Page 1 of 7 Vital Signs Taking Vital Signs Vital signs may include
advertisement

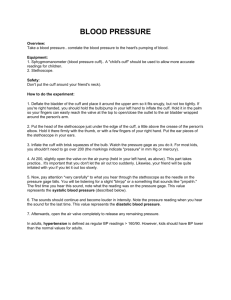
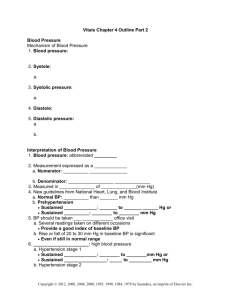
Page 1 of 7 Vital Signs Taking Vital Signs Vital signs may include: Respirations, Pulse, Oxygen saturation, Temperature, Blood pressure, Pain __________________________ Check suspicious condition Monitor existing condition Limitations May or may not detect important physiologic changes Indicate further investigation Normal does not equal ______________ Temperature Cellular metabolism requires a stable core, or “deep body,” temperature of a mean of 37.2° C (99° F) Body maintains steady temperature through a thermostat, or feedback mechanism, regulated in hypothalamus of brain Thermostat balances heat production (from metabolism, exercise, food digestion, external factors) with heat loss (through radiation, evaporation of sweat, convection, conduction) Various routes of temperature measurement reflect body’s core temperature Celsius vs Fahrenheit Most facilities document in celsius (universal) Fahrenheit to Celsius (°F - 32) x 5/9 = °C Celsius to Fahrenheit (°C × 9/5) + 32 = °F °F to °C Deduct 32, then multiply by 5, then divide by 9 ° C to °F Multiply by 9, then divide by 5, then add 32 Variables affecting Temperature Circadian (________________) Rhythms Trough occurs in early morning hours and peak occurring in late afternoon to early evening Hormones (progesterone) Age (infant, elderly) Exercise Stress Environment Temperature Routes Oral 37° C (98.6° F), with a range of 35.8° C to 37.3° C (96.4° F to 99.1° F) Convenient, accessible Right or left posterior sublingual pocket Accuracy varies ingestions of hot/cold drinks immediately prior to assessment Wait 15-20 minutes Rectal 0.4° C to 0.5° C (0.7° F to 1° F) higher than oral Considered most accurate Invasive and uncomfortable Used in infants and children Page 2 of 7 Use gloves, probe covers, and lubrication Risk for __________________________ Insert only ½-1 inch Check setting on digital thermometer Axillary 0.4° C to 0.5° C (0.7° F to 1° F) lower than oral Safe and noninvasive Placement and position of thermometer tip affects reading Middle of armpit with arm down at side Wait at least 15 minutes after bathing or exercising Tympanic (calibrated to oral or rectal scales) Convenient, safe, fast Research inconclusive of accuracy Technique affects reading Temporal Artery Scans the forehead area for the temporal artery Easy to Use Non-invasive Ideal for all age groups Clinically proven to be more accurate than tympanic thermometry Assessment of Pulses May evaluate carotid, brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis Apical pulse Pulse Characteristics Rate: Number of beats in 1 minute Influenced by blood pressure, age, gender, activity, emotions, pain, environment, medications, and disease Adult: ___________________ bpm May take for 30 seconds x2 Most accurate rate is measured apically using a stethoscope for a 60 second count period Infants –use brachial or apical Rhythm: Regular vs Irregular Second most important observation Symmetry: Right vs Left Amplitude: Pulse strength Absent to bounding If not palpable, try a ____________ ultrasonic stethoscope Graded Grading Pulses Grade Findings 0 Absent pulse 1+ Weak and thready 2+ Normal 3+ Full and bounding (Some agencies use a four-point scale) Page 3 of 7 Respirations One inspiration and one expiration = 1 breath Adult = _________________ breaths per minute In adults, frequently taken with pulse Pulse for 30 sec, Respirations for 30 sec Discreetly observe client’s breathing In babies, taken with stethoscope If chief complaint is respiratory, client is an infant, or you have difficulty assessing rate, take for a full 60 seconds May vary with anxiety, crying, excitement, fever, exercise, medications, altitude, and age Oxygen Saturation Oxygen saturation (SO2) measures the percentage of hemoglobin binding sites in the bloodstream occupied by oxygen. Pulse oximeter = device Normal = 95% - 100% Less than 92% = hypoxia Standing order in most facilities is to start _____________ of oxygen via nasal cannula Pulse Oximeter Need to be calibrated Place probe on tip of finger/toe/ear Reading will vary if: Finger/toenail has polish on it Extremity is cold/decreased circulation Skin is not intact Probe is placed over jewelry Record number/check orders Blood Pressure Force exerted by blood on the arterial walls Blood pressure is expressed in a ratio of systolic/diastolic (120/80) Systolic Blood Pressure: pressure exerted on the arterial wall when the heart ventricles are contracting Diastolic Blood Pressure: pressure exerted on the arterial wall when the ventricles are relaxed Factors Affecting Blood Pressure Age Gender Race Diurnal rhythm Weight Exercise Emotions Stress Cardiac Output Peripheral Vascular Resistance Blood Volume Viscosity Elasticity of Walls Page 4 of 7 American Heart Association recommended blood pressure levels BP Category Systolic Diastolic Normal less than 120 less than 80 Prehypertension 120–139 or 80–89 High (HYPERTENSION) Stage 1 140–159 or ____________ Stage 2 160 or higher or 100 or higher Hypertension Due to: Thickened arteries, inelastic arteries Smoking Obesity Lack of exercise Hypercholesterolemia Stress Hypotension Low blood pressure <___________________ This is relative… Orthostatic Hypotension Measured supine, sitting, then standing Wait 1 -3 minutes between positions Decrease in SBP of more than 20 points (this again, is relative) Equipment Sphygmomanometer Aneroid: Dial Mercury Electronic Sphygmomanometers Stethoscope Bell vs Diaphragm Side Doppler Ultrasound stethoscope Stethoscopes Tubing Eartips Chestpiece ______________ – low pitch Diaphragm – High pitch How to work your stethoscope If you have a double sided: If you have a one sided: Ear Placement Correct: Hold the headset in front of you with the eartips pointing away Once the eartips are in your ears, they should point forward Incorrect – Eartips back Page 5 of 7 Blood pressure cuff Blood pressure cuff Cuff size important Bladder width should be about _____________% of the arm circumference Cuff too narrow: False-high blood pressure Cuff too wide: False-low blood pressure Korotkoff’s sounds Phase 1: systolic BP –first sound heard, sharp tapping Phase 2: swishing/swooshing (can be an absence of sound) Phase 3: tapping, softer than phase 1 Phase 4: softer blowing muffled, last sound is diastolic BP Phase 5: silence Methods Direct (insertion of catheter into an artery) Indirect Auscultatory – usual method Palpatory – used to determine initial reading, used when unable to auscultate BP Site Choice Either arm, using brachial artery When not to use a particular limb Use thigh when arms unavailable (burns or injuries to both arms) Use opposite arm in cases of: Mastectomy with lymph node dissection IV infusion Fistula Do not take over _______________________ Do not use forearm Implementation Position appropriately Have sit quietly for 5 minutes Extend arm and support at heart level, palm up Make sure client does not have legs crossed Wrap deflated cuff around upper arm – apply center of the bladder directly over the brachial artery - one inch above antecubital space Determining a Target Pressure Perform a preliminary palpatory determination of SBP if this is an initial examination Palpate the brachial artery Pump up cuff until you no longer feel the brachial pulse, note pressure on sphygmomanometer Release cuff, wait 1 – 2 minutes (avoids false ____________ readings) Implementation Position stethoscope appropriately Auscultate the patient’s blood pressure Page 6 of 7 Pump up cuff until sphygmomanometer reads 30 mm Hg above the point where the brachial pulse disappeared Release valve carefully so that the pressure decreases at the rate of 2-3 mmHg per second Try to identify 5 phases Deflate cuff rapidly and completely Remove cuff Document data (even numbers) SBP/DBP = 106/68 Record RA (right arm) or LA (left arm), RL (right leg) or LL Erroneously High BP Bladder cuff too narrow Arm unsupported Insufficient rest before the assessment Repeating assessment too quickly Cuff wrapped unevenly Assessing immediately after a meal, smoking, caffeine containing beverage Assessing when client has pain Erroneously Low BP Bladder cuff too wide Deflating cuff too quickly (low SBP) Arm above level of heart Failure to identify auscultatory gap Sources of Pain Visceral pain – large interior organs Deep somatic pain – blood vessels, joints, muscles, bones Cutaneous pain – skin surface ________________ pain – Originates from a different location than felt Types of Pain Acute pain Short term Self-limiting Follows a predictable trajectory Dissipates after injury heals Chronic pain Continues for 6 months or longer Types are malignant (cancer-related) and nonmalignant Does not stop when injury heals Pain Assessment Pain assessment questions Where is your pain? When did your pain start? What does your pain feel like? How much pain do you have now? What makes the pain better or worse? Page 7 of 7 Pain Assessment Tools Initial pain assessment Brief pain inventory Short-Form McGill Pain Questionnaire Pain rating scales Numeric rating scales Descriptor scale Charting Vitals: 128/86 LA sitting 37.2°C orally Apical pulse 82 regular, Radial pulses +3, symmetrical and regular at 80 O2 sat 98% on room air RR = 16 Pain = 0 on 0-10 scale Can also use a graphing flow sheet