MECHANISMS OF HUMAN DISEASE
advertisement

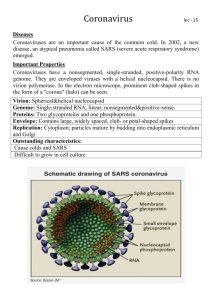
GI Tract Infections Faculty Copy – Page 1 VIROLOGY CASE-BASED SMALL GROUP DISCUSSION SESSION 20 GI TRACT INFECTIONS FRIDAY, MARCH 9, 2001 10:30AM – 12:30PM Reading Assignment: Sherris Medical Microbiology, Chapters 35, 36, 38 GI Tract Infections Faculty Copy – Page 2 CASE HISTORY 1 The patient was a 1-year-old male admitted to the hospital in December because of dehydration. His parents reported that he had a 1-day history of fever, diarrhea, emesis, and decreased urine output. On admission, his vital signs revealed a temperature of 39.5C, slight tachycardia with a pulse of 126 beats/min, and respiration of 32/min. He was less interested in play than usual. His general physical examination was remarkable for dry mouth, decreased tears when crying and hyperactive bowel sounds. Urinalysis was significant for a high specific gravity and ketones (consistent with the patient's dehydration). Stool, blood, and urine samples were sent for culture. A stool sample was also checked for ova and parasites. There were no fecal leukocytes. The patient was given intravenous normal saline and had nothing by mouth. Over the next 48 h his emesis abated. Once he was rehydrated and was tolerating oral feedings, he was discharged home. All routine cultures gave negative results, but a rapid test for rotavirus in stool was positive. BACKGROUND This child has a rotavirus infection. Rotavirus is a member of the family Reoviridae (double strand RNA viruses with segmented genomes). Group A rotavirus is the most common diarrheal pathogen seen in children less than 5-years-old in the United States. The clinical spectrum varies from asymptomatic infection to severe disease. It generally is self-limited, lasting approximately 1 week in most cases. This disease is often referred to as "winter vomiting disease". It may be responsible for as many as 50% of pediatric hospitalizations during the winter. Characteristically, rotavirus illness occurs sporadically and not in widespread outbreaks. Group B rotavirus has caused a large outbreak of diarrheal disease in Chinese adults, but is very uncommon in the United States. The differential diagnosis for acute diarrhea includes bacterial, parasitic, and viral etiologies of gastroenteritis. Because of the absence of fecal leukocytes, agents of invasive diarrhea such as Salmonella, Shigella, and Campylobacter spp. and Entamoeba histolytica are less likely, although certainly possible. The leading parasitic possibilities include Giardia and Cryptosporidium spp., especially if this child was in a day-care center. The viruses that can cause gastroenteritis include rotavirus (most frequent), enteric coronaviruses and unclassified small round viruses, Norwalk and Norwalk-like viruses, enteric adenovirus, calicivirus, and astrovirus. Norwalk virus infections can result in community outbreaks of diarrheal illness primarily in adults. GI Tract Infections Faculty Copy – Page 3 STUDY QUESTIONS 1. What type of isolation should the patient be in while in the hospital? Enteric isolation. The virus is transmitted by fecal-oral contamination. Strict hand-washing and the use of gloves by health care workers delivering care to patients with gastroenteritis are necessary. Hospital outbreaks of rotavirus infection have occurred when health care workers have transmitted the virus from one patient to another. 2. Why does rotavirus cause a watery diarrhea instead of a bloody diarrhea? Classic explanation: Rotavirus causes a malabsorptive diarrhea, which can be reduced by stopping oral feedings. The virus causes a blunting and atrophy of small intestinal villi, which results in reduced adsorptive capacity. New idea (1996). Rotavirus encodes a viral enterotoxin (NSP4). The viral enterotoxin is responsible for the acute diarrhea. (Dr. Mary Estes from Baylor Medical School demonstrated this in an animal model). Rotavirus infection does eventually result in blunting and atrophy of the intestinal villi (this process takes 2-4 days to occur and it can take 2-8 weeks to regenerate effective villi), therefore malabsorptive diarrhea is also a major problem after the initial enterotoxin induced diarrhea. 3. Describe the rapid test for rotavirus detection. The enzyme immunoassay (EIA) for rotavirus antigen was positive. This test and latex agglutination are the most common tests used to detect rotavirus. The virus was first discovered in the stools of children with vomiting and diarrhea by using electron microscopy. It was named for its characteristic wheel-like ("rota") morphologic appearance on electron microscopy. However, this technique is not routinely used because of the ease of EIA and latex agglutination. RNA gel electrophoresis can also be used to detect rotavirus in stool specimens, but its use is primarily as a research tool for epidemiologic and vaccine studies. Virus isolation is not routinely performed in a clinical laboratory setting because it is inefficient and too time consuming. 4. What is the best treatment for rotavirus infection? Effective treatment to date includes aggressive use of intravenous and/or oral rehydration therapy. Oral rehydration is limited to patients without severe vomiting. There is no specific antiviral agent for rotavirus infections. Vaccines for prevention or modification of rotavirus-induced diarrhea are A vaccine for prevention or modification of rotavirus-induced diarrhea has recently been approved (see question 7). GI Tract Infections Faculty Copy – Page 4 5. Can patients get this infection again? Yes. Type specific immunity is generated in response to rotavirus infection, which provides partial protection from another infection. However, at least 4 serotypes of rotavirus exist. 6. Are other family members likely to acquire this infection? Yes, but due to pre-existing immunity, the disease is likely to be much less severe. 7. Is there an effective vaccine to prevent illness? A new vaccine (RV-TV for rotavirus-tetravalent) was being evaluated and FDA approved on August 31, 1998. This vaccine was developed by placing the gene encoding the human rotavirus capsid protein of different serotypes into a rhesus rotavirus. All four rotavirus serotypes, are included hence the tetravalent vaccine. In the attached study, the vaccine gave 88% protection against severe diarrhea caused by rotavirus, 75% protection against dehydration and produced a 70% reduction in hospital admissions. The researchers concluded that the quadrivalent rhesus rotavirus – based vaccine induced a high level of protection against severe diarrheal illness caused by rotavirus. However, this vaccine was withdrawn from use in July, 1999. (See attached article from MMWR). This action was based on reports to the Vaccine Adverse Events Reporting System of Intussception (a type of bowel obstruction that occurs when the bowels folds in on itself) among 15 infants who received rotavirus vaccine. GI Tract Infections Faculty Copy – Page 5 CASE HISTORY 2 The patient was a 32-year-old male who presented to the emergency room with a 3-day history of fever (maximum temperature, 40C), malaise, and back pain. Laboratory data revealed a WBC count of 4,700/mm3 and abnormal liver function test results. Blood cultures were done and were subsequently reported as negative. He developed anorexia and jaundice in addition to fevers and malaise. He denied a history of intravenous drug use, sexual contact (for 2 months), and transfusions. Five weeks ago he was visiting friends in New York City, and they ate raw oysters. Recent telephone contact with one of the friends revealed that he had a similar illness. On examination the patient was mildly icteric (jaundiced). There was no rash or lymphadenopathy. The abdominal examination revealed a tender liver, which was slightly enlarged. The spleen tip was nonpalpable. Laboratory tests showed an AST level of 2,501 U/liter, and alkaline phosphatase level of 298 U/liter, a bilirubin level of 2.2 mg/dl, and a lactate dehydrogenase (LDH) level of 1,102 U/liter. Serum Hepatitis A IgM antibody was positive. Over the next month his symptoms resolved and the liver function test results returned to within normal limits. BACKGROUND This patient had hepatitis A virus (HAV) infection. HAV is a single-stranded RNA virus belonging to the picornavirus group. It can survive readily in a variety of environments, including seawater. This patient had extremely elevated liver enzyme levels, indicating that he had hepatitis. Given his case history, it is likely that his hepatitis was of an infectious etiology. The differential diagnosis of infectious hepatitis includes infection with hepatitis A, B, D (delta), and non-A, non-B (C, E) viruses, Epstein-Barr virus and cytomegalovirus, toxoplasmosis, leptospirosis, and secondary syphilis. Noninfectious (e.g., drug-induced, alcoholic) hepatitis, cirrhosis, hepatic tumor, and abscess may also result in elevated liver enzyme levels and should also be considered in his differential diagnosis. STUDY QUESTIONS 1. How is the virus transmitted? It is spread by the fecal-oral route and is well known to be acquired by eating raw oysters harvested from fecally contaminated water. Filter-feeding shellfish such as oysters, clams, and mussels are believed to concentrate the virus. This patient's history of eating raw oysters 5 weeks prior to the development of hepatitis symptoms is consistent with the incubation period for this virus, which is 2 to 8 weeks. GI Tract Infections Faculty Copy – Page 6 Because HAV is usually obtained by ingestion of fecally contaminated food or water, good hygiene practices can usually prevent spread of this infection. Since HAV is frequently associated with ingestion of raw shellfish, eating only adequately cooked seafood will eliminate the risk since the virus is inactivated by boiling for 1 min. In outbreak situations, immune globulin is valuable in preventing or suppressing HAV infection. Immune globulin is also given to nonimmune individuals (e.g., Peace Corps workers, missionaries, soldiers, and some tourists) who are traveling to areas of high endemicity which have poor sanitation. Protection in this situation usually lasts for 6 months, and people who remain in these areas for longer than 6 months must receive doses of immune globulin at 6-month intervals. 2. Describe how the HAV infection was detected? The laboratory diagnosis is a serologic one in which the serum is examined for the presence of anti-HAV immunoglobulin M (IgM) antibodies. The detection of IgM antibodies is necessary because the presence of IgG antibodies to HAV indicates a previous infection at any time in the past. The virus is not cultivable by standard laboratory methods, nor is direct detection of the virus by immunologic or electron-microscopic techniques widely available. 3. Why was liver function so abnormal and then returned to normal? differences in clinical presentation between adults and children? Explain the After initial replication in the gut, there is viremic spread of the virus to the target tissue (liver). Acute HAV and HBV infections are clinically indistinguishable. HAV infection, as was seen in this case, is generally a benign, self-limited disease. Fulminant hepatitis has been reported with this virus, but is rare. Unlike HBV, HAV does not cause chronic infection and carrier states, nor is it associated with increased risk for hepatic carcinoma. Children more frequently have asymptomatic infection which they may acquire at day care centers. They are often the source of infection for an adult. 4. What are the long term consequences for HAV infection? Recovery is generally complete with lasting immunity. 5. There is now a vaccine available for HAV. What type of vaccine is this and who should receive it? HAV vaccine has recently been licenced by the FDA. This vaccine is inactivated HAV and is very effective in preventing disease. It should be administered to international travelers, children who live in high risk GI Tract Infections Faculty Copy – Page 7 communities (Alaskan Native villages, American Indian reservations, selected other communities) homosexual men, persons with chronic liver disease, and possibly food handlers. Also, it can be used to control an outbreak of hepatitis A in a community. 6. What should be done for household contacts of the patient? They should receive Immune Globulin. CASE HISTORY 3 A 20-year-old college student developed nausea and vomiting, followed by diarrhea. Low grade fever, malaise and muscle aches were also present. After two days, all symptoms resolved without specific treatment. Several other students living in the same dormitory developed similar symptoms over the next few weeks. A Norwalk virus is suspected as the cause of this outbreak. BACKGROUND Norwalk virus is classified as a member of the Caliciviridae. These are single-strand RNA viruses with 27-38nm naked capsids. Currently there is no quick and easy assay for detection of this viral infection. Outbreaks reported to the CDC are analyzed by electron microcopy and seroconversion studies. STUDY QUESTIONS 1. How is the virus transmitted? Fecal-oral contamination. Infectivity can last for as long as 2 days after resolution of symptoms. The virus particles are extremely hardy; their infectivity persists after exposure to acid, ether and heat (60o C for 30 min). 2. What is known about the pathogenesis of the infection? The incubation period is 24-48 hours, and the mean duration of illness is 12-60 hours. Nausea is prominent, with vomiting, non-bloody diarrhea, and abdominal cramps occurring in most cases. These symptoms are experienced by all age groups, but diarrhea is relatively more prevalent among adults, whereas a higher proportion of children experience vomiting. From 25-50% of affected persons also report headache, fever chills, and myalgias. (It is not clear whether these systems are caused by a viremia or the production of interferon). Adults have died during illness caused by Norwalk-like viruses, presumably from electrolyte imbalance. Late sequelae have not been reported, GI Tract Infections Faculty Copy – Page 8 but the elderly often report persistence of constitutional symptoms for up to several weeks. 3. If the student with these symptoms visited the doctor, would laboratory tests likely be ordered? What treatment would be recommended? No laboratory tests. Symptomatic care (encourage fluids) would be administered as long as patient appeared generally well. If the patient appeared dehydrated, then rehydration IV or oral would be needed. Further workup would only be performed if the patients symptoms worsened or did not resolve in 1-2 days. 4. Is the student likely to have this infection again? Studies of volunteers have documented the paradox that persons with the highest preexisting levels of Norwalk antibodies are at highest risk of developing symptomatic infection. Most persons' antibody levels against Norwalk virus rise after infection; these titers normally peak by the third week and persist until approximately the sixth week, after which they decline. Although preexisting antibody levels correlate with risk of symptomatic illness upon exposure to the virus, acutely elevated antibody levels appear to correlate with resistance to reinfection. The nature of resistance and susceptibility to the Norwalk-like agents is poorly understood. GI Tract Infections Faculty Copy – Page 9 CASE HISTORY 4 In September, a 3- year-old black male presented to his pediatrician with a 1 day history of fever to 101.5o F. The child complained of pain when swallowing and the mother had begun to see small bumps on the palms and soles of the feet. Physical examination revealed several pharyngeal ulcerations and papulovesicular lesions on the palms and soles. A clinical diagnosis of enteroviral infection was made. The next week, the boy’s 8-year-old brought home a note from school describing a recent outbreak of this disease (see attached note). BACKGROUND Enteroviruses are positive strand RNA viruses. Hand, Foot and Mouth Disease is generally associated with infection with coxsackie A16, A5 or A10. STUDY QUESTIONS 1. How is the virus transmitted? Fecal-oral contamination. The virus is highly contagious and can reach epidemic levels, particularly in the summer and fall. Virus may be shed in the feces for three months. 2. What caused the pharyngeal ulcerations and papulovesicular lesions? The incubation period is approximately one week. After initial replication in the gut, the virus is spread to the target organ by viremia. Most patients present with papulovesicular lesions and mild fever. The lesions may last three to four days. The maculopapular eruptions may also be evident on the buttocks, extremities, and face, more often in young children. 3. Why did the physician make a clinical diagnosis instead of ordering laboratory tests to identify the infectious agent? The classic presentation and non-threatening nature of this viral infection generally allows for a clinical diagnosis. The virus can be cultured from the cutaneous vesicles or oral lesions and causes lytic cytopathic effect (CPE) in cultured cells. Immunofluorescence can then be used to "type" the virus. These studies are generally carried out for research or epidemiologic purposes, not diagnosis. 4. Are other family members likely to become infected? Yes, if they dont have pre-existing immunity. adults than in children. 5. Disease is no more severe in Will the child have recurrent infections? Type specific immunity is generated, providing protection from re-infection with that specific serotype of enterovirus. However, there are 64 serotypes of enterovirus, and little if any cross-protection. GI Tract Infections Faculty Copy – Page 10 Slide #1 Hand, foot and mouth disease Fig. 1: Hand lesions appearing as maculopapular eruptions. Fig. 2: Foot rash. Fig. 3: Ulcerated lesion on hard palate. Slide #2 Hand, foot and mouth disease Fig. 4: Palmar lesions with cloudy fluid in many vesicles. Fig. 5: Close-up view of cutaneous lesions with youngest lesions appearing as clear-fluid vesicles. Fig. 6: Palmar and lower arm lesions in a 14-month old child. GI Tract Infections Faculty Copy – Page 11 GI Tract Infections Faculty Copy – Page 12 OPTIONAL ARTICLES FOR GASTROINTESTINAL VIRUSES CASE STUDIES 1a. Efficacy of the Rhesus Rotavirus-based Quadrivalent Vaccine in infants and young Children in Venezuela (1997), Perez-School et al. NEJM, 337: 1181-1187. 1b. Withdrawl of Rotavirus Vaccine Recommendation. 1999. MMMWR, Vol. 48:1007. 2. Who should receive hepatitis A vaccine? (1995), Martha A. Brewer, B.S., Kathryn M. Edwards, M.D. and Michael D. Decker, M.D., MPH, Pediatr Infect Dis J, Vol 14, no 4:258-259. 3a. Viral Agents of Gastroenteritis. (1990), MMWR, Vol. 39, No RR5:1-2, 6-7, 16-19. 3b. Transmission of Norwalk Virus during a Football Game. (2000), NEJM 343:1223-1227. 4. Hand, Foot, and Mouth Disease. (1993), Isabelle Thomas, M.D. and Camila K. Janninger, M.D. Pediatric Dermatology, 52:265-266. *****