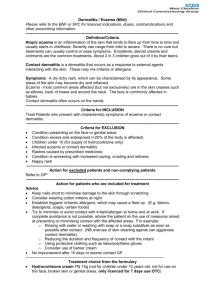
Dermatitis is inflammation of the superficial dermis and
advertisement

Protèque International, LLC 4020 Westchase Boulevard Suite 220 C Raleigh NC 27607 (919) 828-2877 Voice 919-828-2595 fax 800-953-9250 Customer Service E-mail: info@proteque.com Website: http://www.proteque.com PROTÈQUE SPONSORED EDUCATION “What every family with Eczema should know: Education Guide for Parents and Physicians” CONTENTS Page 1) 2 2) Who gets eczema? What are the symptoms and trigger factors? a) What is it and what are the symptoms? b) What are the trigger factors? 3) Cure it, Outgrow it, or Relieve it — What is most likely? a) Is there a cure for eczema? b) How long does it take for a child to outgrow eczema? c) How concerned are physicians about relief of eczema symptoms versus relapse control using steroids? 4) 4 4 4 How to manage eczema by preventing outbreaks? a) Prevention b) Relief c) Side effects: Emotional, and Physical 4) 2 3 5 6 7 What to do next? a) What to ask your doctor about? b) Survey -- Reasons physicians and consumers recommend non-steroid Proteque SPS Lotion. REFERENCES © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 9 9 10 page 1 __________________________________________________________________________________ 1) Who gets eczema? Doctors refer to most skin problems as “eczema”(pronounced ek-zema) or “dermatitis”. The symptoms are dryness, itch, redness, swelling, irritation, burning, rash, blisters, small bumps, or peeling. Dermatitis is common in babies, children, adolescents and many adults. At least two-thirds of eczema sufferers are female. In 1976, the statistics for prevalence of dermatitis between 1 and 5 years of age were 34.5 per 1000; between 6 and 11 years, 26.7 per 1000; and between 12 and 17 years, 35.5 per 1000. 1 Since 1970, the incidence of atopic dermatitis has nearly tripled. In 1999, according to noted dermatology researcher, Amy Paller, MD, Children’s Hospital, Chicago, 10 to 20 percent of all infants are sufferers, with a majority of cases diagnosed as early as twelve months of age. Studies point to environmental factors as contributing to the dramatic boost in the number of people with eczema including irritants and allergens that trigger the immune system. ________________________________________________________________________________________________ 2) What are the symptoms and trigger factors? 2a) What is it and what are the symptoms? Atopic Dermatitis (AD) A chronic inflammatory skin disorder seen in individuals with a hereditary predisposition to a lowered cutaneous (skin) threshold to pruritus (itch), and principally characterized by extreme itching, leading to scratching and rubbing that in turn results in the typical lesions of eczema. Usually there are other family members that have history of asthma, allergic rhinitis (hay fever) or actually have been diagnosed as “atopic”. Atopic dermatitis (AD) is a familial disease (runs in families) and the exact cause is not known. It usually develops in infancy, childhood and sometimes into adult life. AD is NOT a contagious disease. Atopic dermatitis (AD) in infants can appear at 1-6 months of age and lasts about 2-3 years. The lesions can be generalized and widespread over the body sparing only the diaper area. Typically there is a rash of red itchy papules, which will ooze and crust. The rash can cover the head, neck, and trunk as well as the extensors of the extremities. In childhood AD occurs between the ages of 4-10 years. The lesions involve the flexures of the arms and legs, neck, wrists and ankles. These areas tend to develop secondary infections caused by breaks in the skin from intense scratching. Although the outbreak may become chronic these children often do have periods of remission. By 10-14 years of age 75% of these individuals improve while the other 25% may develop chronic adult disease. Usually the flexures of the arms and legs and the neck are the areas of involvement however some patients will develop widespread lesions. Eczema (ek´zêma) A general term for any superficial inflammatory process involving primarily the epidermis, marked early by redness, itching, minute papules and vesicles, weeping, oozing, and crusting, and later by scaling, lichenification, (thickening of the skin) and often pigmentation. Eczema is a common allergic reaction in children but it also occurs in adults, usually in a more severe form. Childhood eczema often begins in infancy, the rash appearing on the face, neck, and folds of elbows and knees. It may disappear by itself when an offending food is removed from the diet, or it may become more extensive and in some instances cover the entire surface of the body. Severe eczema can be complicated by skin infections. Childhood eczema may persist for several years or return after the child is older. Persons suffering from childhood eczema may develop another allergic condition later, most often hay fever or asthma. Eczema is sometimes caused by an allergic sensitivity to foods such as milk, fish, or eggs. Inhalant allergens such as dust and pollens 1 Prevalence of dermatologic disease among persons age 1 - 74: US, Washington, DC 1977, USDHEW Advanced Data © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 2 rarely cause eczema. Treatment involves the use of soothing baths, moisturizing creams, topical steroids, and oral antihistamines to alleviate itching. Dermatitis (der´mah-ti´tis) -- Inflammation of the skin. Dermatitis can result from various animal, vegetable, and chemical substances, from heat or cold, from mechanical irritation, from certain forms of malnutrition, or from infectious disease. In some cases, dermatitis may have a psychologic rather than a physical cause. The symptoms may include itching, redness, crustiness, blisters, watery discharges, fissures, or other changes in the normal condition of the skin. The treatment of dermatitis varies greatly and is determined by the cause. Cortisonecontaining creams, lotions, and ointments are frequently prescribed as a palliative measure. Contact Dermatitis An immune system skin response marked by itching, swelling, blistering, oozing, and scaling. It is caused by direct contact between the skin and a substance to which the person is allergic or sensitive. The irritation or rash usually occurs only on that area of the body that has come into contact with the substance. The most common form of allergic contact dermatitis is that caused by POISON IVY, OAK, OR SUMAC; nickel in jewelry; and latex gloves. Other plants, too, sometimes cause an allergic reaction. Contact dermatitis may also be caused by paper, industrial oils, medicines, cosmetics, perfumes, mouthwashes, deodorants, rubber, plastics, metals, and clothing made of various materials and treated with certain preservatives and dyes. Irritant Contact Dermatitis A non-allergic type of CONTACT DERMATITIS due to exposure to a substance that damages the skin rather than acting as a sensitizer or allergen. A non-allergic form, irritant contact dermatitis, may be induced by a substance acting as an irritant rather than as a sensitizer or allergen. Some soaps, detergents, and other cleansing products can cause a condition of the hands often referred to as irritant contact dermatitis (popularly called "housewives” dermatitis or dishpan hands"). According to dermatitis researcher Dr. Howard I. Maibach, 80% of Dermatitis is irritant and 20% is allergic. Itching associated with Eczema and Dermatitis The presence of itching is so characteristic of eczema that most dermatologists won’t make a diagnosis without it. Atopic eczema has been called “the itch that rashes” The itching that occurs with this condition is extremely severe and intense, and a child will scratch so hard that the skin will be broken. Once there is a break in the skin it becomes the portal of entry for bacteria to enter the blood stream and cause a secondary bacterial infection. It is important to focus on relieving the itch not trying to stop the child from scratching. 2b) What are the trigger factors? Factors that can trigger an outbreak Dry skin Sweating (neck, bends of elbows and knees) Sensitivity to irritants in environment Sensitivity to allergens Infection Stress and anxiety Changes in temperature or humidity Irritating clothing (especially wool) Food allergies Topical medications © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 3 ________________________________________________________________________________________________ 3) Cure it, Outgrow it, or Relieve it — What is most likely? 3a) Is there a cure for eczema? It is important to know that there is NO CURE for dermatitis or eczema. The exact cause of eczema is not known. 3b) How long does it take for a child to outgrow eczema? Nearly 40 percent of child sufferers outgrow eczema. That still leaves the other 60 percent who don’t outgrow it, suffer with it, and incur untold medical expenses trying to manage it with steroids, special cleansers, special diets, skin care and hair care products, and antibiotics. With the right therapy prescribed by their physician, and avoiding factors that can trigger an outbreak, remissions do occur for periods of time. Dr. Guy Webster, dermatologist, Jefferson Medical College, Philadelphia, Pa. Says, "While its causes remain unclear, we know that patients have defects in one or more of their genes that makes their skin's immune system overactive. Environmental irritants, allergens and stress provoke skin flares." It is important to learn to manage the condition and teach the child to avoid contact with substances known to irritate the skin to prevent outbreaks of the rash. ALWAYS KEEP THE SKIN MOISTURIZED. Even after all the necessary precautions are taken and a flare up occurs, the child and the parents should not feel guilty. Just start a treatment as soon as possible to get it under control. 3c) How concerned are physicians about the relief of eczema symptoms versus relapse control using steroids? Short-Term Relief Of Eczema versus Relapse Control Dr. Robin Graham Brown, a dermatological consultant at the Leicester (England) Royal Infirmary, presented results at the Society of Investigative Dermatology annual meeting. Dr. Brown surveyed 340 physicians who had appreciable eczema case loads. The physicians were from eight countries, including the United States, Germany, Korea, and Mexico. When asked how they treated eczema, most said they aimed for immediate symptomatic relief for the patient. Only a small number tailored their approach so that it was part of a long-term management plan. In the United States, for instance, 50% of the physicians said they aimed for immediate relief, while only 10% of the physicians addressed preventing or reducing relapse. “This short-term focus when actually treating was not just a reflection of Western culture or a phenomenon of developed countries or specific to a particular payment system,” Dr. Graham-Brown said. It was common across national groups. In Korea, for example, 80% of the physicians surveyed said they aimed for immediate relief. The physicians on the whole said they were confident in their ability to manage patients and were satisfied with the treatments. But they also acknowledged that many patients seek treatment elsewhere and that a majority of patients are dissatisfied with their care. Topical corticosteroids were the therapy used most often by the physicians surveyed. But the physicians also indicated that concerns about corticosteroid use somewhat hampered their use. Most of the physicians said they were confident that they knew how corticosteroids should be used, but they also agreed with a statement that side effects lead to inappropriate underusage. Protèque Editorial Note: Non-Steroid Protèque® has been developed and clinically tested as a complementary steroidsparing strategy for prevention and long-term management of eczema/dermatitis, and to prevent relapse commonly experienced by users of corticosteroids. Pharmaceutical companies realized over $1.5 billion annual sales in the US from corticosteroid sales, much of which are medium to high potency, without the patient knowing or understanding the longterm side effects of osteoporosis, thinning of the skin, hyperpigmentation, cataracts, and growth retardation in children. Consumer and physician education, especially for Pediatricians and GP/Family Practice Physicians and Allergists is primary means by which the Protèque® brand will be adopted as the new standard by eczema suffers and the parents of children with eczema. Corticosteroids continue to play a vital role in healthcare and should be used properly in the right concentrations, with the right patients, for the right duration, with more appropriate complementary, ongoing management and prevention therapies and education © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 4 ________________________________________________________________________________________________ 4) HOW TO MANAGE ECZEMA BY PREVENTING OUTBREAKS? Always consult your physician for a proper diagnosis before treating any skin condition that you or your child may have. 4a) PREVENTION Avoid contact with any known substances that can cause the skin to break out. This could be food, clothing, plants, chemicals, metals, etc. Limit bathing. Water and soaps strip the natural oils from the skin causing drying of the skin. Bathe using lukewarm water because hot water will dry skin. Use a mild soap and very little of it to wash important areas. Use a towel to blot the skin dry. Rubbing can cause irritation to the skin. Avoid using bubble bath in tub water. In cold climates (winter) Use a humidifier to add moisture to the environment especially the bedroom while sleeping. Dry heat in a home will cause dryness of the skin and cause itching. Dress in layers so it will be possible to add or remove layers when needed. Wear clothes made of cotton fabrics. Wool, polyester and nylon fabrics are especially irritating to the skin Permanent press clothing has formaldehyde resins in the fabric and can cause allergic contact Dermatitis in those that are sensitive. Use Protèque SPS protectant daily to prevent moisture loss, itching and irritation for hours. In warmer (summer) climate Keep environment cool (air conditioning) especially when sleeping. Wear light cotton bedclothes. Avoid activities outside when it is hot especially during a flare up. Sweating can cause itching. Wear clothes made of cotton fabrics. Cotton is less irritating and will absorb perspiration and keep the skin cool Use Protèque SPS protectant daily to prevent moisture loss, itching and irritation for hours. Apply Protèque SPS water- resistant protectant before swimming in pools. Chemicals in pool water can irritate the skin. Always wash off chlorine after swimming and reapply Protèque SPS skin protectant. (ALWAYS use sun block) Use Protèque SPS as a skin protectant daily to prevent moisture loss, itching and irritation for hours. Dry skin associated with eczema can cause itching. It is not known what will trigger an outbreak of eczema or when it will happen, so always take preventive measures. IT IS BETTER TO PREVENT THE OUTBREAK THAN HAVE TO TREAT IT. Skin should ALWAYS be protected even when there are no sings of irritation. The skin, the largest organ of the body, is a waterproof barrier that protects all the other organs against infection, injury, and harmful sun rays. One of the biggest challenges of AD is to prevent a flare up, and maintain a safe and healthy skin environment. Diet Eliminate foods from your child’s diet only if there is a known allergy to them. Examples of foods that some children are sensitive to are eggs, peanuts, tomatoes, milk, soy, wheat and seafood . Consult your physician before eliminating any foods from your child’s diet for prolonged periods of time to avoid malnutrition. Keep a diary of foods eaten and the condition of the skin. When weaning off the foods, do it slowly and make observations of the skin condition and any reactions. Consider “nickel” as a cause or trigger. Rash may occur in areas where you might wear jewelry, or on the chest and back from snaps on clothes, or © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 5 the metal closure of a bra. Notice if there is a rash on the abdomen at the waistline where a belt buckle or a zipper closure is located. Girls experience more contact allergy than boys as a result of greater use of jewelry and possibly because of hormonal differences Consider latex or rubber products as a cause or trigger. A rash may be present on the feet (from tennis shoes) or the waist area from the elastic waistband on Clothes especially under garments, or rash on the face when blowing up a latex balloon Young children may experience perioral dermatitis from putting rubber toys into their mouths Clothes Wash clothes in very mild detergents Avoid using fabric softeners and bleach Wear cotton clothes – synthetic fabrics and wool can irritate the skin Learn to recognize the signs and symptoms of skin infection: Bacterial “Staph” infections are common. Crusting Pustules Increased redness Swelling Red streaks Fever Bacteria called Staph. aureus colonizes on the skin and can cause secondary infections. Monitor for signs and symptoms of secondary infection and notify your physician immediately. antibiotics may be prescribed only if there is a clinical infection. PARENTS MAY CARRY STAPH AUREUS ON THEIR HANDS AND CAN REINFECT THE CHILD. WASH YOUR HANDS frequently and apply Protèque to hands 1-2 times daily to reduce cross infection! Staph Aureus can also be carried in the nasal passages and this area would have to be cultured by a physician for diagnosis and treatment. 4b) RELIEF / TREATMENT TOPICAL STEROIDS – When the skin becomes severely inflamed topical steroids may be needed. Use topical steroids as prescribed by your physician. There are strengths of steroids: mild potency, mid-potent, potent, and super potent. The strength of the steroid is determined by the age of the patient, the severity of the outbreak, and the area of the body to be treated. The physician should monitor the patient regularly while using steroids. Side effects of steroids are due to overuse beyond recommended 10 days, use on face and diaper areas and inappropriate use of over potent steroid strength. TOPICAL STEROIDS ARE NOT MEANT TO BE USED AS A MOISTURIZER. ALWAYS USE GOOD JUDGEMENT WHEN USING CORTICOSTEROID CREAMS AND OINTMENTS. Ask your physician about the potency of prescription corticosteroids and possible side effects of the medication with long term use. Do not use high potency steroids on the face Do not use topical steroids in the diaper area. DO NOT OVERUSE! RELIEVE THE ITCH! – Atopic dermatitis is called the “Itch that rashes”. The itching can be severe and intense and wake a child out of a sleep. They will scratch so hard creating a break in the skin where bacteria can enter and cause a staph. infection. Sometimes they will scratch themselves while sleeping rubbing their arms and legs on the bed linens. antihistamines can be prescribed to help control itching. They work best at night because they act like a sedative and cause sleepiness. keep the fingernails short to prevent breaks in the skin cover the hands with cotton gloves at bedtime to prevent scratching when sleeping use cotton clothing and bedding – cotton keeps the skin cool © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 6 reduce dust mites in the house – mites thrive in warm moist environments like bedding, mattresses, curtains and carpets. Regular vacuuming, damp dusting and airing of bedding are effective ways to accomplish this distraction during the day often helps not to focus on itching use Protèque SPS 1 – 2 a day to relieve the itching Be patient STING – STING FACTOR “ When every application of medication causes a struggle, the child and the family are affected by it and compliance is bound to suffer. Physicians can apply topical drugs to a child’s intact skin and then to an area affected by acute dermatitis to see whether a sting reaction occurs. If there is no sting reaction the child will smile,” reported dermatologist Dr. Mary Spraker of Emory University of Atlanta. (Skin & Allergy News, May, 2000) 4c) Side Effects SIDE EFFECTS OF TOPICAL STEROIDS LOCAL Striae (stripes or bands, like stretch marks) especially in genital area & underarms Persistent erythema (redness) & telangiectasis (chronic dilation of blood vessels on the skin) Pustular acneiform eruption (face) steroid rosacea Atrophic, shiny, erythematous skin (thin, shiny red skin) Steroid Addiction Syndrome Allergic Contact Dermatitis Hypertrichosis (abnormal growth of hair) Foliculitis (inflammation of hair follicle, lesions may be pustules or pimples) SYSTEMIC Stunted growth in children Cataracts and glaucoma Glycosuria (glucose in urine) Cushings Syndrome (abnormality of the pituitary gland characterized by obesity, moon face, hypertension, excessive hair growth, stunted growth in children, menstrual irregularities, or other serious medical problems) Osteoporosis Diminished resistance to infection Suppression of Hypothalmic – pituitary- adrenal axis TOPICAL STEROID ADDICTION “Since potent and superpotent topical glucocorticosteroids have become available, a syndrome of topical steroid addiction has been recognized. The syndrome is the result of chronic daily application for greater than a month of a potent glucorticosteroid preparation to the facial skin. As the treatment continues, the patient experiences a rebound vasodilatation of the facial skin 2-6 hours after the application. The face becomes red, and the patient applies the steroid more frequently. Soon, burning of the skin is experienced and is only relieved by further steroid applications. Permanent redness of the facial skin eventuates, with thinning and fine wrinkling of the skin is observed. It is difficult to withdraw the steroid because the patient cannot tolerate the burning sensation, which is relieved only by topical steroids. Substitution of a bland ointment for the topical steroid plus the administration of oral antihistamines will result in progressive improvement over 4 weeks. In susceptible infants and children, application of potent or moderately potent glucocorticosteroid preparations to the facial skin may also result in redness and acneiform papules and pustules located on the nose, chin, cheeks, and lower eyelids. This is known as “acne rosacea”. Abruptly stopping the topical steroid preparation will result in increased numbers of papules and pustules over the subsequent 7 days. Treatment is that recommended for acne, with severe forms requiring systemic antibiotics. © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 7 William L. Weston, M.D., Alfred T. Lane, M.D., Joseph G. Morelli, M.D.,“Color Textbook of Pediatric Dermatology”, 2nd Edition, 1996 Emotional Because there is no cure for AD, managing the disease is frustrating for both the parents and the child. It is extremely stressful for a parent to watch their child battle a problem 24 hours a day for months or even years at a time. A parent’s instinct is to protect their child from problems that can take their joys in life and also affect their quality of life. Sleep deprivation for parents and the child is a big problem. The lack of sleep leads to absences form school, the child is unable to concentrate and unable to participate in class or in after school activities. Chronic scratching causes breaks in the skin creating open weeping sores and sometimes infection. Difficulty with how classmates and teachers relate to the child often occurs. The child develops a poor self image and has a lack of self confidence. Unable to participate in contact sports at school because of breaks in the skin that bleed, and the inability to hold a ball due to pain and chronic irritation of the skin. Other parents will NOT allow their children to play with a child with AD because they think the skin condition is contagious and they don’t want their children to touch them. Emotional Stress Emotional stress and anxiety can trigger a flare up. Stress can increase the sense of itching. Daily treatments can be stressful for the child and the parent. Medications may sting when applied to the inflamed skin causing pain and creating stress. This will affect compliance of treatments. Although it is very difficult to eliminate stress completely, it is extremely important to find ways to reduce stress. Reduce the stress Massage - in clinical research by Dr. Lawrence Schachner, Pediatric Dermatologist, University of Miami, massage therapy for 20 minutes a day has been proven to be effective in reducing stress and anxiety. and can improve the parent child relationship by creating a relaxed positive experience for both. Therapeutic drug interventions - may be necessary. Many doctors treat the skin condition but either don’t have the time to counsel parents properly about their appropriate application and really don’t see the emotional problems that can develop from AD for the parents as well as the child. Many parents blame themselves for their child’s inherited skin condition, and therefore, disciplining an AD child may be very difficult. Parents are worried that if they discipline their child, this will cause stress and cause itching which can start the cycle all over again. The child will then learn to manipulate the parents creating a dysfunctional relationship. Try to set limits and boundaries and try to keep the child’s ADL (activities of daily living) as normal as possible. These children usually have a poor self-image of themselves and a lack of self-confidence. As the child becomes older teach the importance of good skin care and prevention and encourage the child to get involved in the management of AD. It is extremely important for the doctor to address the emotional problems that develop and be empathetic to the parents and the child. This can lead to improvement in skin condition, the emotional well being of the child, and enable them to adjust better to social situations. Many children outgrow AD, however many continue to battle AD all through adulthood and will also have children with AD. For these adults, a lifetime of struggling with the disease, many suffer from low self esteem, psychological problems and deep emotional scars. © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 8 ________________________________________________________________________________________________ 5) What to do next? 5a) What to ask your physician about…. Allergy testing? Don’t just test for atopic allergens, look for contact allergens as well. The most common causes of contact allergy in children include: metals( E.G. nickel) pharmaceutical products (neomycin, corticosteroids, sulfonomides, emulsifiers and vehicle components) cosmetics toys rubber or latex items plastic materials plants Hazards of steroid overuse? Steroids in the samples given or the prescription products you are using? What potency is right for you? How long to use steroids SAFELY? Where on the body NOT to use steroids? ( i.e. diaper area ) Changes in diet with help of physician or a nutritional dietician that would strengthen the immune System? Protèque as a non-steroid approach to managing eczema? Protèque as a complementary steroid sparing approach used in combination with low potency corticosteroids to get the condition under control quickly? 5b) Survey -- Reasons physicians and consumers recommend non-steroid Proteque SPS Lotion. Treatments for eczema are constantly changing and research is ongoing. The following reasons are why are over 10,000 pediatricians, dermatologists, and family practitioners are recommending non-steroid Protèque SPS for patients (based on actual surveys with physicians who have used Protèque with patients)? According to Survey Results, the most important features of Protèque are: No Steroids Anti-pruritic (Stops Itch) Effective for relieving eczema or dermatitis symptoms quickly Non-irritating Cosmetically pleasing (not greasy) Inexpensive (about $5 per month) Water-resistant (15-20 washings) Safe for use on the face; diaper areas and groin where steroids are not allowed to be used for children Safe to use for prolonged periods of time for ongoing prevention and relief Can be used on any age infants and children without the dangers of topical steroids Can reduce colonization of Staph arueus on the skin and reduce the chance of spreading infection Affordable compared to more expensive prescription ointments Works for patients when other products have failed Use as a prevention as well as a relief © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 9 REFERENCES 1) Bernard A. Cohen M.D., Pediatric Dermatology, Second Edition, 1999 2) William L. Weston M.D., Alfred T. Lane M.D., Joseph G. Morelli M.D., Color Text Book of Pediatric Dermatology, Second Edition, 1996 3) Jeffery D. Bernhard, ITCH, Mechanisms and Management of Pruritis, 1994 4) “Atopic Dermatitis – Emotional Scars Are Deepest”, Dermatology Times, November 1999 5) “Atopic Dermatitis in Children”, National Eczema Association For Science and Education 6) “Prevalence of Pediatric Atopic Dermatitis Is Increasing”, Skin and Allergy News, October, 1999 7) “Compliance Suffers When Topical Drugs Sting” Skin and Allergy News, May 2000 8) “Test Atopic Children For Food Allergies”, Skin and Allergy News, May, 2000 9) “Look for Allergens in Kids’ Dermatitis”, Skin and Allergy News, Sept, 2000 © Protèque International 2001, Raleigh NC www.proteque.com 800-953-9250 page 10