For Lecture notes click here
advertisement

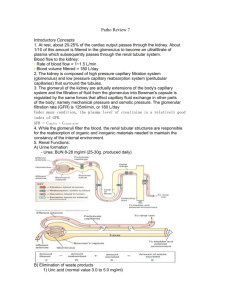
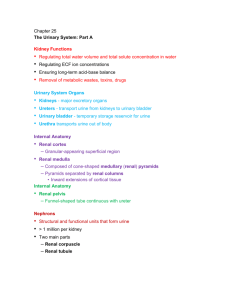
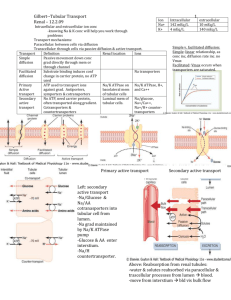
Introduction body contains trillions of cells bathed in extracellular fluid cells burn nutrients to obtain energy organic waste are removed by urinary system Urinary System Function 1. Regulating blood volume and blood pressure 2. Regulating plasma ions 3. Helping to stabilize blood pH 4. preventing nutrient excretion in 5. detoxifying poisons These activities regulated to keep composition of blood within limits The urinary system has two major functions: (1) excretion, performed by the two kidneys (produce urine). Urine leaving the kidneys travels along the urinary tract, which consists of paired tubes called ureters, to the urinary bladder, a muscular sac for temporary urine storage and from bladder, urine passes through the urethra, which conducts the urine to the exterior (2) elimination, urinary bladder and urethra are responsible for urine elimination, a process called urination The excretory functions of the urinary system are Kidneys: located on either side of the vertebral column, superior surface -adrenal gland shaped like a kidney bean; about 10 cm in length, 5.5 cm in width and weighs about 150 g hilus - point of entry exit for the renal arteries, vein and ureter. Each kidney is protected 3 layers of connective tissue: 1. The renal capsule, 2. The adipose capsule, 3. The renal fascia, The kidney itself has two layers: An outer cortex and an inner medulla cortex is reddish brown and granular medulla consists of 6 to 18 distinct conical called renal pyramids Each pyramid has a series of grooves renal pyramids are separated by cortical tissue called renal columns, renal lobe consists of a renal pyramid, the overlying area of renal cortex, and tissues of the renal columns. Urine production occurs in the renal lobes Ducts within each renal papilla discharge urine into minor calyx Four or five minor calyces merge to form a major calyx major calyces combine to form renal pelvis renal pelvis, is connected to the ureter Urine Production Urine production begins in nephrons Each kidney has 1.25 million nephrons, Blood Supply receive 20–25 percent of your total cardiac output 1200 ml of blood flows through kidneys each minute receives blood from a renal artery renal artery provides blood to the segmental arteries Segmental arteries divide into a series of interlobar arteries, interlobar arteries supply blood to the arcuate arteries, Each arcuate artery gives rise to a number of interlobular arteries interlobular artery branch to numerous afferent arterioles,(deliver blood to capillaries supplying individual nephrons) From capillaries of the nephrons, blood enters venules and small veins that converge on the interlobular veins interlobular veins deliver blood to arcuate veins, into interlobar veins into renal vein INNERVATION OF THE KIDNEYS kidneys and ureters are innervated by renal nerves The sympathetic innervation o adjusts rates of urine formation by changing blood flow and blood pressure at the nephron, o stimulates release of renin, which restricts losses of water and salt in urine by stimulating reabsorption at nephron THE NEPHRON lol consists of a renal tubule renal tubule - tubular passageway, begins at renal corpuscle renal corpuscle, contains a capillary network called the glomerulus, Blood arrives at glomerulus by way of an afferent arteriole and departs in an efferent arteriole In renal corpuscle, blood pressure forces fluid and dissolved solutes out of the glomerular capillaries and into the capsular space. This process is called filtration Filtration produces an essentially protein-free solution, known as a filtrate, From the renal corpuscle, filtrate enters the renal tubule. The renal tubule is responsible for: 1. Reabsorbing organic substrates. 2. Reabsorbing water 3. Secreting waste products The renal tubule has two segments—the proximal convoluted tubule (PCT) and the distal convoluted tubule (DCT separated by loop of Henle. tubular fluid(filtrate) gradually changes in composition as it moves Each nephron empties into the collecting system (tubes carry tubular fluid away from nephron) Collecting ducts receive fluid from many nephrons. Collecting duct carrying fluid to a papillary duct minor calyx. Nephrons from different locations differ slightly in structure 85 percent of all nephrons are cortical nephrons 15 percent of nephrons are juxtamedullary nephrons The Renal Corpuscle 150–250 µm in diameter. It includes capillary network of the glomerulus glomerulus is surrounded by Bowman’s capsule, The glomerular capillaries are fenestrated capillaries During filtration, blood pressure forces water and small solutes across this membrane into capsular space The larger solutes, are excluded Filtration at the renal corpuscle has one major limitation (glucose, free FA, AA, vitamins, and other solutes enter the capsular space) These materials are recaptured before filtrate leaves kidneys, The Proximal Convoluted Tubule the first segment of the renal tubule The lining of the PCT is a simple cuboidal epithelium with microvilli on the surface absorb organic nutrients, ions, water, and plasma proteins from the tubular fluid Reabsorption is the primary function of the PCT The Loop of Henle The PCT makes an acute bend that turns the renal tubule toward the renal medulla This turn leads to the loop of Henle, or nephron loop loop of Henle can be divided into a descending limb and an ascending limb Fluid in the descending limb travels toward the renal pelvis, and that in the ascending limb travels toward the renal cortex Each limb contains a thick segment and a thin segment. (The terms thick and thin refer to the height of the epithelium, not to the diameter of the lumen.) The thick descending limb has functions similar to those of the PCT: It pumps sodium and chloride ions out of the tubular fluid The thin segments are freely permeable to water but not to solutes The Distal Convoluted Tubule the third segment of the renal tubule begins as ascending loop of henle ends The initial portion of the DCT passes between the afferent and efferent arterioles DCT has a smaller diameter and its epithelial cells lack microvilli The DCT is an important site for: The active secretion of ions, acids, and other materials. The selective reabsorption of sodium ions and calcium ions from tubular fluid. The selective reabsorption of water, which assists in concentrating the tubular fluid. The Collecting System The distal convoluted tubule, the last segment of the nephron, opens into the collecting system The collecting system consists of collecting ducts and papillary ducts Several collecting ducts converge to empty into a larger papillary duct, which in turn empties into a minor calyx In addition to transporting tubular fluid from the nephron to the renal pelvis, the collecting system adjusts its composition and determines the final osmotic concentration and volume of urine. BASIC PRINCIPLES OF URINE FORMATION The goal of urine production is to maintain homeostasis by regulating the volume and composition of blood This process involves the excretion of solutes, specifically metabolic waste products organic waste products are: 1. Urea. Urea is the most abundant organic waste. You generate roughly 21 g of urea each day. Most of it is produced during the breakdown of amino acids. 2. Creatinine. Creatinine is generated in skeletal muscle tissue by the breakdown of creatine phosphate, a high-energy compound that plays an important role in muscle contraction. Your body generates roughly 1.8 g of creatinine each day, and virtually all of it is excreted in urine. 3. Uric acid. Uric acid is formed by the recycling of nitrogenous bases from RNA molecules. You produce approximately 480 mg of uric acid each day. kidneys ensure that the fluid that is lost does not contain potentially useful organic substrates, such as sugars or amino acids, that are contained in blood plasma To accomplish these goals, your kidneys rely on three distinct processes: 1. Filtration. blood pressure forces water across a filtration membrane at the renal corpuscle. 2. Reabsorption. is the removal of water and solutes from the filtrate, across the tubular epithelium, and into the peritubular fluid. Reabsorption occurs after filtrate has left the renal corpuscle. Most of the reabsorbed materials are nutrients that your body can use. Whereas filtration occurs solely on the basis of size, reabsorption is a selective process. Solute reabsorption may involve simple diffusion or the activity of carrier proteins in the tubular epithelium. The reabsorbed substances pass into the peritubular fluid and eventually reenter the blood. Water reabsorption occurs passively, through osmosis. 3. Secretion. Secretion is the transport of solutes from the peritubular fluid, across the tubular epithelium, and into the tubular fluid. Secretion is necessary because filtration does not force all the dissolved materials out of the plasma. Tubular secretion provides a backup for the filtration process that can further lower the plasma concentration of undesirable materials. Secretion can be the primary method of excretion for some compounds, including many drugs. All segments of the nephron and collecting system participate in the formation of urine. Filtration occurs exclusively in the renal corpuscle, across the filtration membrane. Nutrient reabsorption occurs primarily along the proximal convoluted tubules, but it also occurs elsewhere along the renal tubule and within the collecting system. Active secretion occurs primarily at the proximal and distal convoluted tubules. The loops of Henle, especially the long loops of the juxtamedullary nephrons, and the collecting system interact to regulate the final volume and solute concentration of the urine. FILTRATION occurs in the renal corpuscle The process of glomerular filtration involves passage across the filtration membrane. This membrane has three components: (1) the capillary endothelium, (2) the lamina densa, and (3) the filtration slits Glomerular capillaries are fenestrated capillaries with pores ranging from 60 to 100 nm These openings are small enough to prevent the passage of blood cells, but they are too large to restrict the diffusion of solutes, even those the size of plasma proteins The lamina densa is more selective; only small plasma proteins, nutrients, and ions can cross it filtration slits are the finest filters of all. The gaps are only 6–9 nm wide, which is small enough to block the passage of most small plasma proteins As a result, under normal circumstances no plasma proteins other than a few albumin molecules (average diameter 7 nm) can cross the filtration membrane and enter the capsular space Filtration Pressures the balance between hydrostatic pressure (fluid pressure) and colloid osmotic pressure (pressure due to materials in solution) on either side of the capillary walls. Hydrostatic Pressure The glomerular hydrostatic pressure (GHP) is the blood pressure in the glomerular capillaries. It tends to push water and solute molecules out of the plasma and into the filtrate. The GHP is significantly higher than capillary pressures elsewhere in the systemic circuit due to the arrangement of vessels at the glomerulus. Blood pressure is low in typical systemic capillaries, because capillary blood flows into the venous system, where resistance is relatively low. However, at the glomerulus, blood leaving the glomerular capillaries flows into an efferent arteriole, whose diameter is smaller than that of the afferent arteriole The efferent arteriole offers considerable resistance, so relatively high pressures are needed to force blood into it. As a result, glomerular pressures are similar to those of small arteries, averaging 45–55 mm Hg instead of the 35 mm Hg typical of peripheral capillaries. The net hydrostatic pressure (NHP) is the difference between glomerular hydrostatic pressure, which tries to push water and solutes out of the bloodstream, and capsular hydrostatic pressure, which tries to push water and solutes into the bloodstream. Colloid Osmotic Pressure The filtration pressure (FP) at the glomerulus is the difference between the hydrostatic pressure and the colloid osmotic pressure acting across the glomerular capillaries. Under normal circumstances, this relationship can be summarized as Glomerular Filtration Rate The glomerular filtration rate (GFR) is the amount of filtrate your kidneys produce each minute Each kidney contains about 6 m2 of filtration surface, and the GFR averages an astounding 125 ml per minute. This means that roughly 10 percent of the fluid delivered to your kidneys by the renal arteries leaves the bloodstream and enters the capsular spaces A creatinine clearance test is often used to estimate the GFR (Creatinine, which results from the breakdown of creatine phosphate in muscle tissue, is normally eliminated in urine. Creatinine enters the filtrate at the glomerulus, and it is not reabsorbed in significant amounts. By monitoring the creatinine concentrations in blood and the amount excreted in urine, a clinician can easily estimate the GFR) Controlling the GFR Glomerular filtration is the vital first step essential to all other kidney functions If filtration does not occur, waste products are not excreted, pH control is jeopardized, and an important mechanism of blood volume regulation is lost Three interacting levels of control stabilize your GFR: (1) autoregulation at the local level, (2) hormonal regulation initiated by the kidneys, and (3) autonomic regulation, primarily by the sympathetic division of the autonomic nervous system. Autoregulation of the GFR The goal of autoregulation is to maintain an adequate GFR despite changes in local blood pressure and blood flow This goal is accomplished by changing the diameters of the afferent arterioles, the efferent arterioles, and the glomerular capillaries A reduction in blood flow and a decline in glomerular blood pressure trigger (1) the dilation of the afferent arteriole, (2) the relaxation of supporting cells and the dilation of the glomerular capillaries, and (3) the constriction of the efferent arteriole Hormonal Regulation of the GFR The GFR is regulated by the hormones of the renin–angiotensin system and atrial natriuretic peptide (ANP) Renin is an enzyme released by the juxtaglomerular apparatus (JGA). This release occurs when (1) renal blood flow declines as a result of a decrease in blood volume, a fall in systemic pressures, or a blockage in the renal artery or its tributaries; or (2) the osmotic concentration of the tubular fluid that reaches the distal convoluted tubule decreases. In the renin–angiotensin system, renin converts the inactive protein angiotensinogen to angiotensin I, and the angiotensinconverting enzyme in the capillaries of the lungs then converts angiotensin I to the active form, angiotensin II. Figure 26-10 diagrams the primary effects of angiotensin II. These effects include the following: In peripheral capillary beds, angiotensin II causes a brief but powerful vasoconstriction of arterioles and precapillary sphincters, elevating pressures in the renal arteries and their tributaries. At the nephron, angiotensin II causes the constriction of the efferent arteriole, further elevating glomerular pressures and filtration rates. It also directly stimulates the reabsorption of sodium ions and water at the PCT. At the adrenal glands, angiotensin II stimulates the secretion of aldosterone by the adrenal cortex. The aldosterone accelerates sodium reabsorption in the DCT and cortical portion of the collecting system. In the CNS, angiotensin II (1) causes the sensation of thirst, (2) triggers the release of antidiuretic hormone (ADH), stimulating the reabsorption of water in the distal portion of the DCT and the collecting system, and (3) increases sympathetic motor tone, further stimulating peripheral vasoconstriction. Autonomic Regulation of the GFR Most of the autonomic innervation of the kidneys consists of sympathetic postganglionic fibers Sympathetic activation has one direct effect on the GFR: It produces a powerful vasoconstriction of the afferent arterioles, decreasing the GFR and slowing the production of filtrate The sympathetic activation triggered by an acute fall in blood pressure or a heart attack will override the local regulatory mechanisms that act to stabilize the GFR. As the crisis passes and sympathetic tone decreases, the filtration rate gradually returns to normal levels. REABSORPTION AND SECRETION Reabsorption and secretion at the kidneys involve a combination of diffusion, osmosis, and carrier-mediated transport. We have considered diffusion and osmosis in many chapters, so we shall pause now only for a brief review of carrier-mediated transport mechanisms. Carrier-Mediated Transport In previous chapters, we considered four major types of carrier-mediated transport: (1) facilitated diffusion, (2) active transport, (3) cotransport, and (4) countertransport. In facilitated diffusion, a carrier protein transports a molecule across the cell membrane without expending energy.The transport always follows the concentration gradient for the ion or molecule transported. Active transport is driven by the hydrolysis of ATP to ADP The Proximal Convoluted Tubule The cells of the proximal convoluted tubule normally reabsorb 60–70 percent of the volume of the filtrate produced in the renal corpuscle. The reabsorbed materials enter the peritubular fluid and diffuse into peritubular capillaries. The PCT has five major functions: 1. The reabsorption of organic nutrients. Under normal circumstances, before the tubular fluid enters the loop of Henle, the PCT reabsorbs more than 99 percent of the glucose, amino acids, and other organic nutrients.. 2. The active reabsorption of ions. The PCT actively transports ions, including sodium, potassium, magnesium, bicarbonate, phosphate, and sulfate ions. The ion pumps involved are individually regulated and may be influenced by circulating ion or hormone levels. For example, angiotensin II stimulates Na + reabsorption along the PCT. By absorbing carbon dioxide, the PCT indirectly recaptures roughly 90 percent of the bicarbonate ions from tubular fluid Bicarbonate is important in stabilizing blood pH, 3. The reabsorption of water. The reabsorptive processes have a direct effect on the solute concentrations inside and outside the tubules. The filtrate entering the PCT has the same osmotic concentration as that of surrounding peritubular fluid. As transport activities proceed, the solute concentration of tubular fluid decreases and that of peritubular fluid and adjacent capillaries increases. Osmosis then pulls water out of the tubular fluid and into the peritubular fluid. Along the PCT, this mechanism results in the reabsorption of roughly 108 liters of water each day. 4. The passive reabsorption of ions. As active reabsorption of ions occurs and water leaves tubular fluid by osmosis, the concentration of other solutes in tubular fluid increases above that in peritubular fluid. If the tubular cells are permeable to them, those solutes will move through passive diffusion across the tubular cells and into the peritubular fluid. Urea, chloride ions, and lipid-soluble materials may diffuse out of the PCT in this way. As this diffusion occurs, it further reduces the solute concentration of the tubular fluid and promotes additional water reabsorption by osmosis. 5. Secretion. Active secretion also occurs along the PCT. Because the DCT performs comparatively little reabsorption, we will consider secretory mechanisms when we discuss the DCT. The Loop of Henle and Countercurrent Exchange The loop of Henle will reabsorb roughly half of the water as well as two-thirds of the sodium and chloride ions remaining in the tubular fluid. Countercurrent refers to the fact that the exchange occurs between fluids moving in opposite directions The thin descending limb is permeable to water but relatively impermeable to solutes The thick ascending limb, which is relatively impermeable to both water and solutes, contains active transport mechanisms that pump sodium and chloride ions from the tubular fluid into the peritubular fluid of the medulla. Countercurrent multiplication operates as follows: Sodium and chloride are pumped out of the thick ascending limb and into the peritubular fluid. This pumping elevates the osmotic concentration in the peritubular fluid around the thin descending limb. The result is an osmotic flow of water out of the thin descending limb and into the peritubular fluid, increasing the solute concentration in the thin descending limb. The arrival of the highly concentrated solution in the thick ascending limb accelerates the transport of sodium and chloride ions into the peritubular fluid of the medulla. The Distal Convoluted Tubule The composition and volume of tubular fluid change dramatically as it travels from the capsular space to the distal convoluted tubule Only 15–20 percent of the initial filtrate volume reaches the DCT, and the concentrations of electrolytes and organic wastes in the arriving tubular fluid no longer resemble the concentrations in blood plasma Selective reabsorption or secretion, primarily along the DCT makes the final adjustments in the solute composition and volume of the tubular fluid. Throughout most of the DCT, the tubular cells actively transport Na + and Cl– out of the tubular fluid Tubular cells along the distal portions of the DCT also contain ion pumps that reabsorb tubular Na + in exchange for another cation (usually K+) The ion pump and the Na+ channels involved are controlled by the hormone aldosterone, produced by the adrenal cortex. The DCT is also the primary site of Ca2+ reabsorption. This process is regulated by circulating levels of parathyroid hormone and calcitriol The Collecting System The collecting ducts receive tubular fluid from many nephrons and carry it toward the renal sinus along the concentration gradient in the medulla The normal amount of water and solute loss in the collecting system is regulated in two ways: (1) by aldosterone, which controls sodium ion pumps along most of the DCT and the proximal portion of the collecting system; and (2) by ADH, which controls the permeability of the DCT and collecting system to water The collecting system also has other reabsorptive and secretory functions, many of which are important to the control of body fluid pH. Reabsorption Important examples of solute reabsorption in the collecting system include the following: Sodium ion reabsorption. The collecting system contains aldosterone-sensitive ion pumps that exchange Na+ in tubular fluid for K+ in peritubular fluid (Figure 26-13b ). Bicarbonate reabsorption. Bicarbonate ions are reabsorbed in exchange for chloride ions in the peritubular fluid (Figure 26-13c ). Urea reabsorption. The concentration of urea in the tubular fluid entering the collecting duct is relatively high. The fluid entering the papillary duct generally has the same osmotic concentration as that of interstitial fluid of the medulla—about 1200 mOsm/l—but contains a much higher concentration of urea. As a result, urea tends to diffuse out of the tubular fluid and into the peritubular fluid of the deepest portion of the medulla. Secretion The collecting system is an important site for the control of body fluid pH by means of the secretion of hydrogen or bicarbonate ions. The Control of Urine Volume and Osmotic Concentration Urine volume and osmotic concentration are regulated by controlling water reabsorption The volume of water lost in urine depends on how much of the water in the remaining tubular fluid (15 percent of the filtrate volume, or roughly 27 liters per day) is reabsorbed along the DCT and the collecting system THE FUNCTION OF THE VASA RECTA The solutes and water reabsorbed in the medulla must be returned to the general circulation without disrupting the concentration gradient This return is the function of the vasa recta SUMMARY: RENAL FUNCTION STEP 1: The filtrate produced at the renal corpuscle has the same osmotic concentration as does plasma, about 300 mOsm/l. It has the composition of blood plasma without the plasma proteins. STEP 2: In the PCT, the active removal of ions and organic substrates produces a continuous osmotic flow of water out of the tubular fluid. This process reduces the volume of filtrate but keeps the solutions inside and outside the tubule isotonic. Between 60 and 70 percent of the filtrate volume has been reabsorbed before the tubular fluid reaches the descending limb of the loop of Henle. STEP 3: In the PCT and descending limb of the loop of Henle, water moves into the surrounding peritubular fluids, leaving a small volume (15–20 percent of the original filtrate) of highly concentrated tubular fluid. The volume reduction has occurred by obligatory water reabsorption. STEP 4: The thick ascending limb is impermeable to water and solutes. The tubular cells actively transport Na + and Cl– out of the tubular fluid. This transport lowers the osmotic concentration of tubular fluid without affecting the volume of the tubular fluid. The tubular fluid reaching the distal convoluted tubule is hypotonic relative to the peritubular fluid, with an osmotic concentration of only about 100 mOsm/l. Because only Na+ and Cl– are removed, urea now accounts for a significantly higher proportion of the total osmotic concentration at the end of the loop than it did at the start. STEP 5: The final adjustments in the composition of the tubular fluid are made in the DCT and the collecting system. Although the DCT and collecting duct are generally impermeable to solutes, the osmotic concentration of tubular fluid can be adjusted through active transport (reabsorption or secretion). Some of these transport activities are hormonally regulated. STEP 6: The final adjustments in the volume and osmotic concentration of the tubular fluid are made by controlling the water permeabilities of the distal portions of the DCT and the collecting system. These segments are relatively impermeable to water unless exposed to ADH. Under maximum ADH stimulation, urine volume is at a minimum and urine osmotic concentration is equal to that of the peritubular fluid in the deepest portion of the medulla (roughly 1200 mOsm/l). STEP 7: The vasa recta absorbs solutes and water reabsorbed by the loop of Henle and the collecting ducts and thereby maintains the concentration gradient of the medulla. THE COMPOSITION OF NORMAL URINE More than 99 percent of the 180 liters of filtrate produced each day by the glomeruli is reabsorbed and never reaches the renal pelvis The composition and concentration of urine are two integrated but distinct properties The composition of urine reflects the filtration, absorption, and secretion activities of the nephrons Some compounds, such as urea, are neither actively excreted nor reabsorbed along the nephron. In contrast, organic nutrients are completely reabsorbed, and other compounds, such as creatinine, that are missed by the filtration process are actively secreted into tubular fluid. Urinary transport, storage Filtrate modification and urine production end when the fluid enters the renal pelvis The urinary tract (the ureters, urinary bladder, and urethra) is responsible for the transport, storage, and elimination of urine. THE URETERS The ureters are a pair of muscular tubes that extend from the kidneys to the urinary bladder—a distance of about 30 cm Each ureter begins at the funnel-shaped renal pelvis (Figure 26-4 ). The ureters extend inferiorly and medially, passing over the anterior surfaces of the psoas major muscles (Figures 26-2b and 26-3 ). The ureters are retroperitoneal and are firmly attached to the posterior abdominal wall. The paths taken by the ureters in men and women are different due to variations in the nature, size, and position of the reproductive organs. As Figure 26-18a shows, in males, the base of the urinary bladder lies between the rectum and the pubic symphysis; in females, the base of the urinary bladder sits inferior to the uterus and anterior to the vagina (Figure 26-18b ). THE URINARY BLADDER The urinary bladder is a hollow, muscular organ that functions as a temporary storage reservoir for urine (Figure 26-18c ). The dimensions of the urinary bladder vary with the state of distension, but the full urinary bladder can contain about a liter of urine. THE URETHRA The urethra extends from the neck of the urinary bladder to the exterior. The urethrae of males and females differ in length and in function. In males, the urethra extends from the neck of the urinary bladder to the tip of the penis, a distance that may be 18–20 cm (7–8 in.). The male urethra can be subdivided into three portions (Figure 26-18a ,c ): (1) the prostatic urethra, (2) the membranous urethra, and (3) the penile urethra. Aging In general, aging is associated with an increased incidence of kidney problems. We described examples, such as nephrolithiasis— the formation of calculi, or kidney stones—earlier in the chapter. Other age-related changes in the urinary system include: A decline in the number of functional nephrons. The total number of kidney nephrons drops by 30–40 percent between ages 25 and 85. A reduction of the GFR. This reduction results from decreased numbers of glomeruli, cumulative damage to the filtration apparatus in the remaining glomeruli, and reductions in renal blood flow. A reduced sensitivity to ADH. With age, the distal portions of the nephron and collecting system become less responsive to ADH. Less reabsorption of water and sodium ions occurs, and more sodium ions are lost in urine. Problems with the micturition reflex. The following three factors are involved in such problems: 1. The sphincter muscles lose muscle tone and become less effective at voluntarily retaining urine. Incontinence results, commonly involving a slow leakage of urine. 2. The ability to control micturition can be lost after a stroke, Alzheimer’s disease, or other CNS problems affecting the cerebral cortex or hypothalamus. 3. In males, urinary retention may develop secondary to enlargement of the prostate gland (prostatic hypertrophy). In this condition, swelling and distortion of surrounding prostatic tissues compress the urethra, restricting or preventing the flow of urine.