North Florida Community College
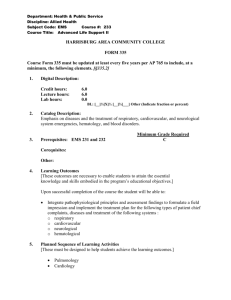
advertisement

North Florida Community College 2009 EMT Syllabus Lead Instructor: Albert “Mac” Leggett Phone: (850) 973-1673 Fax: (850) 973-1678 Email: Leggetta@nfcc.edu Office location: Building 13, Room 127 Medical Director: Dr. Robert Spindell Americans with Disabilities Act: NFCC is dedicated to the concept of equal opportunity. Students wishing modifications in class or on campus due to a disability may choose to inform the instructor at the beginning of the semester or contact the Office of Student Disability directly. Accommodations and modifications will be made after the student registers with the Office for Student Disability Services and provides appropriate documentation of the disability. After the accommodation is evaluated, the instructor may be involved in providing accommodations in order to equalize the educational experience. Please call 973-9484 (V); 973-1682 (V); or 973-9611 (TTY) for information. Course Description: EMS 1119- Emergency Medical Technician (180 hours- 6 credit hours) Pre-requisite Current American Heart Association CPR for Healthcare Providers Card College Placement Test scores must be approved by the Program Coordinator prior to acceptance into the program, achieving a minimum of: Reading= 71 Sentence Skills= 68 Arithmetic= 42 The TABE with 10 grade equivalency may be substituted for the CPT Co-requisite EMS 1119L- Emergency Medical Technician Lab (90 hours; 3 credit hours) EMS 1411- Emergency Room Clinicals (30 hours; 1 credit hour) EMS 1421- Rescue Clinicals (30 hours; 1 credit hour) Total: 330 hours; 11 credit hours *All co-requisites must be completed at the completion of the semester. Courses required for graduation: The following are mandatory attendance for graduation: Trauma Scorecard Methodology: 2 hours HIV/AIDS Training: 4 hours SIDS Training Any student who misses any of the above lectures will be responsible for finding a course which provides these lectures and bring proof of attendance prior to being eligible for graduation. Course Description: The Emergency Medical Technician- Basic (EMT-B) course is the entry level into the Emergency Medical Services career field. The NFCC EMT-B program follows the most current United States Department of Transportation (USDOT) National Standard Curriculum for EMT-B. This program trains students to work in the prehospital emergency medical environment as an entry level EMT-B provider. Purpose: This prehospital training course provides lectures and skills practice required for entry level practitioners. This course provides classroom, clinical, ambulance, as well as the emergency department in the hospital, to train for the management of medical and trauma patients at the basic life support level. Graduates of the program will be eligible to take the State of Florida Certification Exam. Completion of this program does not guarantee State Certification or employment. Course Textbooks: Required Texts: Emergency Care 11th Edition, Limmer, O’Keefe Recommended texts: Emergency Care 11th Edition Workbook, Limmer, O’Keefe Course Design- Each lesson for this course has: An introduction Lecture Discussion or group work requirements that include brief classroom presentation Skills practice and testing DOT Objectives include: Chapter 1: 1. 2. 3. 4. Define Emergency Medical Services (EMS) systems. (pp. 6-8) Differentiate the roles and responsibilities of the EMT-Basic from other prehospital care providers. (pp. 10) Describe the roles and responsibilities related to personal safety. (pp 10) Discuss the roles and responsibilities of the EMT-Basic towards the safety of the crew, the patient, and bystanders. (pp. 10) 5. 6. 7. 8. 9. Define quality improvement and discuss the EMT-Basic’s role in the process. (pp 14-15) Define medical direction, and discuss the EMT-Basic’s role in the process. (pp. 1516) State the specific statutes and regulations in your state regarding the EMS system. (pp. 16) Assess areas of personal attitude and conduct of the EMT-Basic. (pp. 12) Characterize the various methods used to access the EMS System in your community. (pp. 9) Chapter 2: 1. List the possible emotional reactions that the EMT-Basic may experience when faced with trauma, illness, death, and dying. (pp. 30-33) 2. Discuss the possible reactions that a family member may exhibit when confronted with death and dying. (pp. 34-35) 3. State the steps in the EMT-Basic’s approach to the family confronted with death and dying. (pp. 35) 4. State the possible reactions that the family of the EMT-Basic may exhibit due to their outside involvement. (pp. 33) 5. Recognize the signs and symptoms of critical incident stress. (pp. 30-33) 6. State possible steps the EMT-Basic may take to help reduce or alleviate stress. (pp. 33-34) 7. Explain the need to determine scene safety. (pp. 35-37) 8. Discuss the importance of body substance isolation. (pp. 22-23) 9. Describe the steps the EMT-Basic should take for personal protection from airborne and bloodborne pathogens. (pp. 22-30) 10. List the personal protective equipment necessary for each of the following situations: (pp. 23-30; 35-40) Hazardous materials Rescue operations Violent scenes Crime scenes Exposure to bloodborne pathogens Exposure to airborne pathogens 11. Explain the rationale for serving as an advocate for the use of appropriate equipment. (pp. 24) Skills 1. 2. Given a scenario with potential infectious exposure, the EMT-Basic will use appropriate personal protective equipment. At the completion of the scenario, the EMT-Basic will properly remove and discard the protective garments. Given the above scenario, the EMT-Basic will complete disinfection/cleaning and all reporting/documentation. Chapter 3: 1. 2. 3. 4. 5. 6. 7. Define the EMT-Basic scope of practice. (pp. 45) Discuss the importance of “Do Not Resuscitate” (DNR) orders (Advance Directives) and local or state provisions regarding EMS application. (pp. 49-50) Define consent and discuss the methods of obtaining consent. (pp. 45-46) Differentiate between expressed and implied consent. (pp. 46) Explain the role of consent of minors in providing care. (pp. 46) Discuss the implications for the EMT-Basic in patient refusal of transport. (pp. 4648) Discuss the issues of abandonment, negligence, and battery and their implications to the EMT-Basic. (pp. 47; 50-51) 8. 9. 10. 11. 12. 13. 14. 15. State the conditions necessary for the EMT-Basic to have a duty to act. (pp. 51) Explain the importance, necessity, and legality of patient confidentiality. (pp. 51-52) Discuss the considerations of the EMT-Basic in issues or organ retrieval. (pp. 52-53) Differentiate the actions that an EMT-Basic should take to assist in the preservation of a crime scene. (pp. 53; 55) State the conditions that require an EMT-Basic to notify local law enforcement officials. (pp. 55) Explain the role of EMS and the EMT-Basic regarding patients with DNR orders. (pp. 49-50) Explain the rationale for the needs, benefits, and usage of advance directives. (pp. 49-50) Explain the rationale for the concept of varying degrees of DNR. (pp. 49-50) Chapter 4: 1. 2. Identify the following topographic terms: medical, lateral, proximal, distal, superior, inferior, anterior, posterior, midline, right and left, mid-clavicular, bilateral, midaxillary. (pp. 61-63) Describe the anatomy and function of the following major body systems: respiratory (pp. 69-71), circulatory (pp. 71-76), musculoskeletal (pp. 65-69), nervous (pp. 7678), endocrine (pp. 80-81). (Scan 4-1, pp. 82-90; Scan 4-2, pp. 91-92) Chapter 5: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Define body mechanics. (pp. 101) Discuss the guidelines and safety precautions that need to be followed when lifting a patient. (pp. 101-103) Describe the safe lifting of cots and stretchers. (pp. 107-109; 115) Describe the guidelines and safety precautions for carrying patients and/or equipment. (pp. 101-103) Discuss one-handed carrying techniques. (pp. 101) Describe the correct and safe carrying procedures on stairs. (pp. 109) State the guidelines for reaching and their application. (pp. 102) Describe correct reaching for log rolls. ( pp. 106-107) State the guidelines for pushing and pulling. (pp. 102-103) Discuss the general considerations for moving patients. (pp. 101-103) State three situations that may require the use of an emergency move. (pp. 103) (Scan 5-1, pp. 104; Scan 5-2, pp. 105; Scan 5-3, pp. 106) Identify the following patient carrying devices: (Scan 5-4, pp. 108; Scan 5-5, pp. 110-111; Scan 5-6, pp. 112-114) wheeled ambulance stretcher portable ambulance stretcher stair chair scoop stretcher long spine board basket stretcher flexible stretcher Explain the rationale for properly lifting and moving patients. (pp. 101) (Scan 5-7, pp. 116-118; Scan 5-8, pp. 120) Skills 1. Working with a partner, prepare each of the following devices for use, transfer a patient to device, properly position the patient on the device, move the device to the ambulance, and load the patient into the ambulance: wheeled ambulance stretcher portable ambulance stretcher stair chair 2. scoop stretcher long spine board basket stretcher flexible stretcher Working with a partner, the EMT-Basic will demonstrate techniques for the transfer of a patient from an ambulance stretcher to a hospital stretcher. Chapter 6: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. Name and label the major structures of the respiratory system on a diagram. (pp. 128-129) List the signs of adequate breathing. (pp. 130-133) List the signs of inadequate breathing. (pp. 129-133) Describe the steps in performing the head-tilt, chin-lift. (pp. 135) Relate the mechanism of injury to opening the airway. (pp. 133-136) Describe the steps in performing the jaw thrust. (pp. 136) State the importance of having a suction unit ready for immediate use when providing emergency care. (pp. 151) Describe the techniques of suctioning. (pp. 153, 155) (Scan 6-4, 99. 154) Describe how the artificially ventilate a patient with a pocket mask. (pp. 138-140) Describe the steps in performing the skill of artificially ventilating a patient with a bag-valve mask while using the jaw thrust. (pp. 141-143) List the parts of a bag-valve mask system. (pp. 140) Describe the steps in performing the skill of artificially ventilating a patient with a bag-valve mask for one and two rescuers. (pp. 141-143) Describe the signs of adequate artificial ventilation using the bag-valve mask. (pp. 137) Describe the signs of inadequate artificial ventilation using the bag-valve mask. (pp. 137) Describe the steps in artificially ventilating a patient with a flow-restricted, oxygenpowered ventilation device. (pp. 144-145) List the steps in performing the actions taken when providing mouth-to-mouth and mouth-to stoma artificial ventilation. (pp. 137; 145) Describe how to measure and insert an oropharyngeal (oral) airway. (pp. 146-147) (Scan 6-2, pp. 148-149) Describe how to measure and insert a nasopharyngeal (nasal) airway. (pp. 147-148) (Scan 6-3, pp. 150) Define the components of an oxygen delivery system. (pp. 156-160) (Scan 6-6, pp. 164-166) Identify a nonrebreather face mask and state the oxygen flow requirements needed for its use. (pp. 167-168) Describe the indications for using a nasal cannula versus a nonrebreather face mask. (pp. 167-168) Identify a nasal cannula and state the flow requirements needed for its use. (pp. 167168) Explain the rationale for basic life support artificial ventilation and airway protective skills taking priority over most other basic life support skills. (pp. 128) Explain the rationale for providing adequate oxygenation through high inspired oxygen concentrations to patients who, in the past, may have received low concentrations. (pp. 161) Skills 1. 2. 3. 4. Demonstrate the steps in performing the head-tilt, chin-lift. Demonstrate the steps in performing the jaw thrust. Demonstrate the techniques of suctioning. Demonstrate the steps in providing mouth-to-mouth artificial ventilation with body substance isolation (barrier shields). 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. Demonstrate how to use a pocket mask to artificially ventilate a patient. Demonstrate the assembly of a bag-valve mask unit. Demonstrate the steps in performing the skill of artificially ventilating a patient with a bag-valve mask for one and two rescuers. Demonstrate the steps in performing the skill of artificially ventilating a patient with a bag-valve mask while using the jaw thrust. Demonstrate artificial ventilation of a patient with a flow-restricted, oxygen-powered ventilation device. Demonstrate how to artificially ventilate a patient with a stoma. Demonstrate how to insert an oro-pharyngeal (oral) airway. Demonstrate how to insert a nasopharyngeal (nasal) airway. Demonstrate the correct operation of oxygen tanks and regulators. Demonstrate the use of a nonrebreather face mask and state the oxygen flow requirements needed for its use. Demonstrate the use of a nasal cannula and state the flow requirements for its use. Demonstrate how to artificially ventilate the infant and child patient. Demonstrate oxygen administration for the infant and child patient. Chapter 7: 1. 2. 3. 4. 5. 6. 7. 8. Recognize hazards or potential hazards. (pp. 178-181) (Scan 7-1, pp. 179) Describe common hazards found at the scene of a trauma and a medical patient. (pp 178-181) (Scan 7-2, pp. 182) Determine if the scene is safe to enter. (pp. 180-181; 183-184) Discuss common mechanisms of injury or nature of illness. (pp. 184-191) (Scan 7-3, pp. 185) Discuss the reason for identifying the total number of patients at the scene. (pp. 191) Explain the reason for identifying the need for additional help or assistance. (pp. 191) Explain the rationale for crew members to evaluate scene safety prior to entering. (pp. 178) Serve as a model for others, explaining how patient situations affect your evaluation of mechanism of injury or illness. (pp. 184-191) Skills 1. Observe various scenarios and identify potential hazards. Chapter 8: 1. Summarize the reasons for forming a general impression of the patient. (pp. 196; 200) 2. Discuss methods of assessing altered mental status. (pp. 200-202) 3. Differentiate between assessing the altered mental status in the adult, child, and infant patient. (pp. 200; 202; 205; 207) 4. Discuss the methods of assessing the airway in the adult, child and infant patient. (pp. 200; 202; 205; 207) 5. State reasons for management of the cervical spine once the patient has been determined to be a trauma patient. (pp. 196; 200) (Scan 8-1, pp. 197) 6. Describe methods used for assessing if a patient is breathing. (pp. 200-202; 207) 7. State what care should be provided to the adult, child and infant patient with adequate breathing. (pp. 198; 200-202; 207) 8. State what care should be provided to the adult, child or infant patient without adequate breathing. (pp. 198; 200-202; 207) 9. Differentiate between a patient with adequate and inadequate breathing. (pp. 200202) 10. Distinguish between methods of assessing breathing in the adult, child and infant patient. (pp. 200-202; 205; 207) 11. Compare the methods of providing airway care to the adult, child and infant patient. (pp. 198; 200; 202; 205; 207) 12. Describe the methods used to obtain a pulse. (pp. 201-202; 207) 13. Differentiate between obtaining a pulse in an adult, child and infant patient. (pp. 201-202; 205; 207) 14. For further information on these objectives… Objectives 3-2.4, 6, 7, 8, 9, 10, 11 (airway, breathing) Objectives 3-2.12, 13 (pulse) Objective (external bleeding) Objectives 3-2.15, 16, 17, 18 (skin/shock) Objectives 3-2.3, 4, 7, 8, 10, 11, 13, 18 (infants/children) 15. Discuss the need for assessing the patient for external bleeding. (pp. 201-202; 207) 16. Describe normal and abnormal findings when assessing skin color. (pp. 201-202; 207) 17. Describe normal and abnormal findings when assessing skin temperature. (pp. 201202; 207) 18. Describe normal and abnormal findings when assessing skin condition. (pp. 201202; 207) 19. Describe normal and abnormal findings when assessing skin capillary refill in the infant and child patient. (pp. 199; 202; 205; 207) 20. Explain the reason for prioritizing a patient for care and transport. (pp. 201) 21. Explain the importance of forming a general impression of the patient. (pp. 194; 196) 22. Explain the value of performing an initial assessment. (pp. 196) (Scan 8-2, pp. 198199) Skills 1. 2. 3. 4. 5. 6. Demonstrate the techniques for assessing mental status. Demonstrate the techniques for assessing the airway. Demonstrate the techniques for assessing if the patient is breathing. Demonstrate the techniques for assessing if the patient has a pulse. Demonstrate the techniques for assessing the patient for external bleeding. Demonstrate the techniques for assessing the patient’s skin color, temperature, condition, and capillary refill (infants and children only). 7. Demonstrate the ability to prioritize patients. See these chapters: Chapter 6, “Airway Management” Chapter 9, “Vital Signs and SAMPLE History” Chapter 26, “Bleeding and Shock” Chapter 9, “Vital Signs and SAMPLE History”, Chapter 26, “Bleeding and Shock” Chapter 31, “Infants and Children” Chapter 9: 1. 2. 3. Identify the components of vital signs. (pp. 212) Describe the methods used to obtain a breathing rate. (pp. 215) Identify the attributes that should be obtained when assessing breathing. (pp. 215-216) 4. Differentiate between shallow, labored, and noisy breathing. (pp. 216) 5. Describe the methods to obtain a pulse rate. (pp. 213) 6. Identify the information obtained when assessing a patient’s pulse. (pp. 213-215) 7. Differentiate between a strong, weak, regular, and irregular pulse. (pp. 213-214) 8. Describe the methods used to assess the skin color, temperature, and condition (capillary refill in infants and children). (216-218) 9. Identify the normal and abnormal skin colors. (pp. 216-217) 10. Differentiate between pale, blue, red, and yellow skin color. (pp. 216-217) 11. Identify the normal and abnormal skin temperature. (pp. 217) 12. 13. 14. 15. 16. 17. Differentiate between hot, cool, and cold skin temperature. (pp. 217) Identify normal and abnormal skin condition. (pp. 217-218) Identify normal and abnormal capillary refill in infants and children. (pp. 218) Describe the methods used to assess the pupils. (pp. 218-219) Identify normal and abnormal pupil size. (pp. 218-219) Differentiate between dilated (large) and constricted (small) pupil size. (pp. 218219) 18. Differentiate between reactive and nonreactive pupils and equal and unequal pupils. (pp. 218-219) 19. Describe the methods used to assess blood pressure. (pp. 220-221) 20. Define systolic pressure. (pp. 218-219) 21. Define diastolic pressure. (pp. 219) 22. Explain the difference between auscultation and palpation for obtaining a blood pressure. (pp. 220-221) 23. Identify the components of the SAMPLE history. (pp. 224) 24. Differentiate between a sign and a symptom. (pp. 224) 25. State the importance of accurately reporting and recording the baseline vital signs. (pp. 213) 26. Discuss the need to search for additional medical identification. (pp. 2240 27. Explain the value of performing the baseline vital signs. (pp. 213) 28. Recognize and respond to the feelings patients experience during assessment. (pp. 225) 29. Defend the need for obtaining and recording an accurate set of vital signs. (pp. 213) 30. Explain the rationale of recording additional sets of vital signs. (pp. 212-213; 221) 31. Explain the importance of obtaining a SAMPLE history. (pp. 224-225) Skills 1. 2. 3. Demonstrate the skills involved in assessment of breathing. Demonstrate the skills associated with obtaining a pulse. Demonstrate the skills associated with assessing the skin color, temperature, condition, and capillary refill in infants and children. 4. Demonstrate the skills associated with assessing the pupils. 5. Demonstrate the skills associated with obtaining blood pressure. 6. Demonstrate the skills that should be used to obtain information from the patient, family, or bystanders at the scene. Chapter 10: 1. Discuss the reasons for reconsideration concerning the mechanism of injury. (pp. 233; 245) 2. State the reasons for performing a rapid trauma assessment. (pp. 246-247) 3. Recite examples and explain why patients should receive a rapid trauma assessment. (pp. 246-247) 4. Describe the areas included in the rapid trauma assessment and discuss what should be evaluated. (pp. 246-253) (Scan 10-1, pp. 234-235; Scan 10-3, pp. 242-244; Scan 10-4, pp. 249; Scan 10-5, pp. 250-252) 5. Differentiate when the rapid assessment may be altered in order to provide patient care. (pp. 246-247; 253-254) 6. Discuss the reason for performing a focused history and physical exam. (pp. 232) 7. Recognize and respect the feelings that patients might experience during assessment. (pp. 235; 237; 248; 253) 8. Discuss the components of the detailed physical exam. (pp. 254-255; 258-261) (Scan 10-6, pp. 255-258) 9. State the areas of the body that are evaluated during the detailed physical exam. (pp. 254) 10. Explain what additional care should be provided while performing the detailed physical exam. (pp. 254-255; 258-261) 11. Distinguish between the detailed physical exam that is performed on a trauma patient and that of the medical patient. (pp. 261) 12. Explain the rationale for the feelings that these patients might be experiencing. (pp. 235; 237; 248; 253) Skills 1. Demonstrate the rapid trauma assessment that should be used to treat a patient based on mechanism of injury6. 2. Demonstrate the skills involved in performing the detailed physical exam. Chapter 11: 1. Describe the unique needs for assessing an individual with a specific chief complaint with no known prior history. (pp. 275) 2. Differentiate between the history and physical exam that is performed for responsive patients with no known prior history and responsive patients with a known prior history. (pp. 274-275) (Scan 11-1, pp. 272-273) 3. Describe the needs for assessing an individual who is unresponsive. (pp. 274; 277279) (Scan 11-2, pp. 276-277) 4. Differentiate between the assessment that is performed for a patient who is unresponsive or has an altered mental status and other medical patients requiring assessment. (pp. 274) 5. Attend to the feelings that these patients might be experiencing. (pp. 269; 271; 275) Skills 1. Demonstrate the patient assessment skills that should be used to assist a patient who is responsive with no known history. 2. Demonstrate the patient assessment skills that should be used to assist a patient who is unresponsive or has an altered mental status. Chapter 12: 1. Discuss the reasons for repeating the initial assessment as part of the ongoing assessment. (pp. 289) 2. Describe the components of the ongoing assessment. (pp. 289-290) (Scan 12-1, pp. 288-289) 3. Describe trending of assessment components. (pp. 286; 289-291) 4. Explain the value of performing an ongoing assessment. (pp. 286; 288) 5. Recognize and respect the feelings that patients might experience during assessment. (pp. 288) 6. Explain the value of trending assessment components to other health professionals who assume care of the patient. (pp. 291) Skills 1. Demonstrate the skills involved in performing the ongoing assessment. Chapter 13: 1. 2. 3. List the proper methods of initiating and terminating a radio call. (pp. 300-301) State the proper sequence for delivery of patient information. (pp. 302) Explain the importance of effective communication of patient information in the verbal report. (pp. 303) 4. Identify the essential components of the verbal report. (pp. 303) 5. Describe the attributes for increasing effectiveness and efficiency of verbal communications. (pp. 303-305) 6. State legal aspects to consider in verbal communication. (pp. 299-300) 7. Discuss the communications skills that should be used to interact with the patient. (pp. 303-305) 8. Discuss the communication skills that should be used to interact with the family, bystanders, and individuals from other agencies while providing patient care, and the difference between skills used to interact with the patient and those used to interact with others. (pp. 303-305) 9. List the correct radio procedures in the following phases of a typical call: To the scene At the scene To the facility To the station At the station 10. Explain the rationale for providing efficient and effective radio communications and patient reports. (pp. 298; 301-303) Skills 1. Perform a simulated, organized, concise radio transmission. 2. Perform an organized, concise patient report that would be given to the staff at a receiving facility. 3. Perform a brief, organized report that would be given to an ALS provider arriving at the scene at which the EMT-B was already providing care. Chapter 14: 1. Explain the components of the written report and list the information that should be included in the written report. (pp. 314-318) 2. Identify the various sections of the written report. (pp. 214-318) 3. Describe what information is required in each section of the prehospital care report and how it should be entered. (pp. 314-318) 4. Define the special considerations concerning patient refusal. (pp. 318-319) 5. Describe the legal implications associated with the written report. (pp. 310; 313; 318-322) 6. Discuss all state and/or local record and reporting requirements. (pp. 323) 7. Explain the rationale for patient care documentation. (pp. 310, 313-314) 8. Explain the rationale for the EMS system gathering data. (pp. 310; 313-314) 9. Explain the rationale for using medical terminology correctly. (pp. 318) 10. Explain the rationale for using an accurate and synchronous clock so that information can be used in trending. (pp. 315) Skills 1. Complete a prehospital report. Chapter 15: 1. 2. 3. Identify which medications will be carried on the unit. (pp. 332-333) State the medications carried on the unit by the generic name. (pp. 332-333) Identify the medications which the EMT-Basic may assist the patient with administering. (pp. 333-335) 4. State the medications the EMT-Basic can assist the patient with by the generic name. (pp. 333-335) 5. Discuss the forms in which the medications may be found. (pp. 336) 6. Explain the rationale for the administration of medications. (pp. 332-336) Skills 1. Demonstrate general steps for assisting patient with self-administration of medications. 2. Read the labels and inspect each type of medication. Chapter 16: 1. List the structure and function of the respiratory system. (pp. 344-345) 2. State the signs and symptoms of a patient with breathing difficulty. (pp. 345-347; 349-350) 3. Describe the emergency medical care of the patient with breathing difficulty. (pp. 346-348; 350-351) 4. Recognize the need for medical direction to assist in the emergency medical care of a patient with breathing difficulty. (pp. 351; 354) 5. Describe the emergency medical care of the patient with breathing distress. (pp. 346348; 350-351) 6. Establish the relationship between airway management and the patient with breathing difficulty. (pp. 346; 348; 350) 7. List signs of adequate air exchange. (pp. 346) 8. State the generic name, medication forms, dose, administration, action, indications, and contraindications for the prescribed inhaler. (pp. 354) (Scan 16-1, pp. 355-356; Scan 16-2, pp. 357) 9. Distinguish between the emergency medical care of an infant, child, and adult patient with breathing difficulty. (pp. 346; 348) 10. Differentiate between upper airway obstruction and lower airway disease in the infant and child patient. (pp. 348) 11. Defend EMT-Basic treatment regimens for various respiratory emergencies. (pp. 346-348; 350-351) 12. Explain the rationale for administering an inhaler. (pp. 354) Skills 1. Demonstrate the emergency medical care for breathing difficulty. 2. Perform the steps in facilitating the use of an inhaler. Chapter 17: 1. 2. Describe the structure and function of the cardiovascular system. (pp. 367) Describe the emergency medical care of the patient experiencing chest pain or discomfort. (pp. 369; 372) (Scan 17-1, pp. 370-371) 3. List the indications for automated external defibrillation (AED). (pp. 380-381; 384-385; 388; 390) 4. List the contraindications for automated external defibrillation. (pp. 393-394) 5. Define the role of EMT-B in the emergency cardiac care system. (pp. 369-372; 378-381; 392) 6. Explain the impact of age and weight on defibrillation. (pp. 388) 7. Discuss the position of comfort for patients with various cardiac emergencies. (pp. 369) 8. Establish the relationship between airway management and the patient with cardiovascular compromise. (pp. 372; 392) 9. Predict the relationship between the patient experiencing cardiovascular compromise and basic life support. (pp. 378-380; 385; 388; 391) 10. Discuss the fundamentals of early defibrillation. (pp. 380) 11. Explain the rationale for early defibrillation. (pp. 378; 380) 12. Explain that not all chest pain patients result in cardiac arrest and do not need to be attached to an automated external defibrillator. (pp. 367-372) 13. Explain the importance of prehospital ACLS intervention if it is available. (pp. 380381; 392) 14. Explain the importance of urgent transport to a facility with advanced cardiac life support if it is not available in the prehospital setting. (pp. 380-381) 15. Discuss the various types of automated external defibrillators. (pp. 381-382) 16. Differentiate between the fully automated and the semiautomated defibrillator. (pp. 383-384; 396) 17. Discuss the procedures that must be taken into consideration for standard operations of the various types of automated external defibrillators. (pp. 385-399) 18. State the reasons for assuring that the patient is pulseless and apneic when using the automated external defibrillator. (pp. 383) 19. Discuss the circumstances which may result in inappropriate shocks. (pp. 383) 20. Explain the considerations for interruption of CPR when using the automated external defibrillator. (pp. 384) 21. Discuss the advantages and disadvantages of automated external defibrillators. (pp. 397) 22. Summarize the speed of operation of automated external defibrillation. (pp. 397399) 23. Discuss the use of remote defibrillation through adhesive pads. (pp. 397) 24. Discuss the special considerations for rhythm monitoring. (pp. 383-384; 397) 25. List the steps in the operation of the automated external defibrillator. (pp. 388-391) (Scan 17-4, pp. 386-388) 26. Discuss the standard of care that should be used to provide care to a patient with persistent ventricular fibrillation and no available ACLS. (pp. 383; 385-394) 27. Discuss the standard of care that should be used to provide care to a patient with recurrent ventricular fibrillation and no available ACLS. (pp. 393) 28. Differentiate between single rescuer and multi-rescuer care with an automated external defibrillator. (pp. 392) 29. Explain the reason for pulses not being checked between shocks with an automated external defibrillator. (pp. 392) 30. Discuss the importance of coordinating ACLS trained providers with personnel using automated external defibrillators. (pp. 392) 31. Discuss the importance of post-resuscitation care. (pp. 392) 32. List the components of post-resuscitation care. (pp. 392) 33. Explain the importance of frequent practice with the automated external defibrillator. (pp. 383; 399) 34. Discuss the need to complete the Automated Defibrillator: Operator’s Shift Checklist. (pp. 399) 35. Discuss the role of the American Heart Association (AHA) in the use of automated external defibrillation. (pp. 378-381) 36. Explain the role medical direction plays in the use of automated external defibrillation. (pp. 399) 37. State the reasons why a case review should be completed following the use of the automated external defibrillator. (pp. 399-400) 38. Discuss the components that should be included in a case review. (pp. 399-400) 39. Discuss the goal of quality improvement in automated external defibrillation. (pp. 399-400) 40. Recognize the need for medical direction of protocols to assist in the emergency medical care of the patient with chest pain. (pp. 370; 372) 41. List the indications for the use of nitroglycerin. (pp. pp. 372) (Scan 17-2, pp. 373) 42. State the contraindications and side effects for the use of nitroglycerin. (pp. 373) 43. Define the function of all controls on an automated external defibrillator, and describe event documentation and battery defibrillator maintenance. (pp. 386-388; 396; 399-400) 44. Defend the reasons for obtaining initial training in an automated external defibrillation and the importance of continuing education. (pp. 400) 45. Defend the reason for maintenance of automated external defibrillators. (pp. 399) 46. Explain the rationale for administering nitroglycerin to a patient with chest or discomfort. (pp. 372) Skills 1. Demonstrate the assessment and emergency medical care of a patient experiencing chest pain or discomfort. 2. Demonstrate the application and operation of the automated with external defibrillator. 3. Demonstrate the maintenance of an automated external defibrillator. 4. Demonstrate the assessment and documentation of patient response to the automated external defibrillator. 5. Demonstrate the skills necessary to complete the Automated Defibrillator: Operator’s Shift Checklist. 6. Perform the steps in facilitating the use of nitroglycerin for chest pain or discomfort. 7. Demonstrate the assessment and documentation of patient response to nitroglycerin. 8. Practice completing a prehospital care report for patients’ cardiac emergencies. Chapter 18: There are no objectives in the National Standard Curriculum that pertain to the material contained in this chapter. Chapter 19: 1. Identify the patient taking diabetic medications with altered mental status and the implications of a diabetes history. (pp. 423; 428) 2. State the steps in the emergency medical care of the patient taking diabetic medicine with an altered mental status and a history of diabetes. (pp. 428) (Scan 19-1, pp. 424425) 3. Establish the relationship between airway management and the patient with altered mental status. (pp. 423; 428; 430-431; 436) 4. State the generic and trade names, medication forms, dose, administration, action, and contraindications for oral glucose. (pp. 428) (Scan 19-3, pp. 428) 5. Evaluate the need for medical direction in the emergency care of the diabetic patient. (pp. 428) 6. Explain the rationale for administering oral glucose. (pp. 423; 428) Skills 1. Demonstrate the steps in the emergency medical care for the patient taking diabetic medication with an altered mental status and a history of diabetes. 2. Demonstrate the steps in the administration of oral glucose. 3. Demonstrate the assessment and documentation of patient response to oral glucose. 4. Demonstrate how to complete a prehospital care report with diabetic emergencies. Chapter 20: 1. 2. Recognize the patient experiencing an allergic reaction. (pp. 447) Describe the emergency medical care of the patient with an allergic reaction. (pp. 448) (Scan 20-1, pp. 449-450) 3. Establish the relationship between the patient with an allergic reaction and airway management. (pp. 445; 447-448) 4. Describe the mechanisms of allergic response and the implications for airway management. (pp. 445; 447-448) 5. State the generic and trade names, medication forms, dose, administration, action, and contraindications for the epinephrine auto-injector. (pp. 445; 447-448) 6. Evaluate the need for medical direction in the emergency medical care of the patient with an allergic reaction. (pp. 448; 451-452) 7. Differentiate between the general category of those patients having an allergic reaction and those patients having an allergic reaction and requiring immediate medical care, including immediate use of epinephrine auto-injector. (pp. 445; 447448) 8. Explain the rationale for administering epinephrine using an auto-injector. (pp. 451453) Skills 1. Demonstrate the emergency medical care of the patient experiencing an allergic reaction. 2. Demonstrate the use of epinephrine auto-injector. 3. Demonstrate the assessment and documentation of patient response to an epinephrine injection. 4. Demonstrate proper disposal of equipment. 5. Demonstrate completing a prehospital care report for patients with allergic emergencies. Chapter 21: 1. 2. List various ways that poisons enter the body. (pp. 460) List signs and symptoms associated with poisoning. (pp. 459; 461; 465-466; 468; 471-472; 474; 476) 3. Discuss the emergency medical care for the patient with possible overdose. (pp. 476-477) 4. Describe the steps in the emergency medical care for the patient with suspected poisoning. (pp. 465-466; 469; 473; 476-477) (Scan 21-1, pp. 462; Scan 21-3, pp. 467; Scan 21-4, pp. 470) 5. Establish the relationship between the patient suffering from poisoning or overdose and airway management. (pp. pp. 466;-467; 473; 4760 6. State the generic and trade names, indications, contraindications, medication form, dose, administration, actions, side-effects, and reassessment strategies for activated charcoal. (pp. 462-464) (Scan 21-2, pp. 463) 7. Recognize the need for medical direction in caring for the patient with poisoning or overdose. (pp. 459; 461-467; 470; 476) 8. Explain the rationale for administering activated charcoal. (pp. 462-464) 9. Explain the rationale for contacting medical direction early in the prehospital management of the poisoning or overdose patient. (pp. 459; 461-465; 476) Skills 1. Demonstrate the steps in the emergency medical care for the patient with possible overdose. 2. Demonstrate the steps in the emergency medical care for the patient with suspected poisoning. 3. Perform the necessary steps required to provide a patient with activated charcoal. 4. Demonstrate the assessment and documentation of patient response. 5. Demonstrate proper disposal of equipment for the administration of activated charcoal. 6. Demonstrate completing a prehospital care report for patients with a poisoning or overdose emergency. Chapter 22: 1. 2. 3. Describe the various ways the body loses heat. (pp. 483) List the signs and symptoms of exposure to cold. (pp. 484-489) Explain the steps in providing emergency medical care to a patient exposed to cold. (pp. 485-490) 4. List the signs and symptoms of exposure to heat. (pp. 491-492) 5. Explain the steps in providing emergency care to a patient exposed to heat. (pp. 491-492) 6. Recognize the signs and symptoms of water-related emergencies. (pp. 493) 7. Describe the complications of near-drowning. (pp. 494-495) (Scan 22-1, pp. 496-497) 8. Discuss the emergency medical care of bites and stings. (pp. 500-506) Skills 1. Demonstrate the assessment and emergency medical care of a patient with exposure to cold. 2. Demonstrate the assessment and emergency medical care of a patient with exposure 3. 4. to heat. Demonstrate the assessment and emergency medical care of a near-drowning patient. Demonstrate completing a prehospital care report for patients with environmental emergencies. Chapter 23: 1. 2. Define behavioral emergencies. (pp. 512) Discuss the general factors that may cause an alteration in a patient’s behavior. (pp. 512-513) 3. State the various reasons for psychological stress. (pp. 512-513; 516) 4. Discuss the characteristics of an individual’s behavior which suggest that the patient is at risk for suicide. (pp. 515-516) 5. Discuss the special medical/legal considerations for managing behavioral emergencies. (pp. 517-518; 520) (Scan 23-1, pp. 519) 6. Discuss the special considerations for assessing a patient with behavioral problems. (pp. 514-517) 7. Discuss the general principles of an individual’s behavior which suggest that he is at risk for violence. (pp. 5170 8. Discuss the methods to calm behavioral emergency patients. (pp. 513; 516) 9. Explain the rationale for learning how to modify your behavior toward the patient with a behavioral emergency. (pp. 513; 516) Skills 1. Demonstrate the assessment and emergency medical care of the patient experiencing a behavioral emergency. 2. Demonstrate various techniques to safely restrain a patient with a behavioral problem. Chapter 24: 1. Identify the following structures: uterus, vagina, fetus, placenta, umbilical cord, amniotic sac, perineum. (pp. 526; 539) 2. Identify and explain the use of the contents of an obstetrics kit. (pp. 529-530) 3. Identify predelivery emergencies. (pp. 531; 545-548) 4. State indications of an imminent delivery. (pp. 528-531) 5. Differentiate the emergency medical care provided to a patient with predelivery emergencies from a normal delivery. (pp. 545-548) 6. State the steps in the predelivery preparation of the mother. (pp. 531-532) 7. Establish the relationship between body substance isolation and childbirth. (pp. 531) 8. State the steps to assist in the delivery. (pp. 532; 534) (Scan 24-1, pp. 533) 9. Describe care of the baby as the head appears. (pp. 532; 534) 10. Describe how and when to cut the umbilical cord. (pp. 537-538) 11. Discuss the steps in the delivery of the placenta. (pp. 538-539) 12. List the steps in the emergency medical care of the mother post-delivery. (pp. 538-540) 13. Summarize neonatal resuscitation procedures. (pp. 536-537) 14. Describe the procedures for the following abnormal deliveries: breech birth, prolapsed cord, limb presentation. (pp. 540-543) 15. Differentiate the special considerations for multiple births. (pp. 543) 16. Describe special considerations of meconium. (pp. 528; 545) 17. Describe the special considerations of a premature baby. (pp. 544) 18. Discuss the emergency medical care of a patient with a gynecological emergency. (pp. 549-5500 19. Explain the rationale for understanding the implications of treating two patients (mother and baby). (pp. 538) Skills 1. 2. 3. 4. 5. 6. Demonstrate the steps to assist in the normal cephalic delivery. Demonstrate necessary care procedures of the fetus as the head appears. Demonstrate infant neonatal procedures. Demonstrate post-delivery care of the infant Attend to the steps in the delivery of the placenta. Demonstrate the procedures for the following abnormal deliveries: vaginal bleeding, breech birth, prolapsed cord, limb presentation. 7. Demonstrate the steps in the emergency medical care of the mother with excessive bleeding. 8. Demonstrate completing a prehospital care report for patients with obstetrical/ gynecological emergencies. Chapter 25: There are no objectives in the National Standard Curriculum that pertain to the material contained in this chapter. Chapter 26: 1. 2. 3. List the structure and function of the circulatory system. (pp. 568-569) Differentiate between arterial, venous, and capillary bleeding. (pp. 570) State methods of emergency medical care of external bleeding. (pp. 572; 574-578) (Scan 26-1, pp. 573) 4. Establish the relationship between body substance isolation and bleeding. (pp. 569; 5720 5. Establish the relationship between airway management and the trauma patient. (pp. 572; 580) 6. Establish the relationship between mechanism of injury and internal bleeding. (pp. 579) 7. List the signs of internal bleeding. (pp. 579) 8. List the steps in the emergency medical care of the patient with signs and symptoms of internal bleeding. (pp. 580) 9. List signs and symptoms of shock (hypoperfusion). (pp. 582-583) 10. State the steps in the emergency medical care of the patient with signs and symptoms of shock (hypoperfusion). (pp. 584) Skills 1. Demonstrate direct pressure as a method of emergency medical care of external bleeding. 2. Demonstrate the use of diffuse pressure as a method of emergency medical care of external bleeding. 3. Demonstrate the use of pressure points and tourniquets as a method of emergency medical care of external bleeding. 4. Demonstrate the care of the patient exhibiting signs and symptoms of internal; bleeding. 5. Demonstrate the care of the patient exhibiting signs and symptoms of shock (hypoperfusion). 6. Demonstrate completing a prehospital care report for patients with bleeding and/or shock (hypoperfusion). Chapter 27: 1. 2. 3. State the major functions of the skin. (pp. 593) List the layers of the skin. (pp. 593-594) Establish the relationship between body substance isolation (BSI) and softtissue injuries. (pp. 596; 600; 627) 4. List the types of closed soft-tissue injuries. (pp. 594-596) 5. Describe the emergency medical care of the patient with a closed soft-tissue injury. (pp. 596) State the types of open soft-tissue injuries. (pp. 596-600) Describe the emergency medical care of the patient with an open soft-tissue injury. (pp. 600) 8. Discuss the emergency medical care considerations for a patient with a penetrating chest injury. (pp. 606; 608-6110 9. State the emergency medical care considerations for a patient with an open wound to the abdomen. (pp. 609; 612-613) (Scan 27-2, pp. 614) 10. Differentiate the care of an open wound to the chest from an open wound to the abdomen. (pp. 608-613) 11. List the classifications of burns. (pp. 613; 615) 12. Define superficial burn. (pp. 615) 13. List the characteristics of a superficial burn. (pp. 615; 620) 14. Define partial thickness burn. (pp. 615) 15. List the characteristics of a partial thickness burn. (pp. 615; 620) 16. Define full thickness burn. (pp. 615) 17. List the characteristics of a full thickness burn. (pp. 615; 6200 18. Describe the emergency medical care of the patient with a superficial burn. (pp. 620-622) 19. Describe the emergency medical care of a patient with a partial thickness burn. (pp. 620-622) 20. Describe the emergency medical care of the patient with a full thickness burn. (pp. 620-622) 21. List the functions of dressing and bandaging. (pp. 625; 627) (Scan 27-3, pp. 626) 22. Describe the purpose of a bandage. (pp. 6250 23. Describe the steps in applying a pressure dressing. (pp. 625) 24. Establish the relationship between airway management and the patient with chest injury, burns, and blunt and penetrating injuries. (pp. 596; 600-604; 606; 608; 610; 612613; 616; 619-620; 623; 624) 25. Describe the effects of improperly applied dressings, splints, and tourniquets. (pp. 625; 627-628). (Air splints and tourniquets were discussed in Chapter 26. Splints will be discussed in Chapter 28.) 26. Describe the emergency medical care of a patient with an impaled object. (pp. 602604) 27. Describe the emergency medical care of a patient with an amputation. (pp. 605) 28. Describe the emergency medical care for a chemical burn. (pp. 621-622) 29. Describe the emergency medical care for an electrical burn. (pp. 623-624) 6. 7. Skills 1. Demonstrate the steps in emergency medical care of closed and open soft-tissue injuries. 2. Demonstrate the steps in emergency medical care of a patient with an open chest wound. 3. Demonstrate the steps in emergency medical care of a patient with open abdominal wounds. 4. Demonstrate the steps in emergency medical care of a patient with an impaled object. 5. Demonstrate the steps in emergency medical care of a patient with an amputation. 6. Demonstrate the steps of emergency medical care of an amputated part. 7. Demonstrate the steps of emergency medical care of a patient with superficial burns 8. Demonstrate the steps of emergency medical care of a patient with partial thickness burns. 9. Demonstrate the steps of emergency medical care of a patient with full thickness burns. 10. Demonstrate the steps of emergency medical care of a patient with a chemical burn. 11. Demonstrate completing a prehospital care report for patients with soft-tissue injuries. Chapter 28: 1. 2. 3. Describe the function of the muscular system. (pp. 635-640) Describe the function of the skeletal system. (pp. 635-640) List the major bones or bone groupings of the spinal column, the thorax, the upper extremities, and the lower extremities. (pp. 635-638) 4. Differentiate between an open and a closed painful, swollen, deformed extremity. (pp. 642) 5. State the reasons for splinting. (pp. 644) 6. List the general rules of splinting. (pp. 645-646) (Scans 28-1 through 28-4, pp. 647652) 7. List the complications of splinting. (pp. 646) 8. List the emergency medical care for a patient with a painful, swollen, deformed extremity. (pp. 644) 9. Explain the rationale for splinting at the scene versus load and go. (pp. 644; 646) 10. Explain the rationale for immobilization of the painful, swollen, deformed extremity. (pp. 644-646) (Scans 28-5 through 28-17, pp. 661-678) Skills 1. Demonstrate the emergency medical care of a patient with a painful, swollen, deformed extremity. 2. Demonstrate completing a prehospital care report for patients with musculoskeletal injuries. Chapter 29: 1. 2. 3. State the components of the nervous system. (pp. 684-685) List the functions of the central nervous system. (pp. 684-685) Define the structure of the skeletal system as it relates to the nervous system. (pp. 685-686) 4. Relate the mechanism of injury to potential injuries of the head and spine. (pp. 686-689; 690-696) 5. Describe the implications of not properly caring for potential spine injuries. (pp. 693) 6. State the signs and symptoms pf a potential spine injury. (pp. 695-696) 7. Describe the method of determining if a responsive patient may have a spine injury. (pp. 695-696) 8. Relate the airway emergency medical care techniques to the patient with a suspected spine injury. (pp. 696) 9. Describe how to stabilize the cervical spine. (pp. 696) 10. Discuss indications for sizing a cervical spine immobilization device. (pp. 696; 698) 11. Establish the relationship between airway management and the patient with head and spine injuries. (pp. 691-693; 696) 12. Describe a method for sizing a cervical spine immobilization device. (pp. 698) 13. Describe how to log-roll a patient with a suspected spine injury. (pp. 703) (Scan 29-3, pp. 705) 14. Describe how to secure a patient to a long spine board. (pp. 703-704; 706) (Scan 29-4, pp. 706-707; Scan 29-5, pp. 709-711) 15. List instances when a short spine board should be used. (pp. 698; 703) 16. Describe how to immobilize a patient using a short spine board. (pp. 698; 703) (Scan 29-1, pp. 699-700) 17. Describe the indications for the use of rapid extrication. (pp. 698) 18. List steps in performing rapid extrication. (pp. 698) (Scan 29-2, pp. 701-702; Scan29-8, 716-717) 19. State the circumstances when a helmet should be left on the patient. (pp. 712) 20. Discuss the circumstances when a helmet should be removed. (pp. 712) 21. Identify different types of helmets. (pp. 712) 22. Describe the unique characteristics of sports helmets. (pp. 712) 23. Explain the preferred methods to remove a helmet. (pp. 712) 24. Discuss alternative methods for removal of a helmet. (pp. 712) (Scan 29-6, pp. 713714) 25. Describe how the patient’s head is stabilized to remove the helmet. (pp. 713-714) 26. Differentiate how the head is stabilized with a helmet compared to without a helmet. (pp. 713-714) 27. Explain the rationale for immobilization of the entire spine when a cervical spine injury is suspected. (pp. 692-694) 28. Explain the rationale for utilizing immobilization methods apart from the straps on the cot. (pp. 704; 707-708; 717) 29. Explain the rationale for utilizing a short spine immobilization device when moving a patient from the sitting to supine position. (pp. 698; 703) 30. Explain the rationale for utilizing rapid extrication approaches only when they indeed will make the difference between life and death. (pp. 698; 703) 31. Defend the reasons for leaving a helmet in place for transport of a patient. (pp. 712) 32. Defend the reasons for removal of a helmet prior to transport of a patient. (pp. 712) Skills 1. Demonstrate opening the airway in a patient with suspected spinal cord injury. 2. Demonstrate evaluating a responsive patient with a suspected spinal cord injury. 3. Demonstrate stabilization of the cervical spine. 4. Demonstrate the four person log roll for a patient with a suspected spinal cord injury. 5. Demonstrate how to log roll a patient with a suspected spinal cord injury using two people. 6. Demonstrate securing a patient to a long spine board. 7. Demonstrate using the short board immobilization techniques. 8. Demonstrate the procedure for rapid extrication. 9. Demonstrate preferred methods for stabilization of a helmet. 10. Demonstrate helmet removal techniques. 11. Demonstrate alternative methods for stabilization of a helmet. 12. Demonstrate completing a prehospital care report for patients with head and spinal injuries. Chapter 30: There are no objectives in the National Standard Curriculum that pertain to the material contained in this chapter. Chapter 31: 1. Identify the developmental considerations for the following age groups: (pp. 739740) infants toddlers preschool school age adolescent 2. Describe differences in anatomy and physiology of the infant, child, and adult (pp. 740-743) 3. Differentiate the response of the ill or injured infant or child (age specific) from that of an adult. (pp. 739-740) 4. Indicate various causes of respiratory emergencies. (pp. 766-767) 5. Differentiate between respiratory distress and respiratory failure. (pp. 766-767) 6. List the steps in the management of foreign body airway obstruction. (pp. 759-760) 7. Summarize emergency medical care strategies for respiratory distress and respiratory failure. (pp. 768-769) 8. Identify the signs and symptoms of shock (hypoperfusion) in the infant and child patient. (pp. 764-765) 9. Describe the methods of determining end organ perfusion in the infant and child. (pp. 764-7650 10. State the usual cause of cardiac arrest in infants and children versus adults. (pp. 766) 11. List the common causes of seizures in the infant and child patient. (pp. 771) 12. Describe the management of seizures in the infant and child patient. (pp. 772) 13. Differentiate between the injury patterns in adults, infants, and children. (pp. 775 777) 14. Discuss the field management of the infant and child trauma patient. (pp. 777) 15. Summarize the indicators of possible child abuse and neglect. (pp. 778-780) 16. Describe the medical/legal responsibilities in suspected child abuse. (pp. 779-782) 17. Recognize the need for EMT-Basic debriefing following a difficult infant or child transport. (pp. 784) 18. Explain the rationale for having knowledge and skills appropriate for dealing with the infant and child patient. (pp. 738; 743-745) 19. Attend to the feelings of the family when dealing with an ill or injured infant or child. (pp. 745-746) 20. Understand the provider’s own response (emotional) to caring for infants or children. (pp. 784) Skills 1. 2. 3. 4. 5. 6. Demonstrate the techniques of foreign body airway obstruction removal in the infant. Demonstrate the techniques of foreign body airway obstruction removal in the child. Demonstrate the assessment of the infant and child. Demonstrate bag-valve-mask artificial ventilations for the infant. Demonstrate bag-valve-mask artificial ventilations for the child. Demonstrate oxygen delivery for the infant and child. Chapter 32: There are no objectives in the National Standard Curriculum that pertain to the material contained in this chapter. Chapter 33: 1. Discuss the medical and non-medical equipment needed to respond to a call. (pp. 807-811) 2. List the phases of an ambulance call. (pp. 806) 3. Describe the general provisions of state laws relating to the operation of the ambulance and privileges in any or all of the following categories: Speed Warning lights Sirens Right-of-way Parking Turning 4. List contributing factors to unsafe driving conditions. (pp. 816) 5. Describe the considerations that should be given to: Request for escorts Following an escort vehicle Intersections 6. Discuss “Due Regard for Safety of all Others” while operating an emergency vehicle. (pp. 816-817) 7. State what information is essential in order to respond to a call. (pp. 815-816) 8. Discuss various situations that may affect response to a call. (pp. 819-820) 9. Differentiate between the various methods of moving a patient to the unit based upon injury or illness. (pp. 823-824) 10. Apply the components of the essential patient information in a written report. (pp. 826) 11. Summarize the importance of preparing the unit for the next response. (pp. 826; 828; 830-831; 834) (Scan 33-4, pp. 829; Scan 33-5, pp. 832-834) 12. Identify what is essential for completion of a call. (pp. 826) (Scan 33-3, pp. 827) 13. Distinguish among the terms cleaning, disinfection, high-level disinfection, and sterilization. (pp. 831) (Scan 33-6, pp. 834) 14. Describe how to clean or disinfect items following patient care. (pp. 831) (Scan 33-5 pp. 832-833; Scan 33-6, pp. 834) 15. Explain the rationale for appropriate report of patient information. (pp. 825-826) 16. Explain the rationale for having the unit prepared to respond. (pp. 811-812; 814) (Scan 33-1, pp. 813) Chapter 34: 1. 2. 3. Describe the purpose of extrication. (pp. 842) Discuss the role of the EMT-Basic in extrication. (pp. 842; 860) Identify what equipment for personal safety is required for the EMT-Basic. (pp. 845846) 4. Define the fundamental components of extrication. (pp. 842-860) 5. State the steps that should be taken to protect the patient during extrication. (pp. 846847) 6. Distinguish between simple and complex access. (pp. 857) Chapter 35: Explain the EMT-Basic’s role during a call involving hazardous materials. (pp. 868877) 2. Describe the EMT-Basic should do if there is reason to believe that there is a hazard at the scene. (pp. 868-877) 3. Describe the actions that an EMT-Basic should take to insure bystander safety. (pp. 868) 4. State the role that the EMT-Basic should perform until appropriately trained personnel arrive at the scene of a hazardous materials situation. (pp. 868-872) 5. Break down the steps to approaching a hazardous situation. (pp. 868-872) 6. Discuss the various environmental hazards that affect EMS. (pp. 868-872) 7. Describe the criteria for a multiple-casualty situation. (pp. 877-889) 8. Evaluate the role of the EMT-Basic in the multiple-casualty situation. (pp. 877-889) 9. Summarize the components of basic triage. (pp. 883-887) 10. Define the role of the EMT-Basic in a disaster operation. (pp. 877-889) 11. Describe basic concepts of incident management. (pp. 878-880) 12. Explain the methods for preventing contamination of self, equipment, and facilities. (pp. 872-8770 13. ` Review the local mass casualty incident plan. (pp. 877-888) 1. Skills 1. Given the scenario of a mass-casualty incident, perform triage. Chapter 36: There are no objectives in the National Standard Curriculum that pertain to the material contained in this chapter. Chapter 37: 1. Identify and describe the airway anatomy in the infant, child, and adult. (pp. 930- 933) Differentiate between the airway anatomy of the infant, child, and adult. (pp. 930933) 3. Explain the pathophysiology of airway compromise. (pp. 930-933) 4. Describe the proper use of airway adjuncts. (pp. 933) 5. Review the use of oxygen therapy in airway management. (pp. 933) 6. Describe the indications, contraindications, and technique for insertion of nasalgastric tubes. (pp. 948) (Scan 37-2, pp. 949) 7. Describe how to perform Sellick’s Maneuver (cricoid pressure). (pp. 942-943) 8. Describe the indications for advanced airway management. (pp. 930-933; 938; 945) 9. List the equipment required for orotracheal intubation. (pp. 935-938) 10. Describe the proper use of the curved blade for orotracheal intubation. (pp. 935-936; 942) (Scan 37-1, pp. 939-941) 11. Describe the proper use of the straight blade for orotracheal intubation. (pp. 935936; 942) 12. State the reasons for and proper use of the stylet in orotracheal intubation. (pp. 937938) 13. Describe the methods of choosing the appropriate size endotracheal tube in an adult patient. (pp. 936-937) 14. State the formula for sizing an infant or child endotracheal tube. (pp. 945-946) 15. List complications associated with advanced airway management. (pp. 9340 16. Define the various alternative methods for sizing the infant and child endotracheal tube. (pp. 945-9460 17. Describe the skill of orotracheal intubation in the adult patient. (pp. 939-941) 18. Describe the skill of orotracheal intubation in the infant and child patient. (pp. 945947) 19. Describe the skill of confirming endotracheal tube placement in the adult, infant and child patient. (pp. 943-944; 947) 20. State the consequence of and the need to recognize unintentional esophageal intubation. (pp. 934; 943-944; 947) 21. Describe the skill of securing the endotracheal tube in the adult, infant and child patient. (pp. 938; 944; 947) 22. Recognize and respect the feelings of the patient and family during advanced airway procedures. (pp. 941) 23. Explain the value of performing advanced airway procedures. (pp. 930; 933) 24. Defend the need for the EMT-Basic to perform advanced airway procedures. (pp. 930-933) 25. Explain the rationale for the use of a stylet. (pp. 937-938) 26. Explain the rationale for having a suction unit immediately available during intubation attempts. (pp. 950) (Scan 37-3, pp. 951) 27. Explain the rationale for confirming breath sounds. (pp. 943-944) 28. Explain the rationale for securing the endotracheal tube. (pp. 938; 944; 947) 2. Skills 1. 2. 3. 4. 5. Demonstrate how to perform Sellick’s Maneuver (cricoid pressure). Demonstrate the skill of orotracheal intubation in the adult patient. Demonstrate the skill of orotracheal intubation in the infant and child patient. Demonstrate the skill of confirming endotracheal tube placement in the adult patient. Demonstrate the skill of confirming endotracheal tube placement in the infant and child patient. 6. Demonstrate the skill of securing the endotracheal tube in the adult patient. 7. Demonstrate the skill of securing the endotracheal tube in the infant and child patient. Required Supplies (must have prior to beginning Clinicals) A wristwatch with a second hand and stethoscope Wearable pouch containing trauma shears, barrier device, gloves, & penlight These items must be with you in all skill labs and clinical rotations. Students who do not have these items will be sent home, receive a “0” for the day’s work, as well as have their hour deducted. Successful students adhere to the following guidelines: Responsibilities: The syllabus and assignment sheets are the primary sources of instructions in any college course. Students are expected to read them carefully and refer to them regularly. Students should write down any oral instructions given by the instructor and should be careful to make sure they have taken accurate notes and ask questions about any uncertainties about assignments before due dates. Successful students will be competent in the required objectives as listed in the syllabus, textbook chapters and lesson assignments as provided in class or lab. Students are responsible for the material in the textbook whether or not it is covered in class or lab. Successful students look up information first, so they ask informed questions, not questions they already have the answers to. If they can’t find the answers they contact the instructor after class via voicemail or email. Planning Time: Students who get A’s or B’s use their time wisely. The standard formula for college coursework is that every one hour of class will result in two to three hours of homework (reading, research and study). As a result, successful students plan their time wisely so they keep up with assignments. They also meet their instructor during office hours so they get much needed feedback on their work. Plagiarism: Plagiarism is copying the work of another person. This includes essays as well as obtaining answers from another student during a test, quiz, etc. Successful students always make sure that their work is original because it is paramount that the instructor be able to gauge what the student has learned. PLAGIARISM IS CHEATING AND WILL NOT BE TOLERATED. Anytime a student uses someone else’s work without giving the author credit, it constitutes plagiarism. Anyone who plagiarizes will receive an “F” on the assignment. If a student is suspected of plagiarism, he or she will bear the burden of proof. The student must be able to present rough drafts on related materials and discuss the topic intelligently. A second offense will result in immediate dismissal from the class. Anyone using another’s test answers will be dismissed from the course immediately. At any time when two students are engaged in allowing cheating, the person copying the answers will be immediately dismissed from the paramedic course and the person allowing the cheating will receive a “0” for the test, quiz, etc. Academic Honesty: NFCC is committed to providing a high quality educational experience to all students, and students are expected to follow appropriate and honest academic practices. A pamphlet discussing various types of academic dishonesty and specific penalties will be provided to all NFCC students and is available on the Academic Affairs webpage at www.nfcc.edu. All cases of academic dishonesty will be reported to the Office of Academic Affairs. Classroom Conduct: Successful students conduct themselves in a professional manner because college is a professional environment. Successful students are ready to start class at the designated time, which includes notebook open, and pens ready to take notes. Diligent note-taking and being attentive during class demonstrates to the professor that the student is a serious student who wants to learn. Notes also provide a reminder of what was discussed and can serve to flag material that is unclear. Later, re-read your notes. If you can’t remember or understand what you wrote, ask about it at the next class meeting via email or voicemail. Successful students direct their questions to the instructor about anything related to EMS that they do not understand during class. Students should not engage in side conversations and whispering because such behavior is disruptive and distracting to others around them. Many students have made huge personal sacrifices to come to college. Don’t disrupt their class. Students who engage in side conversations will be asked to leave the class. Successful students are attentive during class. They do not does off, do homework from other classes, organize their bags or purses, or compose letters to friends. they are also aware of those around them and are sensitive to what might offend others. They don’t engage in personal relationships during class and they choose language that will not be considered offensive. CURSING IS PROHIBITED IN THE CLASSROOM, ON CLINICAL SITES, OUTSIDE WHILE ON BREAK, OR ANY OTHER TIME YOU ARE ACTING AS A STUDENT REPRESENTATIVE OF THE COLLEGE. Any student who curses will be subjected to the progressive disciplinary policy procedures. While in lecture, labs, and clinical sites, please silence all beepers and cell phones as well as watch alarms, as these items are serious distractions in college classes and cannot be tolerated. According to our training program, our qualifications and procedures for the EMT training program adheres to the Florida EMS 64J-1 policies as well as the Chapter 401 of the Florida Statutes. As per EMS 64J-1 each EMT applicant shall demonstrate that the students are not subject to call while participating in class, clinical, or field sessions. Each student will function under the direct supervision of an EMS preceptor and shall not be used to meet staffing requirements. Any student who violates EMS64J-1 will be immediately dismissed from the program. This sill be strictly enforced! Communicating in Class: Students are encouraged to communicate with the instructor to work out difficult questions or problems. The instructors are always approachable, so please do not feel or assume that the instructor is too busy to speak with you. In the event the instructor you need to approach is busy at that moment, the student will be offered an alternate time for the meeting. The instructors may advise tutoring if extensive assistance is required. There is time set aside for group discussion to take place, however, discussions need to be reserved for the specified times. Outbursts will not be allowed, nor will side conversations as they are disruptive and disrespectful to the instructor. Advocate/Ombudsman Office The Student Ombudsman provides confidential, informal, and neutral assistance to students seeking to resolve disputes or address issues of importance. The Student Ombudsman does not serve as a student advocate, but rather as a guide to assist students in the navigation of College organizational structure and understanding of policies and procedures. David Paulk is the current Student Ombudsman. He can be reached at 9739418 or paulkd@nfcc.edu . Attendance: Attendance is expected and you must be on time for all class sessions. Attendance policy: NFCC requires regular and consistent attendance of all students. Students’ grades may be affected or student may be withdrawn from class for non-attendance. Students are allowed two clock hours per credit hour of absence before the grade is affected. This includes excused absences as well as unexcused absences. Due to the length of classroom hours (5 to 6 hours per night) the 6 credit hour EMT course, EMS 1119, meeting twice per week, 2 absences are allowed. Campus Security The administration of NFCC diligently works to make the campus as safe as possible by keeping shrubbery low, security lights at strategic places, security guards on duty and unused buildings locked when not in use. Students should use normal precautionary measures when returning to cars in parking lots. Campus Security can be reached at 850973-0280 for assistance while on campus with non-911 security concerns. Library Services The Marshall Hamilton Library at NFCC is open during the fall semester during the following hours: Monday-Thursday from 8:00 AM to 9:00 PM Friday from 8:00 AM to 4:30 PM Sunday from 1:30 PM to 5:30 PM, beginning Sunday, October 1. Resources and staff are available in the library to support the student learning in the classroom. Students are encouraged to visit, browse the collections, and use the computers during these hours. Librarians are on duty to help with questions and research strategies. Access to the library’s extensive collection of electronic resources such as eBooks and academic databases with full-text articles is available 24 hours per day through the library’s website at www.nfcc.edu/library. Wireless internet is also accessible in the library. Specific policies and regulations applicable to the library are available in the library or by visiting the library’s website. Student Email: All NFCC students will be provided an email account through D2L, NFCC’s learning management system, and this will be the official email address used by faculty and staff for communication with students. Email addresses and instructions for accessing the email will be provided within the first two weeks of classes each semester and students are expected to check this email on a regular basis. Missing an examination: Exams are broken up into two categories: Module EExams and Quizzes. There will be 8 module tests during the year. Anyone missing a module test will not be allowed to make it up and will receive an automatic “0” on the exam. Anyone missing a quiz will be allowed to make up a total of two. If a make-up quiz is administered, the quiz will not be the same as that taken by the rest of the class and a maximum score of 80% is all that will be applied. Clinical policy: Clinicals will be performed at designated locations during times that have been scheduled through the EMS Coordinator. Any student attending a clinical without the knowledge of the EMS Coordinator will not receive credit for the time and/or calls obtained during the unscheduled event. Professionalism is paramount at all clinical sites. Students are expected to arrive on time prepared to go to work. DO NOT SHOW UP AT A CLINCAL SITE NEEDING TO GET INTO YOUR UNIFORM. Students should be prepared to assist in checking off any and all ambulances in the mornings to help get acquainted with the ambulance he/she will be working in that day. After calls, students are expected to assist in cleaning the ambulance as well as restocking after the call is completed. No paperwork should be brought back to the service and expect the preceptors to sign on their next shift. The ONLY exception to this is when the clinical has been completed and the preceptor is unavailable to sign, such as when having been sent on another call. Missing an assigned clinical period will result in the drop of one letter grade. Students who choose not to continue the course are responsible for turning in an Add/Drop Slip to the registrar’s office. The student need not assume a drop slip has been turned in for him/her. Failure to officially drop the course will result in an “F”. Grading policies: Quizzes: Anyone who misses a quiz due to an absence may make-up a total of two quizzes. The quiz will be different from that taken by the rest of the class and the highest possible score is 80%. Module Tests: There will be a total of 8 module tests administered throughout the course of the year. If you miss a module test due to absence, you will be given a “0” for that test. Each module test must be passed with an 80% or higher. Any student taking the division test and scoring less than 80% may elect to retake two tests (once each) to try and obtain a passing score. The failed test and the retake will be averaged together, and the combined grade must be higher than 80% to be considered passing. The highest score possible will be 80% for your recorded grade. Midterm Exam: during each semester, a mid-term exam will be administered. The midterm exam may consist of any and all subject matter covered in lecture, reading assignments, handouts, and skills lessons. Students who score less than 80% on the mid-term will be dropped from the program. Students who score more than 80% on the mid-term but have an overall score less than 80% at the time will be counseled about commitment to the program and remediation will be required during times other than regularly scheduled class/lab time. Students who do not carry an 80% or higher score after the mid-term throughout the remainder of the semester may be dropped from the program. There will be NO MAKE-UP ON THE MID-TERM EXAM. ATTEMDANCE IS A MUST. In the event the student is absolutely not able to attend the make up, this may be discussed with the instructor and a time PRIOR to the exam date may be determined. Comprehensive Written Final Examination: the final examination may consist of any and all subject matter covered in lecture, reading assignments, handouts, skill sessions, and mid-term examination. Passing score for the written final exam is 80% Students who do not score a minimum of 80% on the final examination will not be eligible for the certification test. Comprehensive Practical Examination: The comprehensive written practical examination will be performed by Dr. Robert Spindell, MD or his designee. All tests require a passing score of 80% or higher to complete the course. Skills testing: Skills testing will address each module. Each student will be administered a skills test at the completion of each division. Skills tests must be passed with a score of 80% or greater. Each student will be given one attempt to successfully complete each of the skills. If a skill is failed, the student will be required to commit to 10 hours of remediation and given 1 attempt at a retest on each failure. Maximum of 3 skills can be retested. A failure on a retest will eliminate the possibility of certification. Grading: This course is graded on the following scale: A= 100% - 92% B= 91%-85% C= 84%-80% D= 79%-70% F= 69%-below Grade calculation: Workbook – No grade assigned, this is a course requirement Lab Participation= 10% Quizzes= 15% Module Exams= 20% Midterm= 25% Final= 30% The EMS Coordinator reserves the right to alter this syllabus in part or whole on an individual basis in the event of extenuating circumstances. Extenuating circumstances will be determined on a case-by-case basis as determned by the EMS Coordinator. EMS Clinical Rotation Emergency Department Objectives: During clinical rotations in this area, the EMT-B student should have the opportunity to gain experience and develop proficiency in the following skills: 1. Triage 2. Physical assessment, patient history, documentation in compliance with hospital policy for all age groups 3. Vital and diagnostic signs: recognition and significance. 4. Aseptic techniques and universal precautions. 5. Management of trauma, medical, peds, OB?GYN emergencies 6. Emotional support of patient and family. 7. Wound care and bandaging. EMT-B student is not allowed to discharge a patient from the Emergency Department. Students may go to in-house codes with the approval of the EMS Coordinator. Students may not attend a code without direct supervision of the ER physician or EMS Clinical Instructor/Preceptor. Students should assist emergency department’s staff in all aspects of patient care, including changing beds, transferring patient to floor or X-ray, giving urinals or bedpans, etc. At no time will the EMT student be allowed to document of the patient’s chart. A clinical experience in the emergency department requires the cooperative effort of the students, staff, physicians, and the clinical instructor. Any problems should be brought to the attention of the EMS Clinical Instructor immediately. Problems requiring additional intervention than that of the EMS Clinical Instructor/Preceptor should be brought to the attention of EMS Coordinator, Mac Leggett at 850-973-1673. During the clinical phase of the EMT-Basic training program, the student should have the opportunity to gain experience and applications skills to enhance their proficiency in the following skills: At the conclusion of the course the student will be able to perform to the United States Department of Transportation National Standard Curriculum 1998 EMT-B Objectives- Numbers 1-1.1 through 8-1.35. These objectives are listed in the NFCC EMT handbook. Textbook: Not required during clinical rotation. Grading policy: All evaluations and written reports will be graded. All evaluations will be given a score of 0-100 equaling the following: 0=0; 1=20; 2=40; 3=60; 4=80; 5=100. The written reports will be graded on content as well ass legibility and documentation accuracy. All evaluations and reports will then be averaged and a grade will be submitted accordingly. This course is graded on the scale recorded previously. Clinical experiences at the Madison County Memorial Hospital, Madison County Emergency Services, DMH EMS, Jefferson County EMS, Hamilton County EMS, Leon County EMS and Suwannee County EMS will begin within the first few weeks of the program. These clinical experiences are designed to enhance and compliment those theoretical and practical experiences obtained in the classroom. While on any clinical setting no student may participate in any firefighting activity. Students who respond with the ambulance to a fire-related call are there for the support of the on-duty firefighters and should be prepared to assist in any treatment required by firefighters or victims. According to our training program, our qualifications and procedures for the EMT training program adhere to the Florida EMS 64J-1 policies as well as Chapter 401 of the Florida Statutes. Each EMT applicant will demonstrate that the students are not subject to call while participating in class, clinical, or field sessions. Each student will function under the direct supervision of an EMS preceptor and shall not be in the patient compartment alone during patient transport and shall not be used to meet staffing requirements. Any student violating the above statutes will be immediately dismissed from the program. This will be strictly enforced. EMS 1421 EMS Field Clinical course syllabus for EMS ride time North Florida Community College EMT-B Internship Objectives Learning experiences are designed to progress sequentially from simple concepts to complex integration of those concepts. They are directed toward assisting the student in meeting the objectives of the course. This course will involve ride experience with an Advanced Life Support provider. It will provide the beginning EMT-B student an opportunity to master basic life support skills and therapeutic communications. 24-30 hours of learning experience in a work environment will be required. Enrollment is restricted to those students with concurrent enrollment in the EMT-B program. Pre-requisites/Co-requisites For The Course: Acceptance into the EMT-B Certificate Program EMS 1911, EMS 1911L, and EMS 1411 ER Clinical Experience General Course Information: Topics to be covered include: Field orientation, map reading skills, BLS equipment review, therapeutic communications with patients of all age groups under the direct supervision of a paramedic preceptor. Course Outcomes: At the conclusion of the course, the student will be able to perform to the USDOT National Standard Curriculum 1998 EMT-Basic objectives. Introduction: NFCC and above named Emergency Medical Services would like to welcome the EMTB student to the field internship. The student will be assigned to a paramedic preceptor. These NFCC approved preceptors are graciously volunteering their time to assist the student in this phase of EMT/paramedic preparation. The preceptor should be viewed as a role model, teacher, and evaluator. Educationally rewarding internship experiences require the cooperative effort of the students, EMS, and NFCC. Conduct: Student conduct and attitude should convey a message of serious interest in the care of the patient and the procedure performed. Professional conduct shall reflect respect and consideration. Patient confidentiality shall be respected. Any discussion of the physical or social life of patients, EMS personnel, or personnel from other assisting agencies is strictly unethical. Constructive criticism and suggestions are welcome. If the student notices things which he/she does not understand or that are questionable, please talk to the person involved first. Additional clarification or information may be obtained from supervisors, training staff, or the NFCC EMS Coordinator. Use good judgment for the appropriate time to ask a question. Dress Code: NFCC EMT uniform 1. Clean, pressed NFCC EMS uniform shirt 2. NFCC name tag and student’s name on tag worn on right side of shirt 3. Clean, pressed navy or black uniform style pants 4. Blue or black socks 5. Clean black shoes or black boots (heals less than 1”) 6. Pen with blue ink 7. Stethoscope 8. Watch with second hand Personal Grooming: 1. Rings are limited to wedding bands only 2. Additional jewelry is not allowed while in NFCC uniform. 3. Appropriate fingernail length, care and use of soft, subtle polish if desired 4. Cologne, shaving lotions which can be annoying or cause discomfort to patients and personnel will be avoided 5. Hair must be neat and clean. If longer than shoulder length it must be styles above the collar. To clarify, male or female, your hair cannot touch your collar, PERIOD. 6. Daily bath or shower. Avoid body odor by use of soap, deodorant and mouthwash. Night Shifts Students Must Have Prior Permission From NFCC EMS Coordinator 1. Bring sheets, pillow and blanket or sleeping bag. 2. Sleeping facilities are co-ed; do not sleep in your NFCC uniform. You may sleep in a clean, white crew neck tee shirt and shorts with a minimum inseam of 3”. 3. Shower facilities are available at all stations. 4. Some stations may have kitchen facilities. Student Responsibilities: 1. The student should be on time and dressed in NFCC uniform. Late Policy: A student who reports for an assigned shift who is late on 3 separate occasions may be removed from the program at the discretion of the program director. A student may complete a maximum of 24 hours within a 36 hour time frame. 2. Report to the assigned station/preceptor. 3. If the uniform becomes soiled with blood or body fluids, it is to be removed and the student is responsible for decontamination per OSHA guidelines. If further information is needed regarding decontamination, contact should be made with any of NFCC’s EMS faculty. 4. A second uniform is recommended. If the student does not have an additional uniform to change into once the initial uniform has become soiled, the student will be sent home immediately. 5. The student is to perform only those duties as identified on the List of Objectives under direct supervision of a paramedic preceptor. 6. Hand washing is to be completed between each response and as required. 7. Use of personal protective equipment as needed when exposure to blood and body fluids exists. Note: Failure to use PPE will result in student being sent home for remainder of shift. 8. Valid professional level CPR card, proper ID must be carried at all times. 9. The EMT-B student must call the preceptor if he/she is going to be late. The student must notify the NFCC EMS Coordinator for tardiness or absence. All shifts must be scheduled through the EMS Coordinator only. No other means of scheduling will be accepted. 11. If a student must leave prior to the end of the scheduled shift, the NFCC EMS Coordinator and EMS supervisor must be notified. 12. The student must complete a minimum of 30 hours on a BLS ambulance. Ride time may be extended based on below average performance evaluations and failure to meet listed objectives. 13. Paramedic preceptors are ultimately responsible for patient care. Students are reminded not to take a procedural denial personally. Student Restrictions: 1. Students will not be allowed to drive any EMS vehicles. 2. Students will not be allowed to participate in any fire-related activities. 3. Students may perform only non-emergency radio communications. 4. EMS employees interning on any shift other than their regular assigned shift must wear the NFCC paramedic student uniform. 5. Fire service employees riding on EMS units performing as an NFCC EMT student must wear the NFCC EMT uniform. 6. Fire service employees who must return to fire-related duties must remove NFCC EMT uniform and cease hour time log towards required paramedic internship hours. 7. Students are not allowed to use tobacco products while on EMS clinical duty time at any EMS service. Preceptor Responsibilities: 1. Direct supervision of EMT-B students at all times. 2. Review of EMS services’ operational procedures and policies, standing orders, and medical protocol. 3. Review of ALS/BLS equipment as determined in daily goals. 4. Confirm patient consent for permission of student to administer patient care. 5. Critique calls as soon as possible after completion of run. Include evaluation and scene control; patient assessment; and hx taking communication/documentation skills, team work, judgment/treatment skills, use of equipment, establishment of priorities. 6. Problems or concerns should be brought to the attention of the NFCC EMS Coordinator. Problems of a serious nature should be brought to the attention of the onduty supervisor and the NFCC EMS Coordinator immediately. 7. Complete daily student evaluations and review with the student. List of Objectives: During the field internship, the EMT student should have the opportunity to gain experience and develop proficiency in the following skills: 1. Physical assessment, patient history, and documentation in compliance with EMS policy for all age groups. 2. Recognize and react appropriately to scene/safety hazards. 3. Vital and diagnostic signs: recognition and significance. 4. Aseptic techniques and universal precautions. 5. Observe peripheral IV insertion and drip rate calculations. 6. Observe drug therapy. 7. Cardiac arrest procedures. 8. CPR 9. Management of trauma, medical, peds, psychiatric, geriatric, OB/GYN emergencies. 10. Airway management including insertion of oral airways, suctioning, oxygen therapy, and observation of oral/nasal endotracheal intubation. 11. Observation of use of cardiac monitors. 12. Use of PPE recognition and application. 13. Emotional support of patient and family. 14. Observation of use of IV pumps. 15.0 Wound care and bandaging. 16. Splinting of extremity fractures. 17. Cervical immobilization and proper extrication. 18. Didactical understanding and practical application of all BLS equipment carried on EMS units. Students must be under direct supervision at all times Station Responsibilities: 1. Students are expected to actively participate in daily station cleaning duties with EMS crew members. 2. Assist with cleaning, stocking, and inventory of ambulance. 3. Study and work with preceptor daily. 4. Utilize self-motivation and initiative for ultimate learning experiences. Notification Procedures: Late/Sick- notify preceptor and NFCC EMS Coordinator. If not in office, leave message on voicemail. Do not page for late-sick notification. Injury- this includes any injury to self or patient. Notify on-duty supervisor. Supervisor will page EMS Clinical Coordinator. Infectious Disease Exposure- Complete Exposure Form and turn in to NFCC EMS Coordinator EMS Preceptors- Notify on-duty supervisor of any operational problems and EMS Coordinator of any internship concerns. EMS Supervisors- Page NFCC EMS Coordinator or Allied Health Coordinator for any problems requiring immediate attention.