New Risk Assessment for cat2 conversion of analyser room
advertisement

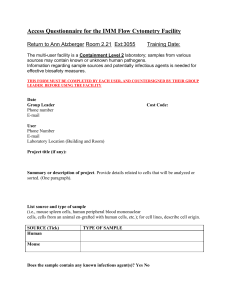
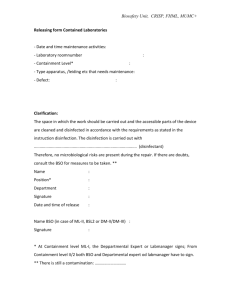
University of Cambridge NIHR BRC Phenotyping Hub, Department of Medicine Risk Assessment Form This form is to be filled in if hazard ratings/quantities/dilutions make University procedures and/or “Good Laboratory Practice” insufficient control. Group leader: Anna Petrunkina Harrison Personnel involved: Simon McCallum, Chris Bowman, Esther Perez, Renato Daniel dos Reis Colaco, Natalia Savinykh and all users of flow cytometry equipment in the analyser room Activity being assessed: HANDLING AND ANALYSING SAMPLES from UNSCREENED HUMAN tissue and blood Hazards identified: Unscreened human blood and other unscreened tissues may contain or be contaminated with Blood Borne Viruses including HIV, Hep BV, Hep CV amongst others or harbour other agents associated with them and should be handled as such. Hazards from contamination include: 1. Percutaneous inoculation from sharps, including needles, scalpels, broken glass etc. including contamination of exposed skin or pre-existing cuts and abrasions etc. 2. Inhalation of aerosols from shaking, agitation, mixing and failure of containment etc. 3. Ingestion from inadvertent sample to mouth transmission. 4. Contamination of Conjunctivae by inadvertent contact with eyes. resulting in infection. Therefore, unscreened human samples should be handled at Containment Level 2 in accordance with the revised ACDP guidance from the HSE. If there is a significant risk that, or it is actually suspected that, the blood/tissue is infected with any Blood Borne Viruses (BBVs), including the above, or any other pathogenic agent, then a separate Risk Assessment must be carried out in order to reduce the risk (e.g. fixation with PFA) and an appropriate Containment Level used. Such samples can be processed in the analyser room only after enquiries with Biological Safety Officer and after approval by Departmental Biosafety Committee. Guidance Documents: See University booklet “Safe Biological Practice (SBP) – for Prevention and Control of Exposure to Biological Agents in the Laboratory” University Clinical School Guidance on Blood Taking, Blood Handling and Work at Containment Level 2. Advisory Committee on Dangerous Pathogens (ACDP) Guidance “Protection against blood-borne infections in the workplace- HIV and Hepatitis (HSE/HMSO : ISBN 0 11 321953 9) Revised Advisory Committee on Dangerous Pathogens Guidance (www.doh.gov.uk/ACDP):- Control measures to reduce the level of risk: Unscreened human samples processed for flow cytometry analysis should be handled at Containment Level 2. In addition to the measures and facilities normally specified for work at Containment Level 2 (see relevant guidance), the additional measures listed below should also apply when, as here, Containment Level 2 is specified. These extra precautions should be in constant use to guard against percutaneous inoculation, contamination of the skin, conjunctivae, mucous membranes and the working surfaces. • All work must be conducted in a designated containment level 2 work area (Phenotyping Hub analyser lab space) with sufficient space to work safely. The right hand area in the analyser room where flow cytometers are located is designated as such an area. The left hand area is office and storage area operated at Containment Level 1 – no samples can be placed on these benches. • Access to CL2 areas is restricted to authorised staff ONLY, in order to ensure that the person(s) conducting the work is (are) free from the risk of disturbance or accidental contact with others. Access is operated via personal ID cards, and transfer/borrowing these cards is not permitted. All users will be advised on the conversion of the analyser area into a CL2 workspace, and on the necessity to adhere to procedures relevant for handling their own samples and to perform risk assessment for their own experiments. This advice is now incorporated in the training for flow cytometry area. • The use of sharps and glassware must be avoided in the Analy room. Where such use is essential, particular care must be taken in their handling and disposal after contact with unfixed materials, and any exception can be only subsequent to the application and review of the RA for the protocols. • Lesions on exposed skin should be covered with waterproof dressings. • Protective clothing must include an appropriate dark blue CL2 dedicated laboratory gown, disposable gloves and other personal protective equipment appropriate to the task, including eye protection when appropriate. It must be stated in the researchers project RA’s which PPE and when has to be worn. • The workstations must be kept clear of unnecessary equipment and not used for storage. • When operating analysers, samples must be handled with care, especially when taking them off the injection port. As all flow cytometers operate at a higher than ambient pressure, aerosols are generated when sample tubes are exchanged. These aerosols can neither be contained nor prevented. THEREFORE, NO UNSCREENED SAMPLES WHICH ARE NOT PFA-FIXED CAN BE PROCESSED IN FLOW CYTOMETRY LABORATORY WITHOUT PRIOR REVIEW OF PROJECT RISK ASSESSMENTS WITH RESPECT TO EVALUATING RISKS RELATED TO PROPAGATION OF INFECTION BY AEROSOLS ACCORDING TO THE PROCEDURE DESCRIBED BELOW: Investigators with unscreened samples which are not PFA-treated must seek advice (prior starting their experiments and using flow cytometry equipment) from Biological Safety Officer. Dr. Mark Wills will assess whether the risk assessment for experiments is adequate, in particular, whether the risk has been sufficiently reduced by additional procedures and factors (e.g. patient risk group, cell isolation, depletion, fixation, viral inactivation, screening for BBV) and refer to the Safety Committee in cases of enhanced risk. In situation where unfixed samples are handled in flow cytometry room and the residual risk is considered to be above low levels, and an approval of Safety Committee cannot be obtained, samples cannot be processed on analysers but the users are advised to contact Hub staff for advice on using operator service for analysing the samples on sorter placed in MSC. • The bench surface and any equipment must be disinfected immediately after completion of work Following disinfection policy is in operation: 1) After completion of flow cytometry work, flow cytometric equipment must be cleaned as described in the guidance notes (detergent, followed by water). The waste tank needs to be supplemented with Virkon tablets in the quantity prescribed for each particularinstruments (final concentration of ~1%). NOTE: Virkon must be never used for cleaning equipment! 2) In case of spillages, surface area has to be sprayed with Trigene and wiped. • For all staff entering the flow cytometry area for conducting work, Hep BV vaccine, together with followup procedures, should be considered. • Contaminated waste will be disposed of in accordance with local guidance and rules for the safe disposal of Containment Level 2 waste; including chemical sterilisation of liquids with autoclaving and incinerating for solids as appropriate. If it can be carried back in containment,users should feed it in to their waste streams. Level of risk remaining: Residual risk of percutaneous inoculation; which must be minimised by the avoidance of sharps. Residual risk of splashes in eyes; which must be minimised by use of suitable eye protection. Emergency procedures: NB: See Guidance Documents as above. First Aid: Wash any contaminated skin, conjunctivae or mucous membrane immediately. In the event of a wound, it should be allowed to bleed by irrigation under running water. Seek medical Advice and contact University Occupational Health Service immediately. Spillage: All spillages and surface contamination must be immediately cleaned up and removed including decontamination with a suitable validated disinfectant (10% solution of Trigene). Blockages of the equipment: If an analyser, Hub staff MUST be advised immediately on the nature of the sample, and deblocking procedure must be performed under standard GLP (with syringe and tubing to inject decon/trigene or ultrasonic bath; for non-fixed samples after shutting down the fluidics/depressurizing the system and in suitable working area covered by separate RA and SOP for deblocking procedure). Name and status of assessor: Anna Petrunkina, Director of the Cell Phenotyping Hub Date of assessment: 01/09/2014 Signature of assessor: Revision due date: 01/09/2015