursday - Grand Rounds - 1 hour Friday - EBM Conference - 1 hour The content of some of these conferences is briefly described. Lecture topics are included in Section 4. Monday and Tuesday - Residents Conference - Faculty in the Department of Medicine presents a series of lectures covering focused topics. Wednesday - Interns Conference - A lecture series of Emergency Medicine Topics mixed with case-based group discussion. Thursday – Grand Rounds Thursday-Mortality and Morbidity–The morbidity and mortality conference centers on a subject relating to patient care in the department. The Vice-Chair of the department conducts this conference Friday – Evidenced Based Medicine Conference – An evidence-based medicine discussion of selected literature by both faculty and residents. The PGY-1 year ACGME Competencies Each PGY-1 resident must develop competence in the following: Patient Care Medical Knowledge Practice-based Learning and Improvement Interpersonal and Communication Skills Professionalism System-based practice In the context of the above rotations, competency is defined for each of the categories Patient care- medical interviews, physical examinations, review of data, procedural skills, diagnostic and therapeutic decision making Medical Knowledge – basic and clinical science, evidence-based medicine, literature searching 5 6 Practice-based Learning and Improvement – evaluation of own performance, incorporation of feedback, use of technology for patient care and self-improvement Interpersonal and Communication Skills – establishment of relationship with patients and families, education and counseling of patients, team skills with colleagues Professionalism – demonstration of respect, compassion, integrity, and honesty, commitment to self-assessment, acknowledges errors, considers needs of patients and colleagues System-based Practice – ability to utilize resources, uses a systematic approach to reduce errors and improve patient care These competencies are reviewed with all residents and faculty and serve as the foundation for monthly evaluation. 6 7 The PGY-2 Year Competency-based Goals and Objectives The PGY-2 year is also composed of a series of monthly rotations coupled with Departmental teaching conferences. On inpatient rotations the role of the PY-2 resident is to be in charge of ward team. In this role the PGY 2 resident: 1. 2. 3. 4. 5. Performs a history and physical examination on each new patient Reviews the treatment plan for each new patient with the PGY 1 resident Reviews the performance of MS 3 students Conducts daily work rounds Supervises all procedures On night float the resident assumes primary responsibility for the care of new patients in a role like that of the PGY 1 resident. Monthly rotations for a PGY-2 resident are as follows: 6. 7. 8. 9. 10. 11. 12. MICU – 1 month Cardiology - 2 months UNC Inpatient Medicine Ward – 2-3 months Ambulatory General Internal Medicine – 2-3 months Subspecialty Consultation – 2-3 months Wake Med – 1 month Night Float 2-3 2 week blocks Cardiology/ICU/Inpatient General Medicine Wards / Inpatient Subspecialty Wards- These have been previously described under the PGY-1 resident. The role of the PGY-2 resident on these services is supervisory. The PGY-2 resident evaluates all patients on service and the PGY-2 resident is integral in constructing a plan of care, which is carried out by the PGY -1 resident. Another major responsibility is teaching. The PGY-2 resident teaches and supervises medical students on these services. Ambulatory General Internal Medicine - PGY-2 residents can choose from several month blocks focusing on outpatient skills of the generalist. Some of the choices are: Wake Hospital Ambulatory Rotation Siler City - PGY-2 residents spend the month in a community setting, supervised by general internists. Subspecialty Consultation - PGY-2 residents can choose among any subspecialty in the Department of Medicine. Consultations are done on inpatients. Patients are also seen in subspecialty clinics. Division faculty provides supervision. Curricula for each rotation are included in Section 3. Night Float - PGY 2 residents report at 7 PM and until 7 AM and are responsible for the primary evaluation and management of all non-intensive care patients admitted to the Department of Medicine. At 7 AM the care of 7 8 those patients goes to the incoming team on call. The Attending Physician of the service provides supervision where the patient is admitted. Teaching Conferences - Like PGY-1 residents, PGY-2 residents attend a series of conferences, which are integrated with the daily work schedule. Some have been described previously including Monday Resident Core Curriculum Tuesday Core Curriculum, Thursday - Grand Rounds, and Friday Evidence Based Medicine. In addition, PGY-2 residents attend Morning Report. This is case-based with residents presenting unknown patients to their peers. The presenting resident completes his/her presentation with a review of a particular subject. This review like all presentations is posted on the internet so that residents my review this at their leisure. These conferences are coordinated by the Chief Residents. The curriculum is set by the chief resident. A list of topics discussed is included in Section 4. The PGY-2 Year ACGME Competencies Each PGY-2 resident must demonstrate competence in the following: Patient Care Medical Knowledge Practice-based Learning and Improvement Interpersonal and Communication Skills Professionalism System-based Practice Competency is defined as outlined above for PGY 1 residents and is used for the monthly evaluation of PGY-2 residents The PGY-3 Year Competency –based Goals and Objectives In many ways the PGY-3 year is similar to the PGY-2 year in that the residents function as described previously under the PGY-2 year, include teaching conferences. The rotations however, are different, and are as follows: 1. 2. 3. 4. 5. 6. Wake Med – 0-1 Month UNC Inpatient Medicine Wards – 1-2 months Same Day Clinic - 1 month Ambulatory General Internal Medicine – 2-3 months Subspecialty Consultations – 2-3 months Special Electives - 1 month 8 9 7. 8. MICU or Cardiology – 1 month 2-3 2 Week blocks night float Inpatient General Medicine Wards / Inpatient Subspecialty Wards - The role of the PGY-3 residents is identical to that described previously for the PGY-2 resident. Same –Day Clinic - The role of the PGY-3 residents is identical to that of the PGY-1 resident. Ambulatory General Internal Medicine - PGY-3 residents can choose from several month blocks including those described for PGY-2 residents. There are additional choices as follows: General Medicine Consults- PGY-2 or 3 residents see patients on other services, providing General Medicine Consultations. Supervision is provided faculty from the Division of General Internal Medicine. Geriatric Medicine - In a one-month block, PGY2-3 residents are exposed to outpatient management of this population. Faculty trained in Geriatrics provide supervision Subspecialty Consultations - The role of the PGY-3 resident is the same as described for the PGY-2 resident on those rotations. Special Electives - These rotations are designed to enhance individual training. Residents pick a faculty mentor to conduct clinical or basic research. Rotations at other institutions can also be done. The PGY-3 Year ACGME Competencies Each PGY-3 resident must develop competence in the following: Patient Care Medical Knowledge Practice-based Learning and Improvement Interpersonal and Communication Skills Professionalism Systems-based Practice Competency is defined as outlined above for PGY 1 residents and is used in monthly evaluation. 9 10 SECTION 2 INPATIENT CURRICULUM Cardiology Intensive Care Unit General Medicine Geriatrics Nephrology Hematology/Oncology Pulmonary Infectious Diseases Neurology 10 Section 2 Inpatient Curriculum General Each inpatient service has designated teaching time, previously described in Section 1. It is the responsibility of the division faculty to review a series of topics during the monthly rotation. The respective division generates these topics with input from faculty and residents as well as data supplied to each division from the preceding In-Training Examination. A dominant theme for these conferences is to review material a general internist must know about each discipline. The curricular goal for each resident is to have a working knowledge of these subjects. CARDIOLOGY INPATIENT CURRICULUM OBJECTIVE 1. Takes a history Demonstrates knowledge necessary to obtain an orderly history on patients suspected of having cardiovascular diseases and recognizes the importance of A. B. C. D. E. F. G. H. I. J. K. L. Dyspnea (resting, exertional, nocturnal, positional) Chest pain (specifically, what constitutes “typical angina) Edema Palpitations/arrhytbinias Exercise tolerance, semiquantitative History of hypertension and u~eatrnent History of rheumatic fever History of congenital heart disease History of cardiac murmurs or valvular disease Cardiovascular risk factors, including family history Presyncope and syncope Claudication OBJECTIVE 2. Performs a physical examination Demonstrates knowledge necessary for performing an orderly, systematic and adequate physicaL examination of patients with cardiovascular problems and recognizes the importance of A. ARTERIAL SYSTEM & JUGULAR VENOUS PULSE 1. Reports and demonstrates the correct method of measuring arterial blood pressure 2. Is familiar with difficulties in measuring arterial blood pressure accurately: a. Variation between extremities, position, and level of extremity b. The auscultatory gap c. Proper cuff size 3. Is familiar with normal and common abnormal findings found by inspection or palpation of the venous and arterial pulses, inc1uding the foilowing: a. a,c,v, waves; visual estimation of central venous pressure; hepatojugular reflux b. effect of inspiration on neck veins c. pulsus alternans, pulsus bisferiens, pulsus paradoxus d. act-tic regurgitation and stenosis B. EXAMINATION OF THE HEART 1. Discusses normal and common abnormal findings found by inspection and palpation of anterior chest. including the following: a. Right and left ventricular heaves: palpable A-waves b. Thrills 2. Understands the events of the cardiac cycle and the genesis of: 13 a. b. c. d. e. f. g. h. Si, S2, S3, S4, summation of gallop, splitting of 52 (normal & reversed), and opening snap mitral valve clicks semilunar valve ejection sounds Artificial valve sounds (normal & abnormal) Innocent murmurs, including flow murmurs, venous hums, mammary souffles Murmurs of vaivular stenosis and regurgitation Maneuvers that alter murmurs, i.e. Valsalva, squatting, inspiration, expiration Pericardial rubs OBJECTIVE 3. Orders or performs diagnostic studies and interprets laboratory data in a reasonable and cost-effective manner A. ELECTROCARDIOGRAPHY (EKG) 1. General knowledge of the range of normal variation in P, QRS, ST, T wave 2. Understanding of EKG diagnosis of LVH, left atrial enlargement, acute ischemia and patterns of mvocardial infarction 3. Basic understanding of the diagnostic utility of the EKG in the diagnosis of arrnytbmias B. CHEST X-RAY 1. General knowledge of normal chest x-ray findings 2. Apvreciation of abnormalities- seen in: a. heart failure b. valvular disease c. hypertensive disease d. ischemic heart disease e. common congenital abnormalities seen in adulthood C. NON-INVASIVE TESTING 1.Basic appreciation of the indications for: a. echocardiographic assessment (transthoracic and transesoDhageal) including 2D and Doppler echocard.iography b. ambulatory EKG (Holter) monitor c. exercise testing with and without perfusion scintigraphv. Including an understanding of the meaning of sensitivity and specificity with regards to the latter test in the diagnosis of coronary disease d. tomograpbic imaging techniques, including MRI and CT D. INVASIVE TESTING 1. Basic knowledge of the methodology involved in performing coronary angiographv, left ventricular hemodynamic assessment and electrophysioiogic testing; understands the indications and risks of invasive diagnostic procedures OBJECTIVE 4. Understands the pathophysiology, natural history, clinical presentation, diagnostic workup and management of: A. HEART FAILURE 13 14 1. 2. 3. 4. Altered myocardial hemodvnamics as well as abnormal neuroendocrine responses Precipitating causes of worsened heart failure Mechanisms and importance of diastolic dysfunction Therapy including relative value and limits of diuretics. digoxin. vasodilators, beta blockers, inotropes, fluid restriction, and other pharmacologic and nonpharmacologic therapies B. CORONARY ARTERY DISEASE 1. Risk factors for coronary artery disease and their modification 2. Differential diagnosis of chest pain 3. Chronic and acute ischemic syndromes (unstable angina and acute MI) with emphasis on proper history taking 4. Noninvasive and invasive testing in patients with suspected coronary artery disease 5. Complications in acute post-myocardial infarction syndromes such as arrhythmias, sudden death, mechanical lesions, pericarditis and cardiac rupture 6. Indications for coronary angiography 7. Role of interventional procedures (e.g. PTCA) and cardiac surgery in treatment of coronary artery disease C. ARRHYTHMIAS I. Bradyarrhythmias including various forms of conduction disturbances and AV block, with emphasis on the indications for pacing 2. Tachyarrhythmias, including an emphasis on the EKG diagnosis of wide complex tachycardias a. atrial 1. atrial tachycardia/AV nodal reentrant tachycardia 2. atrial fibrillation 3. atrial flutter b. ventricular 1. premature ventricular contractions (PVCs) 2. ventricular tachycardia 3. torsades de pointes 4. ventricular fibrillation c. pre-excitation syndromes (e.g. Wolff-Parkinson-White) 3. Understands the importance of the use of catheter ablation techniques in treatment of supraventricular arrhythmias, including atrial fibrillation D. CARDIOMYOPATHY E. 1. Differential diagnosis and laboratory assessment 2. Treatment including indications for cardiac transplantation and mechanical cardiac support 3. Follow-up of the post-transplant patient VALVULAR HEART DISEASE 1. 2. 3. 4. Acute rheumatic fever, including diagnostic criteria Aortic stenosis/regurgitation Mitral stenosis/regurgitation Tricuspid stenosis/regurgitation 14 15 5. Pulmonary stenosis/regurgitation 6. Mitral valve prolapse F. PERICARDITIS 1. Acute: etiologv, symptoms and diagnosis 2. Chronic: including large pericardial effusion, cardiac tamponade and the indications for pericardiocentesis 3. Diagnosis and management of constrictive pericarditis G. CARDIAC TUMORS 1. Cardiac involvement in metastatic cancer 2. Myxoma H. CONGENITAL HEART DISEASE 1. Diagnosis, history and physical of the adult with congenital heart disease especially for the diagnosis of a. b. c. d. e. atrial septal defect ventricular septal defect aortic stenosis pulmonic stenosis coarctation of the aorta 2. Basic understanding of the adult with partially corrected congenital heart disease and post-op complications of the more common repair procedures such as: a. transposition of the great vessels b. tetralogy of Fallot a. Ebstein’s anomaly PULMONARY HEART DISEASE 1. 2. 3. J. Cor pulmonale Pulmonary embolism Primary pulmonary hypertension CARDIAC INVOLVEMENT IN SYSTEMIC ILLNESSES 1. 2. 3. 4. 5. 6. Diabetes mellitus Thyroid disease Obesity Thiamine deficiency Pheochromocytoma Rheumatic disorders including scleroderma, SLE, temporal arteritis. polyarteritis nodosa and rheumatoid arthritis 7. Pulmonary embolism and deep venous thrombosis 8. Arterial embolism K. PERIPHERAL VASCULAR DISEASE 15 16 1. Arteriosclerosis obliterans (ASO) 2. Aneurysms a. abdominal aortic b. thoracic aortic (including aortic dissection) c. peripheral vascular L. MISCELLANEOUS CARDIAC CONDITIONS 1. Trauma to the heart and great vessels 2. Infectious diseases a. viral myocarditis b. infectious endocarditis 3. Assess preoperative risk for non-cardiac surgery OBJECTIVE 5. Develops treatment plan for common cardiac problems A. For each major disease of the cardiovascular system identifies the appropriate therapeutic approach B. Understands the indications for and can perform the following: 1. 2. 3. 4. 5. Cardiopulmonary resuscitation and advanced life support Emergency cardioversion Carotid massage Central venous pressure catheter insertion Recognizes the possible need, and requests medical consultation, for the performance of the following therapeutic procedures: a. b. c. d. transvenous pacemaker pericardiocentesis Swan-Ganz catheter insertion elective cardioversion C. For each of the treatments and drug types listed below identifies indications, dose, mechanism of action, main effects, side effects, adverse reactions, interactions, cost, efficacy, and appropriate follow-up: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Digitalis and other inotropic agents Antiarrhythmic drugs Diuretics Calcium channel entry blockers Beta blockers Angiotensin-converting enzyme inhibitors Vasodilators Anticoagulants & thrombolytic therapy Antihypertensive agents Lipid-lowering agents Rheumatic fever prophylaxis Endocarditis prophylaxis 16 17 13. 14. 15. 16. Nitrates Angiotensin receptor blockers Aldosterone antagonists Inotropes D. Informed, aware, and able to participate in and teach to patients, students, medical personnel and colleagues regarding: 1. 2. 3. 4. 5. 6. 7. Preventive cardiology and patient education Psychological aspects of cardiac disease Behavioral therapy including stress management, risk factor reduction, etc. Proper nutrition, especially regarding lipid management and obesity Medical “cost/benefit” including different national systems and medical care rationing Preventive cardiology The clinical trial and meta-analysis 17 INTENSIVE CARE UNIT INPATIENT CURRICULUM Resuscitation BCLS and ACLS Shock: Causes, assessment and treatment Early Goal Directed Therapy for Septic Shock Pulmonary Respiratory failure: Hypoxemic and Hypercapnic Intubation criteria, oral/nasal/tracheostomy, complications Mechanical ventilator modes, monitors and complications Weaning criteria and techniques, daily spontaneous breathing trials ARDS: Causes, Physiology, Therapy and Complications Asthma and COPD Pulmonary embolism Pulmonary hemorrhage Cardiology Shock: Differential diagnosis and initial treatment Acute MI: Diagnosis, treatment, and complications Arrhythmias Pericarditis, Tamponade and Constrictive Pericarditis CHF and Pulmonary edema Pulmonary artery catheters: Indications, placement, and interpretation Inotropic drugs Nephrology Acute Renal failure: Causes and treatment Renal Replacement Therapy: Continuous and intermittent Electrolyte abnormalities: Na+, K+, C1Acid-Base disturbances and compensations Metabolic acidosis: Increased and normal anion gap Urine electrolytes Metabolism Nutrition: Assessment, requirements, eternal feeding, TPN Diabetic ketoacidosis and non-ketotic hyperosmolar coma Adrenal crisis and steroid therapy Gastrointestinal Upper GI hemorrhage Lower GI hemorrhage Liver disease: Alcoholic, viral, other Pancreatitis The acute abdomen: Causes and Assessment Poisons Initial assessment and treatment options Acetaminophen Anti-depressants Salicylates Alcohols Infections Pneumonias: Community-acquired, hospital-acquired including VAP Aspiration pneumonitis Central Line Related Bloodstream Infections: Prevention and management 19 Tuberculosis Immunocompromised patients and opportunistic infections Hematology Anemia and transfusions Thrombocytopenia, coagulopathy and DIC Hemolysis Sickle Cell Disease Administration/Ethics Admission and discharge criteria Illness severity scores and prognoses Advance Directives Use/limitation of life sustaining treatments Practice and Systems Based Improvements: protocols and data monitoring 19 GENERAL MEDICINE INPATIENT CURRICULUM Likelihood Ratios; testing Community Acquired Pneumonia Physical Examination Pulmonary Emboli Chest Pain Evaluation; CAD Diabetic Ketoacidosis, complications Meningitis Venous Stasis Ulcers Peripheral Vascular Disease W/U of Diarrhea COPD, acute exacerbation Depression, mood disorders Stroke, endarterectomy Hypertension Emergencies Common Biliary Tract Diseases, Cholecystitis, Cholangitis Dementia Delirium Diverticulitis Avitaminoses Peripheral Neuropathy Cellulitis Pulmonary Nodule Anemia, chronic disease, liver disease, etc. Pancreatitis Poisonings, ethylene glycol, arsenic, etc. 21 Geriatrics Inpatient Curriculum Geriatrics Curriculum for Internal Medicine Residents Current requirements from the Residency Review Committee for Internal Medicine, as outlined by the Accreditation Council for Graduate Medical Education, specify that “Residents must have formal instruction and assigned clinical experience in geriatric medicine. The curriculum and clinical experience should be directed by an ABMS –certified geriatrician. These experiences may occur at one or more specifically designated geriatric inpatient units, geriatric consultation services, long-term care facilities, geriatric ambulatory clinics, and/or in home care settings.” The Department of Medicine at the University of Chapel Hill currently has a separate Division of Geriatric Medicine with faculty and fellows in graduate medical training who are dedicated to the education of medical students and residents. Currently residents receive training in the care of geriatric patients in both the inpatient and outpatient settings. Inpatient Geriatric Curriculum: UNC currently has a Geriatric Inpatient Service that is always staffed by one of the faculty from the Division of Geriatric Medicine. Internal Medicine residents who rotate on this service work closely with the Geriatrics Faculty Attending in the care of older adults with acute medical illnesses. Based upon the guidelines as outlined by the AGS Education Committee in 2004, resident trainees on this rotation will meet the following goals in attitudes, knowledge and skills required for the appropriate care of older patients. 1. Attitudes: This training program encourages respect for older people and their autonomy. The rotation on the inpatient service promotes compassionate, high quality care. Residents gain an appreciation for the heterogeneity in older people in respect to functional status, health, values and personal preferences. The resident learns the skills needed to negotiate the goals of care with the patient and family. Our inpatient service offers a truly multidisciplinary experience and the resident learns the importance of this approach to caring for older patients. The resident on our service works closely with a Geriatric Nurse Practitioner, Recreational Therapist, Physical Therapy service, social worker and specialized nurses interested in the care of older adults. The resident on this service truly gains an appreciation for the fact that the maintenance of function and quality of life may be more the goal than cure. 2. Knowledge: Internal Medicine residents who complete a rotation on the inpatient service will know: a. b. c. d. e. f. Age related changes Pharmacokinetics and the importance of polypharmacy Appropriate history and physical exam Decision making capacity, competence, autonomy, ethical considerations Role of exercise and rehabilitation Comprehensive geriatric assessment 21 22 g. Recognition of malnutrition h. Preoperative evaluation and postoperative care in older patients i. End of life care, palliative treatments including management of pain, dyspnea, and other symptoms j. Evaluation and management of : i. ii. iii. iv. v. vi. vii. viii. ix. x. Cognitive impairment/dementia Depression Incontinence Gait and balance disorders, falls Immobility Pressure ulcers Polypharmacy Sensory impairment Pain Delirium k. Difference in incidence, natural history, presentation, management, and outcomes of medical problems when they occur in elderly patients 3. Skills: The resident will be able to: a. Perform assessments of basic and Instrumental Activities of Daily Living (ADL and IADL), cognitive function, and gait and mobility b. Work within an interdisciplinary team to develop a plan of care c. Facilitate medical decision making with older patients, incorporating medical assessment and patient values and preferences d. Diagnose and manage acute and chronic multiple illnesses in older patients e. Conduct discussions regarding goals of care and end of life care 22 23 NEPHROLOGY INPATIENT CURRICULUM I. Teaching materials 1. Reading materials: Selected articles and publications from journals and nephrology database. (Up to Date) II. Topics to be discussed during Rounds: 1. Hemodialysis and peritoneal dialysis: techniques 2. Hemodialysis and peritoneal dialysis: dialysis prescription 3. Evaluation of kidney structure and function a. Urinalysis b. Measurement of GFR c. Evaluation of proteinuria d. Measurement of urinary electrolytes e. Renal imaging techniques 4. Chronic kidney disease 5. Acute kidney injury 6. Metabolic acidosis 7. Metabolic alkalosis 8. Disorders of water metabolism (hyponatremia and hypernatremia) 9. Disorders of potassium and magnesium metabolism 10. Disorders of calcium, phosphorus and bone metabolism 11. Overview of evaluation and treatment of hypertension 12. Glomerular syndromes a. nephritic syndrome b. nephrotic syndrome 13. Diabetic nephropathy 14. Principles of kidney transplantation 23 24 HEMATOLOGY/ONCOLOGY INPATIENT CURRICULUM Hematology/Oncology Inpatient Curriculum Updated 6/2008 Goals: This rotation should acquaint you with the general principles of diagnosing and treating Hematologic and Oncologic diseases. The inpatient services are divided into one that focuses on patients with malignant hematologic diseases such as the leukemias(E1)and lymphomas and the other (E2) on the rest of oncology. While there is some overlap in the services, we suggest that you focus you reading on the service you were assigned to. Every effort will be made for you to do the other service at least once during your residency. A case based teaching program to supplement your reading that combines patients from both services is done from 11:30 to 12:15 on Mondays, Tuesdays, Wednesdays and Fridays. 1. Acute Leukemia a. ALL b. AML i. Genetics of AML c. Clinical Presentation of Acute Leukemia i. Laboratory Diagnosis ii. Bone Marrow Examination D. General Therapy for Acute Leukemia’s i. Therapy for ALL ii. Therapy for AML Tallman MS, Nabhan G: Acute promyelocytic leukemia.Blood 2002;99:759-67. 2. 3. Sickle Cell Disorders Febrile Neutropenia and infected catheters Mermel LA et al: Guidelines for the management of intravascular catheter related infections. Clin Infect Dis 32:1249, 2001 4. Thrombotic Disorders a. Major Risk Factors b. Laboratory testing in thrombotic disorders c. Management of a thombotic defect d. Treatment and prevention of Thrombosis 5. Breast Cancer a. Risk Factors for breast cancer and risk reduction strategies b. W/U of a suspicious breast mass c. Primary therapy for a newly diagnosed breast cancer d. Systemic therapy for breast cancer e. Quality of life in breast cancer survivors Fisher B et al: Twenty-year follow-up of a randomized trail comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation of the treatment of invasive breast cancer. N Engl J Med 347:1233, 2002 Wong ZW, Ellis MJ: First –line endocrine treatment of breast cancer: Aromatase inhibitor or antiestrogen? Br J Cancer 90:20, 2004 Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trails. Lancet 2005; 365, 1687 Ravdin PM et al: Computer program to assist in making decisions about adjuvant therapy for women with early breast cancer. J Clin Oncol 2001; 19:980m . 6. Colorectal Cancer a. Risk factors for colorectal cancer b. Clinical features of colorectal cancer c. Staging of colorectal tumors d. Management of resectable colorectal tumors e. Post resection surveillance in colorectal cancer f. Management of patients with metastatic colorectal cancer 24 25 Baron J et al: A randomized trial of aspirin to prevent colorectal adenomas. N Engl J Med 348:391, 2003 Walsh JME, Terdiman JP: Colorectal cancer screening; JAMA 289:1288, 2003 7. Lung Cancer a. Clinical presentation of lung cancer b. Diagnosis and treatment of lung cancer c. Non-Small Cell Lung cancer d. Small Cell Lung cancer American College of Chest Physicians: Diagnosis and management of lung cancer: ACCP evidence based guidelines. Chest, 123:1S, 2003 8. Cancer a. b. c. of Unknown Primary Site Adenocarcinoma of Unknown primary site Squamous cell carcinoma of unknown primary site Poorly differentiated carcinoma of unknown primary site Hainsworth JD, Greco FA: Management of patients with cancer of an unknown primary site. Oncology 14:563, 2000 9. Lymphadenopathy, lymphoma and Multiple Myeloma Diehl V et al: Hodgkin’s lymphoma---Diagnosis and treatment. Lancet Oncol 5:19, 2004 Barlogie B et al: Treatment of multiple myeloma. Blood 103:20, 2004 10. Prostate Cancer a. The screening controversy b. Treatment of prostate cancer c. The Gleason Score d. Comparison of Treatment modalities e. Sequelae of treatment in prostate cancer f. Management of recurrent prostate cancer Nelson WG et al: Prostate cancer. N Engl J Med 349:366, 2003 11. Testicular Cancer Bosl GJ et al: Testicular germ-cell cancer. N Engl J Med 337:242, 1997 12. Oncologic Emergencies a. Metabolic Emergences (Hypercalcemia, Hyperuricemia, and Hyponatremia) b. Hematologic Emergency: DVT c. Mechanical Emergencies (Spinal Cord Compression, SVC, Pericardial Effusión and Tamponade) Strewler GJ: The parathryid hormone-related protein. Endocrinol Metab Clin. North Amer 29:629,2000 Yim BT et al: Rasburicase for the treament and prevention of hyperuricemia. Ann Pharmacotherapy 37:1047, 2003 13. Chemotherapy, biotherapy and hematopoietic colony stimulate factors: American Society of Clinical Oncology : Update of recommendations for use of hematopoietic colony stimlating factors: Evidence-based clinical practice guidelines. J Clin Oncol 2000: 20;3558-85 14. Antiemetics Wiser, W.Practical management of chemotherapy-induced nausea and vomiting Oncology 2005;5: 637-45 15. Pain Management Levy MH: Pharmacologic treatment of cancer pain. N Engl J Med 335:1124, 1996 25 26 Pulmonary Inpatient Curriculum Pulmonary Physiology Gas Exchange Mechanics Measures of Function Arterial blood gases Lung volumes and DLCO Imaging techniques Obstructive Pulmonary (Airway) Diseases Chronic Bronchitis Emphysema centrilobular panacinar Cystic Fibrosis Bronchiolitis Bronchiolitis obliterans BOOP Bronchiolitis obliterans associated with lung transplantation Bronchiectasis Asthma Epidemiology and definition Classification "Intrinsic or nonallergic" "Extrinsic or allergic" Pathogenesis Clinical manifestations and diagnosis Therapy Respiratory Infections Community acquired pneumonias Infections in the immunocompromised host AIDS Other causes of immunosuppression Tuberculosis and nontuberculous mycobacteria Anaerobic lung infections and aspiration Empyema Intersitial Lung Disease Idiopathic pulmonary fibrosis Drug induced Connective tissue diseases Sarcoidosis 26 27 Eosinophilic granuloma Lung Neoplasms Carcinomas Mesotheliomas Benign tumors Staging evaluation Resectability Lung Transplantation Indications Common diseases transplanted Single versus double lung transplants Survival Complications Pulmonary Vascular Disease Pulmonary thromboemboli Pulmonary hypertension Pulmonary vasculitis Alveolar hemorrhage/hemoptysis Miscellaneous Pleural diseases Effusions Pneumothorax Occupational Lung diseases Sleep disorders Lymphangioleiomyomatosis 27 28 MEDICAL HOUSESTAFF ACTIVITIES ON THE PULMONARY INSERVICE ROTATION 1. Each houseofficer will be expected to prepare a minimum of three 20-30 minute, informal lectures to be given to the rest of the team throughout the month. 2. Houseofficers are expected to attend Chest X-ray Rounds Monday, Wednesday and Fridays at 2:30 PM. 3. The medical houseofficers are encouraged to attend the pulmonary lectures and conferences (Conference schedule enclosed). MED G SYLLABUS JOURNAL ARTICLES ASPIRATION PNEUMONIA Aspiration Pneumonia. Lung Abscess, and Emphysema ASTHMA Review Article-Asthma The Assessment and Management of Adults with Status Asthmaticus COMMUNITY ACQUIRED PNEUMONIA American Thoracic Society Clinical Guidelines for the Initial Management of Adults with Community-Acquired Pneumonia Current Concepts-Community Acquired Pneumonia ATS-Guidelines for the Initial Management of Adults with Community -acquired Pneumonia: Diagnosis, Assessment of Severity, and Initial Antimicrobrial Therapy COPD Management of Chronic Obstructive Pulmonary Disease-James F. Donohue, MI) Current Concepts-Management of Chronic Obstructive Pulmonary Disease CYSTIC FIBROSIS Review Article-Drug Therapy Management of Pulmonary Disease in Patients with Cystic Fibrosis HEMOPTYSIS Massive Hemoptysis: Assessment and Management HOSPITAL-ACQUIRED PNEUMONIA Hospital-acquired Pneumonia in Adults: Diagnosis, Assessment of Severity, Initial Antimicrobial Therapy, and Preventative Strategies LUNG MALIGNANCIES Pulmonary Manifestations of Extrathoracic Management Lesions Staging Systems of Lung Cancer MYCOBACTERJAL DISEASES Clarithromycin Regimens for Pulmonary Mycobacterium avium Complex Control of Tuberculosis in the United States Treatment of Tuberculosis and Tuberculosis Infection in Adults and Children PNEUMOCYSTIS CARINII PNEUMONIA Mayo Clinic Proceedings-Pneumocystis carinii Pneumonia in Patients without Acquired Immunodeficiency Syndrome: Associated Illnesses and Prior Corticosteroid Therapy 28 29 Pneumocystis Carinii Pneumonia in Patients with the Acquired Immunodeficiency Syndrome PULMONARY VASCULAR DISEASES Invasive and Noninvasive Diagnosis of Pulmonary Embolism-Preliminary Results of the Prospective Investigative Study of Acute Pulmonary Embolism Diagnosis (PISA-ped) Clinical Features of Pulmonary Embolism-Doubts and Certainties Value of the Ventilation/Perfusion Scan in Acute Pulmonary Embolism-Results of the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED) Anticoagulation in the Prevention and Treatment of Pulmonary Embolism Venous Thromboembolism SARCOID Conferences and Reviews-Enigmas in Sarcoidosis SLEEP APNEA Current Concepts-Obstructive Sleep Apnea Treatment of Obstructive Sleep Apnea-A Review MISCELLANEOUS Mayo-Rare Pulmonary Neoplasms Mechanisms of Disease -Hvpercania Review Article-Mechanisms of Disease-Pathophysiology of Dyspnea Dyspnea: Mechanisms, Assessment, and Management: A Consenus Statement Review Article-Primary Pulmonary Hypertension 29 30 INFECTIOUS DISEASE INPATIENT CURRICULUM Antibiotics I (antibacterials) Antibiotics II (antivirals and antifungals) Pneumonia HIV I HIV II Sepsis Endocarditis Skin and Soft Tissue Infection (including osteomyelitis) Diarrhea Urinary Tract Infection FUO New and unusual infections, including Lyme Disease and RMSF 30 31 NEUROLOGY INPATIENT CURRICULUM CURRICULAR COMPONENT: NEUROLOGY WARD ROTATION I. OVERALL EDUCATION GOAL: The goal of the ward rotation for residents is to learn the evaluation and management of common neurological problems seen in the inpatient neurology setting. The resident will be part of the Neurology ward team consisting of the neurology attending, neurology senior resident, medicine and psychiatry interns, and medical students who are involved in the care of inpatients on the Neurology ward service. II. OBJECTIVES: 1. The resident will become competent in obtaining a neurological history and performing a neurological exam on patients presenting to the Neurology inpatient service. 2. The resident will learn to effectively present neurological cases. 3. The resident will gain skill in the localization of various neurological symptoms and findings seen on the Neurology inpatient service. 4. The resident will learn to generate a differential diagnosis for common neurological symptomatology and findings seen on the inpatient service. 5. The resident will become an integral part of the Neurology team with the ability to both synthesize cases for presentation to the neurology senior resident and attending. 6. The resident will gain competence and skill in the assessment of common neurological problems seen on the Neurology inpatient service including TIA, stroke, delirium, intractable epilepsy, Parkinson’s disease, myasthenia gravis, acute and chronic inflammatory demyelinating polyneuropathy, polymyositis, acute low back pain, intractable headache, multiple sclerosis, and myelopathic disorders. 7. The resident will learn the appropriate and cost effective evaluation of patients presenting with various problems to the Neurology inpatient service. 8. The resident will gain ability in the use of laboratory tests, lumbar puncture, EMG/nerve conduction studies, EEG, evoked potentials, CT, MRI, and other studies in the evaluation and management of neurology inpatients. 31 32 III. EVALUATION: The residents will be evaluated directly by the faculty member assigned to the Neurology ward service. The faculty members will directly observe the residents’ presentation of cases, and their assessment and plan for the management of patients with neurological disorders. The attending will provide feedback to the resident during the rotation regarding their skills in the assessment and management of neurological patients. In addition, the faculty member will assess the resident’s ability to be an integral member of the Neurology ward team, including their ability to interact with other members of the ward team and ancillary personnel. At the end of the rotation, the faculty member will complete a standard evaluation form, which will be keyed to the learning objectives of the rotation. IV. LEARNING ACTIVITIES OF THE ROTATION: Residents on the Neurology rotation will round with the neurology ward team each weekday and on one weekend day. They will have an opportunity to present cases and be critiqued on both their evaluation and management ability. Residents will have the opportunity to observe the attendings history taking and neurological examination on neurology inpatients. The residents will also be present when the attending discusses their assessment of neurology inpatient cases with the neurology inpatient ward team, as well as didactic presentations by the attending on various neurological issues. The resident will have the opportunity to review neuroimaging studies with the Neuroradiology staff and the neurology inpatient attending. The neurology resident will also have the opportunity to review clinical neurophysiology studies done with the clinical neurophysiology attending staff. Throughout the rotation, the resident may attend the daily noon resident lectures which will cover various neurological topics, including the evaluation and management of a variety of disorders seen on the neurology inpatient service. This will include the Clinical Lecture Series, and other conferences. Topics to be Covered Intracranial Mass Lesions Review of the Neurologic Exam Spinal Cord Injury Neuroradiology - What Study to Order Coma Management of Acute Spinal Disorders Head Injury Neuromuscular Disorders Head CT and MRI Interpretation Management of Back Pain Pediatric Neurosurgery Pain Management Seizures Pediatric Rehabilitation 32 33 Physical and Occupational Therapy Headache Neuro-opthalmologic Evaluation Stroke Introduction to Rehabilitation Management of Acute Spinal Disorders 33 34 SECTION 3 AMBULATORY CURRICULUM Emergency Room Same-day Clinic Cardiology Endocrinology General Medicine Hematology/Oncology Pulmonary Disease Digestive Disease Infectious Disease Rheumatology Nephrology Adolescent Medicine Geriatric Medicine PGY -1 Continuity Elective PGY – 2/3 Continuity Elective Enhanced Care Elective 34 35 Section 3 Ambulatory Curriculum General Each rotation has designated teaching times. The responsibility for teaching is given to the respective department or a division in the Department of Medicine. The topics are generated by the faculty with input from the Department of Medicine. These curricula are designed for consultation as well as direct patient care. 35 36 EMERGENCY MEDICINE CURRICULUM UNC Department of Emergency Medicine The Emergency Department (ED) attendings work 8 hour shifts, 7a-3:00p, 1p-9p, 10a-6p, 3p11p, 6p-2a, and 11p-7a. Two attendings are on duty, with the exception of the time period from 2a to 10a when one attending is on duty. The ED has 3 main areas. The Acute Care area has 24 beds including 2 cardiac rooms and 3 trauma rooms. Team C is an adjacent area with 8 beds. Team C is open 9a to midnight daily. Pediatric Acute Care is a separate unit staffed by Pediatric attendings and residents. Pediatric Acute Care is open 9a-2a daily. After those hours, pediatric patients (ages 15 and below) are treated in the main ED. During your rotation, you will be assigned shifts in both the Acute Care area of the ED and the Minor Trauma area. Guidelines for Houseofficers Department of Emergency Medicine The University of North Carolina at Chapel Hill Introduction and General Principles Welcome to the Department of Emergency Medicine! During this rotation, you will learn skills that are essential to your medical education. You will be supervised by faculty members who are Board Certified or Board Eligible in Emergency Medicine. Our faculty have practiced in a variety of institutions and settings, and thus, your experience here will be enhanced by exposure to different styles of practice. Emergency Medicine differs in many respects from the inpatient and clinic settings. During this rotation, you will see a broad spectrum of illness ranging from the most trivial complaints to lifethreatening disease. It is important to remember that all patients come to the ED for a reason. Many present to the ED early in the course of their illness, therefore a serious disease may initially present to you as an apparently benign complaint. Many may present with complaints that could best be handled elsewhere. It is our role to ensure our patients receive our best efforts to guide them through the increasingly complex healthcare system as well as to diagnose and treat acute care conditions. Remember the Emergency Department is an important portal of entry into the hospital and provides a strong impression of the institution to patients, their families, and referring physicians from other medical centers. House officer Requirements for Successful Completion of Emergency Medicine Rotation 1. Completion of the Online Orientation Module Each houseofficer must complete the online orientation course and exam before starting their Emergency Medicine rotation. The orientation module is available online at www.med.unc.edu/wrkunits/2depts/emergmed. 2. Assigned Shifts in the Emergency Department Be prompt for your assigned shifts. If you are ill or must miss an assigned shift, you need to contact: Your chief resident. Chief residents from each rotating department will be responsible for providing replacement coverage for their individual department residents who are unable to fill an assigned shift. 36 37 The ED attending physician working at the time your shift begins (9664721). In order to successfully complete the ED rotation as required by your residency, you must complete all assigned shifts. Illnesses are only excused if verified by your personal physician (not a resident physician) or your residency director. 3. Resident Conferences In order for the Departments of Emergency Medicine, Medicine, Surgery, Family Medicine and OB/Gyn to meet the requirements of the Residency Review Committee, weekly attendance at our Emergency Medicine Conferences is MANDATORY. These conferences are held on Wednesday mornings from 7a to noon. The schedule of topics is available monthly. Emergency Medicine interns/residents are required to attend conferences 5 hours per week. Off-service interns/residents are required attend 3 hours per week. During your rotation, you will likely be scheduled in the ED on one or more Wednesday mornings. On these mornings you should attend sign out rounds and check in with the ED attending prior to departing for conference. When you are not scheduled to work in the ED, you should attend at least part of the Wednesday morning conference. Attendance will be taken at these conferences and reported to individual residency directors at the end of each rotation along with your final evaluation. If you have questions or concerns, please feel free to contact: Kevin Biese, MD Assistant Professor Education Director 966-6440 Guidelines for Housestaff: Department of Emergency Medicine The University of North Carolina at Chapel Hill Important Items to Keep in Mind: 1. Although you will be quite busy at times, make sure you speak to any family or visitors who may be in the waiting room after you have finished your evaluation. It is important to let them know how well the patient is doing and give them an estimate of the anticipated length of stay. Always overestimate the length of stay. Things take longer than you think. 2. Laboratory studies and X-rays are ordered only if they impact on acute treatment, immediate decision making, or are essential for the provision of follow-up care. The Emergency Department is not the place to begin an extensive workup of non-critical problems. 3. Every patient should be given instructions for follow-up care and referred to a follow-up physician, no matter how trivial the problem may seem. (see documentation and charting guidelines) 4. You should be able to arrive at a reasonable clinical diagnosis on most patients. If you lack a definitive diagnosis, you must have formulated a clear differential diagnosis and have ruled-out all possible life-threatening conditions before the patient can be discharged safely. 5. Information concerning patients seen or discussed in the ED is confidential. It should not be discussed anywhere else, other than in a medical conference setting. This means you must not discuss patient information in the hallways, nor the elevators, nor in downtown restaurants, etc. You are a professional and must conduct yourself as such. 6. All patients who are seen in the Emergency Department are the ultimate responsibility of the attending emergency physician. Consequently, THE EMERGENCY DEPARTMENT 37 38 ATTENDING MUST SEE EVERY PATIENT AND SIGN EVERY CHART PRIOR TO THE PATIENT’S DISCHARGE, ADMISSION OR TRANSFER. 7. Some patients have such serious illness at the time of presentation that they may decompensate in a very short period of time. Because of this, there are certain circumstances when it is vital for you to notify the attending physician of the patient’s condition IMMEDIATELY AND POSSIBLY BEFORE YOU HAVE FINISHED YOUR INITIAL EVALUATION. (You will find a list of these circumstances attached in this handout.) If you think a particular patient is unstable, alert the attending on duty. 8. T System: All ED patients are tracked on a computer system called T System. When you arrive in the ED, you will be instructed how to use this system to sign up as the provider for the patients you are evaluating. In order to access this system, you must have a valid UNC Hospital code and password. 9. As patients enter the Emergency Department, they are triaged by the nursing staff. triage designations are: Stability of vital functions Life-threat or organ-threat Severe pain or severe distress Expected resource intensity The ESI-1 Unstable ESI-2 Stable ESI-3 Stable ESI-4 Stable ESI-5 Stable Obvious Reasonably likely Sometimes Unlikely (possible) Seldom No No No No Medium: multiple diagnostic studies; or brief observation; or complex procedure Low: one simple diagnostic study; or simple procedure Low: exam only Up to 1 hr Could be delayed 6 hr 2 hr Could be delayed 1 hr Immediately Maximum: staff at bedside continuously; mobilization of outside resources Med/staff response Immediate team effort High: multiple, often complex diagnostic studies; frequent consultation; continuous (remote) monitoring Minutes Expected time to disposition Examples 1.5 hr 4 hr Cardiac arrest, intubated/hypotensiv e trauma patient, acute (<3 hr) MI or stroke Most chest Most Closed Sore pain, stable abdominal extremity throat, trauma (MOI pain, trauma, minor concerning), dehydration, simple burn, elderly esophageal lac, recheck pneumonia food simple patient, impaction, cystitis, altered hip fracture typical mental migraine status, behavioral disturbance In general, patients should be seen in the order in which they arrive in the ED, however patients triaged as “1” or “2” should be evaluated before those designated “3-4- 38 39 5”. If you are unsure which patient you should evaluate next, ask the attending or a senior resident to direct you. SCHEDULE Housestaff will be assigned to one section of the department and will report ONLY to the attending staffing that section. RESPONSIBILITIES Role of the Emergency Department Attending The ED attending is primarily responsible for patient flow and consultation. The ED attending will be responsible for the supervision of all medical students and houseofficers. Housestaff cannot sign student orders. Role of the PGY-III Resident The PGY-III Emergency Medicine Resident has three main responsibilities in the ED: 1. Directly evaluate patients as the primary physician, with particular attention to critically ill or injured patients. 2. Ensure that patient flow in the ED is maintained. 3. Supervise one or more PGY-I residents who are working in the ED. 4. Perform or supervise procedures required for patient care. 5. At times, these residents may take a turn at being “in charge” of the ED under the supervision of the attending. . Role of the PGY-I and PGY-II Residents and Medical Students The PGY-I resident and medical student are primarily responsible for patient evaluation and management. Remember that you are here to learn and that specific questions are expected. It is better to ask and ask early! PATIENT CARE AND CASE PRESENTATION It will be the responsibility of the EM PGY-III resident, all PGY-I residents, and medical students to pick up new patients as they are added to the board by the triage nurse. Patients are to be seen according to their time of entry into the ED unless another patient with a potentially life-threatening complaint has not yet been evaluated. Patients with life-threatening complaints are designated by a triage classification of “1” (in red) and should be seen promptly. If you are not certain whether a particular patient is to be seen, ask the attending physician or triage nurse. The residents will see and evaluate the majority of patients. This initial evaluation is to consist of a history and physical examination, which may be “directed” if the patient has an obviously isolated problem (such as a minor extremity injury). All other patients should have a complete history and physical examination including social and family history, medications and allergies. This evaluation should take no longer than 5 to 10 minutes to complete. ANY PATIENT WITH A CONDITION WHICH MAY DETERIORATE PRECIPITOUSLY MUST BE CALLED TO THE ATTENTION OF THE ED ATTENDING IMMEDIATELY, EVEN IF THE INITIAL EVALUATION IS NOT COMPLETED. A list of such conditions is listed in this handout. After formulating a differential diagnosis and treatment plan, but before writing orders, the intern is to present the patient to the ED attending. At that time, an evaluation and treatment plan can be formulated and orders written. No verbal orders are acceptable. After all ancillary studies have been completed, the houseofficer is to present the case to the ED attending again, this time noting the results of laboratory values, X-rays, etc. At this time a disposition will be made and the patient will be either discharged, admitted or transferred to a different institution. 39 40 TYPES OF PATIENTS SEEN Adult patients with a wide variety of complaints are seen in the Acute Care area of the ED. In addition to evaluating and treating patients with general medical and surgical problems, you will gain experience with patients whose complaints include the following: Psychiatric - Our responsibility is medical clearance; be especially careful with elderly patients or those with confounding medical problems; some psychiatric patients will be seen directly by the Psychiatric consultants. OB-Gyn - Women at 20 weeks or greater gestation are transferred directly to Labor and Delivery. The exceptions to this are if they have any type of trauma or a complaint totally unrelated to pregnancy. All women between 10-60 should be assumed to be pregnant until proven otherwise by a negative urine or serum pregnancy test. Trauma - Major trauma patients, as determined by criteria, are seen by the Trauma team, EM Attending and Senior Emergency Medicine Residents. Patients with lesser trauma are evaluated and treated by the general ED staff. Pediatrics (ages 15 and below) - These patients are seen directly by a Pediatric resident, either in Pediatric Acute Care (9a-11p) or in the Acute Care ED at other times. ANCILLARY SERVICES Laboratory Studies 1. Laboratory studies are ordered in writing on the order sheet. 2. Laboratory reports results can be obtained on the computer. Be sure to check the computer frequently for results so the patient can receive disposition in a timely manner. 3. All laboratory studies must be documented on the chart, including those that are pending at the time of disposition. Radiologic Studies 1. If a patient needs an X-ray or other imaging study, write the order on the order sheet and give the order sheet to the clerk. You need to write a reason for the X-ray study, i.e. chest pain or SOB. The X-ray orders are entered into the computer by the nursing staff. 2. Look at the patient’s X-rays even though the radiologist’s interpretation is available. Remember that you have the advantage of knowing the patient’s clinical presentation and thus may notice something the radiologist might have misses. 3. If you have any questions regarding the interpretation of a particular radiograph, you may consult the radiology attending or resident by dialing 68850. 4. All radiologic studies must be documented on the chart! MEALS Housestaff are encouraged to briefly leave the ED for nutrition breaks as patient flow permits, but only after notifying the attending that they are leaving. DOCUMENTATION STANDARDS It is your responsibility to see that these standards are met on every chart. Charts will be returned to you for completion if documentation standards are not met. 40 41 DISCHARGE INSTRUCTIONS AND FOLLOW-UP All patients are to receive a discharge instruction sheet prior to leaving the Emergency Department. There are specific items that must be included on the discharge form. PATIENTS LEAVING THE EMERGENCY DEPARTMENT AGAINST MEDICAL ADVICE (AMA) All patients who threaten to leave the Emergency Department against medical advice (AMA) must be seen by the ED attending immediately. The patient is required to sign an AMA form on the back of the chart and must be properly informed of the risks of departing AMA. SECURITY AND PARKING Escorts to the parking decks are available 24 hours a day. USE THEM!! Use the Point to Point Service (962-7867) or have hospital security accompany you! You cannot park in the ED patient parking lot. DRESS CODE AND IDENTIFICATION Name badges must be worn at all times. Housestaff are expected to look and act like professionals at all times. Scrubsuits are acceptable for wear in the Emergency Department provided they are clean and in good condition. Jeans, shorts, sweats and T-shirts are not permitted. WHEN YOUR SHIFT ENDS You must turn your patients over to an intern or resident on duty in the ED. If your patient is nearing completion of their evaluation – please fill out the chart completely including the discharge form if appropriate. If the evaluation is in progress, please have a clear plan to pass on to the next doctor. Medical Conditions Requiring Immediate Attending Physician Notification The following is a list of conditions that require immediate notification of the Emergency Department attending physician, regardless of your level of training. This list does not cover all possible situations, and you should feel free to notify the attending immediately if you have a patient you feel may deteriorate precipitously or if you are uncomfortable given your present level of training. 1. Any patient who presents with or develops acute cardiopulmonary arrest. 2. Any patient with a complete or partially obstructed airway. 3. Any patient who presents with or develops a significant cardiac arrhythmia, whether stable or not. 4. Any patient with acute onset Alteration of Mental Status (AOMS). This includes any patient presenting with this as the chief complaint or any patient whose mental status deteriorates while in the ED. 5. Any patient with significant hypotension or hypertension. For these purposes, significant hypotension will be defined as blood pressure of less than 100 mmHg systolic and significant hypertension will be defined as a blood pressure of greater than or equal to 180 mmHg systolic or hypertension associated with acute alteration of mental status. 6. Any patient with severe respiratory distress. For these purposes, significant respiratory distress will be defined as a respiratory rate greater than 30 breaths/minute, any patient 41 42 with a pulse oximeter reading of less than or equal to 90 mmHg, any patient with an acute elevation of pCO2 greater than or equal to 60 mm Hg, any patient with a complaint of shortness of breath accompanied by diaphoresis, use of accessory muscles of respiration, cyanosis, alteration of mental status, bradycardia, or any other signs consistent with imminent respiratory failure. 7. Any patient with significant tachycardia or bradycardia. For these purposes, significant tachycardia is defined as a heart rate greater than or equal to 150 beats/minute and significant bradycardia is defined as a heart rate less than or equal to 60 beats/minute. 8. Any patient with a significant cardiac arrhythmia. 9. Any patient with either clinical or EKG evidence of acute myocardial infarction. 10. Any patient with a fever greater than 105 degrees Fahrenheit, any patient with significant alteration of mental status associated with a fever, or any patient with a fever and a potentially immunocompromised state (e.g. HIV disease, cancer patients, transplant patients, etc.) 11. 11. Any patient with significant hypothermia. For these purposes, significant hypothermia is defined as a rectal temperature less than or equal to 95 degrees Fahrenheit. 12. Any patient with severe abdominal pain or abdominal pain associated with peritoneal signs. 13. Any female with abdominal pain and a positive pregnancy test. 14. Any patient with significant upper or lower GI bleeding (whether hypotensive or not). 15. Any patient who develops seizure activity while in the Emergency Department. 16. Any patient with significant abnormality of any laboratory value (e.g. hypo/hypernatremia, hypo/hyperkalemia, symptomatic hypercalcemia, hematocrit less than 28, etc.). 17. Any patient with a history of significant trauma. 18. Any patient with a pregnancy and sign/symptoms of a precipitous delivery. 19. Any patient with an overdose of prescription or over-the-counter medications. 20. Any patient or visitor who gives evidence of becoming significantly agitated, violent, or suicidal. 21. Any patient with a blood sugar of less than 70 mg/dL. 22. Any patient with a snakebite. 23. Any patient with significant bleeding, or bleeding associated with hemophilia (blood dyscrasias). 24. Any patient with a significant allergic reaction. 25. ANY PATIENT WHO YOU FEEL IS BEYOND YOUR PRESENT CAPABILITIES AS A RESIDENT, OR WHO YOU THINK MAY DETERIORATE SUDDENLY. 42 43 Documentation Standards The following information is required on all charts for all Emergency Department patients for legal and billing purposes. Please review this in conjunction with the copy of the chart included in this packet. 1. The Emergency Department uses the T System for charting. Please complete the T System training module before starting your first shift. 2. For all patient charts, documentation should reach a “level 5” by the standards of the T System Documentation System. Please confirm this before signing your chart. 3. It is important to write a short summary of your assessment and plan in each chart.. Based on the differential problem list that you have established, it should be obvious by reviewing the chart how you distinguished among the possibilities and came to your final diagnosis. Some examples: GI cocktail given, patient with complete relief; Phenergan 25mg IV given, nausea relieved and patient tolerating PO well. If you make a clinical diagnosis without any work-up, you need to explain that. For example: 20 year old white female with reproducible chest wall pain, no risk factors for CAD and no associated symptoms, likelihood of cardiopulmonary disease as the underlying etiology is very low. We will treat her with NSAID’s. Patient knows to return if symptoms change or worsen. 4. You need to list the medications the patient is taking and any drug allergies the patient has. 5. If the patient is in the Emergency Room for a significant length of time waiting for disposition or a bed, you need to make note that you reevaluated the patient during this time. For example: 2:45 pm Patient now afebrile and tolerating oral fluids well. Many conditions such as respiratory distress, chest pain and abdominal pain require frequent reevaluation, and you need to document it. 6. If you call a consultant to see the patient, record the time and who you talked with. For example: 6 pm Discussed case with Dr. Smith(General Surgery) who will evaluate patient. “Curbside” consultations are not official. If there is really a question, the patient must be seen by the consultant. 7. Record a procedure note for all procedures done on the patient including laceration repairs, lumbar punctures, central lines, etc. 8. Please select a disposition and diagnosis (often more than 1diagnosis) for each patient. DISCHARGE INSTRUCTIONS The T system has standard discharge instructions for many different diagnoses as well as medications Every discharged patient should receive 1 or more of these instruction sets. All patients should receive Follow-Up. Follow-up options include but are not limited to: 1. Follow-up with their own doctor (MUST BE NAMED) for a specific period of time. If the patient is unable to identify an MD, a referral should be given. 2. UNC Clinic Appointment: Options for obtaining this are: 43 44 * You can call and get an appointment for the patient (Mon-Fri 8a-5p) * Fill out a clinic referral sheet available in the ED, these are faxed to a central office where appointments are made, * You can give the patient the phone number for a specific clinic (listed in the T system discharge instructions) BUT, keep in mind, it may be several months before a patient can get an appointment. Welcome! From the Nurses in the Emergency Department The following handout details survival skills for your emergency department rotation. We hope that it may be helpful to you. The ED is divided into several sections: Triage Acute Area Team C Pediatric Acute Care The nursing staff is assigned by “team.” One or two nurses are assigned to the triage area. These nurses are responsible for screening all patients and prioritizing their care. The Acute Area is divided into Team A and Team B. Two or more nurses are assigned to cover each of these teams. There are three trauma bays, including a pediatric resuscitation bay. There are two cardiac resuscitation rooms. The Acute Area is divided into the A and B teams which are each responsible for ½ the acute area of the department. Team C is a separate area that usually evaluates ESI score 4 and 5 patients (see above). A charge nurse is assigned to coordinate the care of the ED patients. At various times, the charge nurse will also have a patient care assignment. Two nurses are assigned to the trauma team. If there is a trauma in progress and the nurse assigned to a certain area becomes unavailable, refer all questions to the charge nurse. Remember, if you are busy, so is the nursing staff! This is a team-oriented department. Help us and each other! General Information It is mandatory that you wear your name tag! Familiarize yourself with the clean and dirty utility rooms on your first day. You will find this invaluable. Most of the equipment you need is located in these areas. Equipment is secured in the PYXIS. Tidy up after yourself after completing an exam or procedure. There are trash cans located at each patient care bedside. (This includes the lounge!) The ED staff is a lifeform in itself. The nursing assistants, clerks, nurses, and social worker can be great resources for the inside scoop on usual routines, community resources, etc. Clerks can help you with phone calls and paging. Clerks answer the phones, even if you have paged someone. Listen to the intercom for your name or the person you have paged. The key staff in the ED have assigned intercom cell phones. 44 45 Nursing Assistants can perform the following: simple wound preps crutch set-up lab transport patient transport (excluding monitored patients) room set-up assist with procedures Remove all needles and sharps from trays and dispose of them in the sharps box! If a laceration needs sutures, anesthetize the wound prior to wound prep. The department’s infection rate has been consistently 0% because the NA’s do an excellent job. RN’s 1. Unless the patient is acutely ill, please allow the RN to triage the patient prior to beginning your exam or gathering information. 2. ED nurses will assess the acuity of patients and institute treatment and diagnostic procedures prior to your seeing the patient. For example: monitoring, IV access. Orders still need to be written for the patient. Educational Conferences Emergency Medicine conferences are held Wednesday from 7:00 am to noon. All PGY1 residents assigned to the Emergency Department each month will be expected to attend. Scheduling in the Emergency Department PGY-1 Medicine Interns will work 12 hour shifts beginning at 7 am, 10 am, or 7pm. These times will rotate throughout the month. 45 46 Same-Day Clinic CURRICULUM Low Back Pain Monoarticular Arthritis Approach to Arthritis Musculoskeletal Syndromes of the Neck and Arm Depression Initial Diagnosis and Management of Hypertension Initial Diagnosis and Management of Type II Diabetes Bronchitis Rhinitis/Sinusitis Headache Pharyngitis/Mononucleosis PID Chest Pain STD’s 46 47 CARDIOLOGY AMBULATORY CURRICULUM Consultations including preoperative evaluations will be handled by internal medicine residents, cardiology fellows and faculty. When the residents is not involved with patient workups, he or she can see patients in faculty clinics, participate in exercise stress testing, read EKG’s from teaching files and/or ACC patients. The following subjects will be reviewed on the month rotation 1.Evaluation of arrythmias in the post-operative patient 2.Pre-operative risk assessment for the patient with known cardiac disease 3.Evaluation and management of malignant hypertension 4.Use of thrombolytic therapy 5.Evaluation and management of shock in the post-operative patient 6.Endocarditis prophylaxis 7.Evaluation and management of lipid abnormalities 8.Evaluation and management of peripheral vascular insufficiency 9.Recognize common EKG abnormalities 10.Recognize common echocardiographic abnormalities 11.Evaluation and management of patients with left ventricular dysfunction 47 48 ORIENTATION FOR ROTATION IN ENDOCRINOLOGY AND METABOLISM Dear Residents and Students, The Endocrine Division is delighted that you will be taking our Endocrinology and Metabolism Elective. Our clinic is located in Durham near Southpoints Mall off of Hwy 54 (Highgate Specialty Center, 5316 Highgate Dr, Suite 125, Durham NC, 27713. 919-484-1015). The majority of your time will be spent in the clinic working with various attendings and seeing a variety of Endocrine patients. On rare occasions, when too many residents/students are assigned to Endocrinology, you may be asked to spend a few days with the inpatient team. Clinic Operations Highgate Specialty Center opens at 7:30am and closes by 5:30pm. Please arrive by 8:30 each morning and look for Dr. O’Connell who will help coordinate the attending with whom you will work (usually Dr. O’Connell the first day and any day that other attendings are not available). We will try to have you work with almost every attending during your two weeks so you can see a wide variety of patients and styles. Dr. O’Connell is never at Highgate on Thursdays so if your first day is Thursday, simply come and introduce yourself to another attending who is present that day. Dr. Ontjes is usually there on Thursdays and is always amenable to working with residents and students. The clinic is closed most Thursday afternoons to allow everyone to attend Thursday afternoon Endocrine Conferences. Conferences Thursday afternoon Endocrine conferences as described below are from 3 pm to 5:30 pm. You are expected to attend these while on your Endocrine rotation. They are located in the GCRC conference room, 3rd floor bedtower. 3pm: Fellows conference: a faculty member will give a didactic lecture to the fellows/residents 4pm: Endocrine Journal Club: 5pm: 30 minute case presentation and discussion by one of the fellows Evaluations Please give your evaluation form (students) to the Elective Director, who will then distribute it to the fellows and faculty in the division. Evaluations (students and residents) are compiled by the Elective Director after input from other members of the division. We appreciate your attention to these matters and hope that you find your rotation with us to be educational and enjoyable. Please bring any concerns to our immediate attention. Sincerely, Tom O’Connell, MD (pager 216-6359) Resident Elective Director 48 49 Endocrinology and Metabolism Thomas_oconnell@med.unc.edu 49 50 50 51 51 52 52 53 53 54 54 55 Hematology/Oncology Consults Curriculum Updated 6/9/2008 Outpatient Electives for Medical Residents. Out Patient block, Medical Residents Overview: This is a 1month block of time designed to expose medical residents to some of the breadth of outpatient oncology or hematology patients. We suggest that the resident choose either the Oncology block or the Hematology Block and not make a combined block of the various clinics. This will enable the resident to get a good spectrum of one part of this broad field. The resident will see patients along with the attending physician and will be responsible for obtaining histories and examinations, dictate or type consult notes and progress notes, follow up on calls and tests. In many cases there will be a reading list to master. This can be discussed with the attending for each clinic. Residents are also encouraged to participate in the Division conferences and when possible, present at the Case of the month program. Participation at Case of the month should occur if this is offered during the resident’s rotation (The division can let the resident know ahead of time.). Outpatient Rotation. Oncology Monday 7:30 GI Tumor Board. Gravely Gd Floor Breast Cancer Clinic with Dr Carey** 12:30 Monday Lectures Divison lectures.* Breast Cancer Clinic with Dr Carey Tuesday Wednesday 7:30 am Fellows’ Conference*** Room 3004 old clinic (check calendar) Thoracic Oncology Multidisciplinary Thoracic Oncology conference. Gravely Gd floor. Thoracic Oncology Thursday 7:30 am Fellows’ Conference Room 3004 old clinic (check calendar) Friday 7:30 am Head and Neck Conference**. GI Clinic with Dr O’Neil and Dr Bernard GU Clinic Check Breast Conference 10:30 to 12 Gravely Gd Floor Breast Oncology 1:15 GU tumor board. Gravely Gd Floor GU clinic ** If Dr Carey’s clinic does not take place go to head and neck clinic. Head and Neck Conference on Friday is optional but encouraged if you have seen these patients. ***Beginning in 1/2008, Fellows’ Conference is switching to Tuesdays. 55 56 Outpatient Rotation Hematology Monday Tuesday 7:30 am Fellows’ Conference Room 3004 old clinic (check calendar) ** Hemophilia Sickle Cell Clinic with Clinic Dr Key and Ma 12:30 Monday Division Lectures * Coagulation Sickle Cell Clinic with Clinic Dr Moll Wednesday Thursday 7:30 am Fellows’ Conference Room 3004 old clinic (check calendar) ** Heme Parker Malignancy conference Clinic with at 11am if Drs time. VanDeventer Gravely Gd and Floor Voorhees Friday 7:30 am Fellows’ Conference. Room 3004 Old clinic Heme clinic, Dr Ma 1PM Heme conference Heme clinic, Dr Ma Check with the Division re the Conference on Mondays for titles and place **Beginning in 1/2008, Fellows’ Conference is switching to Tuesdays. Check with Dr Ma. She may be moving her clinic to Thursdays. When that happens the clinic will be off site and you will not need to go to Parker Conferences. 56 57 PULMONARY DISEASES AMBULATORY CURRICULUM In overview, the medical resident’s activities will mirror the responsibilities of the Pulmonary consult Fellow, i.e., evaluation of inpatient and outpatient referrals and interpretation of standard pulmonary function tests. The resident will interact closely with the Pulmonary consult Fellow and Attending. The overall educational goals will be accomplished through several formats: 1. Daily inpatient consults on all non—ICU pulmonary referrals (we average -1.5 consults per day). 2. Interpretation of pulmonary function tests and review of tests with the Attending physician. We perform about 600 individual pulmonary function tests per month. Specific attention will be focused on interpretation of blood gases and spirometric parameters. Understanding the indication for lung volume and DI.ICO tests will be a goal for the resident’s experience. 2. Work—up of a new pulmonary outpatient referral and follow—up of selected patients in each Wednesday’s day—long clinic. In conjunction with the consult fellow and clinic attending, this will involve selecting and interpreting appropriate pulmonary function tests. 4. Evaluation of sleep—clinic outpatient referrals on Friday mornings and review of sleep apnea studies in conjunction with a senior Fellow and the Attending. The goal will be to better define for the resident indications for obstructive sleep apnea studies. 5. Evaluation of outpatient “walk—in” referrals or outpatient consults who need to be “added—on” and seen on days other than Wednesday. We see 2—4 new patients per week by this route. 6. Presentation and discussion of cases at the weekly medicine— radiology—chest surgery— oncology conference (1 hour). 7. Three didactic conferences (1 hour each) per week related to critical care medicine, clinical topics, and review of research papers. These presentations draw on faculty and fellows from Pulmonary, Infectious Disease, Radiology, Critical Care Surgery, Anesthesiology, & etc. 8. The weekly pulmonary division clinico—pathologic “work” conference (2 hours) that involves presentation of difficult, complex, and/or interesting cases. Pathophysiologic concepts are emphasized. Although the consult service performs a number of procedures, we will not emphasize the technical aspects of those studies except for aspects of the thoracentesis and/or pleural biopsy. The opportunity to observe decision—making about bronchoscopic procedures, and to visualize endobronchial anatomy during bronchoscopy, will contribute to the resident’s appreciation for the role of this procedure in the evaluation of pulmonary disease. 9. In summary, the medical resident will enjoy an integrated experience of inpatient and outpatient evaluations, learn the indications and interpretation of pulmonary functions tests, 57 58 have exposure to patients referred for sleep—apena studies (and perhaps learn some indications for these referrals), better appreciate the role of fiberoptic bronchoscopy in evaluation of pulmonary disease, and expand their pulmonary physiologic concepts. Overall, this resident rotation complements the resident’s ICU and inpatient exposure to pulmonary diseases. It provides an experience that will be useful for most internal medicine physicians because pulmonary disease is a common cause for clinic visits to the internists. 58 59 DIGESTIVE DISEASES AMBULATORY CURRICULUM On the Digestive Diseases Consultation Service, residents have the opportunity to see patients with gastroenterology as well as hepatology disorders. The following subjects will be reviewed on the month rotation. 1. Evaluation and treatment of diarrhea 2. Evaluation and treatment of jaundice 3. Inflammatory bowel diseases 4. Hepatitis - viral and non-viral 5. Diagnosis and management of peptic ulcer disease 6. Nutritional support - enteral and intravenous 7. Colonoscopy - indication and screening 8. Diagnosis and management of pancreatitis 9. Diagnosis of esophageal motility disorders 10. Evaluation and treatment of abdominal pain 11. Diagnosis and management of cirrhosis 12. Liver transplantation - indicators and outcomes 13. Diagnosis and management of GI bleeding 14. Appropriate use of radiologic studies of the gastrointestinal system 15. Evaluation and management of gallstones/gallbladder diseases 59 60 INFECTIOUS DISEASE AMBULATORY CURRICULUM Role: Residents play an important role on the consult service and in the clinic, where they help to manage outpatients with AIDS, chronic fatigue syndrome, and a variety of different infections including endocarditis and osteomyelitis. Residents are supervised by an attending physician. Teaching Conferences: Teaching conferences include a Wednesday clinical case conference at 8:30 a.m. and a Friday 8:30 a.m.conference which is didactic and/or research oriented. Topics: Topics covered through these conferences can be organized according to an organ system approach in Infectious Disease. These include 1) central nervous system infections, including meningitis and encephalitis; 2) infections of the eyes, ears, nose and throat; 3) infections of the upper and lower respiratory tracts; 4) infections of the cardiovascular system including endocarditis; 5) infections of the intestinal tract including infectious diarrhea and intra-abdominal catastrophe; 6) infections of the urinary tract, including sexually transmitted diseases; 7) systemic infections, including HIV; 8) infectious disease syndromes, including chronic fatigue syndrome. General lectures also include a) antibiotics, b) host defenses, c) microbial pathogenesis. Pathogenesis includes discussion of worms, protozoans, fungi, viruses and bacteria. 60 61 Resident’s Responsibilities for Consults and Ward Service Rounds will begin at 1:30 PM in the Clinical Microbiology lab with discussion of sterile fluid infection, review of new micro data and “unknown” case presentations from Microbiology faculty. Consultations & Rounds: Residents are responsible for full evaluations of patients seen in consultation. Residents are responsible for following in-patients daily, presenting patients during rounds, discussing differential diagnoses with the attending, and writing appropriate notes in the medical record. The on-call schedule and sequence of assignments will be discussed by the Attending or the Fellow at the beginning of the rotation. Conferences The following conferences are held weekly by either the Division of Infectious Diseases or the Department of Medicine. All listed conferences are required. Day/Conference Time Place Wednesday: Case Presentation 8:30am Orthopedic Conference Room Dept. of Medicine Grand Rounds 12:00pm Clinic Auditorium Friday: ID Didactic/Research Conference 8:30am Clinic B Conference Room Thursday: 61 62 RHEUMATOLOGY / ORTHOPAEDICS AMBULATORY CURRICULUM Welcome to the Division of Rheumatology and Immunology. Although rheumatologic and autoimmune disease are, in the aggregate, extremely common, physicians who miss this special opportunity for a rotation on a rheumatology service may never acquire the knowledge and skills required for caring for patients with these disorders. For this reason, emphasis during your rotation will be on learning “nuts and bolts” rheumatology: a) b) C) d) e) f) signs and symptoms of the different arthritides performance of a musculoskeletal history and exam construction of common differential diagnoses choice and interpretation of laboratory tests and x-rays arthrocentesis and soft-tissue injection techniques choice of therapy for commonly encountered conditions. In addition, you will learn the basic elements of the pathogenesis and disease expression in rheumatologic disease. These educational objectives will be accomplished by seeing disease. These educational objectives will be accomplished by seeing patients, clinical discussions with faculty and fellows, literature searches and reviews, various lectures and conferences, and Bob Berger’s “tool-kit.” Rheumatology is largely an out-patient specialty, and the major block of your time will be spent in the Musculoskeletal Module in the ACC. This module houses rheumatology and orthopaedic examining and consult rooms, facilities for physical therapy, occupational therapy, patient education, a library, and a special bone and joint x-ray suite. You will also see in-patient consults at UNCH. Scheduling of consult rounds, on-call responsibilities, your time in clinic, etc., will vary from month-to-month. Schedules and responsibilities will be discussed with you by the Attending and/or Fellow at the beginning of your rotation. There are only four rules: 1) Be in clinic on time. Medicine residents and students should report to clinic at 9:00am. 2) If you are not called to see an urgent consult, be in the clinic. 3) Formal consult rounds will not be held until 3:30pm in order to minimize conflicts with your ambulatory care experience in the clinic. 4) Turn in the evaluation sheet and list of patients seen to me at the end of your rotation. Resident’s Responsibilities for Clinics and Consults Report to the musculoskeletal module, 1st floor, Ambulatory Care Center at 9:00 am following Morning Report. Meet for Consult Rounds at the film assembly desk (“cage “) in Radiology at the times designated by the Attending or Fellow. Clinic Responsibilities: Residents will perform complete evaluations of new patients and return patients, as assigned by the Attending. The nursing staff may also direct residents to do initial work-ups on patients. Residents will be responsible for presenting patients to the Attending, developing a therapeutic plan, discussing differential diagnoses with the attending, and completing a write-up for the medical record. Consultations & Rounds: Residents are responsible for full evaluations of patients seen in consultation. Residents are responsible for following in-patients daily, presenting patients during rounds, discussing differential diagnoses with the attending, and writing appropriate notes in the medical record. The on-call schedule and sequence of assignments will be discussed by the Attending or the Fellow at the beginning of the rotation. Schedule 62 63 The following schedule is subject to some change. Please check with your attending on the first day of the rotation to confirm the following schedule. Monday 8:30 - 3:30 Clinic Tuesday 8:30 - 12:00 Clinic 10:00-11:00 Rheumatology Grand Rounds 3:30-5:00 Clinic or Consult Rounds 12:00-1:00 Immunology Journal Club 2:00-3:00 Research-inProgress 3:30-5:00 Clinic or Consult Wednesday 8:30- 3:30 Clinic 1:OO 3:30 Clinic Thursday 9:00-3:30 Clinic 3:30 - 5:00 Clinic or Consult Rounds’ Friday 8:30 - 3:30 Clinic 3:30-5:00 Clinic or Consult Rounds 3:30- 4:30 Clinic or Consult Rounds Sounds’ Please note that this schedule only includes required events. Optional conferences, etc. are listed separately. • NOTE: Consult rounds are held 2-3 days per week. Days of week may vary in different months. Formal consult rounds will not be held earlier than 3:30. Scheduling of consult rounds far the month will be defined by me Attending at Fellow at the beginning of each rotation. Conferences The following conferences are held weekly by either the Division of Rheumatology and Immunology or the Department of Medicine. Please note that several are required for medical students and others are optional. For more in formation regarding speakers and titles, contact the Rheumatology Division Office in 3330 Thurston Building, (919) 966-4191. Day/Conference Required/Optional Time Place Monday Immunology Journal Club 10:00am 3280 Thurston Optional Rheumatology Grand Rounds Research-I n-Progress 12:00noon 2:00pm 3280 Thurston 3280 Thurston Required Optional Wednesday Lecture:Program On Aging 12:00 Noon Clinic Auditorium Optional Thursday Dept. of Medicine Grand Rounds 12:00 pm Clinic Auditorium Required Friday Ambulatory Care Conference 12:00 Noon Clinic Auditorium Optional 63 64 Nephrology Ambulatory Curriculum Nephrology Consultation Service Resident Curriculum Role of Resident Evaluation and discussion of patients with kidney disease, hypertension, and disorders of fluid, and electrolyte and acid-base balance disorders in the consultative setting under the supervision of Nephrology faculty. Consults Residents will see both hospitalized and ambulatory patients in consultation on a daily basis, unless assigned to their continuity clinic. Patients with a wide range of nephrologic diagnoses will be seen and discussed with the Nephrology Attending and fellow. Residents are expected to communicate consultative recommendations with the referring physicians, and to provide ongoing follow up while on the rotation. Curriculum Topics to be discussed during rounds as well as during formal didactic sessions will include the following: Evaluation of kidney structure and function o o o o o Urinalysis Measurement of GFR Evaluation of proteinuria Measurement of urinary electrolytes Renal imaging techniques Chronic kidney disease Acute kidney injury General principles of dialysis o o o Hemodialysis Peritoneal dialysis Continuous renal replacement therapies Critical care nephrology Metabolic acidosis Metabolic alkalosis Disorders of water metabolism (hyponatremia and hypernatremia) Disorders of potassium and magnesium metabolism Disorders of calcium, phosphorus and bone metabolism Overview of evaluation and treatment of hypertension 64 65 Glomerular syndromes o o nephritic syndrome nephrotic syndrome Diabetic nephropathy Principles of kidney transplantation Clinics Participation in several Nephrology Subspecialty Clinics is available to residents interested in seeing patients with specific diagnoses and is optional. Residents will see patients under the direction of one of the Nephrology Attendings. Monday PM Hypertension Clinic Tuesday AM and PM Transplant Clinic Thursday AM and PM Vasculitis Clinic Renal Conferences Residents are encouraged to attend the following Divisional Educational Conferences during the rotation: Conference Time Leader/Organizer Topic Hypertension 2nd and 4th Review of literature related to Drs. Romulo Journal Club Mondays hypertension Colindres and Steven 4-5 pm Transplant Journal Club Grossman 1st and 3rd Review of literature related to Mondays kidney transplantation Dr. Randy Detwiler 4-5 PM Fellows Tuesday Review of topics in conference 4-5 pm clinical nephrology and Drs. Romulo Colindres and Gerald Renal physiology Nephrology Wednesday Review of nephrology Journal Club 8:30-9:30 am literature; study of issues Hladik Nephrology Division related to design and analysis of clinical studies Nephrology Wednesday Conference 4-5 pm Clinical nephrology Nephrology Division ADOLESCENT MEDICINE AMBULATORY CURRICULUM 1) Knowledge of the epidemiology of adolescent health issues • Describe the major causes of adolescent morbidity and mortality. • Describe the ways that these issues are addressed in routine adolescent care. 65 66 • Understand that the rationale for guidelines for preventive adolescent health care is based on the major causes of adolescent morbidity and mortality. • Describe guidelines for routine health screening, including laboratory tests. 2) Skill in communicating with adolescents • Recognize that adolescents should be interviewed privately as a routine part of physician visits. • Describe how the issues of consent and confidentiality are managed with minor adolescents. • Perform a thorough history, including an adolescent risk assessment. 3) Understanding of normal adolescent development • Describe normal psychosocial and co2nitive development. • Recognize that the timing of psychosocial and cognitive development is independent of pubertal development. • Accurate assessment of Tanner staging. • Describe the range of normal variation in timing of pubertal changes. • Recognize and manage common concerns of puberty (e.g. Am I normal? Gynecomastia in males, Acne, etc.). 4) Sexuality • Perform a complete sexual history in a sensitive and age-appropriate manner. • Demonstrate appropriate anticipatory guidance and risk-reduction counseling. • Perform a complete pelvic exam including collection of cervical cytology and tests for STDs. • Perform a male genital examination including tests for STDs. • Teach self-breast examination and self-testicular examination. • Provide contraception. • Instruct and demonstrate how to use condoms. 5) Common acute and chronic medical problems of adolescence • Recognize, evaluate, and manage common medical problems of adolescence (e.g. acne, dysmenorrhea, STDs, pregnancy diagnosis, scoliosis, Osgood- Schlatter disease, headaches, etc.). 66 67 • Describe a strategy for evaluation and management of chronic somatic symptoms, including recognition that mental health problems may present as somatic symptoms. • Understand the influence of puberty and adolescent development on chronic illness. • Describe the issues regarding the transition of adolescent patients with chronic illness to adult care. 6) Identification and management of mental health problems • Recognize abnormal psychosocial development. • Recognize that significant psychiatric disease can present in adolescence. • Perform an assessment for depression and suicide, and describe appropriate management of patients with varying risk of suicide. • Understand that mental health issues are often associated with multiple risktaking behaviors. • Describe strategies to persuade adolescents and parents of the need for psychological evaluation and treatment. 7) Substance use • Perform an assessment of substance use, including tobacco, alcohol, illicit drugs, and steroids. • Describe risk factors for substance abuse. • Describe physical symptoms or signs associated with substance use. • Describe management plans for adolescents with varying risk of substance abuse. • Understand that mental health problems may be associated with substance use. 8) Nutrition eating disorders • Perform a nutrition history. • Demonstrate ability to accurately assess growth using height, weight, and BMI. • Describe counseling regarding healthy foods and eating patterns. • Describe management for mild to moderate obesity. • Recognize symptoms and signs of eating disorders, and describe strategy for appropriate evaluation and management. 9) Sports Medicine • Perform a pre- participation sports examination. • Describe the indications for limiting/requiring protective devices for sports activities. • Describe the initial management of common sports injuries. • Understand the importance of screening for abnormal eating patterns and steroid use 67 68 GERIATRIC MEDICINE CURRICULUM Outpatient Geriatric Curriculum: Residents in Internal Medicine who complete the Outpatient Geriatric Rotation will be expected to meet the above goals in knowledge, attitude, and skill sets. Residents will work at all times with a Faculty member from the Division of Geriatric Medicine and will rotate through the following sites of care: 1. Long Term Care Communities: Residents will work with faculty and Geriatric Fellows and will see and evaluate patients who are in the outpatient clinic setting as well as the health center/skilled nursing care area in these communities. They will see patients who are older and completely independent who are followed for continuing care at the clinics on site, as well as patients with dementia and other functional limitations who reside in the nursing care area. 2. Hospice: Residents will evaluate patients with the hospice team by doing home visitations. Residents will also meet regularly with the hospice team and director to discuss patient management issues. 3. Geriatric Evaluation Clinic: Residents will work with faculty and Geriatric Fellows in the Evaluation Clinic by seeing and evaluating older patients with complicated issues who have been referred for complete geriatric assessments. Residents will work with an interdisciplinary team to develop a plan of care for patients. 4. Senior Center: Residents will work with one of our Faculty members and a trained Physical Therapist to conduct screenings and assessments of older adults. 5. Residents will also spend time with the Geriatric Psychiatry inpatient unit, Rehabilitation clinic, and memory disorders clinic. Residents may also chose to have additional time with faculty who work with incontinence, urogynecology, dementia, movement disorders, sleep disorders, or other specific interests. 6. Residents with interests in subspecialty training may chose to do additional work with faculty in congestive heart failure, nephrology, intensive care, or other areas of interest. 7. Residents will meet weekly with the division and the fellows for educational conferences. Based upon: 2004 The American Geriatrics Society: Curriculum Guidelines for Geriatrics Training in Internal Medicine Residency Programs. The AGS Education Committee. Updated Jan 2004. 68 69 PGY -1 Continuity Elective Enhanced Intern Outpatient Education Rotation and Ambulatory Medicine Tract & Chief Residency Restructuring Learners: Interns interested in careers in outpatient internal medicine. The emphasis will be acquiring outpatient skills in a diverse primary care setting. The acquired skills and experience will be generalizable to other outpatient internal medicine specialties. Objectives: 1. Fulfill the traditional core residency competencies of patient care, medical knowledge, professionalism, and interpersonal skills and communication in the outpatient setting. The resident will acquire intensive disease and condition specific outpatient training in the following domains: a. Diabetes mellitus b. Anticoagulation c. Chronic pain and comorbid psychiatric conditions d. Acute care medicine through the Same Day Clinic e. Continuity clinics f. Travel medicine through existing Internal Medicine Travel Clinic g. Women’s health h. (Possibly dermatology. Dean Morrell open to this but department has had faculty shortage.) 2. Acquire first-hand experience with new competencies of practice-based learning and systems-based practice within Internal Medicine Clinic Enhanced Care Program a. Learn quality improvement methodology b. Learn the importance of patient tracking through patient registries/databases c. Work in multidisciplinary teams consisting of physicians, clinical pharmacists, nurse practitioners, physicians assistants, dieticians, nurses, care assistants, lab personnel 3. Provide intensive continuity with a panel of patients early in residency Curriculum: Existing curriculum for residents on Continuity Elective with selective adaptations. Infrastructure and Template: 1. Capitalize on existing UNC Internal Medicine and Enhanced Care Programs that already provide an educational environment for medical students, residents in continuity clinic, residents on continuity elective, and pharmacy students and residents. 2. Rotation would last one month 69 70 Sample Schedule Mon Tues Am CC Pain Noon Pm Coag Precept/Mento r Wed DM Ambulator y Conference SDC Thurs Conferences, QI Project, Reading Grand Rounds Fri WH CC SDC Legend: DM=Diabetes program; Pain=Chronic pain management; Coag=Anticoagulation management; SDC=Continuity Clinic; TC=Travel Clinic; CC=Continuity Clinic; Preceptor/Mentor=One-on-one preceptorship and mentorship in attending clinic WH=Women’s health Features: 1. Two continuity clinics per week. 2. Dedicated continuing education time on Thursday 3. Balanced outpatient experience consisting of acute, continuity, women’s health, travel clinic, and disease specific care. 4. Preceptorship with mentoring and role-modeling by experienced internal medicine faculty Resources: 1. Money: None requested 2. Faculty: Sufficient 3. Increased intern time 4. Increased administrative support needed (see below). Proposals for Securing More Intern Time Options: 1. Add Outpatient Internal Medicine (OIM) month as third non-inpatient, non-ER month for selected interns interested in pursuing outpatient internal medicine. This would constitute an ambulatory medicine tract. 2. Invite incoming interns to request OIM month as a rotation. Commentary: Would be a good recruiting tool. Could compensate for lost intern capacity by also offering hospitalist tract to upper levels who might want to pursue hospital medicine. Capacity: One intern per month=One intern FTE. (Would prefer incremental approach with fewer intern months for first year or two to establish program.) Practice-Based Learning Deliverable: QI project Other Responsibilities Consider recruiting motivated and interested residents in participating in the decision-making structure of the UNC Internal Medicine Clinic a la the 70 71 University of Nebraska model that has cultivated ownership of clinic experience through substantive input of residents who sit on “board of directors” of clinic. This will be an enhance systems-based practice experience (i.e. cultivating ownership of patients through cultivation of ownership of the work environment. How can you foster learning of systems-based practice if residents feel they have no ability to influence the system?). 71 72 Administrative Support for Expansion of Outpatient Education Experience Review of Accomplishments to date: 1. Established continuity elective (COE) as novel, diverse outpatient experience for residents. 2. Established SDC as venue for acute outpatient medicine care after Urgent Care was decommissioned by hospital 3. Initiated QI project for improvement of HTN. Administrative Resources: 1. ½ FTE for QI project (Annie Whitney, MS) 2. Considerable burden of administrative work for COE and SDC currently being performed by Dr. Chelminski and other general medicine staff. Proposals for Augmenting Administrative Support: 1. Hire purely administrative person (less desirable as this person will probably not have ownership and show initiative. 2. Designate ambulatory chief resident. Two options: a. ?Third chief (expensive; chief residents paid for by department) b. Retain current complement of two chief residents but designate one as ambulatory chief. c. Ambulatory chief would be expected to continue her or his continuity clinic (analogous to chief residents attending on wards). Division of General Medicine Commitments: 1. Office space for administrative chief. 2. Official and substantive role in the decision-making processes of the clinic. 3. Sponsor attendance at annual SGIM meeting. 4. Provide certificate of advanced ambulatory competency to outpatient chief 72 73 PGY -2/3 Continuity Elective Resident Continuity Elective Rationale Chronic disease has replaced acute disease as the principle consumer of health care resources; more than 75% of resources are expended on chronic illness care. Most chronic disease management occurs in ambulatory settings. Internal medicine residencies, however, have historically trained physicians in managing acute medical problems and have not provided structured, continuous training in ambulatory and chronic illness care. Chronic illness care poses a different set of challenges than acute illness care where patients are symptomatic and understand the imperative for intensive, structured medical care. Chronic illness often produces no symptoms, and prevention is the focus of management. Both providers and patients need to be aware that the absence or stability of symptoms does not preclude intensive patient care that is informed by data from clinical trials. This challenge requires a new set of skills that traditionally have not been imparted in internal medicine residencies. Objectives 1. To improve resident training in ambulatory medicine through exposure to chronic disease management programs in the ambulatory care setting. 2. To develop skills that will prepare residents to provide high quality chronic illness care, regardless of which specialty of internal medicine they pursue. Residents will gain knowledge and expertise in the following areas: Knowledge base for effectively managing chronic illness. Systems for tracking patient outcomes that improve the quality of care. These systems rely on ancillary medical professionals, electronic medical records, databases and information technology. Continuous quality improvement. This elective addresses a core competency emphasized by the ABIM for Improving Performance in Practice. The UNC model has been presented at national meetings and is being adopted at other institutions, though it has not yet directly been applied to resident education at our institution. Collaboration with mid-level providers such as clinical pharmacists, physician assistants and nurse practitioners involved in chronic disease management Structure 1. Combine Urgent Care months with structured ambulatory care time over a two month period. Total Urgent Care time will remain 73 74 2. 3. 4. 5. 6. neutral at one month. By coupling acute and chronic medical care, this elective does not seek to de-emphasize the importance of acute care; rather, it will prepare residents for the realities of independent practice where both acute and chronic issues are addressed continuously. The elective will be offered to residents at all levels of training. It will be an alternative to other electives and provide an additional outpatient option. The resident will rotate through the existing disease management modules: anti-coagulation, chronic pain, diabetes mellitus. The resident will manage patients independently using approved protocols. The resident will receive guidance from attending physicians and clinical pharmacists experienced with systematic disease management. The resident will spend one half day a week seeing patients independently with an attending physician (team leader) who will provide direct teaching related to ambulatory internal medicine on a one-on-one basis. (Recall that the usual precepting and continuity clinic experience diffuses an attending’s attention over up to four residents at a time.) The resident and attending physician will be templated for 12 to 14 patients in this half day. Billing will therefore not need to adhere to the Primary Care Exception. The resident will spend one half day per week in her or his own continuity clinic. The resident will have the option to schedule her or his patients for close follow up during other half days at the ACC when clinically indicated. This will provide an experience of close continuity that is currently lacking in resident continuity clinics. Sample Elective Monday Am DSM: Anticoag Pm CC with team leader Template Tuesday Wednesday Thursday Friday CC UCC Grand UCC Rounds/Conferences DSM: DM UCC DSM: Pain UCC Legend DSM= Disease state management Anticoag= Anticoagulation management DM= Diabetes mellitus management 74 75 Pain=Chronic pain management Logistics 1. The new elective will have a capacity for 12 residents in the first year. 2. This will mean that two residents will be accommodated simultaneously. Team Leaders for Disease Management Precepting 1. Michael Pignone, MD, MPH 2. Darren DeWalt, MD, MPH 3. Paul Chelminski, MD, MPH 4. Second full time ACC clinician (?Cristin Colford) 75 76 Enhanced Care Elective Rotation UNC General Internal Medicine Clinic Ambulatory Care Preceptorship Ambulatory Care Center, UNC Hospitals Primary Preceptor Paul Chelminski, MD, MPH Assistant Professor of Medicine Pager: (919) 216-6163 Office: (919) 966-0471 Email: paul_chelminski@med.unc.edu Disease Management Preceptors Betsy Bryant Shilliday, Pharm.D., CDE, CPP Clinical Pharmacist Practitioner Assistant Professor of Medicine Assistant Clinical Professor of Pharmacy Pager: (919) 216-5723 Office: (919) 843-0391 Email: betsy_bryant@med.unc.edu Robb Malone, Pharm.D., CDE, CPP Clinical Pharmacist Practitioner Assistant Professor of Medicine Assistant Clinical Professor of Pharmacy Pager: (919) 216-5736 Office: (919) 843-0391 Email: rmalone@med.unc.edu Timothy Ives, Pharm.D., MPH, CDE, CPP Clinical Pharmacist Practitioner Associate Professor of Pharmacy and Medicine Pager: (919) 216-0193 Office: (919) 843-0391 76 77 Email: tjives@med.unc.edu Goal The Enhanced Care elective incorporates various components of outpatient medicine including disease management clinics, continuity clinic, urgent care clinic, and one-on-one preceptorship with an attending physician. This elective will provide the opportunity for the learner to build upon information acquired in his/her didactic education and to apply the knowledge and skills in direct patient care activities in the primary care setting and specialty outpatient clinics. This experience will be gained primarily under the Preceptorships of Drs. Betsy Bryant Shilliday, Robb Malone, Tim Ives, and Paul Chelminski. Practice Site Description The Enhanced Care team is an interdisciplinary team that provides disease state management services to patients who have established care with a primary care physician in the UNC General Internal Medicine (GIM) clinic. The patient population consists of adults, ages 18 and older with a variety of medical conditions. Patients can be referred to any of three existing programs: 1) Anticoagulation 2) Diabetes and/or 3) Chronic Pain. Clinical experiences afforded to the learner include, but are not limited to: anticoagulation, hypertension, hyperlipidemia, diabetes mellitus, depression, arthritis, congestive heart failure, cardiovascular risk reduction, chronic pain and osteoporosis. The clinic is located on the 3rd floor of the Ambulatory Care Center (ACC) on Mason Farm Road, Chapel Hill, North Carolina. Hours & Clinic Descriptions Hours of the rotation are typically Monday through Friday 8am to 5pm. However, afternoon hours may vary depending on patient workload and issues that arise during clinic hours. Clinic Template Monday Tuesday Am UCC DSM: Anticoag Pm UCC Wednesday Thursday Friday DSM: Pain Grand UCC Rounds/Div.Meeting DSM Meeting Preceptorship DSM: DM CC UCC with attending UCC: Urgent Care Clinic; DSM: Disease Management; CC: Continuity Clinic The Urgent Care Clinic will be Mondays and Fridays 8am to 5pm. This clinic will familiarize the learner with a variety of acute medical issues. The evaluation of this component of the rotation will occur through the 77 78 normal evaluation process through supervising attending physicians and not separated out to this rotation. The Continuity Clinic will be on Thursday afternoons and will allow the resident learner to increase clinic time for this 2 month block of time. The afternoon clinic slots will begin at 1:30pm. The evaluation of this component will be under the normal evaluation process of supervising attending physicians and not separated out to this rotation. The one-on-one physician preceptorship will allow the resident learner to work in tandem with an attending physician in his or her outpatient clinic to improve outpatient management skills. The Anticoagulation Clinic consists of a Clinical Pharmacist Practitioner, Physician Assistant, Nurse Practitioner, and Registered Nurse who see patients for warfarin initiation/education, INR monitoring, warfarin dosage adjustment and enoxaparin (Lovenox®) bridging. Patients are scheduled for 15-minute appointments as often as necessary but return to clinic at least once every four weeks while on warfarin therapy. The Diabetes Clinic is a multidisciplinary clinic, consisting of Clinical Pharmacist Practitioners, Nurse Practitioner, Registered Dietician and Research Assistants, designed to medically manage and educate patients with uncontrolled diabetes. Patients are followed until their A1c reaches goal < 7%. Though emphasis is placed on diabetes management, clinical care encompasses cardiovascular risk reduction, hypertension, hyperlipidemia, congestive heart failure, depression and arthritis. The Chronic Pain Clinic consists of a Clinical Pharmacist Practitioner, Nurse Practitioner, and Research Assistant specializing in disease management of chronic pain syndromes and associated psychiatric disorders (depression and anxiety). Patients are assessed using screening tools such as the Brief Pain Inventory (BPI) and Center for Evaluation Studies of Depression (CES-D), and use of physical assessment at every visit. Learners will be exposed to the prescribing and use of chronic controlled substances and adjunct analgesics. They will also become proficient in the outpatient monitoring of this patient population, including the potential for medication diversion. Global Program Objectives 78 79 3. To improve resident training in ambulatory medicine through exposure to chronic disease management programs in the UNC Internal Medicine Clinic. 4. To develop skills that will prepare residents to provide high quality chronic illness care, regardless of which specialty of internal medicine they pursue. Residents will gain knowledge and expertise in the following areas: Knowledge base for effectively managing chronic illness. Systems for tracking patient outcomes. These systems rely on ancillary medical professionals, electronic medical records, databases and information technology. Continuous quality improvement and systems-based practice which is a core competency required by the ABIM for Improving Performance in Practice. The resident will have opportunities to performing chart audits of their clinic patients with diabetes. After completion of the self-audit the resident will be able to consider how their performance can improve with their individual practice or with the system as a whole. Collaboration with mid-level providers such as clinical pharmacists, physician assistants and nurse practitioners involved in chronic disease management Specific Program Objectives General: 1. Develop a better understanding of the roles and functions of disease management programs. 2. Assess potential barriers to care including literacy, psychosocial issues, finances, transportation, etc. and assist patients with those obstacles. 3. Focus clinic visit time on the specific chronic disease versus the patient’s acute problems or entire problem list. 4. Adopt a better understanding of the UNC pharmacy benefit program and disease management contracts. Anticoagulation: 1. The learner should familiarize himself/herself with CHEST guidelines. The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004 Sept; 126(3) supp. 2. Understand how to better manage warfarin therapy and bridging with low molecular weight heparin, while taking into account patient specific bleeding and thromboembolic risk factors. 3. Determine an appropriate INR goal for specific patient indications based on CHEST guidelines, learn how to properly adjust warfarin 79 80 dose to target the goal INR and how to dose low molecular weight heparin for various bridging procedures. 4. Assess signs/symptoms of bleeding/bruising. 5. Review current medication list, update in medical record and address any drug-drug interactions, including over-the-counter (OTC) medications such as aspirin and NSAIDs. 6. Educate patient on vitamin K content of diet and importance of consistency while on warfarin therapy. 7. Educate patient on role of warfarin therapy in relation to their indication for therapy, discussing duration of therapy. 8. Educate patient on proper use of OTC items such as pain relievers, herbals, vitamins, supplements, etc. 9. Adjust weekly warfarin dose to target goal INR for patient’s indication using nomograms and patient history. 10. Assess past medical history (PMH) for factors which put the patient at an increased risk for thromboembolic events. 11. Assess PMH for factors which may increase the patient’s risk for bleeding complications from warfarin therapy. Diabetes: 1. The learner should familiarize himself/herself with ADA Guidelines 2005, JNC VII, and NCEP guidelines. 2. Obtain a focused CV and DM history and ROS. 3. Perform foot exams. 4. Assess vaccination status. 5. Assess tobacco use, determine stage of change, and recommend appropriate intervention. 6. Make appropriate referrals to ophthalmology and/or nutrition. 7. Assess current DM, HTN, and lipid therapy for appropriateness. Determine goal blood pressure and lipids based on patient’s comorbid conditions and recommend additional therapy with evidence-based reason, if needed and according to protocols. 8. Assess current level of diabetes control, develop a medication regimen and monitoring plan and properly adjust and/or add medications to obtain glycemic goals. Pain: 1. Assess the type and level of pain, develop a medication regimen and monitoring plan to manage any combination of pain (e.g., nociceptive, neuropathic, inflammation) 80 81 2. Assess and manage co-morbid conditions associated with pain (e.g., depression, anxiety, sleep disorders, hypertension). 3. Learn how to more effectively control the prescribing of controlled substances in patients with chronic pain to protect oneself, the patient and the community from potential drug abuse and diversion (e.g., use of urine toxicology screening). Responsibilities and Activities Take an active role in patient care. Collect pertinent information from each patient’s medical record in preparation for clinic visits. Familiarize oneself with disease management protocols for each program. Formulate a comprehensive, evidence-based, patient-centered therapeutic plan for each patient. Work collaboratively with preceptors during clinic visits. Educate and collaborate with patients and their families/caregivers at their respective literacy level to ensure a patient-centered model of care. Document patient care activities for each visit as directed by preceptor Provide timely patient follow-up via telephone when necessary. Attend grand rounds Thursday mornings at 7:30am, when applicable in the 4th Floor Old Clinic Auditorium. Attend General Medicine Division meeting every Thursday morning at 8:30am in the 5th Floor Conference Room of Old Clinic Building. Attend Disease Management meeting every Thursday morning at 9:30am in room 3004 (Hematology/Oncology Conference Room), 3rd Floor Old Clinic Building. Present at least one journal club of current literature related to pertinent chronic disease topics, with one being presented at General Medicine Division meeting at designated time. Actively participate in ongoing disease management projects and Continuous Quality Improvement (CQI) initiatives pertinent to the disease management programs. Required Readings All required readings can be found in hard copy format as well as full text on a CD kept in the Learner’s Notebook. Disease Management: 1. Ofman J, Badamgarav E, Henning J et al. Does Disease Management Improve Clinical and Economic Outcomes in Patients with Chronic Diseases? A Systematic Review. Am J Med. 2004;117:182-192. 81 82 2. Bodenheimer, T.; Wagner, E. H., and Grumbach, K. Improving primary care for patients with chronic illness. JAMA. 2002 Oct 9; 288(14):1775-9. Anticoagulation: 1. The Pharmacology and Management of the Vitamin K Antagonists: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004;126:204S-233S. 2. Harrison L, Johnston M, Massicotte P et al. Comparison of 5 mg and 10 mg Loading Doses in Initiation of Warfarin Therapy. Annals of Internal Medicine. 1997;126:133-136. 3. Kovacs M, Rodger M, Anderson D et al. Comparison of 10 mg and 5 mg Warfarin Initiation Nomograms Together with Low-MolecularWeight Heparin for Outpatient Treatment of Acute Venous Thromboembolism. Ann Intern Med. 2003;138:714-719. 4. Ridker P, Goldhaber S, Danielson E et al. Long-Term, LowIntensity Warfarin Therapy for the Prevention of Recurrent Venous Thromboembolism. NEJM. 2003;348:1425-1434. 5. Kearon C, Ginsberg J, Kovacs M et al. Comparison of LowIntensity Warfarin Therapy with Conventional-Intensity Warfarin Therapy for Long-Term Prevention of Recurrent Venous Thromboembolism. NEJM. 2003;349:631-639. Supplemental Readings: 6. Antithrombotic Therapy for Venous Thromboembolic Disease: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004;126:401S-428S. 7. Antithrombotic Therapy in Atrial Fibrillation: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004;126:429S-456S. 8. Antithrombotic Therapy in Valvular Heart Disease--Native and Prosthetic: The Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004;126:457S-482S. Diabetes: 1. Krentz A, Bailey C. Oral Antidiabetic Agents: Current Role in Type 2 Diabetes Mellitus. Drugs. 2005;65(3):385-411. 82 83 2. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomized placebocontrolled trial. Lancet. 2003;361:2005-2016. 3. Gaede P, et al. Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet. 1999;353: 617-622. 4. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and reisk of complications in patients with type 2 dieabetes (UKPDS 33). Lancet. 1998;352:837-853. 5. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet. 1998;352:854-865. Supplemental Readings: 6. Rothman R, Malone R, Bryant B et al. A randomized trial of a primary care-based disease management program to improve cardiovascular risk factors and glycated hemoglobin levels in patients with diabetes. American Journal of Medicine. 2005;118:276-284. 7. Rothman R, DeWalt D, Malone R et al. Influence of Patient Literacy on the Effectiveness of a Primary Care-Based Diabetes Disease Management Program. JAMA. 2004;292:1711-1716. 8. Rothman R, Malone R, Bryant B et al. The Spoken Knowledge in Low Literacy in Diabetes Scale: A Diabetes Knowledge Scale for Vulnerable Patients. Diabetes Educator. 2005;31(2)215-224. 9. Rothman R, et al. Pharmacist-led, primary care-based disease management improves hemoglobin A1c in high-risk patients with diabetes. Am J Med Qual. 2003 Mar-Apr;18(2):51-8. 10. Clark PM, Gray AM, Briggs A, et al. Cost-utility analyses of intensive blood glucose and tight blood pressure control in type 2 diabetes (UKPDS 72). Diabetologia. 2005;48:868-877. Pain: 1. Holdcroft A, Power I. Management of Pain: Recent Developments. BMJ. 2003;326:635-639. 2. Ballantyne J, Mao J. Opioid Therapy for Chronic Pain. NEJM. 2003;349:19431953. 3. Strasser F, Driver L, Burton A. Update on Adjuvant Medications for Chronic Nonmalignant Pain. Pain Practice. 2003;3(4):282-297. 83 84 4. Hammett-Stabler C, Pesce A, Cannon D. Urine Drug Screening in the Medical Setting. Clinica Chimica Acta. 2002;315:125-135. 5. Goldenberg D, Burckhardt C, Crofford L. Management of Fibromyalgia Syndrome. JAMA. 2004;292:2388-2395. Supplemental Readings: 11. Chelminski, P. R.; Ives, T. J.; Felix, K. M.; Prakken, S. D.; Miller, T. M.; Perhac, J. S.; Malone, R. M.; Bryant, M. E.; DeWalt, D. A., and Pignone, M. P. A primary care, multi-disciplinary disease management program for opioidtreated patients with chronic non-cancer pain and a high burden of psychiatric comorbidity. BMC Health Serv Res. 2005 Jan 13; 5(1):3. 12. Gardner-Nix J. Principles of opioid use in chronic noncancer pain. CMAJ. 2003;169(1):38-43. 8. Moulin, D. E.; lezzi, A.; Amireh, R.; Sharpe, W. K.; Boyd, D., and Merskey, H. Randomised trial of oral morphine for chronic non-cancer pain. Lancet. 1996; 347(8995):143-7. Assessment and Feedback Self Assessment: A verbal self-assessment will be completed by all preceptors at the end of the fourth week of the rotation. A written self-assessment will be completed the last week of the rotation and reviewed/discussed with the learner upon completion of the rotation. You are welcome at any time to request an informal evaluation of your progress. Preceptor Assessment: A written assessment of the disease management elective should be completed at the end of the rotation. Formative verbal assessment is appreciated throughout the month. 84 85 SECTION 4 TEACHING CURRICULUM Interns’ Conference Ambulatory Care Conference Internal Medicine Update Conference Board Review Occupational and Environmental Diseases Bioethics and the Legal Principles of Medicine Physician Impairment Laboratory Medicine Medical Informatics Evaluation Violence Gender-Specific Health Care Palliation Care & Pain Management 85 86 Section 4 Teaching Curriculum General The Department of Medicine has daily teaching conferences that supplement teaching done on individual rotations. As previously mentioned in Section 1, these conferences are held at times that do not conflict with the activities of the respective services. The formats of these conferences have also been described in Section 1. Content is planned so that each resident is exposed to the breath of information necessary to become a well-trained general internist. Specific curricula are also incorporated into these conferences. These curricula are described in this section. 86 87 INTERNS’ CONFERENCE All PGY-1 residents are excused from clinical dates each Wednesday from noon to 1:00 pm. At the beginning of the academic year, each conference is led by a member of the faculty who discusses a topic pertinent to PGY-1 management of patients. Topics included are outlines below. Following this series of conferences, the format for this conference changes to case-based teaching of 1-2 topics per session. This format continues throughout the year. Topics for Conferences EMERGENCIES Anaphylaxis / PE Hematology/Oncology Emergency SVC Syndrome Tumor Lysis Hypercalcemia Cord Compression Pneumothorax / Aortic Dissection CARDIOLOGY Hypertension Atrial Fibrillation Myocardial Infarction Congestive Heart Failure EKG Interpretation NEUROLOGY Seizures CVA Altered Mental Status PULMONOLOGY Chronic Obstructive Pulmonary Disease Lung Cancer Asthma Pneumonia NEPHROLOGY Acute Renal Failure Chronic Renal Failure ENDOCRINOLOGY Thyroid Disease Adrenal Disease DIGESTIVE DISEASES PUD Pancreatitis Liver Failure / ETOH Liver Disease Hepatitis Diarrhea HEMATOLOGY/ONCOLOGY Anemia Breast Cancer Prostate Cancer Colon Cancer RHEUMATOLOGY Rheumatoid Arthritis/Osteoarthritis Lupus Sarcoidosis INTRO TO EVIDENCE BASED MEDICINE INFECTIOUS DISEASES Human Immunodeficiency Virus Tuberculosis Meningitis 87 88 AMBULATORY CARE CONFERENCE This conference occurs each Friday from noon to 1 pm and is attended by PGY-1, -2, and -3 residents. Each conference is led by a PGY-2 or PGY-3 resident. The resident researches the topic, presents a key article, and critically appraises the article and the literature. The focus of this conference is evidence-based medicine. Topics for Conference HEENT Sinusitis/Rhinitis/Otitis/Laryngitis Hearing Loss Pharyngitis Blinding Eye Diseases Respiratory Cough/Bronchitis Pulmonary Nodule Outpatient Management of Asthma Cardiovascular Evaluation and Treatment of Hypertension Testing strategies for Suspected Coronary Artery Disease Peripheral Vascular Disease (arterial) Chronic Venous Disorders Carotid Bruits and TIA’s GI Irritable Bowel Syndrome Diverticular Disease Dyspepsia Constipation Diarrhea Avitaminoses Endocrine Outpatient Management of Type I DM Outpatient Management of Type II DM Osteoporosis Goiter and Thyroid Nodules Hyper- and Hypothyroidism Musculoskeletal Low Back Pain Common Foot Problems in Primary Care Evaluation of Musculoskeletal Complaints -1- Neck and UE -2- Hip and LE Gout/CPPD Gynecologic/Genitourinary Prescribing Oral Contraceptives 88 89 Menopause/Hormone Replacement Therapy STD’s/Vaginitis/ Safe Sex Counseling Pelvis Inflammatory Disease Sexual Dysfunction BPH/Prostatitis UTI/Asymptomatic Bacteriuria Nephrolothiasis Dysfunctional Uterine Bleeding Hematurias/Proteinuria Incontinence Neurologic Dizziness Syncope Headache Peripheral Neuropathy Psychiatric Anxiety/Panic Disorder Management of Chronic Benzodiazepine Use Narcotic Addiction/Narcotic-seeking Behavior Recognition of Abuse in the outpatient setting (Domestic violence/Incest/Rape) Depression in Primary Care Insomnia Recognition of Personality Disorders in the Outpatient Screening Dermatology Outpatient Dermatology Screening/Prevention Smoking: Counseling and Cessation Tuberculosis Screening and Prophylaxis Immunizations and Post-Exposure Prophylaxis General Principles of Screening and Prevention Care Cholesterol Screening Breast Cancer Screening Cervical Cancer Screening Traveler’s Recommendations Colorectal Cancer Screening Prophylaxis for Procedures Miscellaneous Outpatient Management of HIV infection Preoperative Medical Evaluation in the clinic setting 89 90 INTERNAL MEDICINE UPDATE CONFERENCE This conference occurs each Monday from noon to 1 pm. A series of topics is selected, each one reviewed by a faculty member of the Department of Medicine. The subjects are chosen based upon resident performance on the ACP sponsored In-Training Examination. All residents attend this conference. The following subjects are reviewed in this conference. CARDIOLOGY MI diagnosis MI Management Arrhythmias Diagnostic Testing EKG & Physical Exam CHF Management Chest pain evaluation HTN etiology HTN Management Endocarditis diagnosis Endocarditis Management CAD interventions ICU Aortic Aneurysm Shock Respiratory Failure ARDS Pulmonary Embolism Pneumonias Ionotropic Meds DKA Overdoses NEPHROLOGY Hyponatremia Acidosis Alkalosis Electrolytes Urine Electrolytes Hypernatremic Hematuria/Proteinuria Lupus/Vasculitis Transplants Urinalysis Dialysis / ARF DIGESTIVE DISEASE Nutrition Upper GI bleed Lower GI bleed Liver Failure Pancreatitis Diarrhea Cholecystitis/Cholangitis Diverticulitis Inflammatory Bowel Disease Peptic Ulcer Disease Cirrhosis HEMATOLOGY Sickle cell disease DIC Coagulopathies Hemolysis Anemia Thrombocytopenia Anticoagulation - How to INFECTIOUS DISEASES Meningitis HIV 1 - Opportunistic Infect. HIV 2 - Anti retroviral Hepatitis Antibiotics I Antibiotics II Fever of unknown origin Sepsis Urinary Tract Infections Rare infections PULMONARY Asthma Pulmonary nodule Tuberculosis Interstitial lung disease Pleural effusions Pulmonary Function Tests GENERAL MEDICINE Venous stasis ulcer Depression Stroke Back pain Dementia Neuropathy Screening Occupational Health & Exposure Occupational Health - Toxins ONCOLOGY Lung Cancer I Lung Cancer II Leukemia I Leukemia II Hem/Onc emergencies Lymphoma Breast cancer Colon cancer Prostate cancer Myelophthystic disorders Multiple myeloma Bone marrow transplantation ETHICS DNR Apache Score/ Prognosis Legal RHEUMATOLOGY Crystal disease Inflammatory arthritis Autoimmune 90 91 INTERNAL MEDICINE BOARD REVIEW At the conclusion of each academic year, a review of Internal Medicine is given to prepare PGY-3 residents for the certification examination in Internal Medicine. The core of this review is a series of lectures given by faculty members. All PGY-3 residents are excused from clinical duties to attend. The goal of each lecture is to give a broad overview of the subjects. Each lecture has an accompanying handout. These are collected so that each participant receives a syllabus for the course. OCCUPATIONAL AND ENVIRONMENTAL DISEASES Internists must always consider that certain symptoms and disease processes are related to exposures in the occupational setting or particular environmental settings. At the completion of training, residents should have a working knowledge and sufficient patient experience to satisfy the following goals: Incorporate in a history occupational and environmental exposures. Identify physical and laboratory findings suggestive of occupational/environmental exposure alopecia, wheezing, hearing loss, chest x-ray abnormalities of silicosis, asbestosis, CO poisoning, lead exposure. Understand appropriate reporting to monitoring agencies Know the procedure and how to assess disability Know how to counsel patients about exposure risks The information necessary to meet these goals is the subject of several teaching conferences. It is also part of the Curriculum of the Pulmonary service as well as Allergy Clinic, and part of Rheumatology rotation. 91 92 BIOETHICS AND THE LEGAL PRINCIPLES OF MEDICINE On a day-to-day basis, residents face ethical issues. Residents must gain expertise in the following subjects and be familiar with their societal and legal boundaries. Understand living wills and power of attorney and incorporate this into a history Be able to define criteria for withdrawal of support Be able to counsel a patient when the patient refuses treatment or is ambivalent about treatment. Understand the legal aspects of confidentiality Understand what constitutes malpractice and steps to prevent litigation. Develop expertise with the dying patient and family. Understand the role of hospice and be familiar with referral criteria Be familiar with surrogate decision-making and permission for treatment. Understand the legal aspects of “Do not resuscitate” orders. Understand the legal aspects of confidentiality of medical records. These subjects are reviewed in several teaching conferences in the Department of Medicine. Some of these issues are part of the curriculum in the ICU and the general medicine inpatient service. Finally, at least three Grand Rounds per year are devoted to these subjects. 92 93 PHYSICIAN IMPAIRMENT A significant number of physicians are impaired by alcohol, chemical dependency, and/or psychiatric dysfunction. The recognition of such physicians, how they can be referred for help, and their outcome should be appreciated by residents. Specifically, the following aspects of physician impairment should be part of the knowledge base in internal medicine. What constitutes physician impairment and how to identify it. What is appropriate treatment for impaired physicians? Recognition of the disease of addiction. The utility of a contract for an impaired physician. This subject and its components will be reviewed in a series of ’ conferences conducted by members of the North Carolina Physicians Health Program, a group of experts in the field of physician impairment. Educational reading materials will be provided at the conferences. 93 94 LABORATORY MEDICINE As part of a diagnostic evaluation, internists often order and subsequently interpret a variety of laboratory tests. Internists should demonstrate competency in these areas for the tests listed. This information is reviewed in the subspecialty and general medicine curricula. Allergy and Immunology - levels of complement, C1 esterase, eosinophil count Cardiology - cardiac enzymes, nuclear heart scan Dermatology - Tzanck smear, microscopic exam for scabies Endocrinology - bone mineral densitometry, serum glucose, gylcosylated hemoglobin, serum gonadotropins, serum lipids, serum prolactin, thyroid function tests, thyroid scanning, urine metanephrines, serum calcium, serum phosphate Gastroenterology - assays for H. pylori, serum tests for liver diseases, colonoscopy, stool for O&P, ercp, fecal electrolytes and osmolality, gall bladder scan, serum gastrin, viral hepatitis serology, liver biopsy, stool fat, endoscopy Hematology - bone marrow aspirate and biopsy, cytogenetics, clotting assays, iron studies, lymph node biopsy, electrophoresis, B12 levels Infectious Disease - CD4 counts, csf analysis, ELISA, PCR, serology for common infections, syphilis serology Nephrology - 24-hour urine electrolytes, fractional excretion of sodium, creatinine clearance, renal biopsy, serology for glomerulornephritis, renal angiography Neurology - anticonvulsant drug levels, carotid Dopplers, imaging of CNS, sleep study Oncology - cytology, estrogen/progesterone receptors, serologic tumor markers Pulmonary - bronchoscopy, pleural fluid analysis, and lung scans Rheumatology - antinuclear antibodies, ESR, complement levels, rheumatoid factor, synovial analysis for crystals. 94 95 MEDICAL INFORMATICS The extent of medical information, both educational as well as related to patient care, is vast. Organization of this information is critical for an internist to function effectively. To this end, an internist must have certain knowledge of computer systems to design an information system that is reliable and accessible. The following curricular goals should be achieved. Be able to use basic word processing Be able to use CD-ROM’s and the Internet for education and literature searching Be able to use computer systems for patient care Know essential aspects of information storage. To emphasize these goals, each resident attends a course to develop skills in using the clinical workstations at the UNC Hospitals. Furthermore, there are instructional conferences on CD-ROM for educational use. 95 96 Violence An internist must be able to recognize signs and symptoms of abuse as well as know how to manage or refer patients who are victims of abuse. The following objectives will be addressed in didactic sessions. 1. to learn the signs and symptoms of domestic abuse 2. to learn the signs and symptoms of sexual abuse 3. to learn the signs and symptoms of elder abuse 4. to learn about the hospital & community resources to deal with these problems 5. to learn the legal issues involved in abuse These subjects are discussed at the departmental level, usually at Grand Rounds, by experts in abuse. These experts work under the Beacon Program at the UNC Hospitals, which includes faculty members from the Department of Medicine, the Department of Social Services, & the Legal Department. Gender-Specific Health Care 96 97 Women’s Health The general internist will be called upon to perform health maintenance, recognize and treat common disorders, and refer appropriately for complex diseases of women. In preparation for these functions, the following objectives should be met in the residency: 1. be able to perform bimanual pelvis examination, including preparing pap smears 2. be able to perform a breast examination and instruct patients in self-examination 3. know health maintenance guidelines for these examination (1, 2) 4. be able to prescribe common contraceptives 5. understand the evaluation of galactorrhea 6. be able to diagnose and treat common STD’s-syphillis, gonorrhea, herpes 7. be familiar with rape protocol 8. understand the presenting signs of sexual abuse 9. be familiar with the evaluation of pelvic pain 10. know the physical signs of cystocele, rectocele, uterine prolapse 11. be familiar with the presenting signs of pregnancy 12. be able to prescribe and understand the risks and benefits of hormone replacement Physical examination skills for these objectives will be met in the continuity clinic, urgent care, general medical rotations, as well as the Emergency Room. Didactics on these subjects are covered in these different rotations as well as in Department conferences including Grand Rounds, ACC conferences, update conferences, and resident’s report. 97 98 Men’s Health The general internist also will be involved in health maintenance, referral, diagnosing and treating disorders specific to men. The following objectives should be met: 1. be able to perform a genital examination, including examination of the prostate. 2. know the health maintenance guidelines for the genital examination, including PSA screening 3. recognize presenting symptoms of prostate cancer 4. be able to diagnose and treat prostatitis 5. be able to diagnose and treat common STD’s-syphillis, gonorrhea, and herpes 6. be familiar with the evaluation of impotence 7. be able to recognize and diagnose common hernias 8. be able to recognize and treat epididymitis 9. be familiar with the evaluation of a testicular mass 10. understand the pathophysiology of gynecomastia The appropriate skills and didatics will be covered in the same manner as described for women’s health issues. Palliative Care and Pain Management 98 99 A number of diseases that the general internist faces have no effective treatment. For these diseases once a diagnosis is made, the internist may have to focus all efforts on palliation and terminal care. The following objectives should be met to prepare residents for these patient care situations: 1. to develop an understanding of palliation care as perceived by the patient & family 2. to learn the role of the health care team in the delivery of palliation care 3. to learn the role of the hospice in the care of terminally ill patients 4. to learn the principles of symptoms management including pain, nausea, vomiting, & dyspnea 5. to understand about the financial aspects of palliation care, particularly in the home These subjects will be covered in a series of lectures by expert faculty. Dr. Stephen Bernard, Division of Hematology/Oncology, will give several of these. He has specific training & conducts an elective course in the School of Medicine in palliation care. Members of the Department of Anesthesiology who serve on the pain consultation service will also participate. Regarding specific experience, the Geriatrics rotation includes time at a hospice. 99 100 SECTION 5 EVALUATION Resident performance must be evaluated on every rotation. The categories of evaluation as defined by the Residency Review Committee (RRC) for Internal Medicine are as follows: 1. 2. 3. 4. 5. 6. Patient Care Medical Knowledge Practice-Based Learning and Improvement Interpersonal and Communication Skills Professionalism Systems-based Learning The resident evaluation form asks faculty to evaluate residents in each of the competencies. A copy is enclosed. The competencies have been reviewed with the Attendings in departmental conferences. Separate evaluation forms have been developed for Continuity Clinic and Same-day clinic. The form will be filled out by the clinic preceptor for each clinic session for residents and the data will be aggregated twice a year by the director of the clinic. Copies of the forms are included. All residents are required to complete a clinical evaluation exercise in the first 6 months of the PGY 1 year. A copy of this form is included. All residents are evaluated semi- annually by the Program Director. At the end of each year a global evaluation is submitted to the American Board of Internal Medicine. It is reviewed with the resident and a copy is provided for each resident. Residents are asked to evaluate the faculty on each rotation and to evaluate the curriculum annually. Faculty are also asked to evaluate the curriculum Copies of these forms are provided. 100 101 Procedure Competency The American Board of Internal Medicine requires that residents perform safely and competently the following procedures: 1. 2. 3. 4. 5. ACLS Drawing venous blood Drawing arterial blood Pap smear and endocervical culture Placing a peripheral venous line For other procedures the Board requires that residents know the indications, contraindications, management of complications, and interpretation of results. Performing these procedures is not required for Board certification. These include: 1. 2. 3. 4. 5. 6. 7. 8. 9. Paracentesis Arterial line placement Arthrocentesis Central venous line placement Incision and drainage of an abscess Lumbar puncture Nasogastric intubation Pulmonary artery catheter placement Thoracentesis The Department of Medicine has responded to this initiative by developing a comprehensive procedure curriculum. This is given to all PGY 1 residents. First residents are required to watch videos and read selected articles about the procedures. The next step is a half-day workshop in our simulation lab where residents practice central venous line placement, peripheral venous line placement, and lumbar puncture. Clinical instructors are present for each procedure. A post –workshop is given to each resident. All residents are given a procedure log to use throughout the residency to record all procedures done. The information includes any complications and the supervisor for the procedure. The log becomes part of the resident’s permanent folder. 101 102 102 103 103 104 Curriculum Evaluation 2008 PGY 1 ___ Scale: PGY 2 ___ Strongly Agree 1 Agree 2 PGY 3 ___ Neutral 3 (Please designate your year.) Disagree 4 Strongly Disagree 5 1. Grand Rounds topics were clinically relevant and contributed to my knowledge base. 2. CPC’s presented a wide array of diseased processes and contributed to my knowledge base. _____ 3. Noon Conferences were clinically relevant and contributed to my knowledge base. _____ 4. Teaching conferences placed an appropriate emphasis on Evidence-Based Medicine _____ 5. Teaching conferences placed too much emphasis on Evidence-Based medicine. _____ 6. The In-Training Examination adequately assessed my fund of information. _____ 7. Residents Report presentation’s contributed to my knowledge base. _____ 8. The case-based format of Residents Report was an effective learning environment. _____ 9. The housestaff website was an effective tool for literature searching. _____ 10. My schedule allowed me adequate time to read. _____ _____ Please feel free to add individual comments: 104 105 Curriculum Evaluation 2008 Instructor/Assistant Prof ___ Associate/Full Professor ___ Scale: Strongly Agree 1 Agree 2 Neutral 3 Division ___ ________ Disagree 4 Strongly Disagree 5 1.Grand Rounds topics were clinically relevant and contributed to my knowledge base. _____ 2.Morbidity/Mortality conferences were clinically relevant and contributed to my knowledge base. _____ 3.Textbooks are a main source of reference to prepare resident lectures _____ 4.Journal articles are a main source of reference to prepare resident lectures _____ 5.Electronic references are a main source to prepare resident lectures _____ 6.When I am attending, I hold teaching rounds at least 3 times a week _____ 7.When I am attending, I do bedside teaching at least 3 times a week _____ 8.The current call schedule for residents facilitates teaching _____ 9.The electronic record facilitates teaching _____ 10.The Department values my teaching efforts _____ Please feel free to add individual comments: 105 106 106 107 107 108 108