Medically Important Bacteria
advertisement
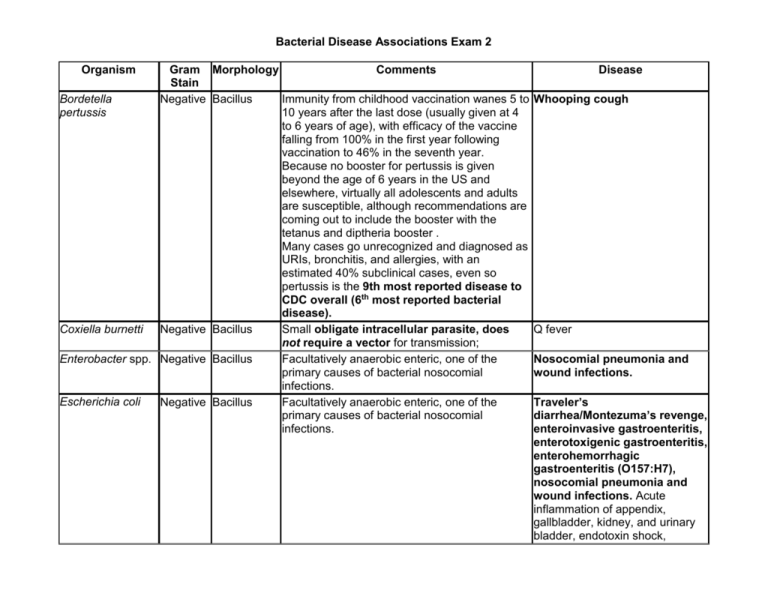
Bacterial Disease Associations Exam 2 Organism Gram Morphology Comments Stain Bordetella Negative Bacillus Immunity from childhood vaccination wanes 5 to pertussis 10 years after the last dose (usually given at 4 to 6 years of age), with efficacy of the vaccine falling from 100% in the first year following vaccination to 46% in the seventh year. Because no booster for pertussis is given beyond the age of 6 years in the US and elsewhere, virtually all adolescents and adults are susceptible, although recommendations are coming out to include the booster with the tetanus and diptheria booster . Many cases go unrecognized and diagnosed as URIs, bronchitis, and allergies, with an estimated 40% subclinical cases, even so pertussis is the 9th most reported disease to CDC overall (6th most reported bacterial disease). Coxiella burnetti Negative Bacillus Small obligate intracellular parasite, does not require a vector for transmission; Enterobacter spp. Negative Bacillus Facultatively anaerobic enteric, one of the primary causes of bacterial nosocomial infections. Escherichia coli Negative Bacillus Facultatively anaerobic enteric, one of the primary causes of bacterial nosocomial infections. Disease Whooping cough Q fever Nosocomial pneumonia and wound infections. Traveler’s diarrhea/Montezuma’s revenge, enteroinvasive gastroenteritis, enterotoxigenic gastroenteritis, enterohemorrhagic gastroenteritis (O157:H7), nosocomial pneumonia and wound infections. Acute inflammation of appendix, gallbladder, kidney, and urinary bladder, endotoxin shock, Haemophilus influenzae Negative Bacillus Carbohydrate capsule important to pathogenicity, especially those with type b capsular antigens - the acronym Hib refers to this; Childhood vaccination Klebsiella pneumonia Negative Bacillus Pseudomonas aeruginosa Negative Bacillus Facultatively anaerobic enteric, one of the primary causes of bacterial nosocomial infections. Extraordinary nutritional spectrum, can degrade many different organic molecules - may grow in disinfectants. Aerobic but can sometimes substitute nitrogen for oxygen, becoming anaerobic. One of the primary causes of bacterial nosocomial infections Small obligate intracellular parasite, requires a vector for transmission. Facultatively anaerobic enteric, inhabits intestinal tracts of animals, birds, reptiles; 3rd most reported disease to CDC. Facultatively anaerobic enteric, most common species in U.S., 10th most common disease reported to CDC (7th most reported bacterial disease). Small obligate intracellular parasite, requires a vector for transmission. Lacks peptidoglycan and lipid A, cells are fragile. HGA is a tick borne disease formerly attributed to Ehrlichia spp.; transmitted by Ixodes scapularis Small obligate intracellular parasite, does not require a vector for transmission; requires ATP from host. 2 forms, elementary bodies, metabolically inactive resistant transmissible form, and reticular bodies, metabolically active inside host. Most common STD in the U.S. and number 1 most reported disease to CDC. Rickettsia rickettsii Negative Bacillus Salmonella enterica Negative Bacillus Shigella sonnei Negative Bacillus Anaplasma phagocytophilum Negative Coccus Chlamydia trachomatis Negative Coccus Invasive disease caused by Haemophilus influenzae may produce any of several clinical syndromes, including meningitis, bacteremia, epiglottitis, or pneumonia. Most common cause of surgical wound infections Nosocomial pneumonia and wound infections, urinary tract infections, burns, dermatitis, otitis externa; can cause septicemia, abscesses, and meningitis. Rocky Mountain spotted fever Dysentery (Salmonellosis) Dysentery (Shigellosis) Human granulocytic anaplasmosis (HGA) Trachoma, the leading cause of blindness worldwide, and nongonococcal urethritis (STD). Ehrlichia spp. Negative Coccus Neisseriae gonorrhoea (gonococcus) Neisseriae meningitidis (meningococcus) Negative Coccus Negative Coccus Borrelia Negative Spirochete burgdorferi Treponema Negative Spirochete pallidum Bacillus anthracis Positive Bacillus Small obligate intracellular parasite, requires Human moncytotrophic a vector for transmission. HE is a tickborne ehrlichiosis (HME) disease transmitted primarily by the Lone Star tick. 2nd most reported disease to CDC Gonorrhea, neonatal gonorrheal ophthalmia Adult and childhood vaccination for those at risk Meningitis (meningococcal; 2nd most common cause of bacterial meningitis) Vector borne; 5th most reported disease to CDC 4th most reported disease to CDC Lyme disease, relapsing fever Syphilis Endospore forming, zoonotic, causes disease Anthrax in animals (cattle, goats, sheep). Endospores may remain viable in soil and animal products for many years. Transmitted to humans by contact with infected animals, especially hides or wool. Produces a powerful exotoxin; cutaneous, gastrointestinal, and inhalational forms of the disease, inhalational is most dangerous form. Spores used as a weapon of bioterror. Clostridium spp. Positive Bacillus Endospore-forming obligate anaerobe, toxin producing, non-invasive, found in soil, sewage, honey, house dust, animal and human intestinal tracts. Clostridium Heat sensitive neurotoxin, binds to motor neurons, produces flaccid Botulism, infant botulism most botulinium paralysis, may kill by respiratory or cardiac failure. Or may be used common form in U.S., commonly cosmetically to reduce wrinkling by inhibiting facial muscle contraction. associated with feeding infants Endospores are destroyed by commercial canning, may be present in less than 1 year honey - spores home canned foods not properly heated during canning (spores germinate and produce toxin. germinate and produce toxin) or cooked before eating. Clostridium perfringens Normal microflora of human intestinal tracts, histotoxic, causes necrotizing infection of skeletal muscle if spores introduced to anoxic tissue, gas produced from carbohydrate fermentation. Enterotoxin produced in gut during sporulation causes hypersecretion associated with gastroenteritis. Clostridium tetani Neurotoxin (tetanospasmin) inhibits relase of inhibitory N.T.'s at spinal cord motor nerves, causes spastic paralysis, trismus (lockjaw) tonic convulsions; death usually results from spasms of diaphragm and intercostal respiratory muscles. Childhood vaccination, should receive booster at least every 5 years along with diptheria booster and now pertussis booster. Clostridium difficile Produces antibiotic-associated colitis days to weeks after antibiotic therapy. Corynebacterium Positive Bacillus Childhood vaccination, should receive booster diptheriae with tetanus booster Listeria Positive Bacillus Excreted in animal feces, found in soil, water, monocytogenes and dairy products. Survives at refrigerator temperatures, can survive in phagocytes, can cross the placenta. Only gram + that contains endotoxin. Gas gangrene, C. perfringens gastroenteritis Tetanus Causes nearly half of all nosocomial diarrhea Diptheria Common cause of food poisoning, 4th most common cause of bacterial meninigitis, can cross the placenta and cause still birth or neonatal meningitis. Mycobacterium Positive Bacillus Acid-fast. Numbers increasing along with drug Tuberculosis tuberculosis resistance; 8th most reported bacterial disease to CDC Mycobacterium Positive Bacillus Acid-fast. Not easily transmissible, requires Leprosy leprae intimate contact with bodily secretions Mycoplasma Positive* Bacillus No cell wall; *stain gram-negative but Pneumonia (Mycoplasmal or pneumonia Pleomorphic genetically related to and taxonomically primary atypical ) classified with the low G+C gram-positive bacteria Enterococcus spp. Positive Coccus Facultatively anaerobic enteric, naturally Most common cause of (faecalis, faecium) resistant to penicillin; one of the 3 gm+ cocci surgical wound infections. important as causes of nosocomial infections Staphylococcus aureus Positive Coccus Normal flora, coagulase +, one of the 3 gm+ cocci important as causes of nosocomial infections Coagulase Staphylococcus (Staphylococcus epidermidis) Positive Coccus Normal flora, coagulase -, one of the 3 gm+ cocci important as causes of nosocomial infections. Streptococcus pneumoniae Positive Coccus Childhood vaccine, recommended for at risk adults. Streptococcus pyogenes (group A beta-hemolytic streptococci) Positive Coccus 10th most reported bacterial disease to CDC Most common cause of nosocomial pneumonia, MRSA accounts for 52.3% of S. aureus nosocomial infections. Also causes boils (furuncles), carbuncles (abscesses), acute bacterial endocarditis, folliculitis, food poisoning, impetigo, otitis media, pimples, scalded skin syndrome, sties, and toxic shock syndrome. Not as invasive or toxic as S. aureus, most important cause of nosocomial sepsis. May also cause acute bacterial endocarditis. Most common cause of pneumonia (pneumococcal pneumonia; typical pneumonia), most common cause of bacterial meningitis (pneumococcal meningitis), otitis media; Nosocomial pneumonia and wound infections. Invasive group A streptococcal infections (pneumonia, bacteremia in association with cutaneous infection, deep softtissue infection - cellulitis, myositis, necrotizing fascitis, meningitis, peritonitis, osteomyelitis, septic arthritis, puerperal fever, neonatal sepsis, and nonfocal bacteremia). Also causes strep throat, scarlet fever, rheumatic fever, impetigo, otitis media, and erysipelas.