Supplementary Information (doc 195K)
advertisement

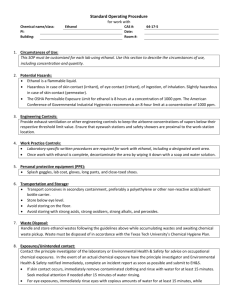
Supplementary Information Nociceptin/orphanin FQ decreases glutamate transmission and blocks ethanol-induced effects in the central amygdala of naïve and ethanol-dependent rats Marsida Kallupi1,2, Florence P. Varodayan1, Christopher S. Oleata1, Diego Correia1,3, George Luu1 and Marisa Roberto1* Materials and Methods Animals. We used adult male Wistar rats (n=68) ranging 435.2±26 g obtained from Charles River (Raleigh, NC) and housed in a temperature- and humidity-controlled room on a 12-h light/dark cycle (lights on at 6:00 am) with food and water available ad libitum. We conducted all care procedures in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals and with the Institutional Animal Care and Use Committee (IACUC) policies of The Scripps Research Institute. Slice preparation. We prepared CeA slices as previously described (Cruz et al, 2013; Cruz et al, 2012; Roberto et al, 2003; Roberto et al, 2004a; Roberto et al, 2004b; Roberto and Siggins, 2006). The rats were anesthetized with isoflurane (3%; Henry Schein, Dublin, OH) and decapitated. We cut transverse slices 300-400 µm thick on a Leica 1000S vibratome (Campden, Lafayette, IN), incubated them in an interface configuration for ~30 min, and then completely submerged and continuously superfused (flow rate of 2-4 ml/min) them with warm (31o C), equilibrated with 95% O2/5% CO2 artificial cerebrospinal fluid (aCSF) of the following composition in mM: NaCl, 130; KCl, 3.5; NaH2PO4, 1.25; MgSO4•7H2O, 1.5; CaCl2, 2.0; NaHCO3, 24; glucose, 10. Drugs were added to the aCSF from stock solutions to obtain known concentrations in the superfusate. Chronic Ethanol Treatment. We used the standard ethanol inhalation method of The Scripps Research Institute Alcohol Research Center to induce ethanol dependence (Cruz et al, 2012; Roberto et al, 2010b; Roberto et al, 2003; Roberto et al, 2004a; Roberto et al, 2004b; Roberto et al, 2006; Rogers et al, 1979). Briefly, rats were housed 2-4 per cage with a 6 AM to 6 PM light on/off cycle and with free access to food and water. Rats were placed into ethanol vapor chambers (n=20) and were intermittently exposed (14 h on, 10 h off) to ethanol vapors for 4 weeks. On experiment days, chronic ethanol exposed rats were maintained in the ethanol vapor chamber until preparation of the CeA slices (under ethanol-free conditions). We recorded from slices of chronic ethanol exposed rats 2-8 h after cutting the slices, as previously described (Roberto et al, 2004a; Roberto et al, 2004b). Naïve/control rats were exposed to air 24 h/day. Blood alcohol level (BAL). We determined BALs of the chronic ethanol treated animals from tail-blood samples. The target range for BALs in dependent rats during vapor exposure was 150200 mg%. Control animals were also routinely sampled to control for possible effects of handling. Intracellular recording of evoked responses. We recorded from CeA neurons (from the medial subdivision of the CeA) with sharp micropipettes filled with 3M KCl using discontinuous current-clamp mode (Cruz et al, 2013; Cruz et al, 2012; Haubensak et al, 2010; Roberto et al, 2004a; Roberto et al, 2004b). Data were acquired with an Axoclamp-2A amplifier (Axon Instruments, Foster City, CA) and stored for later analysis using pClamp software (Axon Instruments). We held most neurons near their resting membrane potential (RMP) and applied hyperpolarizing and depolarizing current steps (200 pA increments, 750 msec duration) to generate I–V curves. We evoked postsynaptic potentials (PSPs) by stimulating locally within the CeA through a bipolar stimulating electrode and we pharmacologically isolated excitatory postsynaptic potentials (EPSPs) by superfusing the slices with the GABAA and GABAB receptor blockers (30 M bicuculline and 1 M [1-(S)-3,4-dichlorophenyl)ethyl]amino-2-(S)hydroxypropyl-p- benzylphosphonic acid (CGP 55845A) respectively) in the aCSF. At the end of the recording we often superfused 30 µM DNQX and 30 µM DL-AP-5 to confirm the glutamatergic nature of the EPSPs. To determine the synaptic response parameters for each cell, we performed an input-output (I-O) protocol (Cruz et al, 2012; Roberto et al, 2010b; Roberto et al, 2003; Roberto et al, 2004a), consisting of a range of five current stimulations (typically between 50 and 250 nA) starting at the threshold current required to elicit an EPSP. From this threshold, the stimulus strength is increased in 3-5 steps of 30-50 nA (rate of 1 pulse per 8 sec) until the voltage required to elicit the maximum amplitude is reached. To show drug effect, we normalized the three middle (omitting threshold and maximal) stimulus intensities of five equal steps as 1-3X. These stimulus strengths were maintained throughout the entire duration of the experiment. The I/O method helps minimize inter-slice variability. We quantified the synaptic responses by calculating the EPSP amplitude with Clampfit software (Axon Instruments). We examined paired-pulse facilitation (PPF) in each neuron using paired stimuli at 50 and 100 msec inter-stimulus interval (Roberto et al, 2004b). The stimulus strength was adjusted such that the amplitude of the first EPSP was 50% of maximal, determined from the I-O relationship. We calculated the PPF ratio as the second EPSP amplitude over that of the first EPSP. All measures were taken before drug superfusion (control), during drug superfusion (10-30 min, depending on the drug), and following washout (20-30 min) and are expressed as mean ± SEM. Whole-cell patch-clamp recording of spontaneous and miniature EPSCs. We recorded from CeA neurons visualized in brain slices (300 m) using infrared differential interference contrast (IR-DIC) optics and CCD camera (ROLERA-XR, QImaging, Surrey, Canada) (Cruz et al, 2013; Cruz et al, 2012; Gilpin et al, 2011; Herman et al, 2013a; Herman et al, 2013b). A w60 water immersion objective (Olympus, Center Valley, PA) was used for identifying and approaching CeA neurons. Whole-cell voltage-clamp recordings were made with a Multiclamp 700B amplifier (Molecular Devices, Sunnyvale, CA), low-pass filtered at 2-5kHz, digitized (Digidata 1440A; Molecular Devices), and stored on a PC using pClamp 10 software (Axon Instruments). All voltage-clamp experiments were performed in a gap-free acquisition mode with a sampling rate per signal of 10 kHz. Patch pipettes (3-5MΏ) were pulled from borosilicate glass (Warner Instruments, Hamden, CT) and filled with an internal solution composed of in mM: K-gluconate, 145; EGTA, 0.5; MgCl2, 2; HEPES, 10; Na-ATP, 2; Na-GTP, 0.2. Glutamatergic spontaneous EPSCs (sEPSCs) were recorded in the presence of 30 M bicuculline and 1 M CGP 55845A, and miniature EPSCs (mEPSCs) were recorded in the presence of 1 µM tetrodotoxin (TTX). Drugs were constituted in aCSF and applied by bath superfusion. All 35 cells were clamped at -60 mV for the duration of the recording. In all experiments, series resistance (<10 MΏ) was continuously monitored with a 10 mV hyperpolarizing pulse and experiments with >20% change in series resistance were not included in the final analysis. Frequency, amplitude and kinetics of s/mEPSCs were analyzed and visually confirmed using a semi-automated threshold-based mini detection software (Mini Analysis, Synaptosoft Inc., Fort Lee, NJ). To accurately determine both the sEPSC and mEPSC amplitudes, only the events that were >5 pA were accepted for analysis. The choice of this cutoff amplitude for acceptance of s/mEPSCs was made to obtain a high signal-to-noise ratio. Averages of s/mEPSC characteristics were based on a minimum time interval of 3-5 min and a minimum of 50 events. All detected events were used for event frequency analysis, but superimposed events were eliminated for amplitude and decay kinetic analysis. All data are expressed as mean ± SEM. Drugs. We purchased picrotoxin and bicuculline from Sigma (St. Louis, MO), Tetrodotoxin from Biotum (Hayward, CA), CGP 55845A, DNQX, DL-AP5, [Nphe1]Nociceptin(1-13)NH2 and nociceptin from Tocris (Ellisville, MO), and ethanol from Remet (La Mirada, CA). All other chemical reagents were purchased from (Sigma-Aldrich, St. Louis, MO). DNQX and bicuculline were dissolved in DMSO (0.01 %), and CGP 55845A, DL-AP5, [Nphe1]Nociceptin(1-13)NH2 and nociceptin were dissolved in distilled water and then added to aCSF. Data analysis and statistics. To analyze data acquired from intracellular and whole cell recordings, we used Clampfit 10.2 (Molecular Devices) and MiniAnalysis 5.1 software (Synaptosoft), respectively. We used GraphPad Prism 5.0 software (GraphPad Software, San Diego, CA) and Statistica 7 Package (StatSoft, Tulsa, OK) for all statistical analysis of results. The s/mEPSC results were evaluated with cumulative probability analysis, and statistical significance was determined using the Kolmogorov-Smirnov, non-parametric two-sample test (Van der Kloot, 1991). The pooled data for each experimental condition were then analyzed by paired t-test analyses for individual means comparisons to evaluate single drug (nociceptin and [Nphe1]Nociceptin(1-13)NH2) effect within the same group (naïve or ethanol exposed rats) or within-subject one-way repeated measures ANOVA to evaluate multiple drugs (nociceptin, nociceptin + ethanol) effects. We used t-test analyses to evaluate differences in individual means of evoked EPSPs between two treatments (e.g., when the effect of each dose of nociceptin or the NOP receptor antagonist, [Nphe1]Nociceptin(1-13)NH2, were compared to the respective baseline values). We also used within-subject one-way RM ANOVA to compare EPSPs in the same group of cells (naïve vs. dependent rats) after application of different drugs (nociceptin, nociceptin + ethanol). When appropriate, the Student Newman-Keuls post hoc test was used to assess significance between treatments. To assess differences resulting from ethanol exposure (naive-control vs. ethanol-dependent rats) and drug interaction between groups, we used a twoway RM ANOVA. When appropriate, the Student Newman-Keuls post hoc test was used to assess significance between treatments. We accepted statistical significance at the p<0.05. All averaged values are presented as mean ± SEM. RESULTS The effects of nociceptin are not cell-type dependent. We also examined whether nociceptin effects were cell-type dependent. Thus, similar to our recent studies with ghrelin (Cruz et al, 2013) and cannabinoids (Roberto et al, 2010a), we classified neurons as Type A or Type B, according to the electrophysiological characteristics (firing pattern and lack of accommodation of action potentials) described by Schiess et al. (Schiess et al, 1999). We found a predominance (84.3%; 32/38 cells) of Type A neurons (little or no spike-frequency accommodation upon depolarization) and less (14.7%; 6/38 cells) of Type B neurons (showing accommodation) in our recorded neuronal population. Our cell typing analysis does not reveal any significant difference in the effect of nociceptin on membrane characteristics of both cell types (Supp. Fig. 1A and B), suggesting that this peptide may act independently on both cell types. Nociceptin also did not alter the number of action potentials upon depolarization (Suppl. Fig. 1C and D) in either Type A or Type B cells. It must be noted that the synaptic responses elicited by local stimulation appeared similar across all neuronal types regardless of firing properties. Supplementary Figure 1. Nociceptin has similar effects in both Type A and Type B neurons. Based on the electrophysiological characteristics ascribed by Schiess et al., (Schiess et al, 1999), we divided our CeA neuronal population into Type A (n=32) and Type B (n=6) neurons. A-B) I-V curves show that superfusion of nociceptin (500 nM) does not change the resting membrane potential in either Type A or Type B CeA neurons. C-D) In both Type A and Type B neurons, there is no alteration of the number of action potentials after 500 nM nociceptin superfusion. The number of actions potentials for Type A neurons in response to 200 and 400 pA current injection were: 4.25±0.6 and 8.95±0.8, respectively, during control recording and 4.35±0.7 and 8.85±0.8 during nociceptin superfusion. The number of actions potentials for Type B neurons in response to 200 and 400 pA current injection were: 3.5±0.6 and 5.4±0.8, respectively, during control recording and 3.25±0.8 and 5.6±0.9 during nociceptin superfusion. E-F) Representative current clamp recordings of Type A (left) and Type B (right) neurons during control (top) and nociceptin superfusion (bottom). Nociceptin did not significantly affect the firing pattern or number of action potentials in our CeA neuronal population. Supplementary Figure 2. Effects of nociceptin and ethanol at CeA synapses. Schematic diagram of a CeA GABAergic synapse and glutamatergic afferent, including presynaptic nociceptin receptors (NOP) that modulate neurotransmitter release and postsynaptic ionotropic receptors located at synapses. A) In the CeA synapse of an ethanol-naïve rat, the predominant presynaptic effect of acute alcohol is increased GABA release. Acute ethanol enhances GABA release from afferents and/or interneurons and inhibits postsynaptic glutamate receptors. Thus, acute ethanol increases the inhibition of CeA projection neurons, leading to excitation (i.e., disinhibition) of downstream (e.g., BNST) neurons. Activation of presynaptic NOP receptors reduces GABA and glutamate release onto CeA inhibitory projection neurons, and inhibits postsynaptic glutamate receptors. This occlusion of the ethanol effects on both the GABA and glutamate systems by nociceptin/NOP decreases the inhibition of the CeA projecting neurons to inhibit the downstream targets (e.g., increasing GABA release in BNST). B) Following chronic alcohol exposure (i.e., the development of alcohol dependence), the net release of GABA is increased at CeA synapses. This increased GABA release may be due to increased number and/or function of CRF1 receptors (not shown in the schematic, see (Roberto et al, 2010b)) in the CeA. There is also evidence for increased number and/or function of presynaptic NOP only on the GABAergic terminals. Activation of presynaptic NOP receptors induces a larger decrease in the release of GABA, but not glutamate, onto CeA inhibitory projection neurons, and still blocks the ethanol effects on both GABA and glutamate levels, thus further increasing the inhibition of downstream targets (e.g., BNST). References Cited Cruz MT, Herman MA, Cote DM, Ryabinin AE, Roberto M (2013). Ghrelin increases GABAergic transmission and interacts with ethanol actions in the rat central nucleus of the amygdala. Neuropsychopharmacology 38(2): 364-375. Cruz MT, Herman MA, Kallupi M, Roberto M (2012). Nociceptin/orphanin FQ blockade of corticotropin-releasing factor-induced gamma-aminobutyric acid release in central amygdala is enhanced after chronic ethanol exposure. Biol Psychiatry 71(8): 666-676. Gilpin NW, Henderson AN, Badia-Elder NE, Stewart RB (2011). Effects of neuropeptide Y and ethanol on arousal and anxiety-like behavior in alcohol-preferring rats. Alcohol 45(2): 137-145. Haubensak W, Kunwar PS, Cai H, Ciocchi S, Wall NR, Ponnusamy R, et al (2010). Genetic dissection of an amygdala microcircuit that gates conditioned fear. Nature 468(7321): 270-276. Herman MA, Contet C, Justice NJ, Vale W, Roberto M (2013a). Novel subunit-specific tonic GABA currents and differential effects of ethanol in the central amygdala of CRF receptor-1 reporter mice. J Neurosci 33(8): 3284-3298. Herman MA, Kallupi M, Luu G, Oleata CS, Heilig M, Koob GF, et al (2013b). Enhanced GABAergic transmission in the central nucleus of the amygdala of genetically selected Marchigian Sardinian rats: Alcohol and CRF effects. Neuropharmacology 67: 337-348. Roberto M, Cruz M, Bajo M, Siggins GR, Parsons LH, Schweitzer P (2010a). The endocannabinoid system tonically regulates inhibitory transmission and depresses the effect of ethanol in central amygdala. Neuropsychopharmacology 35(9): 1962-1972. Roberto M, Cruz MT, Gilpin NW, Sabino V, Schweitzer P, Bajo M, et al (2010b). Corticotropin Releasing Factor-Induced Amygdala Gamma-Aminobutyric Acid Release Plays a Key Role in Alcohol Dependence. Biol Psychiatry(67(9)): 831-839. Roberto M, Madamba SG, Moore SD, Tallent MK, Siggins GR (2003). Ethanol increases GABAergic transmission at both pre- and postsynaptic sites in rat central amygdala neurons. Proc Natl Acad Sci U S A 100(4): 2053-2058. Roberto M, Madamba SG, Stouffer DG, Parsons LH, Siggins GR (2004a). Increased GABA release in the central amygdala of ethanol-dependent rats. J Neurosci 24(45): 10159-10166. Roberto M, Schweitzer P, Madamba SG, Stouffer DG, Parsons LH, Siggins GR (2004b). Acute and chronic ethanol alter glutamatergic transmission in rat central amygdala: an in vitro and in vivo analysis. J Neurosci 24(7): 1594-1603. Roberto M, Siggins GR (2006). Nociceptin/orphanin FQ presynaptically decreases GABAergic transmission and blocks the ethanol-induced increase of GABA release in central amygdala. Proc Natl Acad Sci U S A 103(25): 9715-9720. Rogers J, Wiener SG, Bloom FE (1979). Long-term ethanol administration methods for rats: advantages of inhalation over intubation or liquid diets. Behav Neural Biol 27(4): 466-486. Schiess MC, Callahan PM, Zheng H (1999). Characterization of the electrophysiological and morphological properties of rat central amygdala neurons in vitro. J Neurosci Res 58(5): 663673. Van der Kloot W (1991). The regulation of quantal size. Prog Neurobiol 36(2): 93-130.