Irritable Bowel Syndrome - University of Colorado Hospital
advertisement

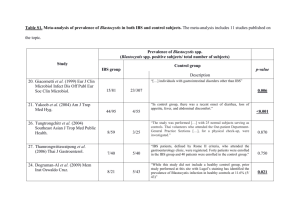
Irritable Bowel Syndrome Stephen R. Freeman, M.D. Associate Professor of Medicine University of Colorado Denver Health Sciences Center Department of Medicine- Gastroenterology Anschutz Outpatient Pavilion Irritable Bowel Syndrome (IBS) is a very common condition affecting people worldwide and is manifest, and indeed, defined by, symptoms of abdominal pain and discomfort, and altered bowel habits and stool form. It is primarily a condition affecting young adults, but also affecting children, and women more so than men. The acronym IBS should not be confused with another common, but more serious digestive disease, IBD or inflammatory bowel disease, a disease associated with an inflammation of the colon or small intestine. IBS is characterized as constipation predominant, diarrhea predominant and mixed types. IBS is one of many human conditions defined by symptoms and the absence of “alarm” symptoms or signs, and these are outlined in a widely agreed upon and scientifically validated set of criteria known as the Rome criteria*. IBS diagnostic criteria are: Recurrent abdominal pain or discomfort at least 3 days/month in the last 3 months associated with two or more of the following: 1. Improvement with defecation 2. Onset associated with a change in frequency of stool 3. Onset associated with a change in form (appearance) of stool These criterions have to be met within the past 3 months and have to have had the onset of symptoms at least 6 months prior to the diagnosis. “Alarm” symptoms or signs are potentially more worrisome problems that might imply a more serious underlying diagnosis, and therefore might mean more testing should be done to look into these symptoms. Examples of such “alarm” symptoms or signs are: 1. Onset at older age > 60 yrs 2. More severe diarrhea: > 6 bowel movements/ day 3. Rectal bleeding 4. Unintentional weight loss 5. Iron deficiency anemia 6. Family history (1st degree relative) of colon or ovarian cancer 7. Family history of celiac disease 8. Nocturnal symptoms 9. Abdominal or rectal mass *The Rome criteria were developed to try to identify similar patients for purposes of clinical research, but have been helpful to physicians in making the correct diagnosis of IBS and in the appropriate treatment of these patients. Page 1 of 5 Created by The Women’s Integrated Services in Health Program Content written by Dr. Stephen Freeman MD /10/2011 The cause of IBS is not known but it appears to be a motility disorder associated with neurologic or muscular hypersensitivity of the colon. This hypersensitivity is also referred to as visceral hyperalgesia and is felt to be usual or normal events occurring in the usual function of the colon causing pain and dysfunction in certain individuals. Other stimuli applied to other parts of the body may also be associated with a heightened pain response in these individuals. An area of controversy exists regarding the role of bacteria in causing IBS symptoms. There is some medical evidence supporting the theory that overgrowth of intestinal bacteria in the small bowel may cause some symptoms of abdominal discomfort and bowel irregularity, and might respond to antibiotic treatment. The methods of testing for this are inaccurate and often misleading, and the treatment is at best temporary, and will alter bacteria in the colon also which also often will give temporary benefit. A risk factor for developing IBS includes having an acute gastrointestinal infection such as “traveler’s diarrhea” or viral gastroenteritis. Other possible risk factors are aerophagia (air swallowing) associated with reflux or postnasal drainage and antibiotic use for non-gastrointestinal conditions. In addition, there are a number of potentially modifiable childhood conditions that seem to be risk factors for IBS continuing or developing in adult patients. There are no associated risks for developing IBS from other factors known to be a risk for other serious health problems, specifically smoking, alcohol use, and coffee. There are also several conditions affecting adult patients that are associated with IBS including fibromyalgia, anxiety and depression, migraine headaches, sleep disorders and a variety of other physical diseases such as asthma, recurrent urinary tract infections, diverticulosis, and previous surgeries like hysterectomy and cholecystectomy. Diagnosis of IBS is based on compatible symptoms and absence of “alarm” symptoms or signs. It is common and usually necessary for some basic testing to be done, mostly blood tests, occasionally other tests like x-rays or, sometimes, endoscopic tests. For the most part, a patient with these symptoms and normal basic tests do not have to undergo a large number of tests to be accurately diagnosed. Of course, there are patients with atypical or more severe symptoms who require more extensive testing before the diagnosis is made. One of the most important diseases to consider in patients felt to have IBS is celiac sprue, as symptoms of both conditions can frequently overlap, and there is a very specific treatment for celiac disease, namely a gluten free diet. This same treatment is not usually necessary in IBS, although may, at times, be helpful. Treatment of Irritable Bowel Syndrome is aimed at the particular symptoms a patient has and there is no one treatment for this condition. What helps one person may not help the next person. Treatment is often by “trial and error”. While there is no cure for IBS, this condition does tend to wax and wane over time and may seem to recede and not bother the person for sometimes long periods of time. Whereas IBS tends to first make its appearance in young people from children to young adults, it may continue to affect susceptible patients well into their middle or older age years. It is quite uncommon for this condition to have its onset after the age of 50 – 60, and symptoms compatible with IBS beginning in these years clearly deserves to be diagnosed with more caution and more testing done to look for other more serious diseases. Page 2 of 5 Created by The Women’s Integrated Services in Health Program Content written by Dr. Stephen Freeman MD /10/2011 Fiber bulking agents are commonly used to improve bowel irregularity problems. They generally tend to be helpful for both diarrhea and constipation types of IBS, but are more useful in the constipation-predominant type. Dietary fiber like wheat bran is an example of insoluble fiber, and a fiber supplement such as psyllium husk is an example of a soluble fiber. Generally speaking the soluble fibers are more helpful in relieving the global symptoms of IBS and the insoluble fibers are better for the treatment of IBS-related constipation. The soluble fibers are sometimes better tolerated than the insoluble varieties, as the latter may be more subject to bacterial action and production of gas within the colon which can contribute to IBS-related abdominal discomfort. Dietary Suggestions for IBS o o o o o o o o o o o o o o Eat regularly and take time to eat Drink 8 or more cups of fluid daily, especially water or other non-caffeinated drinks Limit tea and coffee to 3 or fewer cups daily Reduce consumption of alcoholic and carbonated beverages Limit high-fiber foods such as whole grain breads, cereals high in bran, and whole grains such as brown rice Reduce consumption of ‘resistant starch’ (starch that resists digestion in the small intestine and reaches the colon intact such as wheat and wheat-containing products), which is often found in processed or re-cooked foods Limit fresh fruit intake to less than 240 g daily People with gas and bloating may find it helpful to incorporate oats and linseeds (up to 1 tablespoon per day) in their diet People with diarrhea should avoid sorbitol Keep food diary to determine how food affects symptoms Avoid large meals Reduce fat to no more than 40-50 g daily Avoid foods which may increase gas, such as legumes and cruciferous vegetables Reduce fermentable oligo-, di- and monosaccharide’s and polyols Physical exercise or increased physical activity has been associated with decreased IBS symptom severity. Counseling may be helpful in certain patients with IBS. Cognitive behavioral therapy, hypnotherapy, and/or psychological therapy are a consideration for patients who do not respond to dietary and pharmacological treatments after 12 months and have continuing debilitating symptoms. This generally involves a small minority of IBS patients. Pharmacologic therapies are also available and consist if a few different categories of medications with varying degrees of effectiveness. For constipation, several laxatives that are helpful include the bulking agents, as well as ones that promote stool hydration such as docusate sodium, PEG electrolyte solution, and other osmotic laxatives which are available over the counter. Most of these are most effective if used daily for a period of time rather than sporadically. Page 3 of 5 Created by The Women’s Integrated Services in Health Program Content written by Dr. Stephen Freeman MD /10/2011 Anti-diarrheal medications for diarrhea-predominant IBS are safe to use as needed, including loperamide and kaopectate. Prescription medications are also effective such as diphenoxalate – atropine and alosetron. For pain control, avoidance of potentially addictive narcotic analgesics is generally advisable. Anti-depressants are quite useful as pain modulators as well as treatment for any associated depression or anxiety. These can be tricyclic antidepressants (TCAs) such as nortriptyline or some of the newer serotonin re-uptake inhibitors (SSRIs) such as Paxil and Zoloft. Pain from smooth muscle spasm may respond to anti-spasmodics such as hyoscyamine or dicyclomine. Another medication that may be helpful for spasm is peppermint oil, such as in an Altoid mint. Antibiotics can be used to treat small bowel bacterial overgrowth, and generally can be temporarily effective for abdominal discomfort or bloating, and possibly even constipation. These effects are temporary, but can last for a few weeks following stopping the antibiotic. Most antibiotics used for this purpose are ones which are nonabsorbable such as rifaxamin or neomycin. The risk of antibiotics is the creation of gut organisms which become resistant to these antibiotics, or which allow the overgrowth of harmful bacteria and allow the development of serious infectious colitis such as Clostridia difficile colitis. Probiotics are the pharmacologic use of nonharmful, and potentially useful bacterial organisms to try to repopulate the gut with flora that might be helpful in eliminating noxious symptoms such as constipation, diarrhea, bloating and other abdominal discomfort. There are many small studies which show some benefit from this treatment, but, unfortunately, the weight of the evidence shows that probiotics are not any better than placebo in treating IBS symptoms. The good news is that placebo has always, in many trials of various treatments for IBS symptoms, been a very good treatment with surprisingly high response rates. This phenomenon has made proving efficacy of many IBS drug treatments difficult when appropriately compared to the placebo response. One other aspect of treatment of IBS symptoms that has been found to be effective is a good provider – patient relationship. Having a comfort level and confidence in your provider has been proven to be quite helpful in the successful management of even difficult patients with IBS. Irritable bowel syndrome is a common condition affecting millions of people worldwide of all ages and sexes. It is not a life threatening condition but does cause pain and discomfort, and can be costly in terms of loss of time and productivity from usual activities, and significant medical costs. At times, the symptoms can also cause alterations in usual lifestyle preferences. It is a complex condition, not yet well understood, but clearly involves a relationship between the central and gut neuromuscular systems and interaction between our environment and our bodies. This interaction is multifactorial including diet, medications, other medical conditions, and, importantly, internalized and external stress factors. Management is directed toward symptom control through a variety of means, many of which are imperfect and give incomplete results. Insight into the nature of the problem and its causes and treatments and setting appropriate expectations is an important factor in helping a person cope with this condition. Page 4 of 5 Created by The Women’s Integrated Services in Health Program Content written by Dr. Stephen Freeman MD /10/2011 Guidelines 1. 2. 3. 4. NICE 2008 Feb:CG61 PDF National Guideline Clearinghouse 2009 May 4:13703 BMJ 2008 Mar 8;336(7643):556 Am J Gastroenterol 2009 Jan;104 (Suppl 1):S1 Reviews 1. 2. 3. 4. 5. J Fam Pract 2008 Feb;57(2):100 N Engl J Med 2008 Apr 17;358(16):1692 Altern Ther Health Med 2004 May-Jun;10(3):22 BMJ 2005 Mar 19;330(7492):632 full-text N Engl J Med 2003 Nov 27;349(22):2136 About the Doctor Stephen R. Freeman, M.D. Associate Professor of Medicine University of Colorado Denver Health Sciences Center Department of Medicine- Gastroenterology Anschutz Outpatient Pavilion Dr. Freeman received his medical degree from the University of Arkansas, Medical Sciences College of Medicine. He completed his internship and residency with the Tripler Army Medical Center program. Dr Freeman is dual board certified in Internal Medicine and Internal Medicine-Gastroenterology. He see’s patients at the University of Colorado Hospital. Dr Freeman’s clinical interests include Gastrointestinal Motility disorders, Gastroesophageal Reflux and other Peptic diseases. He is an expert in Inflammatory Bowel Disease and Colorectal Cancer. For more information about The Women’s Integrated Services in Health (WISH) Call 720-848-9474 or go to www.wishforwomen.org Your WISH team can help make a referral to the Gastroenterology Services at the University of Colorado Hospital For more information about The Services for Colorectal Screening and the Gastroenterology team at the University of Colorado Hospital visit our website. Call 720-848-2777 to schedule an appointment. Page 5 of 5 Created by The Women’s Integrated Services in Health Program Content written by Dr. Stephen Freeman MD /10/2011