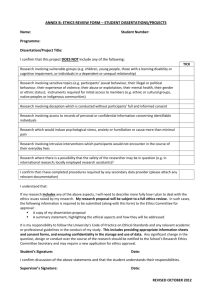
Ethical Guidelines for Research, Consultancy and Project Work
advertisement

___________________________________________________________________________ ETHICAL GUIDELINES FOR RESEARCH, CONSULTANCY AND PROJECT WORK INTRODUCTION Ethical issues may occur in research projects, consultancy work and aspects of taught courses, eg. work placements or special studies. Whilst they are particularly characteristic of practical subjects, e.g. Physiotherapy, Occupational Therapy, Sports and Exercise Science, they may occur in almost any subject. Innovation is being encouraged in taught courses, which may lead to greater use of laboratory and practical techniques or the collection of socio-cultural data. Consultancy work is developing, which sometimes involves people who are neither staff nor students of the University. We are operating in a changing Higher Education environment in which the pressure to engage in research and generate external income is increasing, all of which may lead to projects which raise ethical issues. The following ethical guidelines are intended to ensure that: all students, clients, communities and staff who take part in project work, research and consultancy projects are treated with respect and sensitivity; all project work, consultancy and research activities are covered by our insurance policy and minimise the risk of litigation; project work, research and consultancy activities are in line with appropriate forms of protocol and professional codes of conduct and guidelines. The system is intended to facilitate the work of staff and students and will be operated in an open and responsive manner. ____________________________________________________________________________ OVERVIEW OF THE SYSTEM The ethical review process is summarised in figure 1. It is the responsibility of the member of staff or research student leading the project to consult the guidelines contained within this report. It is expected that all postgraduate and staff research projects will be reviewed against the guidelines. In the case of undergraduate and taught courses, it is expected that the vast majority will fall outside the scope of the guidelines and issues will be decided within the individual Faculties. It is suggested that each Faculty organises their own internal research ethics committee for the reviewing of this work. However if module leaders and project supervisors are in any doubt concerning ethical issues they should always consult with the Research Ethics Sub Committee of the University. The Terms of Reference and Membership of the Research Ethics Sub Committee can be found in the University Committee Directory here. 1 SUMMARY OF ETHICAL REVIEW PROCESS (Figure 1) ____________________________________________________________________________ Researcher, Teacher, Research Cluster Consult and follow guidelines If the guidelines indicate the study is not permissible, stop or restructure the proposal If guidelines indicate the study is clearly permissible without submission to the Research Ethics Committee proceed with the project Submit a formal proposal to the Research Ethics Committee if: The guidelines indicate that submission is mandatory for the type of work proposed. You have any doubts about the application of the guidelines to the project in question. The Chair of the Research Ethics Committee will advise on submissions. Research Ethics Committee decision is made in writing within 28 working days Appeals procedures available in exceptional circumstances 2 A - EXPECTATIONS FOR ALL RESEARCH, TEACHING AND CONSULTANCY ACTIVITIES AT THE UNIVERSITY All work with volunteers, students, clients and communities should be guided by the following criteria:1. That the welfare of the volunteer/client/community representative is paramount. 2. All procedures should follow U.K. law (e.g. The Data Protection Act, 1984). 3. The proposed project should be covered by the insurance policy of the University. 4. All procedures should be in line with the recommendations of the appropriate community, academic or professional bodies (e.g. COT; CSP; Royal Commission for Aboriginal Peoples 1993 ethical guidelines for research). 5. The work should conform to the “Declaration of Human Rights and the Covenants on Human Rights or, where appropriate, Islamic Declaration of Human Rights” (UN General Assembly, December 1984; Vienna Declaration, 1993). Appendix 1 6. All subjects and clients should be told the purpose and nature of the research or consultancy work with its potential benefits put in the context of any potential risk. Participants should be fully informed of any data gathering techniques to be used. For studies involving subject deception appropriate debriefing mechanisms must be established. 7. Informed consent should be obtained in writing for all research or clinical work, especially where there is a degree of risk for the subject. 8. All subjects and clients should be given the opportunity to withdraw from any project and not be obliged to explain their decision. 9. Confidentiality and anonymity should be provided for the subjects and clients. When this is not possible subjects must be informed as part of the informed consent procedure. Press and media coverage of any project must be constructed in such a way as to protect the anonymity and confidentiality of subjects, except where express permission has been given in advance. 10. All projects should include an appropriate evaluation procedure. This must include the reporting to the Research Ethics Sub Committee and Health and Safety Officer of any harm suffered by a volunteer in a project conducted at the University. 11. Information on the sources of funding should be freely and transparently available. Sponsors should not exert pressure which compromises the academic freedom of the research, consultancy or project work. 12. Projects which include collaboration with other organisations (e.g. hospitals, community associations) may also need to seek approval from their Ethics Committees. In collaborative research, researchers should establish procedures to enable participants to take part in the planning, execution and evaluation of research results. In community-based studies, researchers should ensure that the multiplicity of community experiences and perspectives is represented. 13. All projects should be run with reference to the University’s health and safety and equal opportunities policies. Questionnaires and procedures should be screened to ensure that there is no inappropriate racial or sexual bias. 14. Students should be treated with the same degree of care as volunteers from outside of the University and paying clients with the same degree of care as unpaid volunteers. Student special studies which contain an element of risk should be treated in the same way as staff projects. ____________________________________________________________________________ 3 B - WORK THAT CAN BE CONDUCTED AT THE UNIVERSITY WITHOUT SUBMISSION TO THE UNIVERSITY RESEARCH ETHICS SUB COMMITTEE. Many projects conducted at the University which follow the guidelines above will not need to be submitted to the University Research Ethics Sub Committee (though will probably need some form of internal Faculty review). To help colleagues identify these areas the following guidelines are given. However, if there is any doubt, an application should be made. The Chair of the Research Ethics Sub Committee will advise on the need to submit an application. Work in the following categories can normally be conducted without a submission to the Research Ethics Sub Committee:1. That which contains minimum risk to the subjects’ health or welfare. This would include most questionnaires, interviews and focus groups unless they covered areas that can be reasonably considered controversial topics. Research must respect the privacy and dignity of all participants and take into account the knowledge and experience of all who take part. 2. That which can be demonstrated to be normal professional practice and which has been shown by past experience not to require specific ethical approval. This would include anthropometric measures and standard laboratory demonstration contained in standard text books. ____________________________________________________________________________ C - WORK WHICH SHOULD NOT BE CONDUCTED AT THE UNIVERSITY. Normally work that breaks any of the guidelines in section A will not be permitted at the University unless an exceptional case can be made to the Research Ethics Sub Committee. In addition the following activities are prohibited:1. Those in which the risk to the subject’s health or welfare is demonstrably excessive. 2. Those which would bring the University into disrepute. 3. Those which involve experimentation on animals when other methods are available. 4. Those where it is judged that the freedom of the research is likely to be compromised by pressure from sponsors. ____________________________________________________________________________ D - WORK WHICH MUST BE SUBMITTED TO THE RESEARCH ETHICS SUB COMMITTEE. The following guidelines are designed to identify those projects which must be submitted to the Research Ethics Sub Committee:1. Those projects which are not clearly covered by the guidelines described in section B or in which a reasonable degree of ambiguity exists as to whether the work holds minimum risk or is normal professional practice. 2. Those projects in which there is a potential risk to the health, welfare or sensitivity of the volunteers and participants. 3. Projects including invasive procedures involving any risk to the health and welfare of the volunteer (e.g. blood sampling). 4. Questionnaires, interviews or focus groups the nature of which might be offensive, distressing or deeply personal. 5. Proposals which may endanger the physical or mental health of the staff involved. 6. Projects which involve financial payment or payments in kind to the volunteers. 7. Research proposals to be carried out by persons unconnected with the University but wishing to use staff and/or students as volunteers. 4 8. Those projects in which one of the standing guidelines in section A of this report will not be followed. 9. Projects involving work with children outside normal classroom practices, unless previous authorisation has been given. ____________________________________________________________________________ Maintained by: Research QA Ref: RES5 Last updated: December 2008 5 Appendix 1 HUMAN RIGHTS ACT (summary) 1998 Human Rights Act. 2000 October, enforceable in UK. This act incorporates most of the provisions of the European Convention on Human Rights into English law, the main provision of which we need to be generally aware of. As a very brief guide the following Articles of this law may effect how health care works, Article 2 3 5 6 8 9 10 12 14 right to life prohibition of torture right to liberty and security right to a fair trial right to respect for private and family life freedom of thought, conscience and religion freedom of expression right to marry prohibition of discrimination These can be further expanded on by including rights which offer an absolute prohibition - 3, 12 & 14 those which are subject to specific exceptions - 3, 12, 14, 2, & 5 individual right which can be balanced against the rights of others or society's interests - 8, 9 & 10. There is also a need to interpret 'the right' and the extent to which 'the right' imposes a positive obligation on the state, in our case the English law. All this means that English medical law is no longer just that, it has to consider, and apply where appropriate arguments of other European signatories. However there is no distinct 'stand alone' European medical law. The nearest to such a directive is the European Convention on Human Rights and Biomedicine. As yet the UK has not affirmed to this part of the Act. There appears to be a general tendency to avoid enshrining medical human rights into law, and instead a preference for setting up separate 'governing bodies' e.g. The Warnock Committee, HFEA, House of Lord's Select Committee on medical ethics examining euthanasia and issues surrounding dying, The Human Genetics Commission etc. The upshot of this seems to be that many decisions are made on the basis of - this applies to patient 9 (a) only, is not case law and cannot be used in any similar application. However these 'Judge' type decisions are often used as arguments for subsequent dilemmas. Maybe we should consider that appealing that a basic human right should be to have a level of consistency within that medical law which affects individuals. Other specific areas where the support of the Human Rights Act can be sought are: access to fertility treatment allocation of resources assistance in committing suicide/physician assisted suicide claim to treatment confidentiality conscience consent, withdrawal of consent discrimination disposal of body parts health professionals, consistency of actions foetus (rights of) 6 human genome integrity of the person incompetent patient parental rights assisted conception choice in dying. Additional information can be found at the following websites: Human Right Acts (1998) http://www.hmso.gov.uk/acts/acts1998/19980042.htm European Court of Human Rights http://www.echr.coe.int/ Islamic and Middle Eastern Law Materials on the Net http://www.soas.ac.uk/Centres/IslamicLaw/Materials.html (Guidelines approved by Academic Board, June 2004) 7 Appendix 2 PROTOCOL FOR USING INTERNET RESEARCH RESOURCES 1. All research undertaken within the University, which uses the internet, must adhere to the University’s current Acceptable Use Policy (see below for the most recent policy). Where access to material, which contravenes this policy, is required for academic research or study, clearance must be obtained, prior to any access, via the Research Ethics Sub Committee. In this context this means the use of University resources for assessing, viewing and/or downloading, for example, pornographic, racist, homophobic or extreme right-wing materials. It must be noted that permission may not be granted. 2. If unintended or unanticipated access occurs then the Dean of Faculty and IT services must be contacted immediately. Unauthorized use is a disciplinary offence. The University’s IT Acceptable Use Policy, approved by the Senior Management Team in November 2008, is available from the Staff Information Point or via the following link http://www2.yorksj.ac.uk/aup/aup2008.doc 8