Allergy Resources
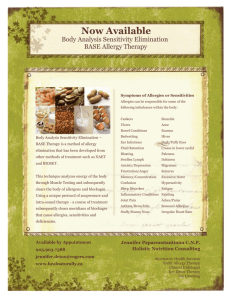
advertisement

9 Spots Where Allergy Triggers Hide Posted on November 29, 2013 You may think you’ve got allergy and asthma triggers under control in your own home. But do you really? Allergic Living helps root out some crafty culprits that have your household wheezing and sneezing: 1. The Dirt on Houseplants If you think the philodendron is setting off your sneeze attacks, think again. Indoor foliage is rarely allergenic, but the soil in over half of all houseplants is a breeding ground for mold. To prevent mold, start by replanting your greens in sterile soil. Avoid overwatering, and allow the top inch of the soil to dry out before re-wetting. Keep the plant in a sunny location and tidy up dead leaves. Finally, cover the plant soil with a layer of rocks. You’ll look like a home decor diva and the barrier will help to block the release of spores. If you do spot mold, zap it with a solution of equal parts vinegar and water. 2. Inflamed Fragrances Scented candles add ambiance to our homes, but comforting aroma comes at an irritating price. Candles, air fresheners, and even incense can emit volatile organic compounds (VOCs) into the air that increase asthma risk and can elicit eye, skin, and nasal inflammation. In a study published in the Journal of Environmental Health, 19 percent of the participants reported having breathing difficulties or other health issues when exposed to air fresheners. To limit your VOC exposure, try other types of mood lighting and natural home fragrances, like fresh baked cookies and allergy-friendly plants. For clean-air plants, see this article. 3. Too Cool Laundry Some washing machines have heat settings that can be adjusted manually, but others feed the water straight from the pipes. If you need to turn up your hot water heater for a sanitizing clean, do use caution if you have young children. A temperature that high can scald little hands.You’re washing the sheets regularly in hot water, but the sniffling still ensues when your head hits the pillow. Question: Is the water actually hot? In a South Korean study, cotton sheets that were laundered at a standard 104 degrees F only shed 6.5 percent of their dust mites. However, a wash at 140 degrees F killed off 100 percent of the mites. 4. Mite-y Plush Toys Sure you encased the mattresses in barrier bedding, but then you tucked little junior in with that cute stuffed lion (aka the dust mite colony). Those snuggly animals are a magnet for mites. To eradicate the allergen army, you can wash stuffed animals in hot water, followed by a high temperature dry, but that may cause the toys to lose their fluff. A good alternative? Freeze the toys in a plastic bag for 24 hours; freezing also kills dust mites. You can then wash them on the gentle cycle with warm or cold water, and let them air fluff in the dryer. 5. Faux Christmas Trees It’s that time of year for the Christmas tree in many living rooms. And along with the pine comes the perennial debate about which is worse for allergies, the real or the fake tree. Dr. Eric Schenkel, director of Valley Allergy and Asthma Treatment Center in Bethlehem Township, Pennsylvania, cuts down the myth that pollen-producers are always to blame. “I find more problems develop with artificial trees because they have been kept up in an attic filled with dust, and that bothers people more.” Schenkel says pine pollen is not as allergenic as most people think, although freshcut trees can introduce mold into the house. To minimize the spores, shake out the live tree or blast it outside with a leaf blower. Keep its stay in your home to a minimum; one study suggests a maximum of seven days for those sensitive to mold. 6. Dry-Cleaning Those dry-clean only labels are not only a pain to your pocketbook, they can introduce chemicals like perchloroethylene (or PERC), a VOC, into your home. The solvents used in dry-cleaning can off-gas for weeks, triggering respiratory irritation, not to mention headaches or dizziness. Avoid taking your health to the cleaners by purchasing fabrics that can be machine or hand washed. If professional help is a must, hang dry-cleaning outside for a few days of fresh air or better yet, seek out “green” cleaners who use processes that avoid harmful chemicals. For more information and tips on how to keep your home allergy free see this article. 7. Gas-tronomy When it comes to kitchen ranges, the gas vs. electric war rages on. But for asthma sufferers, electric is the mitts down winner. Gas stoves emit nitrogen dioxide, a potent and sneaky asthma trigger. Tests have shown that even if a bedroom is away from the kitchen and on a different floor, levels of nitrogen dioxide from a gas stove were high enough to trigger asthma attacks. But you’re not entirely off the hook with electric. Steam from cooking can reach ceilings and the tops of cabinets, creating a breeding ground for mold. Ensure that you have a powerful stove exhaust fan to vent both nitrogen dioxide and steam, and use it! 8. Fishy Friends Fish may seem like allergy-friendly pets, but without sufficient upkeep, Nemo can become a symptom trigger. Mold grows on various parts of fish tanks or bowls, and on areas outside of the tank that remain damp, including the underside of the lid. Scattered fish food can also encourage mold on your furniture or flooring and help to nourish a dust mite colony. To keep mold at bay, dry off above-water tank parts daily, and periodically give the tank or bowl and all its decorations a thorough cleaning. Filter media should be changed once a month to prevent mold growth and to keep fresh oxygen flowing. When you feed the fish, immediately clean up any flakes that miss the tank. 9. Hot Houses Dry sinuses and cold-induced asthma may prompt you to hibernate, but Dr. Schenkel advises his patients not to sweat it. “Dust mites are non-existent in areas of low humidity. But everywhere else in the country, you close the house up, crank the heat, and dust mite levels go really high. They thrive if the humidity is above 50 percent in your house, as does mold.” For more information on dust mites allergy see this article. You can purchase a hygrometer to monitor indoor humidity. If you’re harboring a tropical climate, consider a dehumidifier to keep the moisture levels below 35 percent during the frosty months and 50 percent for the remainder of the year. As for asthma symptoms to cold air, the good doctor says to “bundle up and stay hydrated.” DATA PRESENTED AT WORLD ALLERGY ORGANIZATION ANNUAL SYMPOSIUM DEMONSTRATES SAFETY OF SELFADMINISTERED ALLERGY SHOTS Posted on December 13, 2013 SAN ANTONIO– December 13, 2013 – United Allergy Services (UAS)®, a leading healthcare services company assisting family physicians and health systems to deliver safe and effective allergy testing and customized immunotherapy services, today announced that data from a recent retrospective study citing the safety of UAS’ protocols for seasonal and perennial allergy treatment in the primary care setting will be presented at the World Allergy Organization’s (WAO) Annual Symposium on Immunotherapy and Biologics in Chicago. The abstract was also recognized with a Top Abstract Award by the WAO. The study, “The Safety of the United Allergy Services Immunotherapy Protocol,” concludes that the risk of systemic, or adverse, reaction is less with United Allergy Services treatment protocol than traditional dosage and fast-build up RUSH methods that involve immunotherapy shots administered at a physician’s office. The UAS protocol in the study was administered by primary care physicians and utilized self (home) administration. These results are due to UAS’ slower, more incremental, immunotherapy build up phase as a self-administered treatment for patients suffering from seasonal and perennial allergies. Patients that receive allergy shots according to UAS protocols are under the care of primary care physicians. Until recently, the only real relief for allergies and allergic asthma remained primarily in the hands of allergists who administer immunotherapy shots. This already small community of approximately 5,000 U.S. specialists[i] is expected to decline by 6.8 percent by 2020, while demand for allergy-related services is projected to increase by 35 percent by the same year.[ii] This forecast only scratches the surface of the true demand for allergy and asthma care, as only a portion of the approximately 60 million Americans suffering from allergic rhinitis are aware of their condition and seek specialty care. Got the sniffles? Migraines spike with allergies and hay fever, researchers find Posted on November 25, 2013 CINCINNATI— People with migraine who also battle allergies and hay fever (rhinitis) endure a more severe form of headaches than their peers who struggle with migraine, but aren’t affected by the seasonal or year-round sniffles, according to researchers from the University of Cincinnati (UC), Montefiore Medical Center and the Albert Einstein College of Medicine of Yeshiva University and Vedanta Research. About 12 percent of the U.S. population experiences migraine, which is three times more common in women than men. Allergies and hay fever—also known as allergic rhinitis—are quite common as well, affecting anywhere from a quarter to half of the U.S. population. They produce symptoms such as a stuffy and runny nose, post nasal drip and itching of the nose. The results were published in the Monday, Nov. 25, 2013, online edition of the journal Cephalalgia. The study is one of the first tying the relationship of rhinitis— irritation and inflammation of the nasal mucus membrane caused by allergic and non-allergic triggers—to the frequency of migraine headaches, says Vincent Martin, MD, professor of medicine in UC’s division of general internal medicine, co-director of the Headache and Facial Pain Program at UC and lead author of the study. “We are not sure whether the rhinitis causes the increased frequency of headaches or whether the migraine attacks themselves produce symptoms of rhinitis in these patients,” Martin says. “What we can say is if you have these symptoms, you are more likely to have more frequent and disabling headaches.” Martin and Jonathan Bernstein, MD, professor of medicine and director of clinical research in the division of immunology, allergy and rheumatology at UC, teamed with Richard Lipton, MD, and Dawn Buse, PhD, both of Montefiore and Einstein; and Kristina Fanning, PhD; Daniel Serrano, PhD; and Michael Reed, PhD, all from Vedanta Research, to conduct the study. The researchers analyzed data from the American Migraine Prevalence and Prevention (AMPP) Study. A 2008 questionnaire was filled out by nearly 6,000 AMPP Study respondents from across the country who have experienced migraine. To define rhinitis, participants were asked the question, “Do you suffer from nasal allergies, seasonal allergies or hayfever?” Rhinitis occurred in two out of three people with migraine in this study. Bernstein adds, “The fact that rhinitis occurred in more than half of these individuals emphasizes that these disorders are intimately linked.” Based on the results, researchers found the odds of experiencing more frequent headaches for individuals with rhinitis and migraine was 33 percent greater than those battling migraines without rhinitis. The study also categorized participants with rhinitis in subsets—allergic, mixed and non-allergic rhinitis—based upon their response to questions regarding specific allergic and non-allergic rhinitis triggers. They were considered to have “allergic rhinitis” if they “only” reported having nasal symptoms with exposure to allergic triggers such as cats, dogs, molds or tree pollens. They were called “mixed rhinitis” if they “not only” had nasal symptoms with allergic triggers, but also had them with non-allergic triggers such as cigarette smoke, weather changes, perfumes and gasoline. They had “non-allergic rhinitis” if they “only” reported having symptoms when exposed to non-allergic triggers. Those with mixed rhinitis—experiencing both allergic and non-allergic triggers— fared worse than others. They were 45 percent more likely to experience more frequent headaches and 60 percent more likely to endure headaches more disabling than those without rhinitis. These findings could have implications for treatment, says Richard Lipton, MD, codirector of the Montefiore Headache Center, professor of neurology at Einstein and principal investigator of the study. “The nose has largely been ignored as an important site involved in the initiation and exacerbation of migraine headache,” Lipton explains. “If rhinitis exacerbates migraine, as these results suggest, treating rhinitis may provide an important approach to relieving headache in people with both disorders.” This builds on past research conducted by UC researchers regarding the link between allergic rhinitis and migraine, explains Martin. They found in a past study that migraine patients with allergic rhinitis receiving allergy shots had 52 percent fewer migraine attacks than those not receiving allergy shots. “This and other research indicate that allergies and hayfever may not just represent innocent bystanders in the migraine patient,” Martin states. “Clearly more research needs to be done to define their precise role.” The National Headache Foundation was a sponsor of this study. The AMPP Study was funded through a research grant to the National Headache Foundation from McNeil-Janssen Scientific Affairs LLC, Raritan, N.J. The AMPP study database was donated by McNeil-Janssen Scientific Affairs LLC to the National Headache Foundation for use in various projects. There are no financial conflicts of interest declared by the study authors. Your Month-by-Month Guide to Allergies Posted on November 22, 2013 You may feel as though you have year-round allergies, and you may be right. See what’s most likely to be causing you to sneeze and wheeze as the months go by. If you suffer from allergies for even part of the year, you may wonder when you’ll get a reprieve. People with spring allergies, fall allergies, or winter allergies might feel relief during their off seasons, but for those who experience allergy symptoms yearround — it’s a constant battle with allergens in the air. Here’s a look at which allergies plague people most — and when. January During the winter, there’s less pollen (if any) floating around, but cranking up the heat indoors can kick up house dust, a winter allergy trigger. If you’re allergic to dust, winter allergies can be just as bad as in the spring and fall. To reduce dust exposure, it helps to keep your home’s humidity below 55 percent, use a vacuum with a HEPA filter regularly, and encase pillows and mattresses with dust-mite-proof covers. February Mold and dust can cause year-round allergy symptoms, but even if dust and mold don’t bring on the sniffles for you, trees can cause your allergies to flare at this time of year, depending on where you live. “We can see tree pollen as early as February, even in the Northeast,” says Marjorie L. Slankard, MD, an associate attending physician and director of the Allergy Clinic at New YorkPresbyterian/Columbia University Medical Center. In the United States, trees that commonly cause allergies include catalpa, elm, hickory, olive, pecan, sycamore, and walnut. Tree pollen can cause the same symptoms as most spring allergies — watery eyes, sneezing, and nasal congestion March Tree pollen remains high on the list of allergens for March, which marks the beginning of spring. “If the trees, grasses, and pollens start coming out early, March can be rough going for people with spring allergies,” Dr. Slankard says. Though nice spring weather beckons you outside, if you have spring allergies, keep your eye on the pollen count. The higher the count, the worse the allergies will be. A good place to check pollen counts is at the National Allergy Bureau of the American Academy of Allergy Asthma & Immunology. April April showers can bring … spring allergies. All that rain can make for blooming flowers, but as beautiful as they are, flowers and their pollen means discomfort for people with spring allergies. In some areas of the country, grass pollen emerges in April, too. Between the pollen from the flowers and the pollen from the grass, spring allergies may make you feel especially miserable. May Allergic to tree pollen? Although tree pollination can begin as early as February, it can last through May. That means you might need to slog through spring allergies for four long months. Grass pollen can also emerge this time of year in some parts of the country. June June is a key grass pollen month in many areas, and it’s likely that grass pollen will start to trigger your spring allergies by this time of year if it hasn’t already. As the days get longer and the temperature gets higher, you’ll probably want to spend more time outdoors. If you suffer from spring allergies, you may have good days and bad days — the temperature, the rainfall amount, and even the time of day will affect grass pollen levels, and you’ll need to adjust accordingly. July The good news is that by July, grass pollen should subside and you might feel like your spring allergies are finally becoming manageable again. The bad news is that July marks the start of fungus spores and seeds, so if you’re allergic to molds and spores, too, you may feel like your allergies never end. Mold can grow on fallen leaves, compost piles, grasses, and grains. August August is a prime month for people with summer allergies to mold spores, which peak during hot, humid weather. You might want to stay inside on days when the mold spore count is particularly high. The best way to keep away from these allergens is to run the air conditioning with a HEPA filter — this cool comfort indoors should help you feel better during the dog days of August. September Late summer/early fall ragweed is the most common cause of fall allergies. Depending on where you live, ragweed-fueled fall allergies can start in August or September and continue through October and possibly November. Pollen grains are lightweight and spread easily, especially on windy days. The more wet and windy autumn is in your area, the more easily the pollen spreads, and the worse your symptoms will feel October Chances that fall allergies will ease by October get better the farther north you go in the United States. But in warmer climates, fall allergies can linger well into this month. Seasonal rain and wind can also ramp up mold spores — if your fall allergies include mold or fungi spores, your symptoms may linger. November The ragweed pollen season usually ends by mid-November in most areas of the country. If you have fall allergies and react to fungi and molds, you probably face your worst symptoms in late summer and early fall. Although you might feel miserable from the end of March until November, making it seem like you have yearround allergies, you should get a break now. November may be one of the best months for people with outdoor allergies, which allows for enjoying the crisp weather. Then, just in time, indoor allergies to pet dander and indoor molds pick up. December As pretty as they are, real Christmas trees can make you wheeze and sneeze. It’s likely not the tree itself that triggers allergies but the microscopic mold spores that can harbor in its branches. If you can’t resist buying a live tree despite winter allergies, take it home a week before you plan to decorate it and leave it in a garage or an enclosed porch. Then give it a good shake to try to get rid of any spores. Study: Hay Fever More Commonly Found In Southern U.S. Kids Posted on November 15, 2013 Children in the southern United States are more likely to suffer from hay fever, according to research conducted by the American College of Allergy, Asthma, and Immunology (ACAAI). Researchers looked at data from over 91,000 kids, finding that over 18 percent suffered from the disorder. Hay fever rates were highest in the southern and southeastern U.S., while the lowest rates occurred in Alaska, Montana and Vermont. “According to the study, wetter regions with average humidity were associated with a decreased number of children with hay fever,” said Dr. Micheal Foggs, president elect of the ACAAI. “The study also found areas of the south with warm temperatures and elevated UV indexes seem to harbor more hay fever sufferers.” Over the counter hay fever remedies include nasal corticosteroid sprays, antihistamines, decongestants, montelukast (Singulair), allergy shots and sinus rinses. Cat Allergies Double Among Asthma Sufferers, Study Reveals Posted on November 8, 2013 The number of people with asthma who are allergic to cats is on the rise — it’s doubled over 18 years, a new study finds. “From 1976 to 1994, positive allergy skin tests in people with asthma have increased significantly,” study author Dr. Leonard Bielory said in a news release from the American College of Allergy, Asthma and Immunology (ACAAI). “Not only have we found the number of asthma sufferers allergic to cats has more than doubled, but those with asthma are also 32 percent more likely to be allergic to cats than those without asthma,” he added. The researchers also found that people with asthma are more likely to be allergic to several environmental triggers common in the fall, including ragweed, ryegrass and fungus. The study was scheduled for presentation Friday at the ACAAI’s annual meeting, in Baltimore. The data and conclusions should be viewed as preliminary until published in a peer-reviewed journal. About 60 percent to 85 percent of people with asthma have at least one allergy, but the most common types of allergies in people with asthma have not been well researched, according to the ACAAI. “This study helps us better understand common trends in allergy and asthma, which can lead to improved diagnosis and treatment,” Dr. James Sublett, chair of the ACAAI indoor environment committee, said in the news release. “While it is unknown exactly why there has been an increase in asthma and allergy sufferers, it is thought a number of environmental factors can be responsible.” During the holidays, allergy symptoms can suddenly appear in people with asthma and those who’ve never had allergies. For example, while visiting friends and relatives with cats, a person may develop a runny nose, sneezing and itchy eyes. There is also something called the Thanksgiving Effect, where college students return home and discover that they are now allergic to a pet that never before triggered symptoms. “Allergies can strike at any age in life, with symptoms disappearing and resurfacing years later,” Bielory said. “Allergies and asthma are serious diseases. Misdiagnoses and inappropriate treatment can be dangerous.” Fall Allergies: Leaves Problematic for Mold Allergy Patients Posted on November 1, 2013 Fun fall decorations, such as pumpkins, hay bales and cornstalks are a great way to get in the seasonal spirit. And who doesn’t love stunning fall foliage? But if you have mold allergies, these signs of the season can do a number of your health, Michael Beninger, MD, an ear, nose and throat expert at the Cleveland Clinic warned in a news release. As ragweed season winds down in the North and Northeast, the leaves start to fall, ramping up mold production. When leaves just sit in your yard, moisture accumulates, accelerating mold growth. Fallen foliage from summer gardens gone bad and more can also be mold hot spots. As with all allergens, avoidance is your best strategy, Dr. Beninger said. “If you’re a person with bad mold allergies, you probably should spend more time indoors,” he said in a news release. “Don’t rake your own leaves; be careful with with any kind of vegetables that are rotting [such as Halloween pumpkins].” It’s also best to roll up the windows in your car or home, and run a fan at home to circulate air through your house to fight fall allergies, Warner Carr, MD, an allergist and fellow of the American College of Allergy, Asthma and Immunology, told Weather.com. It’s also essential to visit an allergist to make sure you know what you’re really allergic to, so you can create the best-possible treatment plan. “There are simple, safe and effective therapies that we can do, so people aren’t suffering from seasonal allergies,” Dr. Carr said. “Allergies can have a huge impact on quality of life, and it’s completely unnecessary suffering.” Mold allergies can create the same symptoms as other seasonal irritants: itchy, watery eyes, runny nose and nasal congestion, which often causes sleepless nights and daytime fatigue. Sore throats and headaches can also occur. For people with asthma, mold can exacerbate their symptoms when it’s inhaled, regardless if they have other allergy symptoms — though 70 percent of asthmatics also have allergies, according to the ACAAI. When Allergies Trigger Asthma: Allergic asthma is the most common form of asthma. Proper diagnosis and treatment are key to preventing attacks. Posted on October 29, 2013 More than 26 million Americans have asthma, and the number of people with it continues to rise. A chronic and potentially dangerous disease in which the airways of the lungs become inflamed, asthma is closely intertwined with allergies. “Anything that can cause allergies can also cause asthma symptoms,” said David Rosenstreich, MD, director of the Allergy and Immunology Division at Montefiore Medical Center in New York City. As many as three out of four adults with asthma have at least one allergy. In fact, the most common form of asthma is allergic asthma, which accounts for 60 percent of all cases. Allergic asthma, also known as extrinsic asthma, is set off by inhaled allergens such as dust mites, mold, pollen, and pet dander. “When some people breathe in allergens, the tubes in their lungs become inflamed,” said Dr. Rosenstreich. “People think of seasonal allergies as a runny nose, but your airway starts at your nose,” said Boyd Hehn, MD, a pulmonologist at Thomas Jefferson University and Hospitals in Philadelphia. “So it’s a chain reaction where that runny nose will cause the asthma to act up and the airway to become inflamed.” Non-allergic, or intrinsic asthma, can be triggered by other factors such as anxiety, stress, exercise, cold air, and viruses. But many of the symptoms are the same for both kinds of asthma, including coughing, wheezing, tightness in the chest, and shortness of breath. Rachel Lewis has been dealing with allergic asthma since she was a child, and she suffered her first asthma attack at age 7. “The doctors told me I would grow out of my allergies, but they’ve only gotten worse,” said Lewis, 30. For people like Lewis, it’s critical to manage their exposure to allergens that may trigger attacks. Doctors who suspect a patient has allergic asthma perform tests to see what they’re specifically allergic to. This can be done with a skin test, where a small amount of allergen is placed on top or slightly below the skin with a needle. Doctors then look for an immediate reaction, usually a rash resembling a mosquito bite. A blood test can also be done to look for allergen-specific antibodies in the bloodstream. Fall allergy season is here, and people sensitive to common autumn allergens such as ragweed and mold are starting to feel its effects. “Once the ragweed comes out, a lot of asthma patients are coming into the office,” said Dr. Hehn. “Controlling the allergies can only help in limiting asthma symptoms.” Lewis lives in Texas, where fall can be a windy season with a lot of allergens blowing around. She’s looking forward to winter, “when I can go outside and actually breathe.” Experts recommend those sensitive to seasonal allergies limit their time outdoors on days when there are high allergen counts. These daily counts can be found online through the National Allergy Bureau, part of the American Academy of Allergy, Asthma & Immunology. There are several simple steps that someone with allergic asthma can take to control their symptoms. Here are a few suggestions: Keep home and car windows shut during peak allergy times. Use an in-home air filtration system. Protective bedding covers can keep dust mites out of pillows and mattresses. Limit cats and dogs to certain rooms in the home, and keep them out of the bedroom. Bathing pets regularly reduces allergen counts, and frequent vacuuming can help control dander. Lewis has her own strategies to manage her allergic asthma: She takes hot showers after she’s been outside and exposed to pollen. She only uses fragrance-free laundry detergents. When she cleans, she wears a mask. She keeps a lint roller with her to get pet dander off her clothing. “It’s a constant effort to keep all my symptoms balanced and controlled,” said Lewis. “Some people think I’m overreacting and making my allergic asthma a bigger deal than it is. But until you go through that experience of not being able to breathe, then you don’t really know what it’s like and how scary it can be.” Think You Have A Cold? Think Again Posted on October 24, 2013 Itchy throat? Runny nose? You must have caught that bug that is “going around” the office, right? Well, not so fast. While we’re quick to jump to the “I’ve got the latest bug” conclusion, most of us neglect considering another extremely common ailment this time of year: allergies. There are actually tons of reasons why you might suffer from these late-onset seasonal allergies, even if you’ve never had a problem with them before. Sometimes stress causes our body to deplete its stores of vitamin C — leaving our immune system vulnerable. Allergic reactions can also often affect our guts, leading to sluggishness and even depression. Ultimately, consider getting a professional allergy test if you’ve got a cold that you just can’t seem to shake — it could be something else entirely.