Minimum Requirements for Protective Attire in Animal Facilities
advertisement

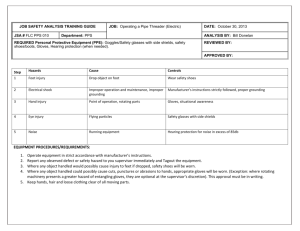
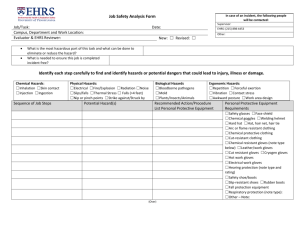
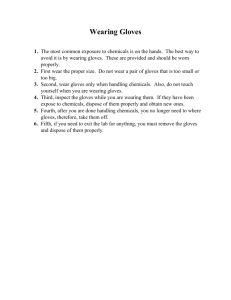
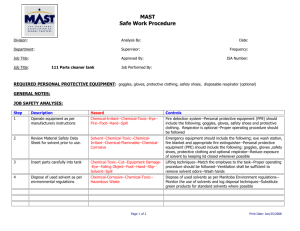
TITLE: MINIMUM REQUIREMENTS FOR PROTECTIVE ATTIRE IN ANIMAL FACILITIES Based on NIH Recommendations Purpose: Provide basis for utilizing a protective program through assessment of risk when working with various animal species and specific protective measures to reduce the risk, with an emphasis on personnel protective equipment and hygiene. Principles serving as the basis for selecting appropriate protective measures include: 1) reducing or avoiding animal-related accidents by understanding the potential for physical risks unique to each species, i.e. biting, scratching, kicking, etc; 2) sound personal hygiene based on knowledge of when contamination is most likely to occur, methods of avoidance and methods of decontamination, as exemplified by proper use of barrier methods and adequate hand washing practices; and 3) decreasing or eliminating exposure to zoonotic diseases by understanding common diseases that may be encountered with each species. In addition to protection provided by Personal Protective Equipment, PPE, hand washing is an important adjunct to the use of disposable gloves or in place of exam gloves for prevention of the spread of infectious organisms or other contaminants to both personnel and animals. While the use of gloves will greatly decrease the spread of contaminants from a person’s hands, they do not completely eliminate this transfer due to micro-breaks in the glove materials, regardless of type (latex, vinyl or nitrile). For effective hand washing, soaps or alcohol-based hand rubs are recommended. Definitions: Uniform: Clothing assigned for use only within the animal facility. It cannot be worn outside the animal facility without appropriate covering. Street clothes covering: A garment such as a laboratory coat or coveralls, worn to protect street clothes from contamination. This garment is not to be worn outside the animal facility. A unifrom may be substituted for a covering garment. Disposable exam gloves: Vinyl, latex or nitrile gloves which prevent contamination of skin by wet or dirty surfaces. Bite protection gloves: Gloves constructed of materials resistant to punctures, such as Kevlar and stainless steel mesh, which are worn either over exam gloves or under other protective gloves to reduce the likelihood of bite punctures. Arm length bite protection gloves: Heavy, reinforced gloves, usually of leather or similar material. The sleeves of these gloves should extend up to or over the elbows offering protection of the hands and forearms. These gloves do not necessarily prevent an animal from biting or inflicting injury; however, they usually prevent the bite from breaking the skin. Mucous membrane protection: A device or combination of devices, such as face shields, surgical face masks combined with protective safety glasses or goggles, etc., which protect the mouth, nose, and eyes from splash or droplet contamination. Shoe covering: Stretch booties, usually made of paper or plastic, worn over street shoes to protect them from contamination. These should not be worn outside the animal facility. Dedicated footwear may be substituted for shoe coverings. If dedicated shoes are worn, shoe coverings may be used to cover them when moving outside the facility. Hand washing: The single most important method in the prevention of the spread of disease to animals and staff is hand washing. Multiple studies have demonstrated that hand washing decreases the risk of oral intake of fecal and oral infective agents. Workers should wash their hands before and after coming into contact with animals. It is not clear that specific antibacterial hand washing agents are better than ordinary soap and water. It should be emphasized that even respiratory diseases are most likely transmitted hand to mouth rather than aerosol to lung, and that hand washing circumvents this route. Zoonoses: Diseases of non-human animals that may be transmitted to man or may be transmitted from man to non-human animals. NONHUMAN PRIMATES (NHP) Zoonotic Diseases: NHPs and humans are similar enough that many of the same agents that cause disease in one species cause disease in one species cause disease in the other, and dissimilar enough that agents relatively asymptomatic in one species can devastate the other. Cercopithecine herpesvirus-1 (Herpes B), tuberculosis, and various enteric infections are some of the more common zoonoses associated with NHPs. Even though research NHPs go through a specific quarantine process, because they may be wild caught and/or living in outdoor housing areas, they may still harbor certain zoonotic diseases. Table 1 outlines select bacterial, viral and parasitic agents that are transmissible from NHPs to humans and vice versa, that can be of concern. Wounds: All animal procedures should be performed by properly trained personnel, with a vigilant approach to the prevention of bites, scratches, and splashes both for the minimization of physical damage and the prevention of disease transmission, especially Cercopithecine herpesvirus-1 for macaque species. Proper sleeves, mucous membrane protection and appropriate gloves should be worn when scratches, bites and splashes are possible. The macaque exposure SOP must be followed when wounds and/or mucous membrane splashes occur, and all incidents reported. Protective measures: Table 2 outlines recommendations for specific activities associated with different risks of exposure. The guidelines assume that NHPs have passed through an appropriate quarantine. RODENT and RABBIT SPECIES: Zoonotic Disease: Zoonotic disease associated with modern rodent and rabbit research holding facilities in infrequent in incidence due to utilizing specific pathogen free animals and breeding programs, sentinel health monitoring programs , approved vendor procurements and policies for the importation of rodents and rodent products. Most zoonotic threats from rodents originate from wild caught species used for research (which necessitates special PPE requirements and husbandry), the use of contaminated rodent products or rarely from feral rodents gaining access to research animals. Human infections have mainly resulted from direct contact with the animals, their feces or urine, or indirectly by inhaling dried excreta carried on aerosolized dust. Table 3 lists select agents that are transmissible from rodent and rabbit species to humans that can be of concern. Attention to hygiene, to include use of disposable gloves, frequent changing of gloves, careful hand washing, and use of facemasks will aid prevention of zoonotic disease associated with rodent and rabbit species. Allergy: Allergic skin and respiratory reactions are quite common in personnel working with laboratory animals. Hypersensitivity reactions to animal allergens are serious occupational health problems that develop in many individuals after repeated exposure. Hypersensitivity reactions include nasal congestion rhinorrhea (runny nose), sneezing, itching of the eyes, asthma and a variety of skin manifestations such as redness, localized itching and flaking skin, and hives. Of the species used in biomedical research, the guinea pig, rabbit, mouse and rat appear to be the most allergenic. Urinary and salivary proteins from the animal’s fur, bedding, and caging are known source of allergens. Methods of prevention include reduction of direct animal contact time, use of biological safety cabinets, filter tops on animal cages, ventilated caging rack systems, HEPA filtered bedding dump stations, and protective clothing, masks, or respirators when working with these species. The N95 dust and mist respirator has been found to be extremely effective in minimizing exposure to aerosolized allergens. Individual concerns should be discussed with Occupational Health or a personal physician. Wounds: Training in proper handling and restraint of rabbits and rodents is the single most effective measure in protecting personnel from bites and scratches from these species. Other than the reported incidence of rate bite fever, the frequency and severity of bites resulting from rabbits and rodents appears to be minimal. Bite protection gloves may be indicated when working with rabbits and rodents inoculated with hazardous materials that may be shed in the saliva, or when working with fractious rodent species. Wearing long sleeves while handling rabbits can help in avoiding scratches. Protective Measures: Table 4 outlines recommendations for specific activities associated with different risks of exposure. FISH and AMPHIBIAN SPECIES Zoo notice Disease: Zoonotic diseases associated with fish and amphibian research holding facilities is infrequent in incidence, but can occur. Table 5 lists select agents transmissible from fish and frog species to humans that can be of concern. Allergy: Aerosolized fish proteins can be a source of allergic reactions for people and symptoms can range from allergic rhinitis to asthma. There also reports of occasional reactions to amphibious skin and secretions that range from cutaneous to respiratory signs. Protective measures: Table 6 outlines recommendations for specific activities associated with different risks of exposure