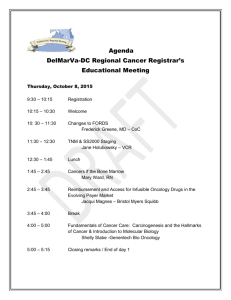
Nova Scotia
advertisement

An Innovative National Distance Education Initiative for Interprofessional Practice in Psychosocial Oncology I. Primary Applicant Organization Capital District Health Authority (Capital Health) Don Ford, President & CEO, Capital Health Suite 2142, 1796 Summer Street Halifax, Nova Scotia B3H 3A7 Project Lead Deborah McLeod Ph.D., R.N. Contact: Clinician Scientist (Nursing), Capital Health Cancer Care Program Assistant Professor, School of Nursing Dalhousie University Canadian Association of Psychosocial Oncology Dickson Building (1st floor) 5820 University Avenue Halifax, NS B3H 1V7 Phone: 902-473-2964 Facsimile: 902-473-2965 Email: deborahl.mcleod@cdha.nshealth.ca (CAPO) Member, Board of Directors and Chairperson, Education Committee Project Management Committee Barry Bultz, Ph.D., C. Psych. Director, Department of Psychosocial Resources Tom Baker Cancer Centre Adjunct Professor and Chair, Division of Psychosocial Oncology, Department of Oncology, Faculty of Medicine, University of Calgary Phone: 403-355-3205 Email: bdbultz@ucalgary.ca Susan Cadell, Ph.D. Assistant Professor School of Social Work and Family Studies University of British Columbia Associate, SocioBehavioral Research Unit B.C. Cancer Agency Rm.231, 2080 West Mall Vancouver, B.C. V6T 1Z2 Phone: 604- 822-5302 Email: scadell@interchange.ubc.ca Serge Dumont Ph.D. (Project Co-Lead) Professor, School of Social Work Université Laval, Québec City, CAPO, Member Board of Directors Quebec, G1K 7P4 Phone: (418) 656-2131 Ext. 7991 serge.dumont@svs.ulaval.ca Esther Green M.Sc.(T)., R.N. Chief Nursing Officer Director, Health Human Resource Planning Cancer Care Ontario President, CAPO 620 University Avenue Toronto, Ontario Canada, M5G 2L7 Phone: (416) 217-1278 Email: Esther.Green@cancercare.on.ca Grant Charles Ph.D Assistant Professor School of Social Work and Family Studies University of British Columbia Associate, SocioBehavioral Research Unit B.C. Cancer Agency Rm.337, 2080 West Mall Vancouver, B.C. V6T 1Z2 Phone: 604 822-3804 gcharles@interchange.ubc.ca Gary Rodin M.D., FRCPC. Head, Psychosocial Oncology and Palliative Care Program Princess Margaret Hospital, UHN Professor of Psychiatry and Head of the Behavioural Science and Health Research Division. University of Toronto 610 University Ave. Toronto, ON, Canada, M5G 2M9 Phone: 416-340-3044 gary.rodin@uhn.on.ca 1 Project Summary Project title: An Innovative National Distance Education Initiative for Interprofessional Practice in Psychosocial Oncology Capital Health’s Mandate: Capital Health provides core health services 40 per cent of the population of Nova Scotia, and tertiary and quaternary acute care services to residents of Atlantic Canada. Capital Health, particularly the QEII health Sciences Centre, is a primary clinical academic and research center for Dalhousie University. One of four strategic directions of Capital Health is to build knowledge, through, in part, fostering interdisciplinary care teams and promoting research and education Project Partners: The project partners include universities and clinical cancer agencies or programs in 7 provinces (NS, Nfld, NB, QC, ON, AB, BC). Each university includes 3-5 medical and health profession faculties, with one theological school partnering. The Canadian Association of Psychosocial Oncology is a key national partner. Project Objectives: 1)To develop an innovative approach to interprofessional education in psychosocial oncology at the post-licensure level in both English and French using blended, distance technologies. The outcome will be an introductory course that can be offered as a graduate level elective at the partner universities and adapted as a professional development option to be offered through CAPO/ACOP. 2) To establish a Canadian network of psychosocial oncology educators and researchers committed to enhancing the health of Canadians and their family members who are affected by cancer through collaborative and interprofessional education initiatives. Major activities/ Deliverables and Timelines: There are 3 phases to the project. In the first phase, a foundation for faculty/course development will be established through focus groups, key informant interviews, and environmental scans. In Phase 2 the two versions of the course (the graduate level, university based, for credit option and the professional development option) in both English and French will be developed. The course development will include the design of innovative strategies to promote interprofessional education and practice using distance technologies. Phase 3 will involve the initial piloting the course(s) and evaluation. Across the 3 phases, faculty development for interprofessional education will be conducted and activities to foster the development of a network of educators/researchers in interprofessional education will be designed. Expected Project Results: 1) Extension of already strong interprofessional education traditions in the partner universities to the post-licensure level of practitioner; 2) extension of professional development options to include explicit focus on interprofessional practice; 3) enhancement of education options for psychosocial oncology generalist and specialist students and practitioners, thus improving psychosocial care delivered to patients and families in Canada; 4) a template for interprofessional education using innovative distance technologies that can be applied to other specialty areas and to other health care practitioners.; 5) development of a network of educators/ researchers that will ensure sustainable activity in this are for psychosocial oncology. Evaluation Methods: A formative evaluation plan will be developed as part of a participatory evaluation approach informed by stakeholders in the project The formative evaluation design will incorporate the use of mixed methods (quantitative and qualitative) and multiple data sources. A results-based logic model will be used to guide the implementation of the program and subsequently inform the evaluation plan Dissemination plan: This project is designed to provide multiple opportunities for knowledge transfer and networking among all participants, including students, clinicians, faculty, patients/family. Knowledge dissemination, including conference and workshop participation, and publication of research results will begin at the end of the first phase of the project and continue throughout.. 2 I. Primary Applicant: Capital District Health Authority Organizational Overview The Capital District Health Authority exists within the largest integrated academic health district in Atlantic Canada, known as Capital Health. Capital Health provides core health services to 395,000 residents, or 40 per cent of the population of Nova Scotia, and tertiary and quaternary acute care services to residents of Atlantic Canada. Specialized adult health services are provided to a referral population from the rest of the province of 550,000, and to residents of New Brunswick and Prince Edward Island. Some 8,500 staff are employed within Capital Health. The Capital Health Cancer Care Program is the largest cancer program in the province, providing primary and secondary level care to residents of Capital Health as well as tertiary level acute care services to residents of Nova Scotia. In addition to providing cancer care in Capital Health, the program also provides care to patients around the province via satellite clinics. The Psychosocial Oncology Team is an interdisciplinary team of professionals providing psychosocial services to patients and families affected by cancer. The team includes advanced practice nurses, psychologists, social workers, a psychiatrist and spiritual care providers, all of whom will be involved in this project. These professionals have a long history of working in interprofessional teams, both with other psychosocial oncology practitioners and with the primary oncology teams of oncologists and oncology nurses. Deborah McLeod is the clinical team leader for this group. Dr. Andrew Padmos, Head of the Cancer Care Program at the QEII Health Sciences Centre, will sit on the Project Management Committee for the project. Dr. Padmos is also Commissioner, for Cancer Care Nova Scotia, and Associate Dean for Cancer Programs at the Dalhousie University's Faculty of Medicine. He holds academic appointments as Professor in the Departments of Medicine and Community Health and Epidemiology at Dalhousie. Dr. Padmos is also VicePresident Research & Academic Affairs for Capital Health and the QEII Health Sciences Centre. As VP for this portfolio, Dr. Padmos is also responsible for the Center for Clinical Research, which will provide necessary infrastructure for the project, including grant administration, office space and human resource support. Capital Health is the primary applicant leading a consortium that includes both clinical and academic partners in 7 provinces and a national professional association, the Canadian Association of Psychosocial Oncology/ Association Canadienne d'Oncologie Psychosociale (CAPO/ACOP). In addition to the national scope of the project, intended to benefit Canadians broadly, there will also be a strong Atlantic Canada collaborative partnership with Nova Scotia, New Brunswick, and Newfoundland collaborating as a regional team for the Atlantic region. These three province have already created a model for collaboration in graduate level education, led by Memorial University, through the Atlantic Region Training Centre for Applied Health Research in which students from all three universities complete their graduate education as a cohort. Capital Health is ideally suited to be the lead organization. It is the primary teaching hospital for Dalhousie University, with long standing affiliate agreements with the faculties of Medicine and Health Professions. Both institutions have a long history of collaboration in clinical and interprofessional education and strong relationships exist among the medical and health faculties and departments based on mutual respect, trust and a spirit of collaboration. 3 II. Project Partners The project partners include universities and clinical cancer agencies in 7 provinces: Nova Scotia, New Brunswick and Newfoundland will form a regional team, with partners in Quebec, Ontario, Alberta, and British Columbia. Another major partner will be a national, multidisciplinary, professional association, CAPO/ACOP. Partner faculties and schools include medicine, nursing, psychology, social work, and spiritual care. All of the partner universities have a strong history of interprofessional education and experience with distance education. Each province will form a local committee of university teachers and clinicians from 4-5 disciplines, with Atlantic Canada forming a regional committee. Each committee will be linked to the larger project through the Advisory Committee, described below, and through the project co-leaders and management committee members. The project links strongly with CAPO/ACOP, particularly the Education Committee, which provided the primary impetus for the project. The Chair of this committee, Deborah McLeod, is the project lead and the President of CAPO (Esther Green) and other Board members (Serge Dumont and Gary Rodin) sit on the project management committee. In addition to being linked to these major partners, this project is also linked to the Psychosocial Oncology Research Training Program (PORT, CIHR $1,800,000 2003-2009) with the principal investigator with PORT, Dr. Carmen Loiselle sitting on the Advisory Committee. Deborah McLeod is also one of the co-investigators/mentors with PORT. This project will complement the PORT agenda by expanding educational opportunities in psychosocial oncology clinical education at the Masters level. 1. Atlantic Canada Nova Scotia In addition to Capital Health, project partners in Nova Scotia include Dalhousie University (Faculties of Medicine, and Health Professions, principally the Schools of Nursing and Social Work), the Atlantic School of Theology, and Cancer Care Nova Scotia. Dalhousie University is the largest post-secondary institution in the Maritimes. Particular strengths of the partnering Faculties and Schools include considerable experience in distance education and well-established relationships with Capital Health. The Faculty of Medicine has over 1300 faculty, 360 medical students and 450 post-graduate physicians. There is already a partnership in place between the Faculty of Medicine, Cancer Care Nova Scotia and Capital Health to strengthen the cancer care system and to collaborate on education opportunities for cancer health care professionals. There is a large continuing medical education department, which is experienced in the provision of distance education to physicians in Nova Scotia. Dalhousie University Continuing Medical Education, Dalhousie University Continuing Pharmacy Education and the Registered Nurses Professional Development Centre recently collaborated with Cancer Care Nova Scotia in creating interprofessional modules for interactive, case based education for cancer care. The School of Nursing is renowned both nationally and internationally for its education programs, which have been offered since 1949, and the quality of faculty research. The School offers a Bachelor of Science in Nursing program, a post-baccalaureate primary health care nurse practitioner program, a master of nursing (MN) program, a joint master of nursing and health services administration (MN/MHSA) and a PhD (Nursing) program to more than 600 students. The School of Nursing is one of nine units within the Faculty of Health Professions (FHP) at Dalhousie and is a key participant in providing interprofessional education at the undergraduate level. 4 The Maritime School of Social Work offers Bachelors and Masters degrees in Social Work, both accredited by the Canadian Association of Schools of Social Work. The School also offers a diversified Continuing Education program. In 2001, the School launched a National Distance Delivery Mode for both the BSW and MSW degrees, the only distance education Masters of Social Work program in Canada. A number of faculty members are recognized as experts in distance education. Dalhousie has a strong history of interprofessional education that includes mandatory undergraduate modules in sexuality, disability, palliative care, family violence and 2 modules focused on working in interprofessional teams. is by The Tri-Faculty interprofessional Academic Advisory Committee (Tri-IPAAC) administers the interprofessional education program. Approximately 900 students who attend each module work together in randomly assigned interprofessional teams. More than 3900 students from the first to third years of their programs attend the interprofessional modules. These modules are supported by over 60 faculty and many more volunteers who are trained as facilitators. The tradition of interprofessional education at Dalhousie provides a strong community to support new interprofessional education initiatives. The proposed project builds on these traditions and initiatives in interprofessional education at the undergraduate level and extends it to post-licensure professionals and graduate students. The Atlantic School of Theology (AST) is an ecumenical university committed to excellence in graduate level theological education and research and in formation for professional ministries in churches, health care settings and the wider society. The two primary graduate programs offered by AST are the Master of Divinity and a Master of Theological Studies Degrees. AST offers courses in dying, death and bereavement, trauma studies, ethics, sexuality and narrative theology. In 2003 AST introduced a new curriculum, the focus of which is transformational leadership. Students are encouraged to be both creative and innovative throughout their time of study. At the heart of the curriculum is the belief that graduates can and indeed must be agents of spiritual and social transformation. Atlantic School of Theology in conjunction with the Institute of Pastoral Training (IPT) offers Clinical Pastoral Education (CPE) programs within a variety of health care setting throughout the Maritimes. IPT is affiliated with the Canadian Association for Pastoral Practice and Education (CAPPE). Both IPT and CAPPE are broadly ecumenical and support the work of all faith groups. They also provide spiritual and professional programming and certification to those who are interested in professional graduate education. Cancer Care Nova Scotia Cancer Care Nova Scotia's (CCNS) mandate is to coordinate, strengthen, and evaluate cancer services in Nova Scotia. CCNS programs include prevention, screening, education, treatment, follow-up care and palliation. Through the development of clinical guidelines and professional education, CCNS contributes to the standardization of cancer services across the province. CCNS develops and implements educational programs for health professionals based on recommendations from the Education Advisory Group. With representatives from across the province, the Advisory Group includes cancer specialists, health professionals and educational experts. The group provides advice and leadership on the development of evidence- and best practice-based educational programs for health professionals, which help to ensure a quality cancer care system. CCNS is also the lead agency in proposing an initiative in the area of 5 interdisciplinary education in cancer care. While it is expected that one project will inform the other, the two projects differ in substantial ways. The target audience in the CCNS project is community based generalist practitioners who wish to develop better knowledge in cancer care generally, whereas this project targets those with specialized interest in oncology and psychosocial oncology. The content of the course produced in our proposed project will provide much more indepth focus on a specialized area. However, it is expected that knowledge generated from both projects will inform and strengthen the outcomes of each. Furthermore, the synergy in focus on interprofessional education and practice in cancer care for both specialists and community based generalists across both projects, at least at the local Nova Scotia level, can be expected to contribute to more significant change in practice than either project on its own. Cancer Care Nova Scotia established the Cancer Patient Family Network in 2001, as a formal communication channel for cancer patients, survivors and family members. This network facilitates the sharing of information, fosters and promotes grassroots support for cancer patients and offers its members a collective voice to ultimately enhance the cancer system across the province. The Network will provide a primary link to patients and families for this project. A representative of the network will serve on the Advisory Committee. New Brunswick and Newfoundland It is anticipated that partnerships will be developed with interprofessional teams in cancer programs in New Brunswick and Newfoundland as well as with the University of New Brunswick (UNB) and Memorial University (MUN). The Schools of Nursing at UNB and MUN have agreed to facilitate the development of partner teams of clinicians and faculty in their provinces. This will allow an Atlantic Regional collaboration in interprofessional, distance based education at the graduate level. 2. Quebec In Quebec, the partner organizations will be Laval University and the Centre de Recherche de l’Hôtel-Dieu de Québec, a cancer research center with a strong basic and clinical research program, which was recently awarded a grant by the Canadian Foundation for Innovation (CFI) to build a new Clinical and Evaluative Research Center. This university research centre hosts one of the largest interdisciplinary team of research in psycho-oncology in Canada. Six clinicianresearchers with full time position in Laval Universty (medicine, pharmacy, nursing, social work, nursing, psychology) play an important role in teaching and research in North American and European French-speaking communities. As an outpatient center, it captures patients early in the course of their cancer trajectory from the diagnostic to the curative and the palliative phase which include all critical periods for psychosocial adjustment. This centre is becoming progressively a major referral center for the entire eastern part of the Province of Quebec, thereby providing access to a large number of patients for student clinical training. The professors currently supervise more than 15 graduate students in psycho-oncology. 3. Ontario The University of Toronto, founded in 1827, is Canada’s largest university. It is consistently ranked as one of Canada’s top research intensive universities. There are teaching programs in 17 academic divisions with educational programs offered across three campuses. There are nine fully affiliated teaching hospitals and over 67,692 students, most of whom are full-time. There are over 11,635 faculty and staff. The library is rated as one of the four top research libraries in North America with over 15 million holdings. 6 The Faculty of Nursing (FON) at the University of Toronto is renowned nationally and internationally for its educational programs and nursing research conducted by its faculty members. The faculty offers a Baccalaureate in Nursing Science, a Masters of Nursing with options for a combined Masters in Business Administration and a Clinical Focused Masters in four specialty areas, collaborative and practitioner programs, and a PhD program. Across all levels there are over 600 students. In 1994, the FON offered the only distance education program for preparing Acute Care Nurse Practitioners. In 2004, a specialty clinical track in oncology was developed. Psychosocial oncology is an important dimension of this program that needs further development. The FON is currently examining a specialty focus in oncology as one of the clinical streams in the Masters of Nursing program. The Princess Margaret Hospital (PMH), is the Oncology Division of the University Health Network, which is a large quaternary acute care hospital located in Toronto, Ontario. Princess Margaret Hospital is a world renowned comprehensive cancer centre. The program is comprised of 114 in-patient beds, with programs and clinics across all cancer sites including transplant. The program served over 38,525 patients in 2003/2004. Psychosocial oncology and palliative care is a very prominent department at PMH, comprised of a multidisciplinary palliative and pain care team, advanced practice nurses, psychiatrists, psychologists and social workers. A research division for psychosocial oncology and palliative care is currently in development. As a provincial cancer agency, Cancer Care Ontario (CCO) is a specialized, knowledge-driven, evidence-based organization that uses data to plan, fund, and report on performance of the cancer system in Ontario. CCO in its relationship with 11 Integrated Cancer Programs in 11 regions of the province, influences the delivery of a broader range of cancer services spanning the entire continuum of care. There is a strong emphasis on prevention and screening, diagnostic services, surgery, supportive and psychosocial oncology and palliative care across the entire system, as well as the traditional treatment aspects of radiation and chemotherapy. Princess Margaret Hospital has a formal affiliation agreement with CCO, as part of the unification of the cancer system. The Cancer Quality Council of Ontario (CQCO) was created with a mandate to publicly report on the quality of cancer services. In partnership with CQCO, CCO has produced several important reports, such as Strengthening the Quality of Cancer Services in Ontario, and the Four-Point Strategy to Reduce Waiting Times in Ontario. In 2005, CCO produced the first-ever Ontario Cancer Plan that provides a new and expanded profile of cancer services within the entire system, identifies the gaps and outlines specific strategies to improve care for people at risk for cancer and those living with cancer. In partnership with the University of Toronto, Faculty of Nursing, CCO is supporting the development of a Master’s program in oncology advanced practice nursing. CCO has guided the development of programs for other disciplines in oncology, and through the Integrated Cancer Programs located in academic health science settings, supports the clinical development of oncologists, social workers, psychologists, radiation therapists and nurses. As a provincial cancer agency and prime advisor to the government on the cancer system, CCO, in partnership with the Program in Evidence-based Care (PEBC) develops clinical practice guidelines in all domains of the continuum, including supportive care and psychosocial oncology. CCO supports research from bench to bedside and health services research. As an example of the latter, CCO has undertaken an evaluation of the integration of the cancer programs, funded by CIHR and CHSRF. 7 4. Alberta In Alberta, the partner organizations are the University of Calgary (U of C) and the Tom Baker Cancer Centre, Alberta Cancer Board. The Alberta Cancer Board is mandated under the Alberta Government, within the Cancer Program Act to coordinate all cancer research, prevention and treatment programs. The board operates 17 cancer treatment facilities, including the Tom Baker Cancer Centre (TBCC) in Calgary and four associate cancer centers in Red Deer, Grande Prairie, Lethbridge and Medicine Hat. The Department of Oncology at the U of C and the Department of Psychosocial Resources, TBCC are well positioned to partner in this project. Most of the staff members at the Department of Psychosocial Resources are cross-appointed as adjunct faculty at the U of C, while the Director of the Department of Psychosocial Resources (Barry Bultz) is also Chair of the Division of Psychosocial Oncology, Faculty of Medicine. The U of C has offered a course in Psychosocial Oncology (MDSC 635) for more than 8 years, the first of its kind in Canada. The course is taught by TBCC clinical staff, which includes psychologists, clinical social workers, and psychiatrists. In addition, the Department of Psychosocial Resources offers the only clinical training program in psychosocial oncology accredited by the Canadian Psychological Association. Other partner faculties include the Faculty of Social Work, which is recognized nationally for its excellence in education and research. In May 2005, the Faculties of Nursing and Social Work joined with Kinesiology, Medicine, Social Work and Veterinary Medicine to create a Division of Health Sciences. This represents a commitment and emphasis on an inter-professional and integrated approach to educating health professionals. 5. British Columbia The major partners in British Columbia include both campuses of the University of British Columbia (UBC Vancouver and UBC Okanagan) and the British Columbia Cancer Agency. These two institutions have many links but the most pertinent to this proposal is the course SOWK 570C Psychosocial Oncology: Grief, Loss and Survival, a graduate level course offered in the School of Social Work and Family Studies at UBC in conjunction with the B.C. Cancer Agency Patient and Family Counselling staff. The course, which has been offered since 2002, is housed in Social Work but is open to all disciplines. The University of British Columbia Vancouver Since opening in 1915, the University of British Columbia (UBC) has developed a reputation for innovation and excellence in both teaching and research, and has become a leader in higher education in Canada. The School of School Work and Family Studies at UBCV is a unique institution of higher education and professional learning in B.C. and Canada. Building on over seventy years of social work education and a quarter of a century of family studies education at UBCV, the recently merged School (1999), the only such institution in Canada, draws on its twin disciplines in education and preparing students as critically aware and reflective citizens, as family practitioners in the human services and for entry level and advanced professional social work practice. The School offers BSW and MSW degrees, both accredited by the Canadian Association of Schools of Social Work, majors in Family Studies at the BA and MA level, and has just started the first PhD program in Social Work and Family Studies in North America. The Faculty of Medicine at UBCV is a dynamic component of one of Canada's most exciting, innovative public universities, and the only medical school in the province of British Columbia. 8 Faculty members from 15 academic departments and 2 schools - Audiology & Speech Sciences, and Rehabilitation Sciences - are actively engaged in leading-edge research, education and community service on university and hospital campuses across the province. The College of Health Disciplines is a unique part of the interprofessional educational leadership at UBCV. The College leads the university's 15 health and human service programs in interprofessional education and research. For example, the College focuses on complex problems like patient safety, HIV/AIDS, family violence, palliative care and many others that demand a collaborative and or team approach. The University of British Columbia Okanagan The University of British Columbia Okanagan (UBCO), formerly Okanagan University College, opened its doors July 1, 2005. Its new Faculty of Health Sciences is comprised of the well established Schools of Nursing and Social Work. The vision for the Faculty is one of interdisciplinary and interprofessional teaching/learning in the context of strong, complex relationships with community partners that involves innovative educational strategies and the widest possible access for students. This will build upon currently existing links to the community, including the British Columbia Cancer Agency Centre for the Southern Interior, and an effective working relationship between the Schools of Nursing and Social Work. Rapid growth of the Faculty to include pharmacy, dentistry, medicine, rehabilitation sciences, and human kinetics is anticipated. A core of interdisciplinary/interprofessional courses is planned and will encompass interprofessional teamwork. Graduate programs in Nursing and Social Work will be launched in September 2006. An interdisciplinary centre focused on population and health services research is established and an interdisciplinary community based research unit focused on chronic illness is being developed. Further, an interprofessional clinical teaching and research unit has been proposed. The British Columbia Cancer Agency The mission of the BC Cancer Agency is to reduce the incidence of cancer; to reduce the mortality rate of people with cancer; and to improve the quality of life of people living with cancer. This mission is achieved by a system that links prevention, early detection, diagnosis and treatment, supportive care, rehabilitation, palliative care, education, research, and support for community programs. This system links research and treatment, leading to new solutions for treating cancer. This is achieved through four regional cancer centres in Vancouver, Vancouver Island (Victoria), the Southern Interior (Kelowna) and the Fraser Valley (Surrey). Each cancer centre provides patient services including assessment & diagnosis, chemotherapy and radiation therapy, counseling services and follow-up care. In addition there are provincial networks in cancer rehabilitation and palliative care. The B.C. Cancer Research Centre is part of the Agency and allows scientists, clinicians, students, and technicians to work to discover what causes cancer, ways to improve treatment and, in future, how to predict its occurrence or prevent it entirely. The BC Cancer Agency also has a SocioBehavioral Research Centre. 9 Canadian Association of Psychosocial Oncology/ Association Canadienne d'Oncologie Psychosociale A key partner and initiator of this proposal is the Canadian Association of Psychosocial Oncology/ Association Canadienne d'Oncologie Psychosociale (CAPO/ACOP). CAPO/ACOP is a multidisciplinary association that was established in 1985, incorporated in 1987, and achieved charitable status in 2003. The purpose of the Association is to foster and encourage interdisciplinary excellence in psychosocial research, education and clinical practice in oncology. The objectives of the Corporation are: To educate and disseminate information on all aspects of psychosocial oncology including promoting the efficiency and effectiveness of registered charities as recognized by Canada Customs and Revenue Agency regarding psychosocial oncology, by: a) conducting conferences and workshops educating professionals, health personnel and the public in clinical skills and theoretical concepts in psychosocial oncology; b) preparing and disseminating educational material to the public and health care professionals across Canada on all aspects of psychosocial oncology; c) providing a national network for the exchange of ideas; and d) establishing a library of educational materials concerning all aspects of psychosocial oncology. CAPO/ACOP was a partner in developing the Centre for Behavioural Research and Program Evaluation of the National Cancer Institute, is a member of the Board of the National Cancer Institute, and in 1999 drafted and adopted a set of Canadian standards for psychosocial oncology. CAPO/ACOP members (approximately 200) are involved in all levels of clinical care, planning, research, and education in cancer care and are regular participants on local, provincial, regional, national, and international planning groups. The CAPO/ACOP Education Committee mandate is twofold, namely to support patient/family education and to foster professional education in psychosocial oncology. Members of the committee represent a number of disciplines (nursing, medicine, psychology, social work, spiritual care and rehabilitation specialists) and all regions of Canada, with the exception of the territories. CAPO/ACOP has a 20-year history of fostering interprofessional and interagency collaboration, as well as collaboration across all levels of government. All major cancer agencies in Canada are represented in the CAPO/ACOP membership. CAPO/ACOP works in collaboration with, or has representation on the following national organizations: the Canadian Strategy for Cancer Control, National Cancer Institute, Canada (NCIC), the Canadian Institute for Health Research (CIHR), and the Canadian Association of Provincial Cancer Agencies. The membership of CAPO includes practitioners, educators, administrators and researchers in psychosocial oncology. CAPO is a respected member of the American Psychosocial Oncology Society (APOS) and the International Psychosocial Oncology Society (IPOS), leading North American and international organizations in the areas of practice, education and research. CAPO/ACOP is recognized not only by the formal cancer system but also by hospitals where systemic care is provided. Many members are faculty or adjunct faculty at leading universities in Canada. Due to its strong history of interprofessional collaboration and commitment to practice standards and education, CAPO/ACOP is ideally suited as a partner in this initiative. A number of CAPO representatives are project leads or co-leads for the project, including the President, Esther Green, the Chairperson of the Education Committee, Deborah McLeod and members of the Board of Directors, Serge Dumont and Gary Rodin. 10 III. Patients/Families and Learners The target audience for the distance course includes graduate students in medicine (including oncology, palliative care, family medicine and psychiatry residents) and the health professions, including nursing, psychology, social work, and spiritual care. The target audience for the professional development version of the course is clinicians who are new to cancer care and psychosocial oncology and who have not had previous education in this specialty area, as well as other clinicians who wish to increase or update their knowledge. The latter group might include oncology nurses, oncologists, family physicians and other community based professionals for whom psychosocial oncology is not a specialty practice but is of interest by virtue of their contact with cancer patients and families as part of their professional practice. The professional development option is expected to be particularly valuable to clinicians working in rural and remote areas where there are few resources and perhaps no psychosocial oncology specialists available. Surveys of the CAPO/ACOP membership have identified that the provision of educational opportunities through CAPO/ACOP is a high priority for them and have endorsed distance education as a key national priority. IV. Project Management, Advisory and Regional/Provincial Committees The Project Management Committee, will provide accountability and overall direction for the project. A larger Advisory Committee will function as an advisory group, providing input and direction for the project. Provincial/Regional Committees will be formed to include academic, clinical, patient/family & learner representatives, with the Atlantic provinces (NS, NB, NFLD) forming a regional committee. The provincial/regional committees will be responsible for ushering the syllabus through appropriate approval channels in their respective universities, gaining ethical approval for project evaluation components where necessary and providing opportunities for both clinicians and faculty to develop working relationships, knowledge, and skill in interprofessional education. Members of each provincial group will function as academic and clinical mentors to students in both the university course as well as in the professional development course. The budget has included costs for faculty members in each of the provinces to lead the universitybased course for the first offering, as well as stipends for other academic and clinical mentors to participate, thus ensuring meaningful involvement of 4-5 disciplines. See Appendix B for the list of participants for each province. Regional/Provincial Committees: Each regional/provincial committee will consist of the members of the advisory committee from that region or province plus additional clinical staff from the partner clinical agency psychosocial team/department as necessary. At least one of the members of the project management team will sit one each provincial/regional committee. In addition, 2 graduate students and 2-3 health professional members (oncology or community based professionals) will be appointed. The intent is to have good representation both from the university partner and the clinical agency partner, with at least 3, and preferably 5 health disciplines represented (medicine, nursing, psychology, social work and spiritual care). The provincial groups will work together to develop both academic faculty and clinical mentor knowledge and skill in interprofessional education. These educators will participate in the course offerings in Phase 3 of the project, functioning as mentors both locally and nationally. 11 V. Project Objectives The objectives of the project are: 1) To develop an innovative approach to interprofessional education in psychosocial oncology at the post-licensure level in both English and French using blended, distance technologies. The outcome will be an introductory course that can be offered as a graduate level elective at the partner universities and adapted as a professional development option to be offered through CAPO/ACOP. 2) Within the CAPO/ACOP Education Committee mandate, to establish a Canadian network of psychosocial oncology educators and researchers committed to enhancing the health of Canadians and their family members who are affected by cancer through collaborative and interprofessional education initiatives. VI. Project Description Psychosocial Oncology is an interprofessional sub-specialty in oncology for a variety of health professionals, including medicine, nursing, pastoral/spiritual care, psychology and social work. Psychosocial oncology programs and services in Canadian cancer care settings are always interprofessional in focus, including at a minimum social work, nursing and medicine. While the Canadian Association of Psychosocial Oncology (CAPO/ACOP) Standards of Practice (CAPO, 1999) identify the need for practitioners to be educated at a graduate level (Master’s, Ph.D, or post-graduate medical specialties), there are extremely few formal educational opportunities available for such education in Canada. Therefore, many health professionals employed with psychosocial oncology programs, departments or teams have no formal education in interprofessional, psychosocial oncology practice. The lack of such educational opportunities limits the availability of qualified psychosocial oncology specialists and, by extension, access of patients and families to adequately educated care providers. This project addresses these gaps through the development of an interprofessional, distance course, utilizing blended learning strategies, for graduate students in selected Canadian universities. The course will also be adapted and provided as a web-based professional development course for practicing professionals. It will provide students with opportunities to examine theory and research in psychosocial oncology and gain experience in interprofessional education for collaborative patient centered practice (IECPCP). The course(s) will be informed by, and linked to, existing or emerging courses and faculty members at the partner universities. There are important differences between the proposed course(s) and others that are available in Canada or via the internet, including current courses offered at UBC and U of C, as well as online education offered through the American Psychosocial Oncology Association. Strengths of the proposed course include the breadth and depth of the content, the sophistication of the distance, web based and other learning components, the possibility of university credit (adding credibility and rigor) and, most importantly, the emphasis on education specifically for interprofessional practice. No other course offering in the field in North America has emphasized the need, nor created specific educational strategies for psychosocial oncology practitioners to develop specific knowledge and skill in interprofessional team practice. This project will serve as an important catalyst to build knowledge and skill in interprofessional education strategies at the graduate and post-licensure level. It expands the focus on interprofessional education at the partner universities from undergraduate education to graduate 12 level, post-licensure education and will contribute to the development of innovative strategies for interprofessional education using distance technologies. Although this project will develop one course, it will provide a template for the development of future graduate level interprofessional and multi-site/sectoral courses, both within and beyond a psychosocial oncology focus. It also provides a template for other professions who might wish to develop educational initiatives specific to their discipline, extending the impact of this one project far beyond psychosocial oncology and its member disciplines. The project will be guided by an interprofessional advisory committee, representing 7 provinces (Nova Scotia, New Brunswick, Newfoundland, Quebec, Ontario, Alberta, & British Columbia) and both clinical and academic agencies, learners, patients/families, and representatives of related professional and health associations. The key product of the project will be the development of a unique inter-professional and multi-site blended learning, psychosocial oncology focused course, which will include innovative, distance-based opportunities for mentoring in interprofessional psychosocial oncology teams. The initial phase (0-9 months) of the project will involve environmental scans and national level focus groups. Environmental scans will consist of accepted literature and internet based search strategies. The interviews and focus groups will target the following: 1) psychosocial oncology practitioners (new and experienced) and administrators; 2) graduate student learners, including graduate students in medicine (principally oncology, palliative care, and psychiatry) and health professions (nursing, psychology, social work, and spiritual care); 3) practicing professionals who might be users of the professional development option (e.g. oncologists, oncology nurses, social workers, family physicians and other community based health professionals; and 4) patients and families. The key informant interviews and focus groups will include both urban and rural practitioners. A key benefit of distance-based education is the potential to support health professional working in rural communities. While a great deal of cancer care occurs in large centers, psychosocial oncology care needs often continue or develop closer to home. Since health professionals in rural and even small urban areas are not usually specialists, professional development options that are relevant and accessible are critically important to ensure Canadians receive the care they require. Accessible education is also a factor in support and retention of health professionals in rural and isolated communities. Focus groups with psychosocial oncology team members from clinical agencies partnered with this project will be conducted to explore questions such as: What knowledge/skills/attitudes do health professionals need in order to function well in an interprofessional, collaborative practice? What gaps in knowledge/skills/attitude are evident in practitioners new to this area of practice? What educational strategies would help to overcome these gaps? Focus groups with graduate student learners will explore questions such as: What attributes do you identify as important in a graduate level course focusing on psychosocial aspects of cancer? What knowledge and skills do you identify as essential for working with individuals and families experiencing cancer? Could you suggest some teaching approaches that enhance your learning? What experiences have you had in interprofessional education and what made these good (bad) learning experiences? Focus groups will also be conducted with members of the target audiences for the professional development course including oncology nurses, oncologists, rural practitioners providing support services to cancer patients/families, and family physicians. The question explored with this group is: How do professionals in this area of practice work together? The patient/family focus groups 13 will explore the question: What do health professionals need to know to meet the psychosocial needs of patients and families living with cancer? The second phase of the project (10-20 months) will involve the development of the graduate level, interprofessional psychosocial oncology course. Given the characteristics of the Canadian health care system, as rapidly changing and more certainly focused on community-based care, a call for change in the way that health professionals practice, and consequently in the way that they are taught to practice, is what this graduate level inter-professional course appeals to. These realities highlight the need for courses constituted by a sound educational pedagogy, reflecting narrative, cooperative, case-based teaching and learning strategies to complement current health reform and conventional educational approaches. Members of the Advisory committee and CAPO/ACOP will collaborate to consolidate pedagogical directions and content priorities, while acknowledging and incorporating the findings from the national environmental scans and focus groups. Instructional experts in inter-professional and blended distance learning education strategies, as well as web and graphic designers will be contracted to develop innovative inter-professional teaching and learning strategies with the required flexibility in delivery and content. The inter-professional course we create will immerse learners across Canada, into the realities of Canadians living with a challenging health diagnosis by utilizing a platform of blended learning strategies such as on-line or video-conferencing, casesstudies, and faculty/clinical mentors enriched by discipline decision making and narrative pedagogies. The third phase of the project (21-27 months) will involve the launch of both the university based elective option and the professional development option, as well as the initial evaluations of both. A faculty development/curriculum specialist will be hired as part of the project staff to develop education for faculty and clinical mentors. Local workshops will be offered in each province in Phases 2 and 3 of the project to prepare faculty and clinical mentors for interprofessional education. A national educator/researcher network will be developed and maintained through various CAPO/ACOP activities, including meetings and educational offerings in conjunction with CAPO/ACOP’s annual conference. Significance of the Project There is now good evidence that psychosocial oncology care contributes to a variety of important outcomes for cancer patients and families, including such things as alleviating distress, enhancing quality of life and supporting cancer rehabilitation (e.g. Blake-Mortimer, Gore-Felton, Kimerling, Turner-Cobb, & Spiegel, 1999; Bottomley, 1997; Fawzy, 1999; Meyer & Mark, 1995). There is also good evidence that there is substantial cost savings to be realized by the health care system when patients and families with medical illnesses including cancer receive adequate psychosocial care (Lane, 1998; Lechnyr, 1993; Simpson, Carlson, & Trew, 2001; Sobel, 2000). Provision of educational opportunities for psychosocial oncology clinicians that emphasize interprofessional, collaborative, patient/family-centered activities is essential if patients and families are to receive 14 sound, cost-effective care. Consequently, the need to rebalance care to ensure that psychosocial and supportive care issues are addressed is a strategic direction of the Canadian Strategy for Cancer Control. In order to realize this pan-Canadian approach to transforming the cancer care system to ensure a focus on psychosocial and supportive care as fundamental service elements in all cancer care settings education of all providers will be critical. The Education Committee and the Board of Directors of CAPO/ACOP have clearly identified the need to create, implement and evaluate interprofessional, graduate level psychosocial oncology education opportunities in Canada. The need for a consorted approach to workforce planning and training for interprofessional teamwork has been clearly mandated by the Canadian Health Services Research Foundation and Institute of Health Services and Policy Research (CIHR). In addition, professionals currently employed or new to the field of psychosocial oncology need to be supported and sustained in this challenging area of practice, particularly in rural or isolated areas. This proposal is reflective of a collegial and collaborative national commitment by health professionals, university faculty and researchers across Canada. The objectives of this proposal effectively address national concerns around workforce planning and interprofessional teamwork, contributing to excellence in psychosocial oncology care. The members of the advisory committee and institutional and professional affiliates represented within this initiative offer theoretical, practical and experiential knowledge essential to developing, delivering and evaluating interprofessional courses which clarify the scope of practice for health professionals employed in the specialty area of psychosocial oncology. This project not only appeals to the current and projected needs within the specialty of psychosocial oncology, but also to the challenges around interprofessional teamwork, with the plan to create a template that is generalizable to broader health care settings and learners. Conceptual Framework: Interprofessional Education The investigators of this project are cognizant of the concerns expressed within the health care system, by policy makers and educators to respond to the demand to ensure that the best health opportunities for all Canadians prevail. The current status of graduate level curricula continues to reflect the segregated discipline specific assumptions of a health care system that is predominately hospital or institutionally based. Yet, health care reform is clearly directed towards a community focused and family centred approach. This project is a response to the call for change in the way that health care professionals practice, recognition of what scope of practice means for each discipline and an acknowledgement of how disciplines work together in teams to meet the needs of Canadians safely. In order to offer Canadians safe and appropriate care, health professionals need to learn together in order to practice together. Through inter-professional education, members of each discipline gather together to teach and learn about their practice by utilizing narrative strategies to reflect, think about, decipher and analyze patient care situations with the purpose of identifying actions, accountabilities and responsibilities of each discipline. The focus of interprofessional team learning is on positive patient/family outcomes through discipline specific understandings. Discipline specific understandings are created as individuals of each discipline learn together, through patient care situations with the goal of understanding patients, their families and their contexts and how best to accommodate patient care responses to a complex health diagnosis. Members of each discipline negotiate, with the educator and mentors, specific actions, expectations and responsibilities. Hence, an inter-professional approach to education creates opportunities for individuals of 15 disciplines to understand the meaning of scope of practice and collaborative teamwork as a respectful and accountable taken for granted activity within patient/family centred practice. Narrative pedagogy Clarity within scope of practice and safe clinical decision-making has become a growing expectation within our rapidly changing health system. Insight into the decision-making challenges that health professionals make in practice is essential learning and expected knowing for members of all disciplines. This knowledge is beyond empirical understanding; more aptly this knowledge is more clearly represented through contextual analysis. Stories of Canadians being diagnosed and responding to complex health care issues, such as cancer, enables learners to be reminded of not only empirical knowledge, but also practical, ethical, social-political and personal knowledge. In understanding and exploring what another health professional thinks, deciphers and does within particular situations, students learn about discipline specific decision-making and scope of practice. This contextual mode of knowledge creation is identified by Diekelmann (2001) as narrative pedagogy. Narrative pedagogy (Diekelmann, 2001) has arisen out of interpretive studies of the practices of nursing students and educators. The emphasis in this pedagogy is on the creation of learning communities in which the practices of community hold issues of concern open and problematic. Narrative pedagogy does not supplant, but rather incorporates in conversation, more conventional pedagogies, such as outcomes and competency-based education, and alternative pedagogies such as critical or feminist approaches. In narrative pedagogy, the “concerns focus on presenting multiple epistemologies, exploring ways of knowing and practices of thinking” (Diekelmann, p. 54) as central to learning. With the emphasis within narrative pedagogy on locally generated communities of learning, in which multiple ways of thinking and interpreting are valued, narrative pedagogy offers a way of thinking about meaningful engagement with interprofessional learners and learning. Educators, students, clinicians and perhaps individuals and families living with cancer gather to collectively share and interpret situations in health care and foster understandings and consolidate knowing around practice responsibilities and accountabilities. The philosophical assumptions of narrative pedagogy, guide learners to explicate knowing through sharing, thinking, probing and analyzing situations. Learning in teams is facilitated when learners are able to engage in mastery of cases of increasing complexity in several domains. One type of cooperative learning is “case-based learning” in which interprofessional teams engage in consideration of life like “cases” of increasing complexity. Such learning is experiential, clinically based and addresses real patient/family situations, which are important elements for effective interprofessional learning and practice (D’Eon, 2004). D’Eon offers a hierarchical framework describing the nature of “cases” in ascending difficulty, with simple paper cases with two disciplines at one end of the spectrum, progressing to very complex cases in realistic or real-life settings with many disciplines. This framework provides a foundation for considering the development of cases for the course. “Cases” will include opportunities to consider both patient/family situations, as well as team process. Within the course there will be a strong emphasis on team process, increasing the learner’s awareness of how to contribute to highly functioning teams as well as possible solutions to areas of difficulty. 16 Inter-professional education strategies offer health professionals an understanding of practice that is based on a philosophy of inclusiveness, acknowledging the contributions of each discipline as equally relevant, non-hierarchical and complementary. In contrast to conventional and fragmented approaches which have traditionally been represented in discipline specific education, interprofessional teaching and learning strategies strive to engender consensus, mutual respect and a shared vision that is essential to ensure a synergistically relevant plan of care for Canadians living with cancer (Boon, Verhoef, O’Hara & Findlay, 2004). 17 VII Work Plan and Timelines Project Activities Timeline (month) Responsibility Outcomes Phase1 (0-9 months): Foundation and environmental scan Initial teleconference with Project management committee – monthly or bi-monthly for duration of project Press releases Initial teleconference with Advisory Committee – Project start up and review of project plan (thereafter at least quarterly teleconferences with two in-person meetings during the project in conjunction with the CAPO Annual Conference). Development of job descriptions for project coordinator; research assistants (RAs), curriculum/faculty development consultant Advertise/hire staff/set up staff offices Co-Chairs 1 1 2 2-3 Development of focus group/key informant interview matrix and guides for all constituent groups Prepare ethics submissions for each province 3 Design project webpage – contracted 3 Survey of existing courses First newsletter (every 3-4 months thereafter) Conduct focus groups Develop & release RFPs for web designer & graphic artist Data analysis & report – focus groups and key informant interviews Dissemination of focus group findings & consensus building (ongoing) – CAPO Board, membership, all constituents/partner organizations Development of curriculum templates: university based course professional development course Identification of content experts (CAPO Education committee; CAPO members) 3 3-4 4 4-7 7 8-9 9& ongo ing 7-9 8-9 Co-Chairs Advisory Committee Management Committee Management Committee Project coordinator Project coordinator Project coordinator Project coordinator & RAs Project coordinator RAs Project coordinator & RAs Management Committee Project Coordinator RAs Members of Advisory Committee; Project coordinator Job descriptions Curriculum consultant Advisory Committee Curriculum templates Experts identified Interview guides Submissions REB Web-page Survey report Newsletter RFP Report 18 Phase 2 (Months 10-20): Development of course, consensus building, formation of educators’ network Hire web/graphics designer 10 Develop course development plan outlining roles, timelines and pilot testing junctures with curriculum consultant, web designer, graphic artist Development course content, syllabus, curriculum resources and teacher manual 10-11 Identification of small group (learners, experts, faculty) for pilot testing of web-based course at key junctures 10 Design and testing of web-based components Consensus Building (ongoing) - Presentation of Draft Course syllabus CAPO Scientific Meeting & AGM In conjunction with CAPO Annual Scientific Meeting: initial meeting of psychosocial oncology educators formation of network pre-conference workshop offered on interprofessional education for patient-centered practice (invited speaker) Submission of course syllabus to curriculum committees at partner universities First faculty development workshop in each province – 1 day Finalize web/graphics & distance aspects 10-14 11-18 13 13 16 18 20 Management committee Project Coordinator Content experts Curriculum consultant Advisory/ Provincial Committees Project Coordinator + Advisory Committee Web designer Curriculum consultant + pilot test group Management committee Management committee + faculty development (FD) consultant Provincial Committee FD consultant and provincial committees Web/graphics designer Syllabus & teacher manual Formation of network of educators committed to IECPCP 19 Phase 3 (Months 21-27): Initial Course Offerings and evaluation Pilot test final course versions, including expert psychosocial oncology educators as one constituent group of evaluators. Make revisions. 21 Second faculty development workshop in each province 22 Launch graduate elective course in selected universities (3-5) and as professional development option though CAPO 23 Educators’ Network 2nd meeting in conjunction with annual scientific meeting CAPO Pre-conference workshop offered on IECPCP (invited speaker) Evaluation of educators network Evaluation of courses: focus groups and key informant interviews 24 Final project report 26-27 27 Project coordinator Curriculum consultant FD consultant and provincial committees University Faculty members of Provincial Committee & partner schools CAPO Board CAPO Education Committee & Advisory Committee Project coordinator Curriculum consultant Management Committee Network meeting Data collection Report VII. Evaluation Plan The evaluation of the impact of interprofessional education and practice is rift with methodological and measurement difficulties (Freeth, Hammick, Koppel, Reeves, & Barr, 2002). While there have been numerous attempts at measuring changes in interprofessional learner attitudes, values and skills there is not yet common agreement on universal measurement tools despite a great deal of effort in this area (Geller, Rhyne, Hansbarger, Borrego, VanLeit & Scaletti, 2002; Krist-Janson, Dudgeon, Nelson, Hentelff & Balneaves, 1997; Glennie & Cosier,1994; Freeth, Hammick, Koppel, Reeves, & Barr, 2002). Much of the problem involves attempting to isolate the impact of certain variables that come into play when dealing with complex health and human resource situations. These include learners’ reactions, modification of learners’ attitudes and perceptions, acquisition of knowledge or skills, behavioural changes within professional practice, and changes in the organization and delivery of care and improvements in the health of patients (Freeth et al., 2002). Clearly interprofessional education and practice has a number of dimensions, each of which needs to be accessed in order to determine their impact and contribution to the interprofessional learning and collaboration process (Barr, 1996). It is our intention to evaluate each of these areas as they pertain to our project as part of a formative evaluation approach. The formative evaluation plan will be developed as part of a participatory evaluation approach informed by stakeholders in the project. This approach has been shown to be successful when various stakeholder groups are involved in the development of an 20 initiative and is an essential element in the uptake of innovation and implementation of change. A formative evaluation will allow the program to be refined as it is being developed and will provide the data to inform program change. The formative evaluation design will incorporate the use of mixed methods (quantitative and qualitative) and multiple data sources. Focus groups will be conducted initially to ensure the program implementation is informed by stakeholder needs and to ensure the rigorous development of a relevant and appropriate program given the interprofessional diversity and environmental context across provinces and universities. A results-based logic model will be used to guide the implementation of the program and subsequently inform the evaluation plan. Program logic models have been found to be effective in planning and evaluating projects throughout the healthcare field especially in the promotion of results based performance in multi-stakeholder collaborations. This fits well with the national and complex multi-partner nature of our program. The inputs required in program implementation will be described and the outputs in the form of process indicators and outcomes will be captured. Short and intermediate term outcomes will be identified emphasizing the uptake of the program in various universities in addition to the satisfaction and impact of the program on participants. Long-term outcomes will be identified in relationship to the impact on patients and families and will inform future evaluation and research initiatives. The following is a proposed, preliminary format of the first three steps of a results based logic model to be used to guide the implementation of the educational program and the development of the evaluation framework and evaluation questions. The development of the logic model will be achieved through consensus processes with the stakeholders involved in the project during which time short, intermediate and longer term outcomes will also be formulated. Inputs: This will include all human, financial and material contributions through IECPCP and the project partners including Capital Health, Cancer Care Nova Scotia, CAPO, Princess Margaret Hospital, Alberta Cancer Board, BC Cancer Agency and the partner post-secondary institutions including Dalhousie University, McGill, the University of Toronto, the University of Calgary and the University of British Columbia. Outputs: This will include the development of the partnership process, development and delivery of an online curricula, the number of participants in the development and delivery process, the number of practitioners and students trained in interprofessional practice specific to psychosocial oncology and the increased number of interprofessional collaborations. Short-term Outcomes: These will include improved collaboration between health and education sectors, improved collaboration between professions, sustained national and local partnerships and related initiatives, increased capacity for specialized practitioner and student education and increased patient/community involvement. In addition, satisfaction with course content from participants enrolled will be evaluated as one of the short term outcomes. An intermediate outcome will include the uptake of the course as an accepted elective credit course in various faculties across Canada. It is our intention to establish an evaluation team comprised of representatives from the partners as well as patients and families. Expertise in measurement and evaluation will be accessed through the various community and post-secondary partners. The team will develop a range of measurement tools and methods associated with interprofessional education and collaborative practice specific to our project and to each of the project objectives. The following preliminary plan has been developed as a first step in the evaluation process. 21 The project objectives are: 1) To develop an innovative approach to interprofessional education in psychosocial oncology at the post-licensure level in both English and French using blended, distance technologies. The outcome will be an introductory course that can be offered as a graduate level elective at the partner universities and adapted as a professional development option to be offered through CAPO/ACOP. 2) Within the CAPO/ACOP Education Committee mandate, to establish a Canadian network of psychosocial oncology educators and researchers committed to enhancing the health of Canadians and their family members who are affected by cancer through collaborative and interprofessional education initiatives. Objective 1 1, 2 Focus of evaluation Gaps in knowledge, skills & attitudes: IECPCP /psycho-social oncology Course development & consensus building Method/Data Focus groups/ key informant interviews in 5 regions with: psychosocial practitioners (experts & entry level) health professionals (nurses, oncologists, family physicians) graduate students patients/families faculty currently teaching PS Oncology At key junctures (e.g. at the end of each lesson or phase) of the development of the online course, key informants will pilot test the course for Partners/ constituents involved CAPO membership Responsibility When Project coordinator Phase 1 (Months 4-7) Project coordinator curriculum consultant Begin at first key juncture –(Phase 2, month 11) & Universities (Dalhousie, Laval, U of T, UBC, U of C,) Clinical Agencies: BC Cancer Agency TBCC, Alberta Cancer Board Princess Margaret Hospital (ON) (Quebec) Cancer Care Nova Scotia & Capital Health (NS) Professional Associations: (College of Family Medicine; Canadian Association of Nurses in Oncology; Canadian Association of Social Work; Canadian Psychological Association; Canadian Association of Pastoral Practice Education) Key informants include: 1.University faculty with expertise in psychosocial oncology and interprofessional education 22 1, 2 Development teacher’s manual 2 Inaugural meeting – formation of educator’s network to foster knowledge, skill and research - Invited speaker/ presenter (IECPCP expert) ease of use of the web design satisfaction with content, graphics degree of interactive features congruence with established distance/web adult education principles congruence with principles of interprofessional education 2.Students 3.Practicing professionals expert new urban rural 4. Patients/families Key informants: University faculty with expertise in psychosocial oncology and interprofessional education As each section in the teacher’s manual is written pilot testing with key informants will be done to evaluate: adequacy of direction for faculty, with regard to both psychosocial content and principles of interprofessional education PS Oncology specialists clarity ease of use Key informants: Attendance at educational event Attendees at the educator’s network Pre/post tests of IECPCP (new meeting knowledge, theory, models) university faculty Participant satisfaction psychosocial oncology specialists Key informant interviews ( 3) months after the meeting to evaluate: Key partners involved: knowledge retention universities change in teaching or practice; clinical agencies & PS oncology teams or departments intention to conduct research CAPO web/graphic designers on going until course(s) are complete Project cocoordinator with support from curriculum consultant Phase 2 Months 1014 Project coordinator CAPO Annual Scientific Conference Members of the Advisory Committee Phase 2, Month 13 23 2 2nd Annual networking meeting and IECPCP Education al Event for PS Oncology Educators - Invited speaker/ presenter (IECPCP expert) 1 Course evaluation (knowledge, skill, course process): elective option Attendance at educational event Pre/post tests of IECPCP (new knowledge, theory, models) Participant satisfaction Key informants: Attendees at the educator’s network meeting university faculty psychosocial oncology specialists Project coordinator Members of the Advisory Committee Key informant interviews (3) months after the meeting to evaluate: knowledge retention; change in teaching or practice; intention to conduct research; formation of research teams Key partners involved: universities clinical agencies & PS oncology teams or departments CAPO Pre/Post tests of knowledge, attitudes – congruence with IECPCP Course participants Project co-ordinator Course faculty Education consultant Course process – written and key informant interviews: ease of use interactive design graphics CAPO Annual Scientific Conference Phase 3 (month 24) Phase 3 (month 2627) professional development option 24 IX. Knowledge transfer, Networking, and Dissemination The following strategies will support knowledge transfer, networking, and dissemination: A project website will be developed containing information about the project background and design, project updates, as well as links to information about IECPCP and psychosocial oncology. At each major juncture of the project, the CAPO Board and membership and other key partners will be informed and input solicited. Formal opportunities for knowledge transfer, networking and dissemination will be created in conjunction with at the annual CAPO scientific conference with CAPO members (who represent all regions and partner organizations) and conference attendees. Two such meeting swill be held during the tenure of this project, with ongoing meetings thereafter planned and supported by CAPO. Workshops with invited IECPCP expert speakers will be organized for Phase 2 and Phase 3 of the project and will be held annually thereafter in conjunction with the CAPO conference. The Advisory Committee and partners will seek opportunities for presentation of the project, project findings and IECPCP (using psychosocial oncology as an example) at international, national, regional and local meetings and conferences. In addition, members of the Advisory Committee will attend national networking meetings to disseminate the results of this project. Partner organizations that will be particularly targeted for dissemination include the clinical agencies, university faculties and professional organizations such as the College of Family Medicine, the Canadian Association of Nurses in Oncology, the Canadian Association of Social Work, the Canadian Psychological Association and the Canadian Association of Pastoral Practice Education. A quarterly project newsletter will be created and disseminated both electronically and in hard copy to project partners. Publication in peer-reviewed journals. Presentation of the process, outcome and evaluation of this course is intended at national and international educational and inter-professional forums/conferences. 25 X. Sustainability Plan Sustainable activities: 1. Sustain faculty commitment to offering elective graduate course using principles and strategies of IEPCPC Barriers and challenges Methods and support to overcome barriers Factors favouring sustainability Prior and project activities to increase chances of sustainability Stakeholders involved in sustaining activities University program resources variable and dependent on student interest Commitment from Deans, Directors, and/or Coordinators of Graduate Programs will be enhanced by including them in the project from the outset. Existing psychosocial oncology courses (UBC & U of C) demonstrate the viability of such courses. Regular Advisory Committee meetings will be held to ensure quality of stakeholders involvement. Deans, Associate Deans and Coordinators of graduate programs. Evidence Heads, Psychosocial Time/workload pressures on faculty Many schools are small and have limited elective courses to offer students. Sharing a course may be seen as viable way to enrich programs. Curriculum development costs are extremely high, particularly for high quality distance education courses. Sharing the costs through a national project is a reasonable way for all partners to gain something for students with low direct cost. Case based, interprofessional learning requires greater resources than traditional courses; requires both faculty and clinical mentors in several disciplines Stipends will be provided to support the involvement of faculty/clinical mentors in initial course offerings Involvement of university administrators and clinical agency CEOs is expected to increase commitment. There is a high commitment of clinical agencies already to such courses, with significant numbers of clinical mentors sharing teaching responsibilities with faculty (e.g. UBC & U of C). Clinical agencies are already engaged in considerable education of new staff due to the CEOs, Cancer Care Agencies. generated by the project, including the initial results of focus groups and evaluation of course outcomes, is expected to support ongoing commitment. Oncology/Supportive Care clinical programs The project will incur the cost of the initial course development, a significant factor in sustainability will be the availability of the course itself.. Deans, Associate Deans and Coordinators of graduate programs. The development of the educator’s network will ensure there are faculty and CEOs, Cancer Care Agencies. Heads, Psychosocial Oncology/Supportive Care clinical programs. 26 limited number of formal courses available in universities. clinicians with a high level of commitment to sustaining such a course. Sustainable activities: 1. (cont’d) Sustain faculty commitment to offering elective graduate course using principles and strategies of IEPCPC Barriers and challenges Possible lack of support for the principles of IECPCP Methods and support to overcome barriers Evidence generated by the project is expected to demonstrate the benefits of IECPCP Factors favouring sustainability Partner universities were largely selected because they have a tradition and history of commitment to interprofessional education Prior and project activities to increase chances of sustainability The development of the educator’s network will ensure there are faculty and clinicians with a high level of commitment to sustaining such a course Stakeholders involved in sustaining activities Deans, Associate Deans and Coordinators of graduate programs. CEOs, Cancer Care Agencies. Heads, Psychosocial Oncology/Supportive Care clinical programs. Sustainable activity: 2. Sustain the ongoing revision and updating of professional development course through the CAPO/ACOP website Financial resources of CAPO/ACOP may vary as may commitment of any given Board of Directors Involvement of several members of the Board of Directors, with participation based on position rather than individuals should help sustainability. Currently the President, Chair of the Education Committee and 2 additional Board members are involved in the project. CAPO/ACOP has a long history of commitment to professional education Development of educator/researchers’ network will generate interest and enhance sustainability. Establishment of a forum for this network as an integral part of the CAPO/ACOP annual scientific conference and meeting will also contribute to sustainability CAPO President and the Chairperson of the Education Committee 27 References Barr, H. Interprofessional education today, yesterday and tomorrow. Commissioned by the Learning and Teaching Support Network for Health Sciences and Practice from the UK Centre for the Advancement of Interprofessional Education. Blake-Mortimer, J., Gore-Felton, C., Kimerling, R., Turner-Cobb, J. M., & Spiegel, D. (1999). Improving the quality and quantity of life among patients with cancer: a review of the effectiveness of group psychotherapy. European Journal of Cancer, 35(11), 1581-1586. Bottomley, A. (1997). Where are we now? Evaluating two decades of group interventions with adult cancer patients. Journal of Psychiatric & Mental Health Nursing, 4(4), 251-265. Diekelmann, N. L. (2001). Narrative pedagogy: Heideggerian hermeneutical analysis of lived experiences of students, teachers and clinicians. Advances in Nursing Science, 23(3), 53-71. Fawzy,F.I. (1999). Psychosocial interventions for patients with cancer: what works and what doesn't. European Journal of Cancer, 35(11), 1559-1564. Freeth, D., Hammick, M., Koppel, I., Revves, S. & Barr, H. (2002). A critical review of evaluations of interprofessional education. London: Learning and Teaching Support Network. Glennie, S. & Cosier, J. (1994). Collaborative inquiry: Developing multidisciplinary learning and action. Journal of Interprofessional Care, 8(3), 255-263. Krist-Janson, L., Dudgeon, D., Nelson, F., Hentelff, P. & Balneaves, L. (1997). Evaluation of an interdisciplinary program in palliative care: addressing the needs of rural and northern communities. Journal of Palliative Care, 13(3), 5-12. Lane, J. S. (1998). Medical cost offset: A review of current research and practices. Preferred Mental Health Management. Lechnyr, R. (1993). The cost savings of mental health services. EAP Digest, 22. Meyer, T. J., & Mark, M. M. (1995). Effects of psychosocial interventions with adult cancer patients: A meta-analysis of randomized experiments. Health Psychology, 14, 101-108. Simpson, J. S. A., Carlson, L E., & Trew, M. (2001). Impact of a group psychosocial intervention on health care utilization by breast cancer patients. Cancer Practice, 9(1), 19-26. Sobel, D. S. (2000). The cost-effectiveness of mind-body medicine interventions. Progress in Brain Research, 122, 393-412. 28 Appendix A List of Individuals Providing Endorsement (Letters enclosed) Name Mr. Don Ford Dr. Peter Vaughan Glenn Davis (for Pam Trainor & Susan Graham) Dr. Barbara Downe-Wamboldt Dr. Wanda Thomas Bernard Dr. Eric Beresford Dr. Cheryl Gibson Dr.Vernon Curran Dr. Sandra LeFort Drs. Luc Belanger & Pierre Gagnon Dr. Robert Bell Ms. Sue Mathews Dr. Diane Doran Dr. Terrence Sullivan Dr. Bill DuPerron Dr. Gayla Rogers Dr. George Browman Ms. Marlene Mysak Mr. Craig Knight Dr.Simon Sutcliffe Dr. Patricia Boston Dr.Graham Riches Dr. Marvin Krank Dr. Joan Bassett-Smith Dr. Daniel Salhani Ms. Pamela Faulkner Baker Ms. Eugenia Repetur Moreno Organization & Province CEO, Capital District Health Association-Queen Elizabeth II Health Sciences Centre, Nova Scotia Chief Health Human Resource Officer, Department of Health, Nova Scotia Co-Chairs, Atlantic Advisory Committee, on health Human Resources, Nova Scotia Director, School of Nursing, Dalhousie University, Nova Scotia Director, School of Social Work, Dalhousie University, Nova Scotia President, Atlantic School of Theology, Halifax, Nova Scotia Dean, Faculty of Nursing, UNB, Fredericton, New Brunswick Co-Director, Centre for Collaborative Health professional Education, Faculty of Medicine, MUN, St. John’s, Newfoundland Director, School of Nursing, MUN, St. John’s, Newfoundland Director, L’Hotel-Dieu de Quebec Research Center, Laval, Quebec & Director Research Team in palliative care. President & CEO, University Health Network, Toronto General Hospital, Toronto, Ontario Provincial Chief Nursing Officer, Ontario Ministry of Health and Long Term Care Interim Dean, Faculty of Nursing, University of Toronto, Ontario President & CEO, Cancer Care Ontario, Toronto, Ontario Director, Education & Immigration, Workforce Policy and Planning, Alberta Health and Wellness, Edmonton, Alberta Dean, Faculty of Social Work, University of Calgary, Alberta Director, Tom Baker Cancer Centre, Calgary, Alberta & Vice-President, Alberta Cancer Board Senior Leader, Clinical Services & Nursing Practice, Tom Baker Cancer Centre, Calgary, Alberta ADM, Strategic Policy, Legislation and Intergovernmental Relations, BC Ministry of Health. President, British Columbia Cancer Agency, Vancouver, BC Faculty of Medicine, University of British Columbia, Vancouver, British Columbia Director, School of Social Work, University of British Columbia, Vancouver, British Columbia Dean, Graduate Studies, University of British Columbia, Okanagan, BC Dean, Faculty of Health and Social Development, University of British Columbia, Kelowna, BC Acting Dean, Faculty of Health and Social Development, University of British Columbia, Kelowna, BC President, Canadian Association of Nurses in Oncology , Vancouver, BC President,Canadian Association of Social Workers, Ottawa, Ontario (original sent separately) 29 Appendix B Project Management Committee Members Dr. Deborah McLeod (Project Co-Lead), Capital Health Cancer Care Program, Dalhousie University, CAPO Board of Directors (Chairperson, CAPO Education Committee) Dr. Barry Bultz Director, Department of Psychosocial Resources, Tom Baker Cancer Centre Adjunct Professor and Chair, Division of Psychosocial Oncology, Department of Oncology, Faculty of Medicine, University of Calgary. Dr. Susan Cadell, Assistant Professor, School of Social Work and Family Studies, The University of British Columbia Dr. Serge Dumont (Project Co-Lead),, Professor, School of Social Work, Université Laval and CAPO Board of Directors (member) Ms. Esther Green, Chief Nursing Officer and Director of Health Human Resource Planning, Cancer Care Ontario, Toronto. Adjunct Faculty, University of Toronto and McMaster University. President of CAPO. Dr. Andrew Padmos, Head, Capital Health Cancer Care Program, Commissioner Cancer Care Nova Scotia, Vice-President, Research and Academic Affairs, Capital Health, Associate Dean, Cancer Care programs, Faculty of Medicine, Dalhousie University. Dr. Gary Rodin, Professor of Psychiatry, University of Toronto, Head of the Behavioural Science and Health Research Division. Head, Psychosocial Oncology and Palliative Care Program at the University Health Network (Princess Margaret Hospital). Expert Panel Nova Scotia Brenda Richard, Ph.D., Director (acting), Maritime School of Social Work, Dalhousie University. Jody Clarke, Ph.D. Professor of Pastoral Studies and Director of Supervised Field Education, Atlantic School of Theology, Halifax, Nova Scotia. Janice Howes, Ph.D., Psychologist, Department of Psychology, QEII Health Sciences Centre and Assistant Adjunct Professor, Department of Psychology, Dalhousie University. Emmie Luther-Hiltz, Co-ordinator Patient Family Network, Cancer care Nova Scotia. 30 Deborah McLeod, Ph.D., R.N., Clinician Scientist (Nursing), Capital Health Cancer Care Program, Assistant Professor, School of Nursing, Dalhousie University, CAPO Board of Directors (Chairperson, CAPO Education Committee) Ruth Martin Misener, M.N., Ph.D.(c), DOCHN, RN. Associate Director, Graduate Programs, School of Nursing, Dalhousie University. Douglas Sinclair, MD, CCFP [EM], FRCPC. Associate Dean, Continuing Medical Education, Faculty of Medicine, Dalhousie University. Chief of Pediatric Emergency Medicine at the IWK Health Centre. New Brunswick Karen Tamlyn, Professor & Assistant Dean, Undergraduate programs, Faculty of Nursing Newfoundland Pamela Faulkner Baker, B.N., M.N., R.N. President, Canadian Association of Nurses in Oncology. Health Services Consultant, Canadian Council on Health Services Accreditation, (CCHSA), Surveyor. Sandra Lefort, Ph.D., R.N., Associate Professor and Director, School of Nursing, Memorial University. Quebec Michele Aubin, MD, FRCPC. Professor, Faculty of Medicine, Laval University. Serge Dumont, Ph.D., Professor, Faculty of Social Work, Laval University Lise Fillion, Ph.D., Professor, Faculty of Nursing, Laval University Pierre Gagnon, MD, FRCPC. Psychiatrist, L'Hotel-Dieu-de-Quebec and Professor, Faculty oif Pharmacy, Laval University. Josée Savard, Ph.D. Professor, School of Psyhcology, Laval University Carmen Loiselle, Ph.D., Assistant Professor, School of Nursing, McGill University Ontario Mary Elliott, MD, FRCPC, Staff Psychiatrist and Head of Resident Training, Department of Psychosocial Resources and Palliative Care, Princess Margaret Hospital. Esther Green, M.Sc.(T), R.N., Chief Nursing Officer, and Director of Health Human Resource Planning, Cancer Care Ontario. Adjunct Faculty, University of Toronto and McMaster University. President of CAPO. 31 Doris Howell, Ph.D., R.N., Assistant Professor, Faculty of Nursing, University of Toronto and Oncology Clinical Track Leader in the ACNP program, RBC Financial Group Chair, Oncology Nursing Research, University Health Network (Oncology and Hematology Divisions of PMH), Toronto, Ontario. Gary Rodin, MD, FRCPC, Professor of Psychiatry, University of Toronto, Head of the Behavioural Science and Health Research Division. Head, Psychosocial Oncology and Palliative Care Program at the University Health Network (Princess Margaret Hospital). Alberta Barry Bultz Ph.D., C.Psych., Director of the Department of Psychosocial Resources at the Tom Baker Cancer Centre of the Alberta Cancer Board. Adjunct professor in the Departments of Surgery and Psychiatry, Faculty of Medicine, University of Calgary; adjunct professor and chair of the Division of Psychosocial Oncology, Department of Oncology, University of Calgary. Jeannette Waegemakers Schiff, Ph.D., Associate Professo, Faculty of Social Work, University of Calgary Helen MacRae, Ph.D., Clinical Psychologist, Tom Baker Cancer Centre, Dept. of Psychosocial Resources and Adjunct Assistant Professor Faculty of Medicine. Calgary, Alberta Guy Pelletier, Ph.D., Clinical Psychologist, Tom Baker Cancer Centre, Dept. of Psychosocial Resources and Adjunct Assistant Professor, Faculty of Medicine, Calgary, Alberta. British Columbia Susan Cadell Ph.D. Assistant Professor, School of Social Work and Family Studies, The University of British Columbia Grant Charles, Ph.D., Assistant Professor, School of Social Work and Family Studies, University of British Columbia, Vancouver Gina MacKenzie, MSW, Professional Practice Leader, Patient and Family Counselling, Lower Mainland Cancer Centres, BC Cancer Agency. Carole Robinson, Ph.D., R.N., Associate Professor, Faculty of Health & Social Development (Nursing), University of British Columbia, Okanagan. Daniel Salhani, Ph.D., R.N. Acting Dean, Faculty of Health and Social Development and Director, School of Social Work, University of British Columbia Okanagan. Patient/Family Representatives: (4 from different provinces) 32 Learner Representatives: 2 graduate students (nursing/ psychology/social work/pastoral care) 1 representative from each group of the following professionals: family medicine, oncology, oncology nursing, social work. Professional Representatives 1 Representative from: Canadian Association of Pastoral Care and Pastoral Education Canadian Association of Nurses in Oncology College of Family Physicians of Canada Canadian Psychological Association Canadian Association of Social Work 33