Collaborative Care For Seriously Mental Ill Consumers
advertisement

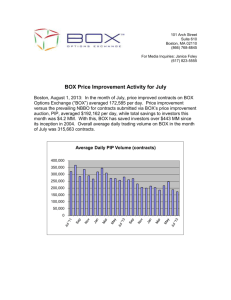
DRAFT #7 -Collaborative PIP Collaborative Care For Seriously Mental Ill Consumers MHO: Verity Integrated Behavioral Health Care System Project Leader: Charmaine Kinney Telephone: 503-988-5464 x24424 Study Period: April 2008-April 2009 Introduction: The selected clinical-focused Performance Improvement Project, (PIP) is titled “Increasing Coordination and Integration of Medical and Mental Health Services”. This project will examine whether case management increases Primary Care Physician (PCP) visits and decreases urgent and emergency care for Serious and Persistent Mentally Ill individuals. Two models will simultaneously be implemented. Model A will be a face-to-face venue within a behavioral health setting. A Registered Nurse (RN) who has experience in both medical and mental health will be place into a behavioral healthcare setting to screen and assist clients in establishing care with a PCP. Model B will be a telephonic model with limited face-to-face contacts utilizing an Exceptional Needs Care Coordinator (ENCC) who is also a RN. Both nurses will screen clients for physical health risk, which will include not having an established Primary Care Physician, (PCP) and/or identification of a physical health care concern. The nurses will help establish care with a PCP and coordinate care between the physical health care and mental health care provider until the patient is fully established with a PCP and major concerns are addressed. Project participants include Care Oregon Fully Capitated Health Plan, (FCHP), and Kaiser Physician Care Organization, (PCO) Verity Mental Health Organization (MHO) and two mental health agencies in the Verity Network, LifeWorks Northwest and Cascadia Behavioral Healthcare System. The AIM of this PIP is to have 65% of enrolled clients have an encounter with a PCP within 12 months after enrollment into the medical risk project, if they have not seen a PCP within the 12 months prior to enrollment, or if the RN case manager identifies a physical health concern. Step 1.1. The topic was based on relevant information The topic must reflect the demographics, prevalence of diagnoses, potential risks, or service needs of the MHO’s Medicaid population. Recent literature reveals the following: Collaboration between Physical Health and Mental Health Providers is a national concern. As early as 1999 the Surgeon General of the United States began recommending integration of these health care delivery systems. The Institute of Medicine recommends that collaboration and coordination of mental health and physical health services be the norm, not the exception. There are numerous national public health reports and studies, on conditions and risks for specified populations, which demonstrate the need for mental health and physical health collaboration as well as the potential benefits of such collaborations. (NASMHPD, 2006) Adding to the challenge of creating an integrated and coordinated system, clients with psychotic disorders or major mood disorders may be unable to build a lasting relationship with a Primary Care Provider in a medical health setting due to symptoms of paranoia, isolation, or depression. (NASMHPD) The Addictions and Mental Health Division (AMH), Division of Medical Assistance Programs (DMAP), and the Public Health Division, (PHD), have been working with many partners on a variety of initiatives that relate to behavioral health and primary care. We know there are consequences when care is not well integrated and coordination across behavioral health and physical health systems. Mental health Collaborative PIP Page 1 2/17/2016 DRAFT #7 -Collaborative PIP conditions rarely exist in isolation. The mental conditions frequently co-occur with medical illnesses such as heart disease, cancer, diabetes and neurological illnesses. “People with severe mental illness die, on average, 25 years earlier than the general population”. This information has been corroborated by a recent AMH study, which found that in Oregon, people with severe mental illness die, on average, 24.1 years earlier than the general population. Generally, 60% of the premature death in persons with schizophrenia is due to medical conditions such as cardio-vascular, pulmonary, and infectious diseases. (NASMHPD) Barriers to Primary Medical Care have found to contribute to lower health care quality, and reduced medical problem identification. In addition, primary care access did not assure high-quality medical care. (Miller, et al, 8/2003) Barriers include lack of coordination and communication between primary care and mental health providers, training issues for both physical and mental health providers, clients lower level of functioning, and transportation issues. (Bazelon Center for Mental Health Law; Druss, et al, 9/2001; Miller, et al 8/2003). Integrated care was found as an effective intervention to improve health status, coordination, and client and staff satisfaction. (Druss, et al 9/2001) Research has shown that underlying mental health and substance use disorder (SUD) problems account for up to 70% of all PCP visits. The World Health Organization (WHO) and several studies report (Chwastiak, et al, 8/2006) that mental illnesses affect and are affected by chronic conditions such as cancer, heart and cardio-vascular diseases, diabetes, Hepatitis C and HIV/AIDS. (NASMHPD) 1.2. Topic was determined through a systematic selection and prioritization process. Verity reviewed suicide prevention and putting a physical health nurse into a mental health setting as possible collaborative studies. The latter was chosen because the project had already started sponsored by a Care Oregon grant and the possible positive impact to the target population. The collaborative topic was selected due to the high rate of chronic physical illness seen in people with severe mental illness. As stated above research shows that, “People with severe mental illness die, on average, 25 years earlier than the general population”. This information has been corroborated by a recent AMH study, which found that in Oregon, people with severe mental illness die, on average, 24.1 years earlier than the general population. The team determined that in order to affect this statistic that the collaborative project had to work directly with the population in the setting they were most likely to be seen in. Mental health conditions rarely exist in isolation of other medical issues. More intensive case management for this population is needed. The question that remains is telephonic or face-to-face more effective. Interventions to coordinate mental health and physical health concerns in high-risk mental health populations will promote: 1) Timely identification and assessment of the client’s medical conditions 2) Detection of co-morbid medical condition(s) 3) Coordination of medications to decrease negative medication interactions and/or changing medications 4) Coordination in dialogue and efforts in joint treatment plan development between the behavioral and medical care teams and could include: Collaborative PIP Medical physician Psychiatrist RN MSW/counselors Page 2 2/17/2016 DRAFT #7 -Collaborative PIP Care Support Exceptional Needs Care coordinators Others, as appropriate to need 2.1. The MHO has clearly defined the questions the study is designed to answer. a. Does screening and case management of individuals with mental health and physical health concerns increase PCP visits? b. Does screening and case management of individuals with mental health and physical health concerns decrease urgent and/or emergency care usage? c. Is model A, (primarily face-to-face) or model B, (primarily telephonic) more effective? 3.1 Indicators are objective, measurable, clearly defined, unambiguous statements of an aspect of quality to be measured. Population will include all Verity/Care Oregon adult clients being served at selected Lifeworks clinic, and all Verity/Kaiser adult clients being served at any Verity contracted facility who have been screened for medical risk and enrolled in the medical risk project. Indicators below will include a 12 month look-back period to determine medical care appointments prior to enrollment into the medical risk project. a. Model A Numerator: Number of who clients who had a non-emergent encounter with a PCP or seen in a primary care clinic within 12 months after RN case management intervention. Model A Denominator: Total Number of clients screened into the medical risk project b. Model B Numerator: Number of urgent and emergency room visit encounters 12 months after RN case management intervention. This measure will be stratified by those who have had at least one PCP encounter and those who had none. Model B Denominator: Total Number of clients screened into the medical risk project c. Difference of Model A and Model B, PCP and urgent/emergency room encounters. 3.2 The indicators measure changes in health status, functional status, or enrollee satisfaction, or valid proxies of these outcomes Research clearly demonstrates that indicators in 3.1 are good markers that a patient is receiving better continuity of care and serves as a proxy measure of such. Studies show that having regular health care access not only reduces Emergency Room use but also increases health care outcomes through preventative measures. Many of these study findings come from the general Medicaid population who share some of the characteristics of the SPMI population, such as poverty and lack of understanding of the medical system. Improved collaborations between PCP’s and local hospitals has increased Medicaid beneficiaries’ use of regular office visits, reduced Emergency Room visits, and increased healthcare outcomes. In one study, heart disease related Emergency Room visits were reduced by 95% through these collaborative methods. “Partnership for Medicaid, 2005” Research is clearly showing that SPMI clients are dying at a far higher rate than the general population, and that “increased morbidity and mortality are largely due to treatable medical conditions that are caused by Collaborative PIP Page 3 2/17/2016 DRAFT #7 -Collaborative PIP modifiable risk factors such as smoking, obesity, substance abuse, and inadequate access to medical care.” SPMI clients are less likely to seek out medical care in a Primary Care Setting and have a high use of emergency services. This population has a higher rate of risk factors such as smoking, substance abuse, poor nutrition, and other modifiable behaviors. In addition social conditions as a result of their illness, such as homelessness, poverty, trauma, incarceration, and social isolation increase vulnerability factors. The impact of SPMI symptoms like paranoid ideation and disorganized thinking presents an access barrier, from both fear by the client but also misunderstanding and competing demands of providers. (Parks, et al, 2006) Barriers to Primary Medical Care have found to contribute to lower health care quality, and reduced medical problem identification. In addition, primary care access did not assure high-quality medical care. (Miller, et al, 8/2003) Barriers include lack of coordination and communication between primary care and mental health providers, training issues for both physical and mental health providers, client’s lower level of functioning, and transportation issues. (Bazelon Center for Mental Health Law; Druss, et al, 9/2001; Miller, et al 8/2003). Integrated care was found as an effective intervention to improve health status, coordination, and client and staff satisfaction. (Druss, et al 9/2001) Criterion 4.1. The study population is clearly defined so that all the MCO’s Medicaid enrollees who are eligible for the study are included. The target population is all Medicaid clients presenting at behavioral health clinics where a nurse will provide screening for medical risk that is not being addressed, and follow up with case management to connect individuals to a PCP in the health care setting. Clients will sign an acknowledgement that health plans will be exchanging health care data and this will be placed in their charts. Identification of at risk clients will be identified by two methods. First, the case managers at identified agency sites will fill the screening tool at the clinic sites and identify risk concerns with no ongoing medical care occurring. Individuals screened as high risk will be referred to RN at the identified behavioral health clinic, or ENCC at the health plan depending on the model employed at the clinic. Second, the medical health plan will review their risk identification measures and the ENCC will screen clients who are not at the identified face to face site by phone. Clients will be stratified by the LOCUS level of care determination instrument. Criterion 4.2. When the study includes the MCO’s entire eligible population, the data collection approach captures all eligible enrollees. All Medicaid clients will have a risk screening either face-to-face or through other risk screen scoring system. Criterion 4.3. The MCO has described the method for determining the sample size. N/A Criterion 4.4. The sampling methodology is valid and protects against bias. N/A Criterion 4.5. The sample is large enough to allow calculation of statistically meaningful measures. N/A Criterion 5.1. The study design clearly specifies the data to be collected. Criterion 5.2. The data sources are clearly identified. Criterion 5.3. The study design describes a systematic method of collecting valid and reliable data on the entire MCO population to which the indicator(s) apply. Collaborative PIP Page 4 2/17/2016 DRAFT #7 -Collaborative PIP Criterion 5.4. For manual data collection, the data collection instrument provides for consistent, accurate data that are appropriate for the study indicators and that can be used over the study time period. Criterion 5.5. The study design prospectively specifies a data analysis plan Criterion 5.6. For manual data collection, the study design includes the rationale for the data abstraction and the staff qualifications. Collaborative PIP Page 5 2/17/2016 DRAFT #7 -Collaborative PIP Bibliography: Collaborative SMI Care Parks, Joe MD, et al Morbidity and Mortality in People with Serious Mental Illness, National Association of State Mental Health Program Directors (NASMHPD) Medical Directors Council. http://www.nasmd.org/medicaid_mental/docs/NASMHPD_Morbidity_and_Mortality_Report.pdf Miller, Carolyn Levinson, M.P.H., et all, (2003) Barriers to Primary Medical Care Among Patients at a Community Mental Health Center PSYCHIATRIC SERVICES, August 2003 Vol. 54 No. 8. http://psychservices.psychiatryonline.org Koyanagi, Chris, (June 2004) GET IT TOGETHER How to Integrate Physical and Mental Health Care for People with Serious Mental Disorders BAZELON CENTER FOR MENTAL HEALTH LAW pubs@bazelonorgwww.bazelon.org Druss, Benjamin G., MD, MPH, et al (2001) Integrated Medical Care for Patients With Serious Psychiatric Illness, A Randomized Trial. Arch Gen Psychiatry/Vol 58, Sep 2001 Www.Archgenpsychiatry.Com (accessed February, 2008) Chwastiak, Lydia A. M.D., M.P.H., (2006). Interrelationships of Psychiatric Symptom Severity, Medical Comorbidity, and Functioning in Schizophrenia PSYCHIATRIC SERVICES August 2006 Vol. 57 No. 8 http://psychservices.psychiatryonline.org Collaborative PIP Page 6 2/17/2016