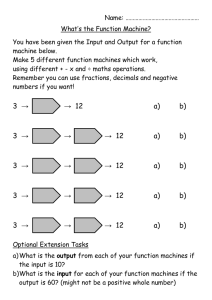
A. Required
advertisement

急診醫學科(部)住院醫師訓練計畫書 壹.簡介 急診醫學在台灣之發展肇始於民國七十八年。由於急診人口之急速增加 以及民眾對急診醫療品質之要求提昇,造成急診醫學之發展有其特殊性及迫 切之需要性。從民國七十八年至民國八十六年,此段時間為急診醫學之孕育 期。及至民國八十七年,有鑑於急診醫學專科醫師對急診醫療品質提昇之卓 越貢獻,以及社會大眾對良好急診醫療品質之殷切盼望,衛生署正式頒佈及 公告急診醫學專科為衛生署認定之原始專科,急診醫學專科醫師制度於是正 式宣告開始。然而急診住院醫師之訓練仍缺乏一套完整細緻之制度及計劃, 每家急診專科訓練醫院根據其特色及理念,均發展出一套具有「特色」的訓 練制度。一般而言,訓練制度大致可分為二大類,一為五年制訓練計劃,即 完成內科、外科或家醫科之專科醫師科訓練後再接受二年急診專科醫師訓 練。此制度的特色有二:一、將急診視為其他專科之次專科,二、急診專科 醫師養成過程大部分的時間均在病房。此制度的好處在於對單一疾病認識較 為情深,但是卻容易失去其對疾病認識之廣度,再則其他專科之思考養成訓 練與急診專科並非全然相同,因此往往會造成衝突。第二種訓練制度為橫向 性教學之急診醫學教育體系,住院醫師急診部門內「全科性」之學習及急診 醫師「不分科」之值班制度。次制度最大的特色即從「你的病患」身上直接 學習,用最短的時間,最有效率的方法,於三年內學習急診醫學之大部分內 容。此制度的成功關鍵在於必須有熱情、善於教學且學有專精之急診主治醫 師給於住院醫師適時、適地、適人之教學與完善且堅定的教育制度。本院急 診科即取用此一教學制度。 本院急診科醫師採「不分科」之值班制度以相應住院醫師之訓練制度, 每班均有急診專科主治醫師給予住院醫師臨床指導,而本院急診處之規劃及 硬體設施實已達醫學中心之水準。又本科與新光吳火獅紀念醫院急診科以建 1 教合作之方式,讓住院醫師能接觸、學習不同類型之病人與疾病,相信此一 教育制度,必能訓練出傑出之急診醫師。 總言之,大林慈濟醫院急診醫學科之教育訓練精神在「養將不養兵」, 透過慎密之思考及研究,發展新的知識,傳授已成熟之新知,進而為國內急 診醫學界注入源源不斷之新血。 「如臨深淵,如履薄冰」 ,是大林慈濟急診醫 學科全體教學人員從事教育時心情之寫照。期盼在急診醫學之未來發展裡, 本院急診醫學科能扮演著重要且必要之「繼往開來」的角色。 2 訓練計畫概要 一.急診醫學專科住院醫醫師訓練 (一)期間:三年 (二)資格:醫學院畢業之醫學系學生,必需於受訓期滿一年內取得國家 醫師考試之資格或已取得國家醫師考試通過之證明者。 (三)目的:課程之目的在培養急診醫學專科醫師,故訓練之內容完全符 合衛生署急診醫學專科醫師甄審委員會之規定。 (四)訓練內容:如附件一 (五)訓練容量:每一名急診專科醫師可訓練二名住院醫師 (六)訓練成果之評估 1.由急診醫學科主任及主治醫師,於招訓住院醫師時予以甄試,擇 優者錄取。 2.訓練期間定期由專兼任教師予以考核,評分,每年並舉行筆試以 為公正之評量。 3.定期以問卷方式敦請住院醫師對指導教師及訓練計劃內容予以 評估。 4.本院教育研究及發展委員會定期對急診醫學科之授課內容予以 評估 5.急診醫學科之教育訓練計畫,依衛生署專科醫師甄審委員會之決 議,需逐年修訂。 6.各式評估表如附件二,評估結果登錄於科內考核記錄表中。 (七)急診醫學科各職級住院醫師訓練排程表。(附件三) (八)科內學術會議及其他教學活動概況。(附件四) (九)授課資料及必讀書籍。(附件五) 3 Emergency Medicine Residency Training: Goals, Objectives & Core Content Introduction Injury or illness may strike at any time, day or night. Whenever patients, their families, or bystanders feel the condition is an EMERGENCY they quickly rush the patient to hospital. As a result the sickest or most severely injured victims usually present first to the Emergency Department for help. The speed and correctness of decision making by the "first contact medical personnel" is frequently the prime determinant of whether or not the patient has a successful outcome. This is why we like to focus on the "Right Patient, Right Place, Right Time." In light of what we have just said it is clear that you need a physicians with the knowledge, skill, and experience to be able to handle all kinds of emergency situations 24 hours per day, 365 days per years. While it is possible that very large hospitals could support, both financially and in patient volume, subspecialty Emergency Attendings in Medicine, Surgery and Pediatrics 24 hours per day, the majority of hospitals cannot. The logical solution is to train horizontally integrated Emergency Physicians capable of responding to all kinds of emergencies with appropriate and rapid backup support as required by other specialties. This is less daunting than it seems as many skills are readily transferable with minor modifications, such as airway management for trauma or non-trauma patients or the management of shock in a diffuse array of conditions. Having expertise in early trauma care, pediatric emergencies, medical emergencies and those selected emergency conditions that may occur in other subspecialty fields, Emergency Physicians are best suited to provide the medical leadership for Emergency Medical Services and staff the majority of Emergency Departments. The purpose of this document is to ensure our future graduates have the necessary knowledge and skill base to meet these objectives. The course content and procedures to be included in all Emergency Resident Training Programs in the Shin Kong Wu Ho-Su Memorial Hospital are outlined. 4 Formatted Approach to Evidence-Based Emergency Medicine Residency Training 1. Procedural Skills A. Required B. Optional 2. Basic Knowledge Overview of syndrome or specific disease, including etiology, pathophysiology, clinical pictures/presentation, differential diagnosis, treatment, complication, etc. This basic knowledge could be provided by participation in lectures, seminars, journal readings, textbook reading, or case-based learning. A. Required B. Optional 3. Symptom-Based Approach Learned through cases seen by trainee, with initial presentation of the following symptoms (e.g. chest pain, respiratory distress), which need differential diagnosis and immediate management even when the definitive diagnosis has not yet been made. Also by M+M rounds, symptom based core lectures and formal reading. A. Required B. Optional 4. Disease or Syndrome Specific Evaluation and Management Learned through case rounds, core lectures and textbook and journal reading, but more firmly imprinted on the resident's mind by trainee-managed cases whose final diagnosis or tentative syndrome have been confirmed after initial evaluation and management in the ED, ICU, or in the ward. This requires a 5 system of individual case follow up by the treating physician. A. Required B. Optional Some diseases may not be seen because of prevalence or epidemiological reasons during the 3-5 years of emergency training. These cases are categorized as optional, but at least one third of the cases of listed optional diseases/syndromes are required to be managed by the trainee. 5. Diagnostic Tools This is one area of evidence-based medicine that requires stress during training and need a clear understanding of pre-test likelihood of the disease in your patient the likelihood ratio of your chosen diagnostic test for predicting. The presence or absence of said disease now gives you a posttest likelihood of the disease. Depending on the potential seriousness of the disease and risk /benefit ratio and cost of treatment, you are now ready to make a reasoned decision about the need for a given test. A. Required B. Optional 6. Pharmacological Agents Drug therapy requires the same evidence-based approach. This is especially true given the large number of newer and more expensive drugs. Valid studies (preferably not drug company supported) must be analyzed to determine the risks versus benefits of one therapeutic agent over another. A. Required B. Optional 6 Training Objectives in Gastrointestinal Disorders 1. Procedural Skills A. Required (1) History taking/ Physical exam. (2) NG/Blakemore ( or similar tube) insertion (3) Paracentesis (4) Screening abdominal echo (5) Gastrograffin /Barium swallow (6) Perianal abscess I& D B. Optional (1) Panendoscopy (2) Anoscopy/Proctoscopy 2. Basic Knowledge A. Required (1) Functional anatomy and physiology of digestive systemesophagus, stomach, small bowel, colon, liver, pancreas and gall bladder. (2) Pain pattern, location and related diseases. B. Optional (1) Parenteral nutrition 3. Symptoms- Based Approach A. Required (1) Epigastric/Abdominal pain (2) Nausea/Vomiting/Heartburn (3) Diarrhea/Constipation (4) GI bleeding (Hematemesis/Hematochezia/Melena) (5) Hepatomegaly/Jaundice (6) Abdominal distention/Ascites (7) Dysphagia/odynophagia (8) Hiccough (9) Anorexia/Weight loss 7 B. Optional None 4. Disease or Syndrome- Specific Evaluation amid Management A. Required 1. Esophageal Disorders (1) Dysphagia/odynophagia/spasm (2) Esophagitis/reflex/EV bleeding (3) Foreign body ingestion (4) Obstruction/Boerhaave's syndrome 2.Gastfic/Duodenal Disease (1) Gastroparesis (2) Gastritis (3) Peptic ulcer disease (a) Gastric erosion/ulceration (b) Duodenal ulcer (4) Pyloric stenosis (5) Upper GI bleeding (a) Mallory-Weiss tears (b) Esophageal/gastric varices (c) Hemorrhagic esophagitis/gastritis/duodenitis (d) Bleeding gastric/duodenal ulcer (e) Aortoenteric fistula of GI tract 3.Disorders of the Small/Large Bowel (1) Bowel obstruction (2) Hernias (a) Inguinal/femoral/umbilical (b) Incarcerated/strangulated (3) Infectious gastroenteritis (a) Bacteria/viral/parasitic (b) Toxin (c) Staph/scromboid (4) Intussusception (5) Appendicitis/mesenteric adenitis (6) Inflammatory bowel disease 8 (a) Regional ileitis( Crohn's disease) (b) Ulcerative colitis (c) Pseudomembranous antibiotic associated enterocolitis (7) Mesenteric thrombosis/infarction/irradiation colitis (a) Ischemic colitis (8) Disorder of colon motility (a) Irritable bowel syndrome (b) Diverticular disease (c) Constipation/obstipation/impaction (9) Volvulus (a) Sigmoid/cecal (10) Perforation (a) Peptic ulcer (b) Gall bladder (c) Small bowel (d) Large bowel (11) Anorectal disorders (a) Hemorrhoids/anal fissures (b) Abscess/fistulas (c) Proctitis (d) Rectal prolapse (e) Foreign bodies (12) Lower GI bleeding (a) Inflammatory bowel disease (b) Diverticular disease (c) Anorectal lesions (d) Neoplasms (e) Meckel's diverticulum 4. Disorders of the liver/bilitary tract/pancreas (1) Hepatitis (a) Viral/toxin (2) Hepatic faliure/cirrhosis (a) Spontaneous bacterial peritonitis (3) Hepatoma (a) Spontaneous bleeding/rupture (4) Alcoholic liver disease 9 (5) Cholecystitis/cholangitis (6) Gallstones (7) Pancreatic disease (a) Acute/chronic (b) Pseudocyst (c) Tumor 5.Antibiotic associated colitis B. Optional 1.Angiodysplasia of GI tract 2.Traveler's Diarrhea 3.Megacolon (a) Congenital (b)Acquired 4.Malabsorption 5. Diagnostic Tools A. Required 1.Interpretation liver enzyme (biochemistry data: GOT, GPT, alk phosphate, bili & amylase, etc) 2.Interpretation of KUB, abdominal series, esophagogram, abdominal echo , abd CT B. Optional 1. Interpretation of RIA Data ( B markers, AFP, CEA ) 2. Interpretation of upper& lower GI series 3. Interpretation of angiography 6. Pharmacological Agents A. Required 1. Antacids 2. H2 Receptor Antagonists/Sucralfate 3. Antimicrobials 4. Antidiarrheals 5. Antiemetics 6. Antispasmodics/Anticholinergics/Analgesics 7. Stool Softners 8. Vasopressin/Sandostatin ondateron/Hepatitis prophylaxis 10 thiamine/Multivitamins/Folic acid 9. Lactulose 10. X-ray Contrast Media B. Optional 1.Enzymes/Digestant 2.Antiflatulents 11 Training Objectives in Cardiovascular Emergencies 1. Procedural Skills A. Required 1.Cardiovascular physical examination - including recognition of sounds/ murmurs/rubs/ waves 2.Arterial line insertion & monitoring 3.CVTI insertion (subclavian & internal jugular) 4.Defibrillation/ Cardioversion 5.Transcutaneous cardiac pacing 6.Pericardiocentesis 7.Screening cardiac echo (identify cardiac tamponade and gross wall motion abnormality) B. Optional 1. Swan-Ganz insertion 2.Doppler vascular studies 3.Transvenous pacemaker 2. Basic Knowledge A. Required 1.Cardiac anatomy 2.Frank-Starling law 3.Chronotropic/ Inotropic medication 4.Afterload/ Preload 5.Pacemaker cell action potential B. Optional 1.Congenital abnormality development 3. Symptom-Based Approach A. Required 1.Chest pain 2.Syncope 3.Palpitations 4.Peripheral edema 5.Dyspnea/ cyanosis 12 6.Hypotension 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1.Ischemic heart disease (a)Angina (b)Myocardial infarction 2.Congestive heart failure (a)Hhigh output (b)Low output (c)Cor pulmonale 3.Diseases of the heart/ Pericardium (a)Valvular disease (b) Endocarditis (c) Myocarditis (d) Pericarditis (e) Cardiomyopathies 4.Diseases affecting arterial circulation (a)Aneurysm/ dissection (b)Hypertension (acute/ chronic) (c)Arteritis 5.Thromboembolic disease (a) Venous/ arterial (b) Target organs 6.Diseases of conduction system (a)Supraventricular dysrhythmias (b)Ventricular dysrhythmias (c) Conduction blocks (d)Preexcitation syndromes 7.New technologies and their delayed complications (a)PTCA/ stenting/ laser reaming (b)Iimplantable pacemaker/ defibrillator (c) Per cutaneous ablation surgery (d)heart transplants B. Optional 1.Congenital abnormalities (recognition of the need for consultation 13 and the ability to initiate treatment based on hemodynamic findings is adequate) 2.Myocardial manifestations of systemic diseases (a)Endocrine (b)Rheumatologic 5. Diagnostic Modalities A. Required 1. ECG interpretation (a) Basic components (b)Ischemia/ myocardial infarction/ myopericarditis (c) Dysrhythmia (d)Conduction defects (e) Preexcitation syndromes (f) Chamber hypertrophy (g)Drug/ electrolyte effects 2. Chest x-ray interpretation (a) Heart size and shape (b) Mediastinal vessels (c) Pulmonary edema 3. Cardiac sonography (a) Identify pericardial fluid and wall motion 4.Cardiac enzymes interpretation B. Optional 1.Cardiac sonography (a) Identify wall motion abnormailities and valve dysfunction. 2.Doppler studies (a) Arteries/ veins/ heart 6. Phamacologic Agents A. Required 1. Thrombolytics (a) TPA/ streptokinase/ antistreplase 2. Anticoagulants (a) Heparin/ low molecular weight heparin/ warfarin 3. Antiplatelet/ Antiinflammatory agents 14 (a) Aspirin/ NSAID's 4 Analgesic agents (a)morphine/ demerol 5. Nitrates (a) NTG/ isordil 6.lnotropic agents (a) Epinephrine/ dopamine/ dobutamine/ norepinephrine 7.Antiarrhythmic agents (a) Lidocaine/ beta-blockers/ procainamide/ bretylium/magnesium sulphate (b) Adenosine/ verapamil/ digoxin/ atropine 8.Antihypertensive agents (a)Nnitroprusside/ labetalol/ hydralazine (b) Calcium channel blockers/ ACE inhibitors 9.Diuretic agents (a) Loop/ thiazide/ potassium sparing B. Optional l.Unproven or high risk antiarrhythmic agents (a) Amiodarone/ sotalol/ newer experimental drugs 2.Cholesterol lowering agents (a) Cholestyramine/ gemfibrozil/ lovastatin 15 Training Objectives in Cutaneous Disorders 1. Procedural Skills A. Required 1.Incision and Drainage of cutaneous abscess B. Optional 1.KOH prep 2.Use of Wood's Lamp 2. Basic Knowledge A. Required 1. Structure and function of skin 2. Recognition of skin lesion (ex. maculae, papule,pustule...etc.) B. Optional None 3. Symptom-Based Approach A. Required 1.Pruritis 2.Rashes 3.Exfoliation 4.Erythema and Swelling B. Optional None 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1. Infections and Infestations (a)Erysipelas /cellulitis/impetigo (b)Scabies (c)Herpes zoster (d)Toxic epidermal necrolysis (scalded skin syndrome) (e)Viral xanthems 2.Vascular disorders (a)Urticaria and angioedema 3.Drug eruptions 16 (a)Steven-Johnson syndrome 4.Malar "butterfly" rash of SLE 5.Eczema/Dermatitis/Scaling Eruptions (a)Exfoliative dermatitis (b)Contact dermatitis (c)Atopic dermatitis B. Optional 1. Psoriasis 2. Fungal Infections 3. Neoplasms (a)Squamous/basal cell carcinoma (b)Melanomas (c)Kaposi's sarcoma 4. Disorders of sebaceous/sweat glands 5. Diagnostic Modalities A. Required 1.Interpretation of Gram-stain of pus 2.Identification of body lice, scabies and other cutaneous infestations. B. Optional None 6. Pharmacologic Agents A. Required 1. Antihistamine (a)Diphenhydramine (benadryl) 2.Topical steroids 3.Systemic steroids 4.Systemic antibiotics (a)penicillins / cephalosporins 5.Systemic antifungal agents (a)Griseofulvin / ketoconazole 6. Systemic antiviral agents (a)Acyclovir B. Optional 17 1.Pediculicides/Scabicides 2.Desquamating agents 3.Paraaminobenzoic acid 18 Training Objectives in Endocrine, Metabolism, Nutritional 1. Procedural Skills A. Required 1.Bedside glucose quantification B. Optional None 2 . Basic Knowledge A. Required 1.Acid-base homeostasis 2.Glucose metabolism and role of insulin 3.Thyroid function and metabolism B. Optional 1. Pituitary homeostasis 2. Adrenal/Pancreatic function and metalolism 3. Symptom-Based Approach A. Required 1. Hyperpnea/ Kussmaul respiration 2. Myxedema 3. Muscle cramps/Tetany B. Optional 1.General weakness 2.Dehydration 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1.Acid-base disturbance (1) Metabolic (a)Acidosis (b)Alkalosis (2)Respiratory (a)Acidosis 19 (b)Alkalosis 2.Fluid and Electrolyte disturbance (1)Sodium (a)Hypernatremia (b)Hyponatremia (2)Potassium (a)Hyperkalemia (b)Hypokalemia (3)Calcium (a)Hypercalcemia (b)Hypocalcemia (4)Water (a)Excess (edema, SIADH) (b)Dehydration 3.Glucose Metabolism (1)diabetes mellitus (a)DKA (b)Hyperosmolar coma (c)Diabetic lactic acidosis (d)Hypoglycemia (e)DM foot with gangrene (f)Other complications of DM 4.Alcoholic ketoacidosis 5.Adrenal disorders (1)Cushing syndrome (2)adrenal insufficiency 6.Thyroid (1)Hyperthyroidism/thyroid storm (2)Hypothyroidism/myxedema coma (3)Thyroiditis 7.Parathyroid disease 8.Vitamin deficiency (1)Wernicke/Korsakoff syndrome (2)B12 deficiency with pernicous anemia 9.Pheochromocytoma 10.Panhypopituitarism 20 (1) pituitary apoplexy B. Optional 1. Mxed acid-base disorders 2. Magnesium disturbance 3. Phosphorus disturbance 4. Other vitamin deficiencies 5. Diagnostic Modalities A. Required 1. Interpretation of ABG and electrolyte abnormalities 2. ECG changes with electrolyte disturbances B. Optional None 6. Pharmacological Agents A. Required 1.Hypoglycemic agents (1) oral agents (2) insulin B. Optional 1.Magnesium 21 Training Objectives in Environmental Disorders 1. Procedural Skills A. Required 1.History/Physical examination 2.Rapid cooling techniques 3.Rewarming techniques 4.Decontamination ( Radiation exposure) 5.Burn management (a)Airway management (b)Wound care/ dressing/debridement B. Optional 1.Escharotomy 2.Hyperbaric therapy 2. Basic Knowledge A. Required 1.Thermoregulatory mechanisms 2.Radiation theory 3.Altitude/Diving physiology 3. Symptoms- Based Approach A. Required 1 Altered mental status 2 Paresthesias/Paralysis/Motor disorders 3 Muscle cramps/Joint pain 4 Fever 5 Pruritis/Urticaria/Mottled rashes 6 Stridor/Wheezing/Cough 7.Subcutaneous emphysema 8.Dyspnea/Pulmonary edema 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1.Altitude sickness (a)Acute mountain sickness 22 (b)High altitude cerebral edema (c)High altitude pulmonary edema 2.Dysbarism (a)Barotrauma (b)Decompression sickness (c)Recompression therapy 3.Cold disease/Injury (a)Hypothermia (b)Frostbite 4.Heat illness syndrome (a)Heat cramps (b)Heat exhaustion (c) Heat stroke 5.Near-drowning/Drowning 6.Radiation Injury (a)Exposure/contamination (b)Acute radiation syndromes 7.Venom, Bites, Stings (1)Animal bites (a)Rabies prophylaxis (2)Venomous arthropods (a)Hymenoptera (b) Spiders/scorpions (3)Marine animals 8.Burns (1)Thermal burns (a)Classifications/ fluid resuscitation (b)Management (2)Criteria for transfer to burn center (3)Pulmonary inhalation injury (4)Chemical burn (5)Electrical burns/lightning injuries (6)Smoke/noxious gas inhalation (a) CO toxicity (b)Products of combustion (7)Poisonous plants 23 B. Optional 1.Outpatient care of burns 5. Diagnostic Modalities A. Required 1.ABG interpretation(O2,CO2, CO level) 2.Idenfication of Taiwan snakes 3.ECG interpretation of Osborn waves B. Optional 1.Radiation readings interpretation 2.Identification of Taiwan marine dangers and poisonous plants 6. Pharmacological Agents A. Required 1.Catecholamine/Antihistamine/Steroids use 2.Diuretics( carbonic anhydrase inhibitor/ loop diuretics) 3.Silver salfadiazine 4.Cholinergic/Anticholinergic agents 5.Antivenom B. Optional l. Rabies prophylaxis 2. Pharmacokinetics in hypothermia 24 Training Objectives in Head and Neck Disorders 1. Procedural Skills A. Required 1.Neurological assessment 2.CT Scan interpretation 3.X-ray interpretation 4.Spine immobilization (a)Manual (b)Backboard/ C-Collar/ sandbags/ tape B. Optional 1.Lumbar puncture 2.Cervical traction 3.Perimortum Skull Trephination 2. Basic Knowledge A. Required 1.Functional Neuro-anatomy 2.Anatomy of the Spine 3.Brain Stem Reflexes 4.Blood Brain Barrier B. Optional 1.Physiology of Neuromuscular Transmission 2.Cerebral Perfusion Pressure and Autoregulation 3. Symptom-Based Approach A. Required 1.Altered Mental Status (a)Syncope/ coma (b)Dementia/ delirium 2.Dizziness/ Vertigo 3.Weakness/ Easy Fatiguability 4.Headache/ Muscle Pain 5.Nausea/ Vomiting 6.Seizures 7.Battle's Sign 25 8.Periorbital Ecchymosis 9.Rhinorrhea/ Otorrhea 10.Hypotension/ Bradycardia 11.Urinal Retention/ Priapism 12.Sphincter Tone Loss B. Optional 1.Paresthesia/ Hyperesthesia/ Hypalgesia 2.Motor Disorders (a)Ataxia/ tremor (b)Dysphagia/ dysarthria (c)Facial asymmetry/ ptosis (d)Paralysis 3.Speech Disorders (a)Aphasia, dysphasia, dysarthria 4.Reflex Abnormalities 5.Meningismus 6.Post Traumatic Amnesia 4. Disease or Syndrome-Specific Evaluation and Management A. Required 1. Altered Mental Status (a)Syncope/ coma (b)Encephalopathies 2.Cerebrovascular Disorders (a)Aneurysm (b)Arteriovenous malformation (c)Cavernous sinus thrombosis (d)Stroke syndromes 3. Seizure/ Status Epilepticus (a)Etiology (b)Classification (c)Short/ long term management 4.Headache (a)Vascular (b)Other causes 5.Infection 26 (a)Meningitis/ encephalitis (b)Brain abscess (c)Myelitis (d)Osteomyelitis 6.Traumatic Injuries (a)Closed head injury (b)Skull fractures (c)Cerebral edema/ increased ICP (d)Spinal shock/ automatic dysfunction (e)Cord syndrome (f)Vertebral injury 7.Lower Back Pain Syndromes (a)Diskogenic (b)Non-diskogenic B. Optional 1.Cranial Nerve Disorders (a)Bell's palsy (b)Trigeminal neuralgia (c)Other nerve palsies 2.Neuromuscular Disorders (a)Peripheral neuropathies (b)Acute myopathies (c)Myasthenia gravis 3.Demyelinating Disorders (a)Amyotrophic lateral sclerosis (b)Multiple sclerosis 4.Neoplastic Disorders 5.Developmental Abnormalities 6.Cervical/ Lumbosacral Root Injury 7.Metabolic Disorders 5. Diagnostic Tools A.Required 1.X Ray 2.CT Scan B.Optional 27 1.Angiogram 2.MRI 6. Pharmacology A. Required 1.Anticonvulsants 2.Anti-Inflammatories 3.Antimicrobials 4.Anticoagulants 5.Osmolar Agents/ Diuretics 6.Muscle Relaxants 7.Cerebral Salvage Therapeutics B. Optional 1.Anti-Migraine Preparations 2.Anti-Parkinsonism Drugs 3.Drugs acting at Synaptic and Neuro-Affector Sites 4.Hemastatics 28 Training Objectives in Hematology 1. Procedural Skills A. Required None B. Optional 1.Bone marrow aspiration 2.Preparation of peripheral blood smears 2. Basic Knowledge A. Required 1.Cell mediated immunity 2.Coagulation cascade B. Optional 1.Hematopoiesis 3. Symptom-Based Approach A. Required 1.Abnormal bleeding 2.Purpura/ecchymosis/petechiae 3.Lymphadenopathy 4.Hepatomegaly/splenomegaly B.Optional 1. Fatigue/malaise 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1. Differentiation of anemias (1)Hemolytic (2)Hypochromic (3)Megalablastic (4)Normocytic 2.Disorders of hemostasis (1)Clotting factor disorders (2)Platelet disorders (3)Disserninated intravascular coagulation 29 3.White blood cell disorders (1)Leukemoid reaction (2)Leukernia (3)Leukopenias (4)Multiple myeloma 4. Transfusion therapy (1)Component therapy ii)transfusion reactions 5. Lymphoma B. Optional 1.Leukemia management (1)Differentiation (2)Acute management & complications 5. Diagnostic Tools A. Required 1.Physical Examination of patients with anemia, suspected reticuloendothelial system pathology, or suspected acute leukemia 2.Interpretation of red cell indices, Fe, TIBC, reticulocyte counts, platelets, PT & PTT B. Optional 1.Interpretation of peripheral blood smear 6. Pharmacology A. Required 1.Albumin 2.Anticoagulants 3.Hemostatics (1)Antihemophilic factors (2)Tranexamic acid 4.Iron preparations 5.B vitamins B. Optional 1.Antineoplastic agents 2.Hematopoietic agents 30 Training Objectives in Immune System Disorders 1. Procedural Skills A. Required 1.Arthrocentesis B. Optional 1.Plasmapheresis 2. Basic Knowledge A. Required 1.Hummoral Immunity 2.Cellular Immunity B. Optional 1.Complement& chemical mediators 3. Symptom- Based Approach A. Required 1.Facial or throat swelling 2.Urticaria/Rash 3.Fever 4.Joint swelling 5.Discoid skin rash 4. Disease or Syndrome- Specific Evaluation and Management A. Required1.Hypersensitivity reactions (1)Anaphylaxic/anaphyloid reaction (2)Angioedema (3)Serum sickness (4)Urticaria 2.Autoimmune Disorders (1)Acute rheumatic fever (2)Collagen vascular disorder (a)DM/PM/Reiter's (3)Rheumatoid arthritis/AS (4)Sarcoidosis 31 (5)SLE/thyroditis/vasculitis (6)Nephritis 3.Lmmune Deficiency Syndrome 1.HIV B. Optional 1.Immune Deficiency Syndrome (1)Drugs (2)Radiation (3)Malnutrition 2.Transplantation Rejection 5. Diagnostic Tools A. Required 1.Arthrocentesis/Joint fluid interpretation/ Stains B. Optional 1.RIA titer interpretation( Anti-dsDNA, ANA, complement level) 6. Pharmacological Agents A. Required 1.Steroids 2.Antihistamines 3.NSAIDs 4.H2 blockers 5.Epinephrine B. Optional 1. Folic acid antagonist( Methotrexate) 2. Antimalarial agent( Plaquenil) 3. lmmunosupressive agents(Azathioprine/Cyclophosphamide) 32 Training Objectives in System Infectious Disorders 1. Procedural Skills A. Required 1.Gram's stain 2.Acid-Fast stain 3.Blood precautions& aseptic technique 4.Lumbar puncture 5.Thoracocentesis 6.Paracentesis B. Optional 1.Isolation (1)Indication & technique (a)Direct/reverse (2)Blood precautions 2.Chest tube insertion for empyema 2. Basic Knowledge A. Required 1.Bacteriology 2.Parasitology 3.Virology 4.Treatment mechanism of antibiotics 5.Immunizations B. Optional 1.CDC reportable diseases 3. Symptoms-Based Approach A. Required 1.Fever/Chills 2.Exanthems/vrticaria 3.Meningismus/Seizures 4.Septic/Toxic shock B. Optional None 33 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1. Bacterial Diseases (1)Chlamydia (a)Nongonococcal urethritis (b)Psittacosis, trachoma (2)Clostridia (a)Gas gangrene, tetanus (b)Food poisoning (3)Cornybacteria (a)Dipheria (4)Enteric bacilli (a)Gram-negative sepsis (b)Cholera, typhoid, desentery (c)Traveler's diarrhea (d)Cystitis, pyelonephritis (e)Liver/biliary tract infection (5)Hemophilias/Bordetella/Pasturella (a)Epiglottitis, meningitis (b)Ottitis, pertussis, plague (c)Infected animal bites (6)Legionella (7)Mycobacterial infection (a)Tuberculosis, leprosy (b)Atypical mycobacteria infection (8)Mycoplasma (a)Pneumonia (9)Neisseria (a)Meningococcemia (b)Gonorrheal diseases (10)Staphylococcus (a)Abscess formation (b)Sepsis, toxic shock (11)Streptococcus (a)Cellulitis, lymphangitis 34 (b)Acute rheumatic fever (c)Impetigo, pneumonia (d)Otitis, meningitis, sinusitis (12)Rickettsia (a)Typhus (13)Spirochetes (a)Syphilis 2.Fungal diseases (1)Aspergillosis (2)Candidiasis (3)Dermatophytosis (4)Histoplasmosis 3.Viral diseases (1)Adenovirus (a)Conjunctivae, diarrhea (b)Broncholitis, pneumonia (2)HAV/HBV/HCV/HDV/HEV (a)Hepatitis A, B, C, D, E (3)Herpetovirus (a)Herpes simplex/ zoster/ genitalia (b)Infectious mononucleosis (c)Varicella, CMV (4)HIV retrovirus (a)AIDS/ ARC (5)Myxovirus (a)Influenza/ parainfluenza (b)Mumps, rubeola, RSV (6)Rotavirus/ norwalk virus (7)Enterovirus/ adenovirus (a)Acute diarrheal diseases 4. Parasite (1)Malaria B. Optional 1. Rickettsia (1) Q fever, rickettsia, rickettsia pox 2.Spirochetes 35 (1)Yaws, Lyme disease 3.Fungal disease (1)Blastomycosis (2)Cryptococcosis (3)Sporotrichosis 4.Viral disease (1)Picornavirus (Coxsackie, rhino/echovirus) (a)Polio, cardiomyopathies (b)Ppericarditis, pleuritis (2)Poxvirus (a)Variola, vaccinia (b)Molluscum contagiosum (3)Rhabovirus (a)Rabies 5. Diagnostic Tools A. Required 1.Stain interpretation (a)Wright/ Gram/ KOH Giemsa 2.Indications for various cultures 3.X-ray / Sono/ CT indications& interpretation 4.Serologic test interpretation 5.Lumbar puncture interpretation 6.Thoracocentesis interpretation 7.Paracentesis interpretation 8.Streptococcal Ag/Cryptococcal detectation test interpretation B. Optional 1.MRI interpretation 2.Indian ink test 3.PCR for specific organism ( ex. TB) 6. Pharmacological Agents A. Required 1.Penicillin (1)Short/intermediate/long-acting (2)Penicillinase-resistant 36 (3)Broad-spectum 2.Cephalosporins (1)First generation (2)Second generation (3)Third generation 3.Aminoglycosides 4.New β-lactam antibiotics (1)Aztreonam/ imipenem 5.Clindamycin 6.Chloramphenicol 7.Sulfonamides/ Trimethoprim-Sulfamethoxazole 8.Erythromycin 9.Tetracycline 10.Vancomycin 11.Metronidazole 12.Quinolones 13.Anti-TB agents B. Optional 1.Antiviral agents 2.Antifungal agents 3.Malaria Chemoprophylaxis agents 4.Antiparasitic agents 37 Training Objectives in Musculoskeletal Disorders 1. Procedural Skills A. Required 1.Joint and spine examinations 2.Ability to evaluate muscle power 3.Arthrocentesis 4.Local injection for myofascial pain B. Optional 1.Use of gonismeter 2. Basic Knowledge A. Required 1.Musculoskeletal anatomy 2.Important neurovascular structures B. Optional 1.Auto-immune joint involvement 3. Symptom-Based Approach A. Required 1.Pain/ Swelling 2.Heat/ Erythema 3.Crepitus 4.Loss of Motion/Function 5.Weakness 6.Masses/Cysts/Lumps B. Optional 1.Gait Abnormality 4. Disease or Syndrome-Specific Evaluation and Management A. Required 1. Joint Disorders (1)Infections (a)Septic/viral (2)Inflammatory (a)Collagen vascular arthritis 38 (b)Gout/pseudogout (3)degenerative (a)Osteoarthritis (b)Avascular necrosis/osteochondritis dessicans 2. Periarticular Disorders (1)Bursitis (2)Tendinitis 3. Body Disorders (1)Infectious (a)Osteomyelitis (2)Neoplastic (3)Benign tumors (4)Disturbances in bone metabolism (a)Osteoporosis (b)Paget's disease 4. Muscular Disorders (1)Myositis/myositis ossificans (2)Myopathy (3)Rhabdomyolysis 5. Spinal Disorders (1)Inflammatory (a)Ankylosing spondylitis/sacroiliitis (2)Disc disorders (3)Mechanical back pain syndromes (4)Tumors B. Optional 1.Congenitsl Disorders (a)Osteogenesis imperfecta 5. Diagnostic Tools A. Required 1.Interpretation of joint fluid analysis 2.Interpretation of non traumatic skeletal x-rays B. Optional None 39 6. Pharmacology A. Required 1.Analgesics/antiinflammatory agents 2.Muscle relaxants B. Optional 1.Antineoplastic drugs 2.Chymopapain 40 Training Objectives in Nervous System Disorders 1. Procedural Skills A. Required 1.Lumbar puncture 2.Funduscopic examination 3.Neurologic examination B. Optional 1.Caloric testing 2. Basic knowledge A. Required 1.Clinical neuroanatomy (1)Peripheral nervous system (2)Spinal cord (3)Brain stem (4)Visceral nervous system (5)Thalamus and hypothalamus (6)Basal ganglion (7)Cortex (8)Visual system B. Optional None 3. Symptom-Based Approach A. Required 1.Altered mental status 2.Weakness/Paralysis 3.Focal neurological deficit (1)Stroke syndrome 4.Headache 5.Vertigo/Dizziness 6.Seizure disorder B. Optional 4. Disease or Syndrome- Specific Evaluation and Management 41 A. Required 1.Cerebral vascular disorders (1)Ischemic stroke (2)Hemorrhagic stroke (a)ICH (b)SAH (c)Aneurysm (d)AVM (3)TIA (4)VBI 2.Cranial vascular disease (1)Migraine (2)Temporal arteritis 3.Cranial nerve disorders (1)Bell's palsy (2)Trigeminal neuralgia 4.Neuromuscular disorder (1)Guillain-Barre syndrome (2)Myasthenia gravis (3)Periodic paralysis (a)Hypokalemic/hyperkalemc/normokalemic (with/without association of thyroid disease) 5.Spinal cord compression (1)Myelopathy (2)Radiculopathy (3)Seizure disorder 6.CNS infection (1)Meningitis (2)Encephalitis (3)Brain abscess 7.Brain tumor/Space-occupying lesion 8.Normal pressure hydrocephalus B. Optional 1.Amyotrophic lateral sclerosis 2.Multiple sclerosis 3.Myelitis 42 4.Neuritis 5.Dementia 5. Diagnostic Tool A. Required 1.Interpretation of lumbar puncture 2.Reading of brain CT B Optional 1.Reading of spinal CT 2.Reading of myelogram 3.Reading of MRI films 6. Phamacological Agents A. Required 1.Osmotic diuretic agent (to decrease brain swelling) 2.Antiepileptic agents 3.Analgesics 4.Beta-blockers 5.Neurotransmitters (1)Acetylcholine (2)Dopamine 6.Acetylcholinesterase inhibitors (1)Neostigmine (2)Edrophonium bromide (3)Pyridostigmine B. Optional 1. Thrombolytic agents 43 Training Objectives in Obstetrics & Disorders of Pregnancy 1. Procedural Skills A. Required 1.Pelvic examination 2.Normal delivery 3.Bimanual uterine compression 4.Extemal fetal monitoring 5.Neonatal resuscitation 6.Screening pelvic sonogram B. Optional 1.Abnormal delivery 2.Episiotomy repair 3.Vaginal packing 4.Culdocentesis 5.Transvaginal ultrasonography 6.Pudental &/or Caudal block 2. Basic Knowledge A. Required 1.Uterine size in relation to gestational age 2.Maternal physiology changes of pregnancy B. Optional 1.Fetal development 3. Symptom - Based Approach A. Required B. Suspected Pregnancy plus: 1.Abdominal pain 2.Vaginal bleeding 3.Shock 4.Seizures 5.Hypertension C. Optional D. Suspected Pregnancy plus: 44 1.Anxiety/Depression 4. Disease or Syndrome - Specific Evaluation and Management A. Required 1. Complications (Primarily 1st trimester) (1)Abortion (a)Threatened/missed (b)Inevitable (c)Incomplete/septic (d)Complete (2)Ectopic (3)Hyperemesis gravidorum 2.Complications (primarily 3rd trimester) (1)Placental bleeding (a)Abruptio (b)Placenta previa (2)Eclampsia/pre-eclampsia (3)Complicated labor (a)Premature rupture of membranes (b)Abnormal presentation (c)Fetal distress (4)Neonatal resuscitation 3.Complications (post partum) (1)Hemorrhage (2)Retained placenta (3)Endometritis (4)Mastitis 4.Associated problems (diagnosis or management difficulties) (1)Trauma in pregnancy (2)Abdominal pain (3)Appendicitis (a)Jaundice (b)Ureteric colic (4)Post/peripartum conscious change (5)Hypertension 45 B. Optional 1.Standard antenatal care 2.Abnormal pregnancy development (1)High risk patients (2)Poly/oligo - hydramnious (3)Congenital fetal abnormalities 3.Indication for tocolysis and pre-delivery medications 4.Problems associated with breast feeding 5. Diagnostic Tools A. Required 1.Nitrazine testing/Interpretation 2.Interpretation of ferning tests 3.Interpretation of pelvic echo 4.Ability to assess cervical dilatation, effacement, and presentation 5.Interpretation of urine & serum beta HCG testing B.Optional 1.Interpretation of transvaginal ultrasound 2.Interpretation of non stress testing 6. Pharmacology A. Required 1.Drug safety in pregnancy 2.Anti-Rh immune globulin 3.Oxytocics (1)Oxytocin (2)Ergonovine/methylergonovine (3)Prostoglandins 4.Anti-hypertensive/Anti-eclamptic meds (1)Magnesium sulphate/calcium gluconate (2)Hydralazine/labetalol (3)Benzodiazepine/dilantin 5.Antimicrobials (contraindicated) (1)Erythromycin estolate (2)Metronidazole (3)Tetracycline 46 (4)Sulpha drugs (5)Quinolones 6.Analgesics (no specific contraindications) 7.Antiemetics (many are safe) (1)Antihistamines(diphenhydramine, meclizine, trimethobenzamide) (2)Phenothiazines B. Optional 1.Tocolytics (i.e. ritodrine HCL) 2.Antiviral agents 47 Training Objectives in Pediatric Disorders 1. Procedural Skills A. Required 1.Neonatal Resuscitation 2.Pediatric Cardiopulmonary Resuscitation 3.Vascular catheterization (esp. for CVP insertion, umbilical vein and intraosseous route) 4.Pediatric intubation 5.Reduction of a paraphimosis 6.Release of a phimosis 7.Foreign body removal (1)Nose (2)Ear (3)Oropharynx B. Optional 1.Pediatric ultrasonography 2. Basic Knowledge A. Required 1.Apgar Score 2.Normal milestones of childhood development 3.Rules for drug dosing B. Optional 1.Premature pediatrics 2.Congenital abnormalities & Fetal development 3. Symptom - Based Approach A. Required 1. Neonate (1)Crying / irritability / lethargy (2)Feeding difficulties (3)Vomiting / diarrhea (4)Abdon-tinal distension (5)Constipation (6)Rapid breathing 48 (7)Noisy breathy and stridor (8)Apnea / periodic breathing (9)Blue spells / cyanosis (10)Jaundice (11)Fever and sepsis (12)Shock/hypoperfusion 2.Child (1)Conscious disturbance (2)Syncope (3)Cyanosis (4)Palpitations (5)Red eye (6)Fever (7)Pyuria (8)Dyspnea (9)Wheezing (10)Convulsions (11)Vomiting (12)Abdominal pain (13)Diarrhea (14)Gastrointestinal bleeding (15)Jaundice (16)Masses 4. Disease or Syndrome- Specific Evaluation and Management A. Required 1.Sudden infant death syndrome 2.Heart disease (1)Tetralogy of Fallot (2)Congestive heart failure (3)Sinus tachycardia (4)Supraventricular tachycardia 3.Otitis media and pharyngitis 4.Bacteremia 5.Sepsis 49 6.Meningitis 7.Pneumonia 8.Asthma and Bronchiolitis 9.Reye's syndrome 10.Seizures and status epilepticus 11.Gastroenteritis 12.Malrotation with and without volvulus 13.Incarcerated hernia 14.Intestinal obstruction 15.Pyloric stenosis 16.lntussusception 17.Appendicitis 18.Meckel's diverticulum 19.Intraabdominal masses 20.Foreign body in the GI tract 21.Child abuse ( child neglect, sexual abuse,physical abuse) 22.Diabetic child ( including DKA hypoglycemia) 23.Rashes 24.UTI and vulvovaginitis 25.Cellulitis 26.Conjunctivitis B. Optional 1 Leukemia 2.Aplastic anemia 3.Sinusitis 5. Diagnostic Modalities A. Required 1.EKG rhythm & rate interpretation 2.X-ray interpretation (1)Chest, plain abdomen, KUB 3.Pediatric abdominal ultrasonography B. Optional 1.12 lead EKG interpretation 2.Pediatric cardiac ultrasonography 50 6. Pharmacologic Agents A. Required 1.Drugs in the pediatric advanced life support 2.Analgesics/Antipyretics 3.Antispasmotics/Antidiarrheas 4.Sedatives/Anticonvulsants 5.Topical/Systemic antimicrobials 6.Decongestants/Antitussives/Bronchodilators B. Optional 1.Chemotherapeutic agents 51 Training Objectives in Psychobehavior Emergencies 1. Procedural Skills A. Required 1.Interview technique 2.Mental status examination (1)Appearance, behavior, manner of speech (2)Thought processes (3)Cognitive functioning (4)Insight and judgment B. Optional 1.Crisis intervention 2.Suicide risk evaluation 3.Use of restraints 4.Psychiatric commitment 2. Basic Knowledge A. Required 1.Biologic basis for psychiatric illness B. Optional 1.DSM III diagnostic system 3. Symptom-Based Approach A. Required 1.Restlessness/Anxiety/Fearfulness 2.Inappropriate dress/Behavior 3.Destructive/Violent behavior 4.Depression/Withdrawal 5.Substance abuse/Dependence B. Optional 1.Emotional liability 2.Poor personal hygiene 3.Sexual deviation/dysfunction 4.Catatonic syndrome 4. Disease or Syndrome-Specific Evaluation and Management 52 A. Required 1.Affective disorders (1)Major depression (2)Bipolar depression (3)Dysthymic depression 2.Anxiety disorders (1)Anxiety states (2)Post-traumatic stress disorder (3)Panic disorder/hyperventilation (4)Phobic disorder 3.Dissociative disorder (1)Psychogenic amnesia (2)Psychogenic fugue 4.Organic mental disorder (1)Delirium (2)Dementia (a)Alzheimer's (b)Wernicke-Korsakoff 5.Thought disorder (1)Schezophrenia (2)Paranoid delusions 6.Substance use disorder (1)Acute intoxication (a)Alcoholic (b)Narcotics (c)Amphetamine/cocaine (2)Dependence (3)Withdrawl syndromes 7.Suicidal behavior (1)Risk/recognition (2)Prevention B. Optional 1.Disorder manifesting in infancy, childhood or adolescence (1)Anxiety disorder (2)Attention deficit disorder (3)Conduct disorder 53 (4)Development disorder (5)Eating disorder (6)Stereotyped movement disorder 2.Personality disorders (1)Antisocial (2)Borderline (3)Compulsive (4)Copendent (5)Histrionic (6)Passive-aggressive 3.Psychosexual disorders (1)Gender identify disorder (2)Paraphilia (3)Psychosexual dysfunction 4.Somatoform disorder (1)Conversion disorder (2)Hypochondriasis (3)Pychogenic pain disorder 5.Eating disorder (1)Bulimia (2)Anorexia nervosa 5. Diagnostic Tools A. Required 1.Psychiatric and mental status history taking and interpretation B. Optional 1.Psychiatric written testing 6. Pharmacology A. Required 1.Antipsychotics (1)Haloperidol / droperido (2)Stelazine / chlorpromazine (3)Extrapyramidal symptoms (4)Neuroleptic malignant syndrome 2.Drugs used to treat extrapyramidal reactions 54 (1)Diphenhydramine hydrochloride (2)Benztropine mesylate 3.Antidepressants (1)Heterocyclics (2)Monarnine oxidase inhibitors (3)Selective serotonin reuptake inhibitors 4.Sedatives (1)Benzodiazepines (2)Barbiturates 5.Lithium 6.Antagonists (1)Narcotic (a)Naloxone (2)Benzodiazepine (a)Flumazenil B. Optional 1.Hallucinogens 2.Psychostimulants 3.Methadone 55 Training Objectives in Renal Disorders 1. Procedural Skills A. Required 1.Renal ultrasonography 2.Insertion of Hemodialysis Catheter : femoral, subclavian or internal jugular B. Optional 1.Insertion of peritoneal dialysis tube 2.Percutaneous nephrostomy 2. Basic Knowledge A. Required 1.Anatomy of the Kidney 2.Fluid volume, Electrolyte and Acid-Base Balance 3.Anion gap 4.Fractional excretion of Sodium(%)=FENa(%) 5.Renal failure index 6.Hemodialysis, Hemoperfusion and Peritoneal Dialysis B. Optional None 3. Symptom-Based Approach A. Required 1.Flank pain 2.Hematuria 3.Dysuria 4.Oliguria and Anuria 5.Pyuria 6.Generalized anasaca B. Optional None 4. Disease or Syndrome-Specific Evaluation and Management A. Required 56 1.Renal failure (1)Acute (2)Chronic 2.Infection (1)Renal (a)Acute pyelonephritis (b)Perirenal abscess (2)Lower urinary tract (a)Cystitis (b)Urethritis 3.Glomerulonephritis 4.Renal Calculi 5.Fluid, Electrolyte and Acid-Base Imbalance 6.Complications of Dialysis (1)Indications (2)Complications B. Optional 1.Congenital abnormalities 2.Nephrotic Syndrome 3.Tumors 4.Porphyria 5. Diagnostic Modalities A. Required 1.KUB interpretation 2.Renal ultrasonography interpretation (1)Kidney size (2)Echogenicity of kidney (3)Calculi (4)Hydronephrosis 3.Interpretation of urinalysis 4.Blood gas interpretation 5.Serum electrolyte interpretation B. Optional None 57 6. Pharmacological Agents A. Required 1.Diuretic agents (1)Loop/thiazide/potassium sparing 2.Nephrotoxic agents (1)Aminoglycosides/amphotericin B (2)Contraindications in renal insufficiency B. Optional None 58 Training Objectives Thoracic-Respiratory Disorders 1. Procedural Skills A. Required 1.Helmlich maneuver 2.Placement of artificial airway (oral airway, nasal airway) 3.Bag-valve-mask ventilation 4.Endotracheal intubation (1)Oral (2)Nasal (3)Rapid sequence intubation 5.Cricothyrotomy 6.Thoracentesis 7.Needle thoracostomy (Immediate release of tension pneumothorax) 8.Chest tube insertion 9.Mechanical ventilation B. Optional 1.Tracheothyrotomy 2.Tracheostomy 3.Placement of chest tube 4.Percutaneous transtracheal ventilation 2. Basic Knowledge A. Required 1.Anatomy of upper airway&chest 2.Pulmonary function physiology 3.Pulmonary vascular circulation 4.Oxygen and cellular metabolism (1)Physiology of oxygenation and delivery of oxygen to tissue (2)Pathophysiology of hypoxia and hypoxemia 5.Pathophysiology of bronchial asthma and other obstructive lung disease B. Optional None 59 3. Symptom-Based Approach A. Required 1.SOB/Respiratory distress 2.Hemoptysis 3.Stridor 4.Wheezing 5.Cough 6.Hoarseness 7.Subcutaneous emphysema B. Optional None 6. Disease or Syndrome—Specific Evaluation and Management A. Required 1. Acute upper airway obstruction (1)Foreign body (2)Inflammation (3)Caustic injury 2.Disease of pleural, mediastinum, and chest wall (1)Pulmonary fibrosis (2)Pleural effusion/empyema (3)Pneumothorax (a)Spontaneous (b)Iatrogenisc (c)Tension 3.Pneumomediastinum/Subcutaneous emphysema 4.Hyperventilation syndrome 5.ARDS 6.Obstructive lung diseases (1)Asthma/COPD (2)Destructive lung (TB/bronchiectasis) 7.Pneumoconiosis 8.Inhalation/Aspiration injury (1)Smoke/thermal (2)Toxins (metals/plastics) (3)Aspiration pneumonia 60 9.Pulmonary embolism (1)Venous (2)Fat/amniotic (3)Septic 10.Lung tumors (1)Presentations (2)Complications 11.Pulmonary infection (1)Bacterial (2)Tuberculosis (3)Mycoplasma (4)Lung abscess (5)Pneumocystis carini (6)Septic emboli (7)Viral pneumonia (bronchopneumonia) (8)Fungal pneumonia 12.Allergic Pneumonitis (farmer's lung...) 13.Cheniical pneumonitis 14.Hemoptysis (1)Evaluation&care (2)Massive 15.Non cardiac pulmonary edema B. Optional 1.Costochondritis 2.Mediastinal mass 3.Sleep apnea syndrome 4.Thoracic outlet syndrome 5.Primary pulmonary hypertension 5. Diagnostic Tools A. Required 1.Interpretation of CXR 2.Arterial blood gas interpretation 3.Interpretation of pleural fluid examination 4.Interpretation of pulmonary function tests 5.Pulse oximetry interpretation 61 6.Examination of sputum (Gram stain) B. Optional 1.End-tidal CO2 monitoring 6. Pharmacological Agents A. Required 1.Antibiotics 2.Bronchodilators (1)Beta2-agonists (2)Anticholinergics (3)Theophylline 3.Oxygen 4.Inhalation therapy 5.Mechanical ventilation 6.Sedatives 7.Paralyzing agents B. Optional 1.Antitussives 2.Demulcents/expectorants 62 iTraining Objectives in Toxicology and Clinical Pharmacology 1. Procedural Skills A. Required 1. Gastric lavage B. Optional None 2. Basic Knowledge A. Required 1.Phamocokinetics (1)Administration (2)Absorption (3)Metabolism (4)Excretion (5)Reabsorption (6)Drug level (7)Protein bindage of drugs (8)Autonomic pharmacology (a)Muscarinic receptor (b)Nicotinic receptor B. Optional 1.Drug kinetics 3. Symptom-Based Approach/Toxidrome A. Required 1.Cholinergic syndrome 2.Anticholinergic syndrome 3.Altered mental status 4.Hyperthermia 5.Metabolic acidosis 6.Possible drug-induced 7.Extrapyramidal syndrome 8.Cyanosis/Hemoglobinopathy B. Optional 63 4. Disease or Syndrome-Specific Evaluation and Management A. Required 1.General approach to intoxicated/ Poisoned patient 2.Sources of toxicological information in Taiwan 3.Cholinergic agents (1)Organophsphates (2)Carbamates 4.Anticholinergic agents (1)Anticholinergics (2)Antihistamines (3)Antiparkinsonic agents 5.CNS stimulants (1)Amphetamine 6.CNS depressants (1)Opioids (2)Barbiturate (3)Benzodiazepines 7.Anticoagulants (1)Short acting (2)Long acting (rodenticide) 8.Extrapyramidal syndrome (1)Neuroleptic agents (2)Metoclopramide 9.Tissue hypoxia (1)Cyanide (2)Hydrogen sulfide (3)CO 10.Agriculturally used poisons (1)Paraquat (2)Glyphosate (3)Pyrethrine (4)Other rodenticide 11.Cardiovascular agents (1)Beta-blockers (2)Cardiac glycocides 64 (3)Calcium channel blockers 12.Bronchodilators (1)Theophylline 13.Psychiatric agents (1)Antipsychotics (2)Tricyclic antidepressants 14.Corrosive agents (1)Detergents (2)Strong acid/base 15. Salicylates 16.Acetaminophen 17.Alcohols (1)Ethanol (2)Methanol B. Optional 1.Methemoglobinemia (1)Nitrates 2.Lithium 3.Heavy Metals and chelation 4.Cocaine 5.Antiarrhythmics 6.Poisoning by natural agents (1)Mushrooms (2)Chinese herb drugs 5. Diagnostic Tools A. Required 1.Knowledge of need for &interpretation of specific quantitative drug levels B. Optional None 6. Pharmacological Agents A. Required 1.Antidotes for specific toxins 65 2.Renal replacement therapy for poison (1)Hemodialysis (2)Hemoperfusion (3)Plasmapheresis (4)Plasma exchange B.Optional 66 Training Objectives in Traumatic Disorders 1. Procedural Skills A. Required 1. Physical Exam/ Initial Assessment (1)Primary survey/ secondary survey 2.Needle/ Surgical Cricothyrotomy 3.Needle/ Tube Thoracotomy 4.Venous Access (1)Peripheral/ central Lines (2)Cutdowns/ intraosseous routes 5.Diagnostic Peritoneal Lavage 6.Foley Catheter Insertion 7.Immobilization Techniques (1)C-spine/T, L-spine (2)Traction splints 8.Dislocation reduction 9.Splinting/Casting 10.Wound debridement/Suturing 11.Conscious sedation 12.Retrograde urethrogram 13.Retrograde cystogram 14.Screening abdominal echo B. Optional 1.Pericardiocentesis with EKG Monitoring 2.Emergency Thoracotomy (1)Pericardial incision (2)Aortic cross clamp (3)Cardiorrhaphy 3.MAST Suit Application 4.Fracture reduction 5.Application of skull tongs 6.Burr holes 7.Screening cardiac echo 8.Compartment pressure measuring 67 2. Basic Knowledge A. Required 1.Pathophysiology of Shock 2.Mechanism of Injury (1)Vehicular accidents (2)Blast/ crush/ fall/ impalement (3)Weapons (4)Blunt/ penetrating 3.Principles of wound healing 4.Trauma and the immune system 5.Musculoskeletal anatomy B. Optional 1.Physiology of pain 2.Cerebral perfusion pressure and autoregulation 3. Symptom-Based Approach A. Required 1.Dyspnea/ Stridor/ Apnea 2.Altered Hemodynamics, Shock 3.Altered Mental Status 4.Pain/ Crepitation/ Deformity 5.Abnormalities of ROM 6.Paresthesias/ Paralysis B. Optional None 4. Disease or Syndrome-Specific Evaluation and Management A. Required 1.Head trauma (1)Close verse open injuries (a)Mass lesions (b)Cerebral edema (c)Increased ICP (d)Skull fractures 2.Special trauma (1)Vertebral injuries 68 (a)Fractures (b)Dislocations (2)Cord injuries (a)Complete transection (b)Incomplete lesions (c)Spinal shock 3.Facial trauma (1)Maxillary fractures (2)Mandibular fractures (3)Neurovascular injuries (4)Dental injuries (5)Anterior neck trauma 4.Chest trauma (1)Blunt verse penetrating (2)Thorasic injuries (a)Hemo/pneumothorax (b)Rib fractures/ flail chest (c)Tracheobronchial tear (d)Esophageal injury (e)Diaphragmatic injury (f)Pulmonary contusion/ laceration (3)Delayed ARDS/ fat emboli (4)Cardiovascular injuries (a)Cardiac contusion/ disruption (b)Pericardial tamponade (c)Great vessel injury 5.Abdominal trauma (1)Blunt verse penetrating (2)Solid organ injury (3)Hallow organ injury (4)Retorperitoneal injury (a)Kidney (b)Pancrease (c)Aorta 6.Genitourinary trauma (1)Bladder/ uretral injuries 69 (2)Scrotum/ testicle injuries (3)Uterine injuries 7.Musculaoskeletal trauma (1)Open versus closed injuries (2)Fractures/ dislocations (a)Upper limb (b)Lower limb (3)Life/ limb threatening injuries (a)Pelvic fractures (b)Amputation (c)Compartment syndromes 8.Soft tissue trauma (1)Wound care issues (a)Emergency department repair (b)Bite wounds (c)Foreign bodies (2)Special wound care requirements (a)Eyelid/ lip/ ear (b)Nail bed/ traumatic amputations (3)Wound infections (a)Tetanus/ rabies prophylaxis (b)Antimicrobial indications (4)Peripheral neurovascular injuries 9.Pediatric trauma (1)Anatomic and injury differences (2)Stress response differences 10.Trauma in pregnancy (1)Anatomic and physiologic differences (2)Fetal evaluation and care considerations B. Optional None 5. Diagnostic Tools A. Required 1.Interpretation of trauma x-rays (1)C-spine, chest, pelvis, extremeties 70 (2)Brain, neck, chest, and abdominal CTs (3)Urethrogram, cystogram, esophagogram 2.Interpretation of screening ultrasound 3.Interpretation of DPL results 4.Interpretation of compartment pressures B. Optional 1.Interpretation of NMs 2.Interpretation of cardiac echo 3.Interpretation of angiograms 6. Pharmacology A. Required 1.IV fluids (1)Crystalloids (2)Colloids 2.Local anaesthetics (1)Amides (a)Lidocaine/bupivicaine (2)Esters (a)Procaine/cocaine 3.Toxoids/Immune globulins/Antivenoms (1)Tetanus (2)Hepatitis (3)Rabies (4)Snakebites 4.Osmolar agents/Diuretics (1)Mannitol/glycerol (2)Ethacrynic acid 5.X-ray contrast media (1)Water soluble (2)Oil based (3)Low molecular weight B. Optional 1.Cerebral salvage agents (1)O2 free radical scavengers 2.Gram-ve antitoxins 71 3.Shock cascade blockers 72 Training Objectives in Urogenital Gynecologic Disorders 1. Procedural Skills A. Required 1.Pelvic examination 2.Urinary bladder sonogram 3.Screening pelvic sonogram B Optional 1.Male&Female rape exam 2.Child sexual abuse exam 3.Suprapubic cystostomy 4.Culdocentesis 5.Transvaginal ultrasonography 6.Prostatic sonography 2. Basick Knowledge A. Required 1. Anatomy of male and female genital organs 2. Sexual assault 3.Menstrual cycle& ovulation dysfunction B. Optional None 3. Symptom-Based Approach A. Required 1.Lower abdominal pain 2.Hematuria 3.Dysuria 4.Urinary retention 5.Testicular pain 6.Scrotum swelling 7.Vaginal bleeding B. Optional None 73 4. Disease or Syndrome-Specific Evaluation and Management A. Required 1 .Diseases of male genital organ (1)Benign prostatic hyperplasia (2)Fournier's gangrene (3)Paraphimosis (4)Fracture of the penis (5)Testicular torsion (6)Epididymitis (7)Urethral foreign bodies (8)Cystitis (9)Prostatitis 2. Disease of female genital organ (1)Abnormal premenopausal bleeding (non pregnancy) (2)Abnormal postmenopausal vaginal bleeding (3)Dysmenorrhea (4)Menopause syndrome (5)Pelvic inflammatory disease (6)Torsion of ovarian cyst (7)Pelvic abscess (8)Vaginal foreign bodies (9)Vaginitis (10)Uterine prolapse 3. Sexual assault/Abuse (1)Female (2)Male (3)Child B. Optional Priapism 5. Diagnosis Tools A. Required 1.Interpretation of Gram - stained smear of fluid (in Cul-del sac) 2.Interpretation of wet mount of vaginal swab 3.Interpretation of pelvic echo 4.lnterpretation of urine pregnancy test 74 B.Optional 1.Interpretation of transvaginal ultrasound 6. Pharmacologic Agents A. Required 1.Antimicrobials in epididymitis, cystits and prostatitis 2.Antimicrobials in acute pelvic inflammatory disease 3.Vaginal preparations (1)Antimonilials/trichomonacides 4.Premenstrual therapeutics B. Optional 1.Contraceptives (1)Pre/post coital 75 Training Objectives in Administrative Aspects Emergency Medicine A. Required 1.Accreditation (1)Hospital (2)Departmental (3)Residency training program 2.E.D. policies and procedures (1)Setting standards and rules 3.Quality assurance (1)Based on departmental, association or recognized international standards 4.Educational planning (1)Certification requirements for: (a)Doctors (b)Nurses (c)EMTs (2)Departmental teaching (3)CME requirements 5.Medical charting and discharge planning 6.Computer applications (1)Charting (2)Tracking (3)Data collection (4)Auditing (5)Learning (6)Research (7)Personal planner 7.Medico-legal aspects (1)Consent (implied, written, living wills) (2)Protection (law, insurance, risk management) (3)Liability (negligence, malpractice, poor outcome) (4)Legal system 8.Personnel needs 76 (1)Organizational structure (2)Manpower requirements (3)Skills needed (4)Complaints review process (5)Communication skills 9.Trends in emergency care delivery 1.Specialization (1)Trauma centers (2)Specialized critical care centers (i.e. chest pain) (3)Urgent care centers 2.Triage (1)Treatment in the field not hospital (2)Phone or curbside diversion away from ED 3.Expanded primary care role (1)Routine vaccinations (2)Coordination with community care programs B. Optional 1.Practise group dynamics (1)Contracts (2)Structure (3)Benefits 2.Billing management (1)Budgeting (2)Billing/reimbursement (3)Cost containment 3.Equipment/supplies/facility design needs 4.Hospital administration (1)Organizational structure (2)Committee work (3)Disciplinary policy 77 Training Objectives in EMS Systems and Disaster Medicine 1. Procedural Skills A. Required 1.Airway management and ventilation skills 2.Manually triggered resuscitator 3. Setting up an oxygen system 4.Applying tourniquet 5.Applying the MAST 6.Operating AED 7.Log roll technique 8.Remove a helmet 9.Spine management skill 10.Applying a dressing and bandage to extremities, head, joint, and an impaled object 11.Applying a sling to upper extremities 12.Applying a rigid splint to the extremities 13.Applying an air splint to the extremities 14.Applying traction splint 15.Normal childbirth 16.Resuscitation of the newborn 17.Loading a wheeled cot stretcher 18.Placing a patient in supine position on a long spine board using the log roll 19.Perform scoop stretcher 20.Rapid extrication 21.Applying the short spine board 22.Radio communication 23.Decontaminating victims of HAZMAT incident B. Optional 1.Underwater rescue 2.Loading the ambulance 3.Unloading the ambulance 4.Applying the extrication device 5.Performing rapid takedown procedure 78 6.Cardispulmonary resuscitation during transport 7.Confined space medical care (1)Assessment of partially exposed patient (2)Finger-guided intubation 8.Wilderness survival (1)Water &food sanitation (2)Starting a fire (3)Setting up a tent/shelter 2. Basic Knowledge A. Required 1.EMS overview (1)1995 EMS Act, Taiwan (2)EMT Training curriculum development (3)Ambulance standards development 2.EMS system design (1)Key component of EMS system (2)EMS administrative/operational/political design 3.EMS personnel (1)National requirement (including number of hours) for initial training and (2)Continuing education for EMT-I,EMT-II, and EMT-P (3)Understand the patient care capabilities and responsibilities for EMT-I EMT-II, and EMT-P (4)Stress management and infection disease among EMT 4.Medical control (1)Medical control authority structure (including qualification and responsibility) (2)Quality assurance and quality improvement in prehospital care 5.Communication (1)119 system (a)Dispatch priority and call screening 6.EMS equipment and vehicles (1)Types EMS vehicles (ALS and BLS Units) (2)Drug use in the prehospital setting (3)Special requirements for pediatric equipment 79 7.EMS Agencies (1)structure and interrelationship if local, national, medical and political EMS agencies 8.EMS receiving facilities (1)Categorization of trauma center, intensive care unit, pediatric, poison, spinal cord, neonatal/perinatal, burn, psychiatric 9.Legal considerations (1)Concept of vicarious liability and how it applies to EMS activities (2)Risk management to minimize malpractice exposure 10.Mass gathering/Disaster (1)Principles of disaster management (2)Incident command structure (3)Interaction between EMS and disaster response (4)Triage in disaster (5)Hazardous materials B. Optional 1.EMS overview (1)1966 NAS-NRC white paper (2)American EMS history 2.EMS personnel (1)Labor relation activities (2)Health safety problems 3.Medical control (1)On scene medical control and off-line medical control (2)Mechanism for handling scene non-EMS physician interaction (physician intervenor) 4.Communication (1)Base hospital and resource hospital (2)Post-dispatch instruction for cardiac arrest and emergency childbirth (3)Cellular telephone and radio communication 5.EMS equipment (1)Method for evaluation and approval of new EMS equipment and techniques 6.Air medical 80 (1)Use of air medical transport (2)Physiologic changes which occur during air medical transport (3)Aircraft safety procedures for ground operation and inflight problems 7.Mass gathering /disaster (1)Local and national resources available for disaster response (2)Pitfalls to successful triage (3)Interaction of all public safety agencies at local and national levels during a disaster response 8.Research (1)Funding sources available for EMS related research 81 Verification Guidelines to Ensure Compliance With Emergency Medicine Residency Training Core Content I. Training Program Components a) Emergency Medicine minimum exposure 15 months If Trauma and Pediatric Emergency cares are separate sections within our Emergency Department it is suggested that at least 4 months of Trauma/ Surgical ED and 1 months of Pediatric ED be included in this training time. ED administration and EMS training are also to be included. ** EMS training requires reports from each resident of at least 5 ambulance runs to pick up ill or injured patients. b) Internal Medicine Primary Specialty Areas include: Cardiology, Chest Medicine, Gastroenterology, Nephrology, and ICU. Secondary Specialty Areas include: Metabolism, Infection, Hematology, and General Medicine. c) Surgery Primary Specialty Areas include: General Surgery, Orthopaedics, Plastic Surgery Secondary Specialty Areas 'include: Neurosurgery, Cardiovascular Surgery, Urology d) Pediatrics Primary Specialty Areas include: General Pediatric experience, Pediatric Intensive Care Secondary Specialty Areas include: Focused Subspecialty experience, Neonatal Intensive Care e) Other Primary Specialty Areas include: Neurology, Toxicology, Anaesthesia, Obstetrics & Gynaecology, Psychiatry, ENT/ Ophthalmology, Radiology, and Sonography. Suggested Optional Areas include: Research and Electives. To ensure emergency residents receive adequate training each program should be able to the following proof for each of the listed "Primary Specialty Areas." 82 1. A training schedule which includes at least a one month experience on the given "Primary Specialty Area" service, along with an evaluation sheet of the ED resident's performance from the Director of the service or his representative. or 2.Evidence of a minimum of 4 hours of formal classroom teaching for any respective "Primary Specialty Area" (by invited Specialists or well-prepared Emergency Physicians); a minimum of 2 hours of bedside or workshop teaching focusing on key history and physical examination skills related to the body system or specialty in question +/- basic related skills; plus a list of 40 patients with each respective "Primary Specialty Area" complaints or condition including chart number, presentation, ED management, disposition, and F/U information at between 1 week -3 months later (files including a copy of the ED Hx, P.E., orders & pertinent data, along with a brief F/U description for each resident, for each "Primary Specialty Area" are acceptable). 3.** "Primary Specialty Areas" requiring slightly different patient documentation include: Anaesthesia - requires a minimumum of 20 intubations and 20 CVP insertions including: chart number, indications for procedure, technique (including adjunct medications), complications, and follow up CXR findings. Radiology - requires a list of 40 interesting x-rays where the Radiologist found something missed by the Emergency Physician or visa versa, or particularly interesting x-rays, including: chart number, diagnostic change, and key teaching point. Sonography - requires a minimum of 40 monographic studies performed by the resident including: chart number, indications for study, and report of findings countersigned by supervising physician. II. Keep a complete record of all training activities including: a)Time & date 83 b)Type of activity c)Name of presenter d)Number, & names of attendees e)A copy of the teaching material Exmples of teaching activities include: 1)Core lectures 2)Special lectures 3)Case presentations 4)Case discussions (Morbidity & Mortality Rounds) 5)Combined or Special Rounds or Case discussions (i.e. Trauma Rounds, Radiology, Toxicology, etc) 6)Textbook Reading 7)Journal Reading 8)Workshop Teaching 9)Teaching by Residents (i.e. Nurses, Interns, EMTS, etc.) ** Records can be kept on paper or computer format III. Residents need to keep a record of cases they have seen and procedures they have performed in such a way that a random sampling of these charts can be requested and reviewed at the time of any program audit to allow for charting evaluation and auditor-resident interaction to better assess clinical comprehension and ability. Suggested minimums include the following: a. Ability to manage 3-4 patients per hour as a final year Emergency resident show chart numbers of patients managed per shift for at least 2 months of your training for random review. b. Evidence of experience in handling critically ill and injured patients. provide a list of tiiage category I chart numbers for at least 40 non trauma patients, 20 trauma patients (ISS ≧ 16), and 10 pediatric patients managed by each resident. If necessary the pediatric patients may be chosen from a PICU rotation but the trauma & non-trauma adult patients should all come from ED training experience. 84 c. These are the suggested minimum procedural requirements during ED training which need careful documentation. ** Suggest keeping a copy of the patient's progress note written by the resident documenting: reason for the procedure, description of the procedure, and effects of the procedure in a file. i)Endotracheal Intubation 20 ii)CVP insertion 20 iii)Defibrillation/ Cardioversion 5 iv)External Cardiac Pacing 2 v)Chest tube insertion 10 vi)Lumbar puncture 5 vii)Wound repair 10 viii)DPL 5 ix)Pediatric intubation 5 x)Screening echo 40 xi)Report of ambulance run 5 IV. Each year of training all residents should receive at least 2 practise examinations, at least one of which should include an oral examination. The test questions and test results should be kept on file. V. All residents are recommended have some research experience and write at least one publishable quality paper (case report acceptable) to be eligible to sit for their board exam. 85 Emergency Medicine Training and Board Eligibility Eligibility to sit Emergency Medicine Boards exams 1. 2. A minimum of 3-years of a recognized Emergency Medicine training course. A 2-year Emergency Medicine training course following the completion of a recognized training program in Internal Medicine, Family Medicine, Surgery, Anaesthesia, Neurology or Pediatrics. Eligibility to work as an Emergency Physician in a Medical Center 1.A 4-year Emergency Medicine training program. be a Fellowship year. 2.Dual board Emergency Physicians. The final year may Eligibility for a second board of Critical Care Medicine 1. A minimum of 5-years training, 3 of which comply with Emergency Medicine board requirements, the remaining 2 years to comply with the requirements of other subspecialty. Application Requirements for Emergency Medicine Board Exam Candidates. 1. Training certificates from the hospital to confirm completion of their training. 2. A representative sample of critical patients' charts and procedural records as requested by the examining committee. The types of charts & procedures requested may vary from year to year. Any of the materials requested and received can be used by the examiner to prepare a number of oral questions. 86 慈濟醫療志業住院醫師 教育訓練目標與考核方式 壹、宗旨: 培育人本醫療,尊重生命的良醫 樹立人苦我悲,視病猶親的典範 貳、目標: 目標及標準 一、具大愛情懷 1.參加志工早會:每年 10 次,若有心得分享再加分 2.人文共識營:住院醫師訓練期間每三年需參加 1 次 3.醫學倫理討論會:每年至少 2 次 二、能終生學習 1.應具醫療資訊應用、網路資訊、圖書館使用、教材製作等能力,並以此習得專 業知識。 2.每年 1 篇學習成果心得報告 3.全院性學術活動:每年至少參加 15 次 4.參與全國或地區醫學會議:每年至少 1 次 三、備專業識能 1.病歷寫作品質考核。 2.病例報告或原著論文:住院醫師訓練期間每三年內至少繳交 1 篇 3.住院醫師升級考試:口試或筆試方式,每年至少 1 次 四、有團隊精神 1.與科內同仁溝通相處能力 2.與其他醫療科溝通合作能力 3.與護理、醫技、行政等單位溝通合作能力 4.醫病關係:與病人及家屬之互動情形 5.不預期跨院支援之配合 五、負社會責任 健康或衛生教育活動:每年至少 2 次 六、願奉獻服務 1.參與國內外義診(不限慈院所舉辦) :每年至少 2 次 87 目標及標準 2.參與社區服務:訪貧、居家關懷、救災、掃街等,每年至少 2 次 88 財團法人佛教慈濟綜合醫院大林分院住院醫師考核表 姓名:______________ 科別:____________ 職級: 基本資料 項目 備 專 業 識 能 考核期間:___年___月___日 ~ ___年___月___日 初核 考核項目 複核 分數(1-5) 分數(1-5) 1.專業知識 2.臨床診斷及處理能力 3.臨床病例討論表現 4.各種檢驗報告判讀能力 5.病歷寫作品質 6.利用輔助工具學習專業知識能力 7.與科內同仁溝通相處能力 總分 團 隊 精 神 1.與其他醫療科溝通合作能力 2.與其他單位溝通合作能力 3.醫病關係 4.不預期跨院支援之配合 總分 其他特殊才能(如電腦、音樂、繪畫、運動…)或令人難忘的事蹟 總醫師評語或建議(請務必填寫): 簽核: 負責訓練之主治醫師評語或建議(請務必填寫): 日期: 簽核: 日期: 科主任評語或建議(請務必填寫): 簽核: 日期: 教學部主任: 89 急診醫學科住院醫師 急救技能學習項目及最低實施次數標準 學習技術項目 最低次數 一般縫合 100 例 Splint (上肢及下肢) 100 例 Cast (上肢及下肢) 40 例 關節脫臼(徒手復拉術) 肩 10 例 肘 5例 下顎 5例 下顎 5例 面部縫合 50 例 胸管插入 20 例 診斷性腹腔灌洗 10 例 環甲軟骨間造口 5例 腰椎穿刺 30 例 關節穿刺 20 例 swan-Ganz 導管置放 20 例 RSI IABP 導管置放及使用 20 例 10 例 超音波檢查 (1)腹部 (2)胸腔 (3)心臟 100 例 50 例 50 例 體外心臟節律器裝置 10 例 完整 APLS 操作 40 例 完整 PALS 操作 40 例 嬰兒(< 1 歲)插管 10 例 完整 ATLS 操作 40 例 心包膜穿刺 10 例 順產接生 10 例 經食道超音波 10 例 呼吸器操作 100 例 90 學習技術項目 最低次數 經麻醉阻斷: (1)腋 (2)肋間 (3)上肢 (4)下肢 10 例 10 例 10 例 10 例 到院前救護 50 例 91 急診醫學科住院醫師技能評核表 姓 名:_____________ 項 目:_一般縫合 __ 編號 日期 受訓科別:______________ 病歷號碼 成功/失敗 指導者簽名 備註 1 2 3 4 5 6 7 8 9 10 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 *不敷使用者,請自行影印。 92 93 教學活動時間表 日期 星期一 星期二 星期三 星期四 星期五 星期六 星期日 日班 主治醫師 教學迴診 日班 主治醫師 教學迴診 時間 8:00~ 9:00 9:00~ 10:00 10:00~12:00 (隨機教學) 日班 主治醫師 教學迴診 晨會/ 晨會及 Case 病歷討論 conference (Mortality /全院學術演 conference) 講 Case conference/急 診行政及品質 會議 日班 日班 主治醫師 主治醫師 教學迴診 教學迴診 晨會及 Book 病歷討論 reading /Journal (Pain Meeting Managemen t) Case conference 日班 主治醫師 教學迴診 Book 三日內迴診 三日內迴診病 Radiology 12:00~14:00 reading 病例討論會 例討論會 Teaching (Pain Managemen t) 日班 主治醫師 教學迴診 Special Lecture 94 ED&MICU Combined Meeting 14:00~17:30 21:00~24:00 (隨機教學) 夜班 主治醫師 教學迴診 夜班 主治醫師 教學迴診 Booking reading (High altitude medicine) 夜班 主治醫師 教學迴診 夜班 主治醫師 教學迴診 Booking reading (Sedation and analgesia procedures) 夜班 夜班 主治醫師 主治醫師 教學迴診 教學迴診 夜班 主治醫師 教學迴診 95 職 第一年住院醫師 第二年住院醫師 第三年住院醫師 級 臨床研究員 臨床研究員 訓練內容 期間 訓練內容 期間 訓練內容 期間 訓練內容 期間 (或排程) (月) (或排程) (月) (或排程) (月) (或排程) (月) (或排程) 項 訓練內容 期間 (月) 目 各 職 級 住 院 醫 師 及 臨 床 研 究 員 每 年 安 排 之 訓 練 課 程 及 期 間 胸腔醫學 0.5 血液醫學 0.5 心臟醫學 0.5 到院前救護 1 次專科選修 1 心臟醫學 0.5 新陳代謝醫學 0.5 加護醫學 0.5 災難醫學 1 次專科選修 1 胃腸醫學 0.5 毒物醫學 1 加護醫學 0.5 死亡醫學 1 論文寫作 1 腎臟醫學 0.5 婦產醫學 1 新生兒科 1 野外醫學 1 論文寫作 1 外傷醫學 1 加護醫學 1 放射診斷 1 航空醫學 1 到院前救護 1 醫學 外科學 1 精神醫學 1 皮膚科 0.5 旅遊醫學 1 到院前救護 1 外科學 1 外傷醫學 1 外科學 1 急診醫學 1 創傷醫學 1 小兒醫學 1 神經內科學 1 超音波醫學 1 急診醫學 1 創傷醫學 1 耳鼻喉科/ 1 急診醫學 1 研究計畫 1 急診醫學 1 急診醫學 1 急診醫學 1 急診醫學 1 感染急症 0.5 急診醫學 1 急診醫學 1 急診醫學 2 急診醫學 1 緊急醫療 1 急診醫學 1 急診醫學 1 急診醫學 1 急診醫學 1 眼科 救護 急診醫學 2 合計 12 急診醫學 2 急診醫學 3 12 12 12 12 註:急診科 共計 13 個月、內科 共計 4 個月、外科 共計 5 個月、小兒科 共計 2 個月 婦產科 共計 1 個月、精神科/神經科 共計 2 個、耳鼻喉科/眼科/皮膚科 共計 1.5 個月 緊急救護/災難醫學 共計 1 個月、影像判讀 共計 2 個月、毐物學 共計 1 個月、自選科別如: 加護醫學 共計 2 個月、研究計劃 共計 1 個月。 96 急診醫學科第一年住院醫師(前三個月)臨床重點訓練課程 一.復甦術 (含 ACLS,APLS,ATLS,EMS) 二.心臟血管生理學,病理學及治療: 1. 休克 (1)低容性 (2)心因性 (3)分佈性—低或高阻抗 (4)阻塞性 2.心肌梗塞及併發症 3.心律不整及傳導障礙—心律調節器 4.肺栓塞 5.肺水腫—心因性及非心因性 6.急性心包膜疾病 7.急性主動脈或週邊動脈血管疾病 8.心肌病變及心肌炎 9.心臟手術後病人早期之處理 10.血管收縮或舒張劑之治療 11.心臟及微血管間血流動力學—計算及判讀 12.呼吸器對血流動力學之影響 13.高血壓危象 14.急性冠狀動脈疾病之內外科治療 三.呼吸生理學、病理學及治療 1.急性呼吸衰竭 (1)缺氧性—成人呼吸窘迫症 (2)二氧化碳過多性 97 (3)神經性、機械性 2.急性氣喘 3.煙霧吸入、氣道燒傷 4.吸入或化學性肺炎、溺水 5.連枷胸、壓力傷害 6.下呼吸道感染 7.上呼吸道阻塞 8.肺功能測驗: (1) 肺機械學 (2) 呼吸生理—血液氣體分析 9.氧氣治療,氣霧治療 10.呼吸器使用之適應症及併發症 (1) 壓力性呼吸器 (2) 容積性呼吸器 11.呼吸道維護 (1) 氣管內管之插管 (2) 氣切管之使用 12.咳血 四.腎臟生理學、病理學及治療: 1.腎衰竭 (1)腎前性 (2)腎因性 (3)腎後性 2.體液溶積、滲透壓及電解質間之變化 3.酸鹼平衡 4.血液及腹膜透析之原理 98 5.泌尿道出血 五.中樞神經系統的生理、病理及治療原則: 1.昏迷 (1)代謝性 (2)外傷性 (3)感染性 (4)腫瘤性 (5)血管性(含缺氧、失血及出血) (6)藥物中毒及過量 2.腦死之診斷 3.抽搐障礙 六.代謝性及內分泌的重症疾病: 1.滲透性及膠質性壓力 2.營養 (1) 經腸胃道式營養 (2) 非經腸胃道式營養 3.內分泌疾病 (1) 甲狀腺風暴 (2) 黏液水腫性昏迷 (3) 腎上腺亢進危機 (4) 抗利尿激素的代謝不正常 (5) 糖尿病: 酸性昏迷及高滲透壓性昏迷 低血糖症 (6) 腎上腺髓質 七.感染性疾病的生理、病理及其治療原則: 99 1.抗生素的使用及其副作用 2.特殊感染單位的防治護理 3.嚴重感染 4.菌血症及菌血性休克 5.免疫不全病患的感染 6.重症病患的院內感染和投機性感染 八.與血液病相關之急症: 1.急性凝血異常 2.抗凝血及溶血治療 3.凝血因子治療的原則及併發症 4.急性溶血性異常 5.腫瘤疾病及抗腫瘤治療的急性症候群 6.急性溶血異常 7.免疫力被抑制病患的急性異常 8.鐮形紅血球病患的危機 9.血漿過濾術 九.腸胃系統的急症: 1.急性胰臟炎 2.上腸胃道出血,含靜脈曲張的出血 3.下腸道出血 4.急性肝衰竭 5.有毒性巨結腸 6.急性腸胃道穿孔 7.食道破裂 8.急性腸胃道發炎 9.腸道急性血管異常 100 十.泌尿及婦產科急症: 1.阻塞性尿路異常 2.尿路出血 3.懷孕的嚴重併發症 十一.外傷及燒傷的內科處理: 1.多器官外傷的治療 2.中樞神經系統的外傷(含腦部及脊髓部) 3.骨骼外傷,含脊椎骨 4.胸部外傷 5.腹部外傷含挫傷及貫穿傷 6.壓碎傷 7.燙傷 十二.毒物學 十三.手術前後問題之處置及麻醉併發症之處理 十四.急症藥理學: 1.藥物之代謝、毒性及排泄 十五.監視系統、醫學工和及生物統計: 1.預後指數及嚴重度之評估 2.侵襲性之心臟監視系統 3.非侵襲性之心臟監視系統,包括心電圖 4.腦部監視包括腦壓、腦血流、代謝速率等 5.呼吸監視系統 6.代謝監視(氧氣消耗量、二氧化碳產生量、呼吸商) 7.顯影技術(如胸部 X 光、核子醫學攝影、電腦斷層攝影、血管攝影等)。 十六.重症醫學之病理生理學 十七.重症醫學之法律及道德觀 101 十八.重症醫學之心理學與精神科急症 十九.行政管理原則及技術: 1.病歷記載之原則包則包括 SOAP,問題導向的病歷記載 2.重症患者及創傷病人處理的優先次序 3.重症醫學訓練計畫 4.加護中心組織及人員安置 102 急診醫學科第一年住院醫師(前三個月)臨床訓練必需熟悉之技術 一.神智不清患者呼吸道之維護,氣管內插管(經口、經鼻),緊急氣切術 二.呼吸 1. 人工甦醒袋之使用 2. 呼吸器之使用,包括 PEEP,CPAP,IMV 及脫離呼吸器等 3. 使用間歇性陽壓呼吸(IPPB)、濕化器(Humidifier)、噴霧器(Nebulizer) 及誘發性肺活量計(Incentive Spirometer) 三.循環: 1.動脈穿刺術及採血 2.置放中央靜脈導管、動脈導管及肺動脈導管 3.心臟電擊器之使用 4.暫時性心律調整器的放置與處理 四.基本及高級復甦術(含 ACLS, APLS, ATLS, EMS) 五.腸胃道 1.放置食道球控制食道靜脈瘤出血 六.監視系統及醫學工程: 1.轉換器(Transducer)之使用,包括歸零及校正 2.各項記錄器之使用 七.胸廓、心包膜穿刺及引流 八.腹膜灌流術 九.脊椎穿刺 103 教學活動內容說明 一.晨會/Case conference/三日內迴診病例討論會:選擇前日二十四小時內較特殊之 個案進行討論。選案原則如下: 1. 到院前已死亡(DOA)之個案病歷 2. 到院內二十四小時內死亡之個案病歷 3. 送手術之個案病例 4. 四十八/七十二小時再迴診之個案病歷 5. 轉院之個案病歷 6. 滯留四十八小時之個案病歷 7. 新住入急診加護病房之個案病歷 8. 診斷上仍有疑異之個案病歷 9. 有糾紛之醫療案例 由總醫師依上述原則選案,於晨會提出報告,並由會議主持人裁示處理之原則。 該日輪值住院醫師需做會議記錄。 二.全院學術專題演講:由本院教學部主辦,由主治醫師或特聘之院外具專長之演 講者,針對某一特殊主題進行專業性之論述。 三.死亡及罹病討論會:針對前一週死亡之於急診醫學科內之病患,進行討論。由 總醫師挑選一次病案,指派特定住院先做病案整理,同時方請相關主治醫師為 指導者,進行討論。並做會議記錄。 104 四.急診行政及品質會議 1. 行政會議:出席者為主任,護理長,社工師,各班指揮及總醫師。依討論之 事項邀請相關單位人員列席,討論急診內部相關作業流程可改進事項,異常 狀況,醫療糾紛,醫病關係,教學訓練,人員調派等問題。 2. 品質會議:出席者為急診醫學科全體人員包括主任、主治醫師、總醫師、住 院醫師、實習醫師、急診科專科助理、護理長、護理人員、行政書記,討論 內容以維持每月的醫療品質指標及標準救治流程之建立,醫療人員教育訓練 與醫療各科工作之協調為主。如與其他醫療科之作業有效集處,並邀請相關 單位及人員列席或逕自將會議記錄送交全院性工作協調會討論。 五.主治醫師教學迴診 每日上午十時迄十二時及晚間九時至十二時分別為日班及夜班主治醫師教學迴 診時間。輪值領導(Leader)主治醫師率日班住院醫師,實(見)習醫師迴診病患並 做教育。此時,臨床工作之進行全由其他主治醫師及臨床研究員執行,以免影 響教學活動之進行。教學活動以迴診型式進行時,陪同住院醫師要在病歷上留 下教學記錄。 六.BOOKING READING /JOURNAL MEETING 每週一,三,五中午利用午餐時間舉行 Booking reading (Pain Management. Sedation and analgesia procedures. High altitude medicine)。由總醫師指定相關雜 誌,選定文章交由指定之住院醫師事前加以整理並簡短報告;由李宜恭主任主 105 持並加以討論。 七.急救討論會:由總醫師挑選前一週急救 (Resuscitation) 之病例,進行討論,由 相關主治醫師為指導者,可邀請護理人員參與討論。 106 107