CLINICAL CASE

CLINICAL CASE
Unit 4: Reproductive Endocrinology, Infertility and Related Topics
Objective 48: Infertility
A 37-year-old female and her 37-year-old husband present with the complaint of a possible fertility problem. The couple has been married for 2 years. The patient has a
4-year-old daughter from a previous relationship. The patient used birth control pills until one-and-a- half-years-ago. The couple has been trying to conceive since then and report a high degree of stress related to their lack of success.
The patient reports good health and no problems in conceiving her previous pregnancy or in the vaginal delivery of her daughter. She reports that her periods were regular on the birth control pill, but have been irregular since she discontinued taking them. She reports having periods every 5-7 weeks. Past history is remarkable only for mild depression. Imipramine 150 mg qhs for the last 8 months is her only medication. She works as a cashier, runs 12-24 miles each week for the last 2 years, and has no history of STDs, abnormal Paps, smoking, alcohol or other drugs. She has had no surgery.
The patient’s partner also reports good health and reports no problems with erection, ejaculation or pain with intercourse. He has had no prior urogenital infections or exposure to STDs. He has had unprotected sex prior to his current relationship, but has not knowingly conceived. He has no medical problems or past surgery. He works as a long-distance truck driver and is on the road 2-3 weeks each month. He smokes a pack of cigarettes a day since age 18 and drinks 2-3 cans of beer 3-4 times a week when he’s not driving. He occasionally uses amphetamines to stay awake while driving at night. The couple has vaginal intercourse 3-5 times per week when he is at home.
Physical exam
The patient is 5’9” and weighs 130 pounds. Breast exam reveals no tenderness or masses, but bilateral galactorrhea on compression of the areola. Pelvic exam reveals normal genitalia, a well-estrogenized vaginal vault mucosa and cervical mucus consistent with the proliferative phase. The uterus is anteflexed and normal in size without masses or tenderness.
Laboratory
Patient
TSH
Free T4
Prolactin
FSH
LH
Results
2.1 mIU/ml
1.1 ng/dl
60 ng/ml
6 mIU/ml
4 mIU/ml
Normal Values
0.5-4.0 mIU/ml
0.8-1.8 ng/dl
<20 ng/ml
5-25 mIU/ml
5-25 mIU/ml
Basal body temperature chart shows a monophasic temperature graph.
Partner
Semen analysis revealed 2 cc of semen, 4 million per mL, 30% normal forms and 20% motility.
Management
The patient’s major infertility factor is anovulation; the most likely cause is hyperprolactinemia from imipramine. The prolactin level is elevated, consistent with drug-induced hyperprolactinemia. The patient was instructed, in conjunction with her therapist, to taper off the imipramine. Her follow-up basal body temperature chart was biphasic, consistent with ovulatory cycles.
The patient’s partner, however, has a semen analysis that is consistent with oligospermia. The couple was given their options of: 1) In Vitro fertilization with
ISCI; 2) artificial insemination with partner’s sperm; 3) artificial insemination with donor sperm; or 4) adoption.
Teaching points
1.
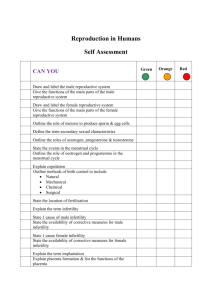
Multiple causes must be considered for infertility diagnosis and treatment.
Female and male reproductive anatomy and physiology should be reviewed in order to encompass the large differential diagnosis and the different factors that may contribute to infertility or subfertility.
2.
Infertility is defined as one year of unprotected coitus without conception.
Infertility may be primary: a woman who has never achieved pregnancy, or secondary: a woman who has achieved pregnancy in the past. Causes of infertility include tubal and pelvic pathology (35%), male problems (35%), ovulatory dysfunctional (15%), unexplained infertility (10%) and unusual problems (10%).
3.
Components of an initial infertility workup include a thorough history and physical examination. Laboratory investigations include a semen analysis to assess male causes of infertility, a method to document that ovulatory cycles are occurring and, often, a hysterosalpingogram to rule out tubal disease.
4.
Disorders of ovulation include polycystic ovarian syndrome (PCOS), hyperprolactinoma, thyroid dysfunction and hypothalamic causes and may be diagnosed by history, as well as laboratory tests that document the occurrence of ovulatory cycles. Basal body temperature recording, urinary LH testing, endometrial biopsy and luteal phase serum progesterone testing are all tests that may help confirm the presence or absence of ovulation.
5.
Dysfunction of the hypothalamic-pituitary-ovarian axis and medical illness, including thyroid disease and pituitary tumors, can cause ovulatory disturbances. Further laboratory workup targeting these problems should be
performed when history, examination and initial laboratory evaluation indicate ovulatory dysfunction. Medication can also cause ovulatory problems.
6.
Ovulatory dysfunction may sometimes be treated with correction of medical disease or change of medications. Most often, ovulatory dysfunction is treated empirically with ovulation induction agents such as clomiphene citrate. A thorough understanding of the normal physiology and pathophysiology of the menstrual cycle aids greatly in the understanding of ovulatory dysfunction.
7.
Management of tubal disease is often surgical, including lysis of adhesions and removal of tubal obstruction via either laparoscopy or laparotomy, depending on the severity of the disease.
8.
Male fertility problems include varicocele, duct obstruction, sperm antibodies, hypogonadism, testicular hyperthermia, drug use and industrial pollutants.