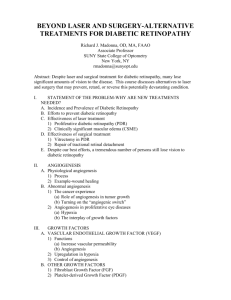
IV. Incorporating Angiogenic Growth Factors Into The Tissue
advertisement

1 A Systems Biology Approach to Promoting Angiogenesis in a Tissue Engineered Scaffold Mark Butler Abstract—Vascularization of a tissue engineered construct is critical to its long term viability in vivo. The formation of new blood vessels, angiogenesis, is a key design parameter in the development of a tissue engineered scaffold. The process of angiogenesis results from a complex cascade of events involving endothelial cell activation, migration and proliferation, organization into immature vessels, association of mural cells (pericytes and smooth muscle cells) with the immature vessels, and matrix deposition as the vessels mature. Using systems biology, the mechanisms and pathways required for each step in the process of angiogenesis are being delineated. With this understanding, more advanced polymeric scaffolds containing angiogenic growth factors can be used to promote vascular growth. Index Terms—Tissue Engineering, Angiogenesis, Scaffold, Systems Biology. I. INTRODUCTION T issue Engineering is an emerging field that involves the development of a new generation of materials capable of specific interactions with biological tissues. Combining novel materials with living cells, the hope is to create a fully functioning tissue. This is particularly useful in the realm of organ tissue replacement where there is a limited availability of donor organs or where, in some cases, (e.g., nerves) no natural replacements are available. In engineering artificial organs, a scaffold design is typically used. This involves taking a small number of cells, perhaps from the patient, and allowing them to grow on a three-dimensional porous scaffold in vitro. With subsequent transplantation in vivo the tissue would continue to grow, the scaffold would degrade, leaving behind a fully functioning organ within the patient. The scaffold design is thus key to the tissue engineered construct. The scaffold must be biocompatible and degradable within the body. It must be highly porous to allow the seeding of cells in a three-dimensional space and allow the transport of oxygen and nutrients to all cells through the development of a vascular network. The lack of vascularization, however, has been the pitfall of many tissue engineering designs resulting in the failure of long-term survival of the implanted tissue [1-2]. When cells are first transplanted into a host, on a threedimensional porous scaffold, the area within the scaffold is avascular and the transplanted cells are dependent on the diffusion of nutrients and waste for survival [3]. This diffusion limitation is adequate if the tissue is small (<1 mm thick) or the cells’ metabolic needs are low. But in the case of engineering an artificial organ, such as the liver, most cells will die soon after transplantation because of mass transport limitations [3]. Blood vessels are naturally brought into the scaffold by the invasion of surrounding tissue, but this alone is usually insufficient to provide necessary nutrients to cells within the scaffold. It is thus necessary to induce the formation of additional blood vessels in these porous matrices to enhance the long-term survival of transplanted cells [3]. The hypothesis here is that using a systems biology approach to understanding angiogenesis, the formation of new blood vessels, the scaffold could be designed to encourage blood vessel development. Angiogenic growth factors could be incorporated into the scaffold chemistry, triggering localized vessel recruitment from the surrounding tissue in the host. Many research groups have shown the feasibility of using growth factors to promote blood vessel growth and growth factors have already been used successfully to promote angiogenesis in cases of myocardial ischemia [4]. This is the result of much progress made in the understanding of blood vessel growth and development. A full systems understanding of the process of angiogenesis, however, would provide more tools for the researcher. A myriad of growth factors, released at key time points in blood vessel development is likely necessary for the sufficient vascularization of an artificial organ. II. MECHANISM OF ANGIOGENESIS Angiogenesis is defined as the growth of new blood vessels from a preexisting microvascular bed [5]. Blood vessels can be categorized into two classes: a) those lacking vascular smooth muscle cells (eg. Capillaries) and b) larger vessels with a muscular coat. Endothelial cells line the blood vessels and are involved with the development of new vessels [5]. The endothelial cell layer inside blood vessels remains dormant until activated by a stimulus, such as hypoxic conditions or growth factors. The process of angiogenesis occurs in the following steps as outlined in Fig. 1. [5-6]: 1. Angiogenic growth factors are produced. 2. Growth factors bind to specific receptors located on the endothelial cells (EC) of nearby preexisting blood vessels. 3. EC are activated once growth factors bind to their receptors. Upon activation, EC produce enzymes. 2 4. Enzymes dissolve tiny holes in the basement membrane surrounding all existing blood vessels. 5. EC proliferate and migrate out through the holes of the existing vessel. 6. Specialized molecules called adhesion molecules, or integrins (v3, v5) act like hooks to help pull the new blood vessel sprout forward. 7. Enzymes such as matrix metalloproteinases (MMP) are produced to dissolve the tissue in front of the sprouting vessel tip in order to accommodate it. As the vessel extends, the tissue is remolded around the vessel. 8. Sprouting EC roll up to form a blood vessel tube. 9. Individual blood vessel tubes connect to form blood vessel loops that can circulate blood. 10. Finally, newly formed blood vessel tubes are stabilized by specialized muscle cells (smooth muscle cells, pericytes) that provide structural support. migration and tube formation of endothelial cells and also induces in these cells the expression of many other factors and enzymes needed in the process of angiogenesis such as urkinase-type plasminogen activator (uPA) and plasminogen activator inhibitor-1 (PAI-1) [7]. In vivo, VEGF has been shown to regulate vascular permeability, which is important for the initiation of angiogenesis [7]. Hypoxic conditions, like those found in ischemic tissues, have been found to trigger the upregulation of VEGF from a variety of cell types to stimulate the expression of VEGF receptors on endothelial cells [5]. Two VEGF receptors have been isolated and characterized on endothelial cells. These are Flt-1 and Flk-1. It is thought that the Flk-1 receptor bound with a VEGF molecule controls both endothelial cell proliferation and the permeability of the vessel [5]. The angiogenic actions of VEGF are depicted in Fig. 2. Fig. 2. Actions of vascular endothelial growth factor VEGF during angiogenesis [5] 6) pericyte recruitment Fig. 1. Stages of Angiogenesis III. ANGIOGENIC GROWTH FACTORS Many growth factors have been found to initiate and control the process of angiogenesis. A growth factor is defined as an extracellular protein present in minute concentrations in vivo that activates target cells through receptor binding [5]. In a system’s biology sense these growth factors can be thought of as “on/off” switches to control the mechanism of angiogenesis discussed above. Although the complete complex mechanism of angiogenesis has not been delineated, many of the growth factors or “on” switches to promote angiogenesis have been discovered. These include Vascular Endothelial Growth Factor (VEGF), Fibroblast Growth Factor (FGF), PlateletDerived Growth Factor (PDGF) and Transforming Growth Factor (TGF). A. VEGF Vascular Endothelial Growth Factor (VEGF) is a major regulator in the vascular system. In vitro, VEGF is involved in the degradation of the extra-cellular matrix, proliferation, B. FGF The Fibroblast Growth Factor (FGF) family of proteins is made up of at least 19 members. The two most important members are acidic FGF (aFGF) and basic FGF (bFGF) because these have the most angiogenic potential [5]. Acidic and basic FGF are heparin binding monomers and are usually found in association with the extracellular matrix. FGFs bind to transmembrane tyrosine kinase receptors, named FGFR-1 through FGFR-4, which express overlapping binding patterns of the FGFs. There are several pathways that FGFs act to produce their mitogenic stimulus. FGFs stimulate the expression of proteases such as uPA and collagenase in endothelial cells [5]. Basic FGF is known to stimulate endothelial cell proliferation and migration and is also produced by endothelial cells to recruit pericytes [5]. The angiogenic actions of FGF are depicted in Fig. 3. 3 Fig. 3. Actions of acidic and basic fibroblast growth factors during angiogenesis [5] C. PDGF Platelet-derived growth factors (PDGF) are synthesized by platelets, endothelial cells, and smooth muscle cells. When PDGF is expressed by endothelial cells it acts as a mitogen for the underlying smooth muscle cells which subsequently promote smooth muscle cell expression of VEGF. PDGF secreted from endothelial cells is also thought to be involved in the recruitment of pericytes and the differentiation of endothelial cell precursors [5]. factor into the scaffold with success. Perets et al (2002) found a four-fold increase in the number of penetrating capillaries into their bFGF-releasing scaffolds compared to the control scaffold [8]. Using a VEGF secreting scaffold, Peters et al. (2001) found a 160% increase in capillary density in their scaffolds compared to the control [9]. These results suggest that a polymer-based delivery system can be used engineer more extensive vascular networks and to create a better environment for the survival and proliferation of transplanted cells. These single growth factor models are not, however, perfect. It was observed by Perets et al. (2002) that there was minimal capillary ingrowth into the pores in both the bFGF loaded and control scaffolds [8]. This is not surprising as angiogenesis is not governed by one single growth factor. A large number of growth factors have been identified, each with a particular role in the complex mechanism of angiogenesis. Richardson et al. (2001) developed a novel system for dual growth factor delivery in a polymer scaffold [10]. They incorporated both VEGF and PDGF into their scaffolds by simply mixing the VEGF and pre-encapsulating the PDGF before mixing with the polymer (Fig. 4). VEGF is a well known initiator of angiogenesis, but its presence is often not sufficient for the formation of complex and mature vasculature. PDGF promotes the maturation of blood vessels by the recruitment of smooth muscle cells to the endothelial lining of the growing vessels. The incorporation of both of these growth factors coupled with the fact that the simple mixing of VEGF gave a fast time release (to initiate angiogenesis) while the pre-encapsulation gave a longer release time of PDGF (to help maturation of vessels) resulted in the rapid formation of a mature vascular network in the scaffold [10]. D. TGF-β Transforming Growth Factor β (TGF-β) acts as a stimulus for angiogenesis through many pathways. Although the complete mechanism is unknown, TGF-β induces the expression of several angiogenic growth factors, acting through paracrine signaling [5]. TGF-β has been shown to upregulate the expression of PDGF in endothelial cells as well as VEGF and bFGF expression by smooth muscle cells [5]. IV. INCORPORATING ANGIOGENIC GROWTH FACTORS INTO THE TISSUE ENGINEERED CONSTRUCT The most critical challenge that must be overcome to tissue engineer scaffolds for artificial organs is how to induce vascularization. One possible solution is the incorporation of angiogenic growth factors, such as VEGF or FGF discussed above, into the polymeric scaffold. Upon implantation, these growth factors would be released from the polymeric scaffold and trigger an angiogenic response. Many studies have looked at incorporating a single growth Fig. 4. Schematic of scaffold fabrication process used by Perets et al. (2002) [10]. Growth factors were incorporated into polymer scaffolds by either mixing with polymer particles before processing into scaffolds (VEGF), or pre-encapsulating the factor (PDGF) into polymer microspheres used to form scaffolds. The VEGF incorporation approach results in the factor being largely associated with the surface of the polymer, and subject to rapid release. In contrast, the PDGF incorporation approach is predicted to result in a more even distribution of factor throughout the polymer, with release regulated by the degradation of the polymer used to form microspheres [10]. An optimum scaffold would release many growth factors with independent kinetics so that different factors could act at 4 distinct stages of vascular development. This could be accomplished through the mode of incorporation of the growth factor in the scaffold. Growth factors needed to initiate angiogenesis could be simply mixed with the polymer to give rapid release kinetics (eg. VEGF). Other growth factors necessary at intermediate time points in the mechanism of angiogenesis (eg. PDGF) could be encapsulated in polymers of varying chemistries with different degradation times to give the appropriate release kinetics. Researching polymeric systems for release of multiple growth factors will therefore become of high importance to the tissue engineer. V. USING SYSTEMS BIOLOGY TO UNDERSTAND ANGIOGENESIS A polymeric system capable of releasing multiple factors with distinct kinetics is useful only if key growth factors have been identified. Although much research has been conducted on understanding the mechanism of angiogenesis, a full systems understanding would provide an exhaustive list of all growth factors necessary and present at all time points during vascular development. Understanding the relationships between growth factors and the pathways that they follow during angiogenesis would allow the design of a scaffold that closely mimics the signals and conditions found in vivo during angiogenesis. This would ultimately improve the vascularization of the tissue engineered construct and render feasible the possibility of engineering large artificial organs. The systems biology approach to studying angiogenesis would involve systematically perturbing the system. Perhaps, the system could be taken as the vascularization of a developing embryo, which could be genetically modified to eliminate or replace the gene responsible for producing the VEGF growth factor. How have the gene, protein, and informational pathway responses changed due to this perturbation? Taking this information, a mathematical model that describes the structure of the VEGF pathway in angiogenesis and how it responds to individual perturbations could be established. Performing these types of experiments would help to piece together the master plan that dictates the overall process of angiogenesis. Hopefully, key nodes in the network would be identified where perturbations have a profound effect on the system. This knowledge would be invaluable when designing a polymeric scaffold to help guide the development of vasculature in a tissue engineered construct. VI. CONCLUSION The success of engineering large artificial organs is a dream that has been limited by the lack of vascularization in porous polymeric tissue engineered constructs. One solution to promote angiogenesis is to incorporate angiogenic growth factors into the polymeric scaffold that would be released as the scaffold degrades. A systems biology approach to angiogenesis would lead to a better understanding of the mechanism of angiogenesis including all growth factors and pathways involved. Many growth factors key to the process of vascularization have been identified. These include VEGF, FGF, PDGF and TGF. Incorporating a single growth factor into a scaffold has been shown to have a successful angiogenic response. This suggests that a polymer-based delivery system can indeed be used engineer more extensive vascular networks and to create a better environment for the survival and proliferation of transplanted cells. The process of angiogenesis is governed not by a single growth factor, however, but by a cascade of growth factors occurring in a certain temporal sequence. A polymeric system capable of releasing multiple growth factors with distinct kinetics is needed to improve vascularization of the tissue engineered construct and make the availability of large artificial organs a reality. REFERENCES Mooney, D. J. et al. “Growing new organs,” Scientific America, vol. 280, 1999, pp. 60-65. [2] Vogel, Viola., et al. “The Tissue Engineering Puzzle: A Molecular Perspective,” Annu. Rev. Biomed. Eng., vol. 5, 2003, pp. 441-463. [3] Peters, Martin C., et al. “Engineering vascular networks in porous polymer matrices,” J Biomed Mater Res, vol. 60, 2002, pp. 668-678. [4] Nomi, M., et al. “Principals of neovascularization for tissue engineering,” Molecular Aspects of Medicine, vol. 23, 2002, pp. 463483. [5] Ahrendt, G., et al. “Angiogenic Growth Factors: A Review for Tissue Engineering,” Tissue Engineering, vol. 4, Number 2, 1998. [6] Conway, Edward M., et al. “Molecular mechanisms of blood vessel growth,” Cardiovascular Research, vol. 49, 2001, pp. 507-521. [7] Liekens, S., et al. “Angiogenesis: regulators and clinical applications,” Biochemical Pharmacology, vol. 61, 2001, pp. 253-270. [8] Perets, Anat., et al. “Enhancing the vascularization of threedimensional porous alginate scaffolds by incorporating controlled release basic fibroblast growth factor microspheres,” J Biomed Mat Res, vol. 65A, 2003, pp. 489-497. [9] Peters, Martin C., et al. “Engineering vascular networks in porous polymer matrices,” J Biomed Mat Res, vol. 60, 2002, pp. 489-497. [10] Richardson, Thomas P., et al. “Polymeric system for dual growth factor delivery,” Nature Biotechnology, vol. 19, November 2001. [1]