RabiesTet2 - CHAMPS Online
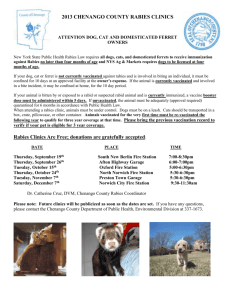
advertisement

Tetanus and Rabies Recommendations Source of Evidence: 1. ACIP. Diphtheria, tetanus, and pertussis: recommendations for vaccine use and other preventive measures – recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR 1991;40(No.RR-10). 2. CDC. Human Rabies prevention – United States, 1999:Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1999;48(44-01):1-21. Target Population: All members who present with traumatic wounds or animal inflicted injuries, particularly bites. Settings for Application: All Internal Medicine, Family Practice, Urgent Care, and Emergency Care departments. Recommendations for Tetanus Prophylaxis in Wound Management Number of prior Tetanus Vaccinations Unknown or <3 3 or more Clean, Minor Wounds Tetanus toxoid (vaccine) Yes No2 Tetanus Immune Globulin No No All Other Wounds1 Tetanus toxoid (vaccine) Yes No3 Tetanus Immune Globulin Yes No 1. Including but not limited to wounds contaminated with dirt, feces, soil or saliva; puncture wounds, avulsions; wounds created by missiles, crushing, burns, or frostbite 2. Yes, if no tetanus toxoid in past 10 years. 3. Yes, if no tetanus toxoid in past 5 years. Rabies Postexposure Prophylaxis PLEASE NOTE: Questions concerning appropriate rabies PEP can be referred to the Public Health Department at the following phone numbers. Reporting of possible rabies exposure to Colorado Department of Public Health: Mandatory reporting within 24 hours: bites by dogs, cats, bats, skunks, or other wild carnivores Mandatory reporting within 7 days: bites by any other animal not listed above Monday – Friday, 8:30 am – 5:00 pm: (303) 692-2700 All other times: (303) 370-9395 Report animal bites from animals whose whereabouts are known to the local animal control agency. Please note there is not one central animal control agency for the entire Denver-metro area. Refer to the phone book for the animal control department for your city / county government. Bite wounds: Any penetration of the skin by teeth. Bite wounds cause nearly all cases of rabies. Non-bite: Rarely do non-bite exposures from terrestrial animals cause rabies. Since there is a slight potential for transmission the following thoughts should be kept in mind. Petting of or contact with blood, urine or feces from a rabid or suspected rabid animal is not an exposure and does not warrant postexposure prophylaxis. Open wounds, abrasions or mucous membranes possibly contaminated with animal saliva, or animal scratches with saliva present warrant consideration of PEP. Recommendations for rabies postexposure prophylaxis* Animal Dogs, cats and ferrets Evaluation of animal Healthy and available for 10 days observation Rabid or suspected rabid Unknown (e.g., escaped) Skunks, raccoons, foxes, bats, groundhogs, woodchucks, foreign dogs (especially along US-Mexican border) and most other carnivores Livestock, rodents (except for groundhogs and woodchucks), rabbits or hares, squirrels and other mammals Consider as rabid unless proven otherwise Consider each case individually exposures to these animals almost never cause rabies Recommendations Do not begin prophylaxis unless animal demonstrates signs of rabies Start postexposure prophylaxis Consult I.D. or Public Health Department Start postexposure prophylaxis Bite exposure: Consult I.D. or Public Health Department Nonbite exposure: Do not start postexposure prophylaxis *Important species notes: The risk of rabies from a domestic dog, cat or ferret in Colorado is extremely low. Most cases do not require PEP. Questionable cases can be referred to ID or Public Health Department. In Colorado, bats are the major vector of rabies. Rabies in other terrestrial mammals is rare in Colorado. Bat bites can be very difficult to notice upon physical examination. Because of this, a high index of suspicion must be maintained in patients with bat exposures. Rabies PEP is usually warranted in patients with possible rabies exposure from bats. Questionable cases can be referred to ID or Public Health Department. Recommended timing of rabies postexposure prophylaxis: Rabies PEP is a medical urgency, not a medical emergency. PEP should be started as soon as possible, but in many cases it is not essential that the person receive PEP immediately. The urgency of PEP depends on the following factors: Type of exposure – if there is clear evidence by history and physical of a bite wound from a high risk animal (e.g. bat) then PEP should be started promptly; alternatively if there is not a clear bite wound or if the wound is from a low risk animal (e.g. domestic dog or cat) then it may be reasonable to defer PEP until the next day if extra time is needed to obtain PEP products and schedule the patient for an appointment. Location of wound – since rabies virus moves in a slow retrograde fashion to the central nervous system, proximity of the wound to the central nervous system (either brain or spinal cord) can help indicate the need for prompt PEP; patients with a bite wound to the face require prompt PEP, whereas those with a bite wound to an extremity may be able to have PEP deferred until the next day if extra time is needed to obtain PEP products and schedule the patient for an appointment. Availability of animal for observation / testing – in most situations where the biting animal is available for observation / testing, it is reasonable to postpone rabies PEP until the results of rabies testing of the animal is complete. Certain high risk situations, however, such as a known bat bite to the face, would likely necessitate prompt rabies PEP administration, even if results of rabies testing are pending. Providers should consider the type of exposure, the location of the wound and the availability of the biting animal for observation / testing in determining the need for prompt PEP administration. Patients who require rabies PEP should receive rabies PEP regardless of the time elapsed since exposure. Rabies postexposure prophylaxis schedule (previously vaccinated patients) Treatment Wound cleansing Rabies immune globulin Rabies vaccine Regimen All treatment should begin with thorough wound cleansing, preferably with virucidal agent such as povidone-iodine, otherwise use soap and water. Do not administer Schedule = 1.0 ml IM on days 0 and 3 1. Rabies vaccine should be administered IM in the deltoid muscle in older children and adults. 2. In infants and small children rabies vaccine should be administered in the midlateral thigh. 3. Rabies vaccine should not be administered at the same site as rabies immune globulin. Rabies postexposure prophylaxis schedule (not previously vaccinated patients) Treatment Wound cleansing Rabies immune globulin Dose = 20 IU/kg. Rabies vaccine Schedule = 1.0 ml IM on days 0,3,7,14,28 Regimen All treatment should begin with thorough wound cleansing, preferably with virucidal agent such as povidone-iodine, otherwise use soap and water. 1. If feasible, infiltrate full dose of 20 IU/kg around the wounds. 2. Administer any remaining dose IM at site distant from wound. 3. IM doses of RIG should not be administered at same site as rabies vaccine. 4. In older children and adults, IM doses of RIG should preferably be administered in the deltoid muscle. 5. In infants and small children, IM doses of RIG should be administered in the anterolateral thigh. 6. Doses greater than 5 ml should be divided and administered at separate sites. 7. The gluteal muscle should only be used when administering large volumes in divided doses to adults. 1. Rabies vaccine should be administered IM in the deltoid muscle in older children and adults. 2. In infants and small children rabies vaccine should be administered in the midlateral thigh. 3. Rabies vaccine should not be administered at the same site as rabies immune globulin. Note on administration – rabies PEP need not be administered in a specialty area. Rather, rabies PEP, can be safely administered in non-specialty areas such as Primary Care and Urgent Care. Procedure for Obtaining Rabies and Tetanus PEP Products 1. Provider or designee to contact facility pharmacy to obtain product. 2. Pharmacy to locate product at the nearest available location. If the product is unavailable from the locations listed, contact St. Joseph’s Pharmacy Department (303) 837-7576 to borrow the product. Utilize courier service to pick up and deliver the product. PRODUCT Rabies Vaccine Rabies Immune Globulin (RIG) Tetanus Immune Globulin (TIG) 3. LOCATION Warehouse / Arapahoe / Boulder / Franklin Warehouse / Arapahoe / Boulder / Franklin Warehouse / Boulder / Franklin / Lakewood / Westminster / East / Arapahoe Pharmacy to arrange for courier service. Monday through Friday 7:15am – 4:00pm: Call courier communications at (303) 8613446 to arrange for delivery. Indicate to the courier communications the following: Location to pick up product including the facility and department. Location to deliver product including the facility and department. Time frame in which product must arrive. Monday through Friday after 4:00pm, weekends or holidays: Call AM Express at (303) 367-3567. Indicate the following to the courier service: The name and phone number of the person placing the call. Location to pick up product. Include the facility name/number and department name/number. (AM Express refers to this as the reference number). For example: Westminster 07-3301. Location to deliver the product. Include the facility name/number and department name/number (AM Express refers to this as the reference number). The account / billing code is 14560. Time frame in which product must arrive. AM Express offers 1 hour, 2 hour, or 3 hour delivery service. For questions or concerns contact Denese Clark at (303) 326-6717 or pager (303) 2037808; Alex Matthews at (303) 344-7030 or pager (303) 203-8736; or Dave Schulte at (303) 344-7025 or pager (303) 203-0767.