Curriculum Vitae
advertisement

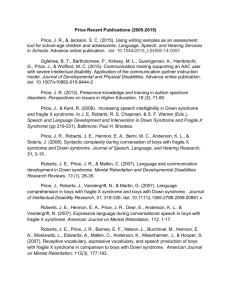
WIMM PI Curriculum Vitae Personal Data Name Nationality Email Irene Roberts UK pending Present Position 2013-present Honorary Consultant in Paediatric Haematology (Oxford Trust) 2013-present Professor of Paediatric Haematology, (University of Oxford) Previous Positions 1978 House Physician to Professor E.M. McGirr, Glasgow Royal Infirmary. 1979 House Surgeon to Mr D.H. Clark, Gartnavel General Hospital, Glasgow. 1979 SHO Obstetrics to Professor C. Whitfield, Queen Mother's Hospital, Glasgow. 1980 SHO Paediatrics to Professor F. Cockburn, Royal Hospital for Sick Children, Glasgow. 1981 SHO/Registrar in Medicine to Dr R. Walker, Law Hospital, Lanarkshire. 1981 Registrar in Haematology to Dr R.L.C. Cumming, Stobhill Hospital, Glasgow. 1983 Research Fellow, Department of Pharmacology and Medicine, Vanderbilt University, Nashville, Tennessee with Dr GA FitzGerald; MD (Hons) University of Glasgow. 1985 Lecturer in Haematology to Professor N.H. Russell, University of Nottingham. Honorary Senior Registrar in Haematology, City Hospital, Nottingham. 1988 Senior Research Fellow with Professor Lucio Luzzatto, Department of Haematology, Royal Postgraduate Medical School, London. 1990 Senior Lecturer in Paediatric Haematology, Royal Postgraduate Medical School. Honorary Consultant Paediatric Haematologist, Hammersmith Hospital, London. 2000 Professor of Paediatric Haematology, Royal Postgraduate Medical School (now Imperial College London). Honorary Consultant Paediatric Haematologist Hammersmith and St Mary's Hospitals (now Imperial College Healthcare NHS Trust), London. Research Achievements Over the last 20 years, we have investigated the biological basis of the high frequency of haematological disorders which affect newborn infants. Through clinical and laboratory studies to properly define their natural history and haematopoietic defects, we found that most disorders originate in fetal life and are the consequence of perturbation of fetal haematopoiesis, for example due to chronic hypoxia or antibody-mediated suppression of progenitor development, rather than secondary to acquired post-natal events. We therefore established a programme to characterise normal human fetal haematopoiesis and, from a clinical point of view, to develop aetiology-based classifications of neonatal thrombocytopenia and anaemia which simplify diagnosis/management and are now in widespread use. In the last 5 years we have specifically focused on the cellular and molecular basis for trisomy 21-mediated perturbation of fetal haematopoiesis and the impact of trisomy 21 on leukaemia initiation. Through immunophenotypic, functional and gene expression studies on isolated primary fetal haematopoietic stem/progenitor cells we have shown that trisomy 21 itself causes abnormal development of fetal haematopoietic progenitors and, more recently, that trisomy 21 interferes with fetal haematopoietic stem cell function, causing a marked megakaryocyte/erythroid bias and profound impairment of B lymphocyte development. On a clinical level the importance of trisomy-21-mediated perturbation of fetal haematopoiesis lies with the recognised markedly increased risk of acute leukaemia in children with Down syndrome (trisomy 21). To investigate the pathogenesis of trisomy 21-associated acute myeloid leukaemia (AML), in collaboration with Paresh Vyas' lab (WIMM), we established a prospective Down syndrome neonatal cohort study to define the natural history at the clinical, haematological and molecular level. This recently found that acquired N-terminal truncating mutations in GATA1 occur at very high frequency (~30%) in neonates with Down syndrome. Multilineage haematopoietic abnormalities are present in all Down syndrome neonates, further implicating trisomy 21 in driving abnormal haematopoiesis. What are the Future Aims of Your Current Group? We now want to identify the molecular mechanisms which explain how the presence of 3 copies of chromosome 21 produces specific defects in fetal haematopoietic stem/progenitor cells and, ultimately, how this contributes to leukaemogenesis in children with Down syndrome. We will continue to work on primary human fetal cells as no mouse models or ES/iPS models fully recapitulate the human disease. As a starting point, we will attempt to identify consistent differences in the gene expression patterns in highly purified haematopoietic stem and progenitor populations from normal and trisomy 21 fetal liver. Initially we expect to focus on differences where expression of chromosome 21 genes is likely to be implicated. Overexpression and knockdown studies in primary cells will be used to test the functional significance of these changes. The role of the trisomy 21 microenvironment will be investigated directly (through gene expression of trisomic and disomic fetal liver stromal cells) and indirectly by investigating the effects of trisomy 21 on primary human fetal bone marrow haematopoietic stem and progenitor cells using similar approaches to our previous work in fetal liver. These studies will also be used to investigate the molecular basis of increased susceptibility of children with Down syndrome to B lineage acute lymphoblastic leukaemia and immune deficiency. In collaboration with Paresh Vyas' lab, data and samples from the Down Syndrome Neonatal Cohort Study will be used to identify the clinical, haematological and molecular characteristics that predict transformation of the neonatal preleukaemic condition TAM, to overt acute myeloid leukaemia. As part of this we plan to measure the kinetics of regression and/or evolution of mutant GATA1 clones following a diagnosis of TAM and the acquisition of additional genetic events in those that transform. How do These Aims Contribute to the Understanding and/or Management of Human Disease The work of my group stems directly from clinical observations made from the neonatal haematology diagnostic service established at Hammersmith Hospital just over 20 years ago. Integration of clinical, haematological and biological findings led to the work on human fetal haematopoiesis as a way of interrogating the mechanism of a number of clinical haematology problems presenting in the neonatal period. The research programme on trisomy 21-mediated perturbation of fetal haematopoiesis and leukaemogenesis sprang directly from this approach. Findings from the fetal studies have informed the prospective clinical study in neonates with Down syndrome allowing the role played by trisomy 21 at different stages of development to be captured and investigated in detail. Similarly, the neonatal study allows the clinical, haematological and molecular evolution of the neonatal preleukaemic disorder TAM to acute myeloid leukaemia of Down syndrome (ML-DS) to be studied simultaneously. In this way TAM/ML-DS represents a tractable model of childhood AML which provides a unique opportunity to investigate the cellular, genetic and epigenetic events which occur at each stage. The ultimate aim would be to use this information to accurately determine which children with Down syndrome will develop ML-DS and to effectively intervene in the transformation process to actively prevent the development of leukaemia using minimally toxic, targeted therapy. Increased understanding of how trisomy 21 transforms haematopoietic cells in children with Down syndrome may also provide insight into acute leukaemia in children without Down syndrome (given that trisomy 21 is the commonest acquired chromosomal anomaly in these leukaemias) and into the impact of aneuploidy on cell growth and differentiation in cancer in general. These translational programmes are shared between our laboratory and that of Professor Paresh Vyas. Lay Summary of Research We are investigating why children with Down syndrome have a much higher risk of developing leukaemia than other children of the same age. There is now considerable evidence that the culprit in this association with leukaemia is the extra copy of chromosome 21 (trisomy 21) which is present in every cell of the body in Down syndrome. This extra chromosome 21 disrupts the normal functioning of blood cells in particular. We know that this happens very early in life. Indeed, trisomy 21 interferes with blood development even before birth. Normally there is a well regulated system which ensures balanced production of all blood cell types. This balanced production of red blood cells, white blood cells and platelets is dramatically disturbed in Down syndrome. The disturbance sets the scene for the development of a unique transient leukaemia in newborn babies (known as Transient Abnormal Myelopoiesis; TAM) and for a full blown acute leukaemia in young children with Down syndrome which is termed Myeloid Leukaemia of Down syndrome. We also know that trisomy 21 interferes with the development of another subset of white blood cells (the lymphoid system). We think that the abnormalities in production of lymphoid cells caused by trisomy 21 help to explain the problems children with Down syndrome have with infection and why later on they may develop acute 'lymphoid' leukaemias. Our work in the lab has 2 main aims. Our first aim is to understand how trisomy 21 interferes with the genes and proteins which control blood production early in life. We are doing this through a combination of studies in the lab and in the clinic. The second aim is to use this information to help design treatment to identify children with Down syndrome at risk of developing leukaemia and design treatment strategies which reduce this risk. All Publications Over the Past 5 Years Patterson S, Chaidos A, Neville DC, Poggi A, Butters TD, Roberts IAG, Karadimitris A. Human invariant NKT cells display alloreactivity instructed by invarIant TCR-CD1d interaction and killer Ig receptors. J Immunol. 2008;181:3268-76. (5.5) Tunstall-Pedoe O, Roy A, Karadimitris A, de la Fuente J, Fisk NM, Bennett P, Norton A, Vyas P, Roberts I. Abnormalities in the myeloid progenitor compartment in Down syndrome fetal liver precede acquisition of GATA1 mutations. Blood. 112, (2008), 4507-11. (10.5) Pinto FO, Roberts I. Cord blood stem cell transplantation for haemoglobinoapthies. Br J Haematol 141, (2008), 309-324. (4.5) Roberts I, Murray NA. Neonatal thrombocytopenia. Sem Fetal Neonat Med 13, (2008), 256264. (3.5) Roberts IAG. The changing face of haemolytic disease of the newborn. Early Hum Dev 84, (2008), 515-523. (2.0) Roberts I, Stanworth S, Murray NA. Thrombocytopenia in the neonate. Blood Rev 22, (2008), 173-186. (6.0) Roberts I, de la Fuente J: Hematopoietic stem cell transplantation for hemoglobinopathies. In: Hematopoietic Stem Cell Transplantation in Clinical Practice. Eds AJ Barrett, J Treleaven, Elsevier, 2008. Stanworth SJ, Clarke P, Watts T, Ballard S, Choo L, Morris T, Murphy MF, Roberts I; Platelets and Neonatal Transfusion Study Group. Proospective, observational study of outcomes in neonates with severe thrombocytopenia. Pediatrics 124, (2009), e826-3834. (5.1) Trompeter S, Roberts I. Haemoglobin F modulation in childhood sickle cell disease. Br J Haematol. 144, (2009), 308-16. (4.5) Roy A, Roberts I, Norton A, Vyas P. Acute megakaryoblastic leukaemia (AMKL) and transient myeloproliferative disorder (TMD) in Down syndrome: a multistep model of leukaemogenesis. Br J Haematol 147, (2009), 3-12. (4.5) Roberts IAG: Prenatal and childhood transfusions. In: Practical Transfusion Medicine 3rd edition; Ch 26, pages 285-307; Editors: Murphy and Pamphilon, Blackwell, London, 2009. Roberts I, Chakravorty S: Haematological Disorders. In: Illustrated Textbook of Paediatrics; 4th edition; Chapter 22, pages 363-385; Ed Lissauer T, Clayden G, Elsevier. 2009. Alford K, Slender A, Vanes L, Li Z, Fisher ECM, Nizetic D, Orkin SH, Roberts I, and Tybulewicz VLJ: Perturbed hematopoiesis in the Tc1 mouse model of Down Syndrome. Blood (2010) 115: 2928-37. (10.5) Halsey C, Tunstall O, Gibson B, Roberts I, Graham G. Role of GATA-1s in early hematopoiesis and differences between alternative splicing in human and murine GATA-1. Blood 115, (2010), 3415-6. (10.5) Johnson MC, Kirkham FJ, Redline S, Rosen CL, Yan Y, Roberts I, Gruenwald J, Marek J, DeBaun MR. Left ventricular hypertrophy and diastolic dysfunction in children with sickle cell disease are related to asleep and waking oxygen desaturation. Blood 116, (2010), 16-21. (10.5) Clarke SA, Skinner R, Guest J, Darbyshire P, Cooper J, Shah F, Roberts I, Eiser C. Healthrelated quality of life and financial impact of caring for a child with Thalassaemia Major in the UK. Child Care Health Dev 36, (2010), 118-122. Ng GY, Roberts I, New HV. Exchange transfusion and intravenous immunoglobulin use in the UK. Arch Dis Child 95, (2010), F6-F7. (3.5) Walters MC, Hardy K, Edwards S, Adamkiewicz T, Barkovich J, Bernaudin F, Buchanan GR, Bunin N, Dickerhoff R, Giller R, Haut PR, Horan J, Hsu LL, Kamani N, Levine JE, Margolis D, Ohene-Frempong K, Patience M, Redding-Lallinger R, Roberts I, Rogers ZR, Sanders JE, Scott JP, Sullivan KM; Multicenter study of bone marrow transplantation for sickle cell disease. Pulmonary, gonadal and central nervous system status after bone marrow transplantation for sickle cell disease. Biol Bone Marrow Transplant 16, (2010), 263-272. (3.7) Roberts I, de Montalembert M. Sickle cell disease: primum non nocere (first do no harm). Haematologica 95, (2010), 4-5. (6.0) Hu M, Bassett JH, Danks L, Howell PG, Xu K, Spanoudakis E, Kotsianidis I, Boyde A, Williams GR, Horwood N, Roberts IAG, Karadimitris A. Activated invariant NKT cells regulate osteoclast development and function. J Immunol. 186, (2011), 2910-7. (5.5) Alford KA, Reinhardt K, Garnett C, Norton A, Böhmer K, von Neuhoff C, Kolenova A, Marchi E, Klusmann JH, Roberts I, Hasle H, Reinhardt D, Vyas P. Analysis of GATA1 mutations in Down syndrome transient myeloproliferative disorder and myeloid leukemia. Blood 118, (2011), 2222-2238. (10.5) Roberts I, Vyas P. Enigmatic variation. Blood 118, (2011), 6723-6724. (10.5) Zhang EG, Regan F, Layton M, Paramasivam G, Wyatt-Ashmead J, Roberts I, Kumar S. Managing the difficult case of fetal anemia. J Matern Fetal Neonatal Med 24, (2011), 1498-1503. Roberts I, Chakravorty S: Haematology. In : Neonatology at a Glance. 2nd edition; Ch 6 and Ch 7, pages 82-83; 132-137; Eds Lissauer T, Fanaroff AA. Blackwell, London, 2011. Chaidos A, Patterson S, Szydlo R, Chaudhry S, Dazzi F, Kanfer E, Macdonald D, Marin D, Milojkovic D, Pavlu J, Davis J, Rahemtulla A, Rezvani K, Goldman J, Roberts I, Apperley J, Karadimitris A. Graft invariant natural killer T-cell dose predicts risk of acute graft versus host disease in allogeneic hematopoietic stem cell transplantation. Blood 119, (2012), 5030-6. (10.5) Roy, A*, Cowan G*, Mead AJ, Filippi S, Bohn G, Chaidos A, Tunstall O, Chan JKY, Choolani M, Bennett P, Kumar S, Atkinson D, Wyatt-Ashmead J, Hu M, Stumpf M, Chou ST, Weiss MJ, Karadimitris A, Jacobsen SE, Vyas P, Roberts I. Perturbation of fetal liver hematopoietic stem and progenitor development by trisomy 21. Proc Natl Acad Sci USA 109, (2012). 17579-84. (9.3) Muthukumar P, Venkatesh V, Curley A, Cahan BC, Choo L, Ballard S, Clarke P, Watts T, Roberts I, Stanworth S; Platelets Neonatal Transfusion Study Group. Severe thrombocytopenia and patterns of bleeding in neonates: results from a prospective observational study and implications for use of platelet transfusion. Transfus Med 22, (2012), 338-343. Psaila B, Lyden D, Roberts I. Megakaryocytes, malignancy and bone marrow vascular niches. J Thromb Haemost 10, (2012), 177-188. (6.1) Chakravorty, Roberts I: How I manage neonatal thrombocytopenia. Br J Haematol 156, (2012), 155-162. (4.5) Roy A, Roberts I, Vyas P. Biology and management of transient abnormal myelopoiesis (TAM) in children with Down syndrome. Semin Fetal Neonatal Med 17, (2012), 196201. (3.5) Mullins E, Prior T, Roberts I, Kumar S. Changes in the fetal and neonatal cytokine profile in pregnancies complicatied by intrauterine growth restriction. Am J Reprod Immunol 69 (2013), 441-448. Chaidos A, Barnes C, Cowan G, May P, Melo V, Hatjiharissi E, Papaioannou M, Harrington H, Doolittle H, Terpos E, Abdalla S, Yarranton H, Naresh K, Foroni L, Reid A, Rahemtulla A, Stumpf M, Roberts I, Karadimitris A: Clinical drug resistance linked to inter-convertible phenotypic and functional states of tumor propagating cells in multiple myeloma. Blood 121, (2013), 318-328. (10.5) Roy A, Cowan G, Vyas P, Roberts I. The impact of trisomy 21 on early human hematopoiesis. Cell Cycle 12, (2013), 533-34. (4.1) Gargiulo L, Papaioannou M, Sica M, Talini G, Chaidos A, Richichi B, Nikolaev AV, Nativi C, Layton M, de la Fuente J, I Roberts, Luzzatto L, Notaro R, Karadimitris A. Glycosylphosphatidylinositol-specific, CD1d-restricted T cells in paroxysmal nocturnal hemoglobinuria. Blood 121, (2013), 2753-61. (10.5) Caputo V, Costa JR, Makarona K, Georgiou E, Layton M, Roberts I, Karadimitris A. Dissection of a functional hierarchy that determines Polycomb recruitment to CpG islands as revealed by inherited disease-associated mutation. Hum Mol Genet 22 (2013), 3187-94. (7.8) Gerrard G, Volganon M, Foong HE, Kasperaviciute D, Iskander D, Game L, Muller M, Aitman TJ, Roberts I, de la Fuente J, Foroni L, Karadimitris A. Target enrichment and high-throughput sequencing of 80 ribosomal protein genes to identify mutations associated with Diamond-Blackfan anaemia. Br J Haematol 162 (2013), 530-36. (4.5) Locatelli F, Kabbara NN, Ruggeri A, Ghavamzadeh A, Roberts I, Li CK, Bernaudin F, Vermylen C, Dalle JH, Stein J, Wynn R, Cordonnier C, Pinto F, Angelucci E, Socie G, Gluckman E, Walters M, and Rocha V. Outcome of patients with haemoglobinopathies given either cord blood or bone marrow transplantation from an HLA-identical sibling. Blood 122 (2013), 1072-78. (10.5) Innes AJ, Beattie R, Sergeant R, Ghandi D, Foroni L, Marin D, Kanfer E, Mielke S, Milojkovic D, Macdonald D, Pavlu J, Rahemtulla A, Roberts I, Slade D, Bray E, Goldman J, Apperley J, Szydlo R, Dazzi F, Rezvani K. Escalating-dose HLA-mismatched DLI is safe for the treatment of leukaemia relapse following alemtuzumab-based myeloablative allo-SCT. Bone Marrow Transplant (2013) Epub May 20 (3.5) Roberts I, Luban N, New HV: Fetal, neonatal and childhood transfusions. In: Practical Transfusion Medicine 3rd edition; Chapter 32; pages 347-367. Editors: Murphy and Pamphilon, Blackwell, London, 2013. Roberts IAG, Chakravorty S: Thrombocytopenia in the newborn. In: Platelets Third Edition; Chapter 45, pages 929-951; Editor: Michelson A, Academic Press, New York, 2013. Roberts, I, Alford K, Hall G, Juban G, Richmond H, Norton A, Vallance G, Marchi E, McGowan S, Roy A, Cowan G, Anthony M, Gupta A, Ho J, Uthaya S, Curley A, Rasiah VS, Watts T, Nicholl R, Bedford-Russell A, Blumberg R, Thomas A, Gibson B, Halsey C, Lee PW, Godambe S, Sweeney C, Perkins K, Bhatnagar N, Goriely A, Campbell P, Vyas P; Oxford-Imperial Down Syndrome Cohort Study Group. GATA1 mutant clones are frequent and often unsuspected in babies with Down syndrome: identification of a population at risk of leukemia. Blood (in press). (10.5) Roberts I, O'Connor D, Roy A, Cowan G, Vyas P. The impact of trisomy 21 on fetal haematopoiesis. Blood Cells Mol Dis (2013) Epub (2.3) Roberts IAG, Murray NA: Haematology. In: Roberton's Textbook of Neonatology 5th edition; Chapter 30; Editor: JM Rennie, Churchill Livingstone, London (in press). Roberts I, Chakravorty S: Neonatal thrombocytopenia. In: Pediatric and Adolescent Hematology: Controversies and Advances in Management. Editors: A Thomas and C Halsey. Karger AG, Basel, Switzerland (in press). Ten Key Publications Throughout your Career Knapp HR, Reilly IAG, Alessandrini P, FitzGerald GA: In vivo indexes of platelet and vascular function during fish oil administration in patients with atherosclerosis. New Engl J Med 314, (1986), 937-942. Reilly IAG, FitzGerald GA: Inhibition of thromboxane formation in vivo and ex vivo: implications for therapy with platelet inhibitory drugs. Blood 69, (1987), 180-186. Reilly IAG, Kozlowski R, Russell NH: Heterogeneous mechanisms of autocrine growth of AML blasts. Br J Haematol 72, (1989), 363-369. Rieux-Laucat F, Le Deist F, Hivroz C, Roberts IAG, Debatin KM, Fischer A, de Villartay JP: Apo-1/ Fas/ CD95 mutations in human lymphoproliferative syndrome associated with autoimmunity and defective apoptosis. Science 248, (1995) 1347-1349. Maher J, Baker DA, Manning M, Dibb NJ, Roberts IAG: Evidence for cell-specific differences in transformation by N-ras, K-ras and H-ras. Oncogene 11, (1995), 16391647. Vaughan JI, Manning M, Warwick RM, Letsky E, Murray NA, Roberts IAG: Inhibition of erythroid progenitor cell growth by anti-Kell (K): a mechanism for fetal anemia in Kimmunized pregnancies New Engl J Med 338, (1998), 798-803. Campagnoli C, Fisk NM, Bennett P, Overton T, Watts TL, Roberts IAG. Circulating hematopoietic cells in first trimester fetal blood. Blood 95, (2000), 1967-72. Tunstall-Pedoe O, Roy A, Karadimitris A, de la Fuente J, Fisk NM, Bennett P, Norton A, Vyas P, Roberts I. Abnormalities in the myeloid progenitor compartment in Down syndrome fetal liver precede acquisition of GATA1 mutations. Blood. 112, (2008), 4507-11. Roy, A*, Cowan G*, Mead AJ, Filippi S, Bohn G, Chaidos A, Tunstall O, Chan JKY, Choolani M, Bennett P, Kumar S, Atkinson D, Wyatt-Ashmead J, Hu M, Stumpf M, Chou ST, Weiss MJ, Karadimitris A, Jacobsen SE, Vyas P, Roberts I. Perturbation of fetal liver hematopoietic stem and progenitor development by trisomy 21. Proc Natl Acad Sci USA 109, (2012). 17579-84. Roberts, I, Alford K, Hall G, Juban G, Richmond H, Norton A, Vallance G, Marchi E, McGowan S, Roy A, Cowan G, Anthony M, Gupta A, Ho J, Uthaya S, Curley A, Rasiah VS, Watts T, Nicholl R, Bedford-Russell A, Blumberg R, Thomas A, Gibson B, Halsey C, Lee PW, Godambe S, Sweeney C, Perkins K, Bhatnagar N, Goriely A, Campbell P, Vyas P; Oxford-Imperial Down Syndrome Cohort Study Group. GATA1 mutant clones are frequent and often unsuspected in babies with Down syndrome: identification of a population at risk of leukemia. Blood (in press). Markers of Esteem 1994 FRCP 1997 FRCPath 2005 FRCPCH 2004 Appointed to the Executive Board, European Hematology Association 2010 Congress President, 16th Annual Congress of the European Hematology Association 2011 Hugh Jolly Lecture Current Grant Support LLR Programme Grant 2008-2013; renewal 2013-2018 (with Paresh Vyas); £1.03M, £1.4M LLR Clinical Research Fellowship 2013-2016 (with Anastasios Karadimitris); £222K Children with Cancer 2012-2014 (with P Vyas, A Karadimitris); £194K Kay Kendall Leukaemia Fund Clinical Research Fellowship 2011-2014; £219K Leuka/KKLF Clinical Research Fellowship 2012-2014; £127K MRC 2011-2014 (PI Michael Stumpf); £20K (total £309.5K) Wellcome Clinical PhD Fellowship 2011-2014 (with A Karadimitris): £251K