Haematology Reference Ranges
advertisement

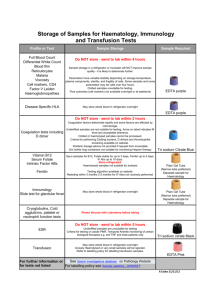
BEAUMONT HOSPITAL DEPARTMENT OF HAEMATOLOGY Laboratory User Guide November 2011 Prepared by: Geraldine Healy Approved By: Dr. Philip Murphy Dr. John Quinn Dr. Patrick Thornton Revision 2: November 2011 Review Date: December 2012 Document Number: HAEMG-LP-038 Page 1 of 21 CONTENTS Introduction ..............................................................................................................3 Location of the Haematology Department ............................................................3 Contacting the Haematology Department .............................................................3 Clinical Advice and Laboratory Test Interpretation ...........................................4 Laboratory Opening Hours ....................................................................................4 Out-Of-Hours Services ............................................................................................4 General Sample Collection & Labelling Guidelines: In-House...........................5 General Sample Collection & Labelling Guidelines: External ...........................7 Specimen Containers ...............................................................................................8 Transport ..................................................................................................................8 Sample Rejection Criteria .......................................................................................9 Storage.....................................................................................................................10 Guidelines for Haematology Specimens: .............................................................11 Guidelines for Haematology Specimens referred to External Hospitals ..........12 Guidelines for Flow Cytometry Specimens .........................................................13 Guidelines for Routine Coagulation Specimens..................................................14 Guidelines for Non-Routine Coagulation Specimens .........................................15 Guidelines for Coagulation Specimens referred to External Hospitals ...........17 Coagulation Reference Ranges ............................................................................19 Haematology Reference Ranges ...........................................................................20 Test Results .............................................................................................................21 Document Number: HAEMG-LP-038 Page 2 of 21 Introduction This user guide is designed to enable medical staff to obtain the maximum benefits from the services provided by the Haematology Department. It provides information on the tests performed both in the laboratory and those referred to other centres. Location of the Haematology Department The Haematology Department is located on the lower ground floor of Beaumont Hospital within the Pathology block. Contacting the Haematology Department Haematology Office- Enquiries Reception- Results 01-8092655 01-8092669 Medical Enquiries Consultant Haematologists Dr. P. Murphy Dr. J. Quinn Dr. P. Thornton (Mon/Wed/Fri only) 01-8093382 01-8092664 01-8093382 Haematology Clinic-Coleman K. Byrne (CKB) 01-8092150/2622 Scientific Enquiries Chief Medical Scientist Mr. Karl O’Regan 01-8092662 Senior in Charge of Coagulation Ms. G Healy 01-8092657 Haematology Laboratory Coagulation Laboratory Flow Cytometry Laboratory Morphology Special Haematology Out-Of-Hours 01-8092703 01-8092656/2663 01-8092763 01-8094776 01-8093226 Bleep 252 Pathology Reception-Appointments Hospital Reception Warfarin Clinic 01-8092674 01-8093000 01-8092083/3982 Document Number: HAEMG-LP-038 Page 3 of 21 Clinical Advice and Laboratory Test Interpretation Haematology clinical advice can be obtained by contacting: The CKB unit at 8092150/2622. The Haematology Registrars at bleep 887/ 276 The Haematology Senior House Officers at bleep 347/ 490/ 461 Interpretation of Laboratory Tests / procedures may be obtained by phoning the Chief Medical Scientist or by requesting a senior member of staff. Laboratory Opening Hours The routine opening Hours of the Haematology department are: Monday-Friday 8am – 8pm Please ensure samples arrive in the laboratory as early as possible in the working day. There is no routine Saturday, Sunday or Bank Holiday service. Out-Of-Hours Services The Medical Scientist on call may only be contacted by bleeping 252. The following emergency tests will be processed - Full blood count (FBC) - Coag screen / INRs /APTTs - D-Dimer - Fibrinogen - Infectious Mononucleosis (IM) screen - Malaria screen - ESR (only where temporal arteritis is suspected) - Sickle screen (urgent theatre cases only) - Other tests in special circumstances may be arranged with the Laboratory. Send Specimens by means of the pneumatic tube system (2703/2656) If a test is urgent hand deliver it to the Laboratory, and notify the Medical Scientist on-call. Document Number: HAEMG-LP-038 Page 4 of 21 General Sample Collection & Labelling Guidelines: In-House In-house samples must be labelled with the order-com label, (which must be placed over the existing bottle label). A list of the appropriate test abbreviations can be found in the tables present in pages 8-15 of this manual. Thrombophilia Screen (TPSC) requests will no longer be able to be ordered on PIPE. In order to process a TPSC request, all requests must first be discussed with the Haematology SpR, Haematology Registrar, or consultants (Dr. Philip Murphy, Dr. John Quinn or Dr. Patrick Thornton) available via the hospital switchboard. If sanctioned, please do the following: Complete a Coagulation Downtime Request Form with the Patient's name, DOB, Episode Number, Ward/Location and Thrombophilia Screen (TPSC) requested Include patient relevant clinical information on the form Indicate on the form the name and bleep number of the Doctor on the Haematology team who has sanctioned the TPSC Date, sign and include the requesting Doctor's bleep number Take FOUR 2.9 mL Tri-sodium citrate 9NC (green) samples and Take ONE 2.7 mL EDTA (pink) sample Send the samples to the Coagulation Laboratory Please note: Anti Cardiolipin Antibodies are processed by Immunology and are not part of this screen. TPSC's which have NOT been sanctioned by the Haematology Team will be rejected and not processed by Scientific Staff. For more details please read the `Thrombophilia Guidelines' which can be accessed through `Haematology Guidelines' on the Intranet under `Medical Quicklinks'. Urgent samples. Due to the large number of samples received daily with the order-com label marked as STAT, it is not possible to process each of these as urgent samples. Therefore it is imperative that if a sample is urgent, the laboratory must be notified by either telephoning the laboratory staff with the urgent sample details or hand delivering the sample directly to the laboratory. Samples from Oncology and CKB must have a blue cap placed over the lid of the sample to be prioritised. Blood Film Requests: Please phone the Haematology Lab if a blood film is required on an FBC, specifying the clinical indication for this request. Add-On D-Dimer Requests: Please phone the Coagulation Lab to prioritise this request Document Number: HAEMG-LP-038 Page 5 of 21 During Computer Downtime: the Haematology Request form (HAEMG-LF007) and/or the Coagulation Request form (HAEMC-LF-026) must be correctly filled out for in-house samples. The forms must include the following details: 1. Patient name 2. Date of Birth and/or Current episode number 3. Test required 4. Ward/area patient is located 5. Dr. Signature The sample must be labelled with at least two unique identifiers, one of which must be the patients’ name. A hardcopy of the result will be sent either by Chute or porter collection to the requesting ward, which must be filed in the patient’s chart. Document Number: HAEMG-LP-038 Page 6 of 21 General Sample Collection & Labelling Guidelines: External GP samples must be accompanied by a fully completed Beaumont Hospital GP request form, to include the following details: The following details must be recorded on the request form: Name of Patient DOB Practice Name/Address Requesting Clinician Tests requested The following details should also be recorded on the request form: Patients Address An Episode number if available Gender Date of collection/time Drawing doctor’s or phlebotomist’s signature Clinical details (where appropriate/relevant-required for ESR)* Contact number The following details must be recorded on specimen: Name DOB Date and time of specimen collection The following details should be recorded on specimen: Drawing doctor’s or phlebotomist’s signature ESR is clinically indicated in the following circumstances only: Temporal Arteritis/Polymyalgia Connective Tissue Diseases Lupus In all other cases, C-Reactive Protein (CRP) is the preferred test. HbA1c is analysed in the Biochemistry Laboratory. Patients requiring a FBC and HbA1c will require 2 EDTA 2.7mL samples sent with the test request. Document Number: HAEMG-LP-038 Page 7 of 21 Specimen Containers The Sarstedt monovette system is the specimen collection system in use in Beaumont Hospital. Cap Contents Application Volume Purple Tri-sodium citrate 4NC Pink EDTA ESR only 3.5 mL Most general Haematology 2.7 mL Flow cytometry 1.2 mL- Paediatric PCR Green Tri-sodium citrate 9NC Coagulation 2.9 mL 1.2 mL- Paediatric Red 0.82mg Magnesium/mL Haematology 2.7mL Orange RPMI & Sodium-Heparin Flow Cytometry 2mL White No anti-coagulant Haptoglobin assay 2.7ml or 7.5ml Transport Transport specimens to the laboratory as quickly as possible. Place all specimens in bio-hazard bags and transport to the laboratory in a way as to minimise damage or risk of leakage. Samples may be sent via the AV tube system (to 2703/2656) or can be collected by Porters in the wards at defined times. Collection times (in-house) are as follows: Monday- Friday collections at 10.00, 12.00, and 15.00 Saturday-Sunday collections at 9.00, 11.00, and 13.00 Collection times (GPs): Each GP on the courier schedule has collections at least twice weekly. Exception to the above: Platelet Function Assay (PFA 100) The PFA 100 test must be tested 30 mins to 4 hrs after collection and transported via the porters to the laboratory. Do not use the chute system as it will interfere with the platelets and consequently the results. This test will only be carried out if prior arrangements have been made with the Coagulation Laboratory. Document Number: HAEMG-LP-038 Page 8 of 21 Sample Rejection Criteria Unlabelled / Incorrectly labelled specimens i.e. without two unique patient identifiers Leaking or improperly sealed containers. Overfilled: ESR samples where blood is collected into the lid of the container. Coagulation containers where the blood is filled beyond the marking on the label. Underfilled: ESR samples must be 85mm full. 2.7 ml FBC and RETFBC samples must have a minimum of 1mL of blood. 1.2 ml paediatric samples should have at least 500µL for FBC (up to first indentation of the lid) and at least 1mL for RETFBC. Coagulation samples must be filled to the line. Obvious inadequacy of specimen for the test(s) required i.e. only one coagulation specimen for a Thrombophilia screen Clotted samples with the exception of a serum clotted sample which can be used for IM and Haptoglobin testing. Incorrect anti-coagulant: Samples in the wrong container for the requested test. Any samples where the laboratory has been informed the specimen was collected from the incorrect patient. Haemolysed Coagulation specimens and ESR samples 10mL and 7.5mL EDTA samples for FBC and RETFBC analysis. These samples are not compatible with the laboratory cap piercing analysers. 8.2 mL sodium citrate samples for Coag screens, INR’s or WINR’s. These samples are not compatible with the Coagulation analysers. All in-house TPSC's which have NOT been sanctioned by the Haematology Team will be rejected and not processed Aged Samples:Coagulation samples must be less than 8 hours old. Samples greater than 8 hours old the clotting factors begin to deteriorate which lead to inaccurate results. INR/WINR samples must be less than 24hrs old. ESR samples should be less than 8 hours old. Samples greater than 8 hours can lead to a false lowering of results. Reticulocyte samples must be less than 6 hours old. Samples greater than 6 hours old can lead to an incorrect result. Flow Cytometry samples for lymphocyte analysis must be less than 48 hours old and stored at room temperature. Samples for white blood cell precursor analysis must be taken in Sodium Heparin and RPMI and be less than 72 hours old and stored at room temperature. FBC: EDTA samples must be <48hours Blood film preparation: samples must be <12 hours old D-Dimer: Request for D-Dimer received >8 hours post sample collection. Note for External Users: ESR requests which do not have the appropriate clinical information will be rejected. In the event whereby 1 EDTA sample is received for FBC and HbA1c analysis, the HbA1c will be given priority and the FBC request rejected. In the case of an in-house sample being rejected, the requesting ward will be informed by telephone and a record of the rejected sample will be kept in the laboratory. Note: Only External INR requests that are rejected will be telephoned. Document Number: HAEMG-LP-038 Page 9 of 21 Storage Samples are stored for one week at room temperature (15-25ºC), after testing, with the exception of ESRs, which are discarded after reporting. Additional requests may be added to the original request as follows: Reticulocyte count may be added following receipt of a FBC sample but must be requested within 6 hours of specimen collection to produce accurate results. Blood film analysis may be added following receipt of a FBC sample but must be requested within 12 hours of specimen collection to produce accurate results. Depending on the time of collection of the FBC and the stability of the assay, the following tests may be added to an FBC sample: IM, G6PD, Sickle screen, PK, HB_El. A Malaria screen can be added onto an FBC within 1 hour of collection. Fibrinogen and D-Dimers may be added following receipt of a coagulation sample but must be requested within 8 hours of specimen collection to produce accurate results Document Number: HAEMG-LP-038 Page 10 of 21 Guidelines for Haematology Specimens: Test Container Required Volume /ml Sample Full Blood count EDTA (pink capped) Platelet Check* 0.82mgMg2+/mL 2.7ml standard In-house: 2-4 Hours 7.5ml and 10ml EDTA 1.2 ml paediatric External: 1 Working Day samples not acceptable Urgent: 1 hour 2.7mL In-house: 2-4 Hours Arrange in advance with External: 1 Working Day laboratory to obtain sample tube. ESR Trisodium citrate 3.5 ml Must be 4NC /3.5 (purple) filled to the line Reticulocyte Count Haptoglobins Infectious mononucleosis Screen Blood film examination G6PD Screen Malaria Expected Further Information Turnaround Time FBC PLTEXACT (Can only be ordered in the laboratory) Addressograph label must only be placed over the manufacturer’s label on the bottle. EDTA (pink 2.7ml standard In-house: 2-4 Hours 7.5ml and 10ml EDTA capped) 1.2 ml paediatric External: 1 Working Day samples not acceptable Urgent: 1 hour Clotted 7.5ml standard 2.5 Working Days EDTA samples no longer sample (white) 2.7 ml paediatric acceptable (August 2011) EDTA (pink 2.7ml standard 1 Working Day capped) Or clotted 1.2 ml paediatric sample (white) ESR EDTA(pink capped) Must be requested by phoning the Laboratory directly or on GP request form EDTA(pink capped) EDTA(pink capped) Document Number: HAEMG-LP-038 1 Working Day Urgent for Temporal Arthritis: 1 hour BHIS Code 2.7ml standard 1-3 Working Days Sample must be <12 hrs old 1.2 ml paediatric With the exception of the weekend and films referred to the Consultant for Review. 2.7 ml Standard 5 Working Days. Refer to page 19 for G6PD Quantitation. 2.7 ml Standard 1-2 hrs for Rapid When RDT is negative, Diagnostic Tests(RDTs) films will be processed on Blood films 4 hours to the next working day next working day depending on results of Page 11 of 21 RETFBC HP IM G6_PD M_PARA Test Container Required Sickle solubility EDTA (pink capped) Screen Fresh EDTA Paroxysmal (pink capped) Nocturnal Haemoglobinuria Screen Bone marrow Bone marrow aspirate aspirate on glass Volume /ml Sample Expected Further Information Turnaround Time 2.7ml Standard RDTs 1 Working Day 2.7ml Standard 1 Working Day A minimum of 5 slides. Stained for next Working Slides must be labelled in BMA Day. Await Consultant pencil with the patients’ reporting. Surname and second unique identifier either D.O.B or episode number. slides. Needles and slides available in Haematology. BHIS Code For Urgent pre- Anaesthetic SICK_SC screen contact Laboratory. Arrange in advance with Laboratory personnel. Sample must be freshly drawn PNH Guidelines for Haematology Specimens referred to External Hospitals Test Specimen required Referral Laboratory Plasma Viscosity 1 X EDTA sample 2.7 ml 1 X EDTA sample 2.7 ml 1 X EDTA sample 2.7 ml 1 X EDTA sample 2.7 ml Haemoglobin Electrophoresis HbA2 St James Hospital, Special Haematology Laboratory, Dublin 8. Test Mnemonic VISC Hb_EL HbA2 Phone No.’s: 01-4162909 (Plasma G6PD Deficient G6_PD Viscosity) Samples 01-4162394 (Hb_EL, HbA2, for Quantitation Positive Sickle Screens 1 X EDTA sample G6PD, PK) Hb_EL 2.7 ml 1 X EDTA sample Fax No.: 01-4103513 Pyruvate Kinase PK 2.7 ml Document Number: HAEMG-LP-038 Page 12 of 21 Turnaround Time Verbal reports available after one week Written reports after 6 weeks Guidelines for Flow Cytometry Specimens Test Container Required Vol /ml Expected Further sample Turnaround Information Time§ CD4 EDTA (pink capped) 2ml 2 Working days Samples must be <48 CD4 hours old Lymphocyte Subsets EDTA (pink capped) 2ml Lymphoproliferative Panel EDTA (pink capped) 2ml 2 Working days Samples must be <48 LY_SUB hours old 4 Working days Samples must be <48 LY_PRO hours old Acute Leukaemia Panel Sodium Heparin (orange capped) with 1ml RPMI 2-3ml Paroxysmal Nocturnal Haemoglobinuria Fresh EDTA (pink capped) Document Number: HAEMG-LP-038 BHIS Code 2 Working days Must be arranged in AL advance with prior consultation with the lab. Containers are only obtained from the lab. 2.7ml 2 Working Days Arrange in advance PNH Standard with Laboratory FLOW personnel. Sample must be freshly drawn. Page 13 of 21 Guidelines for Routine Coagulation Specimens Specimen Container Required Coagulation Screen Coag Screen (UFH) Prothrombin Time Activated Partial Thromboplastin Time INR Trisodium citrate 9 NC/2.9 mL (green capped) Warfarin office INR D-Dimer Fibrinogen Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Document Number: HAEMG-LP-038 Number of Vol /ml Expected samples sample Turnaround required Time§ 1 1 1 1 1 Must be In-house: 2-4Hours filled to the External: 1 working Day line Urgent: 1 hour Must be In-house: 2-4Hours filled to the External: 1 working Day line Urgent: 1 hour Must be In-house: 2-4Hours filled to the External: 1 working Day line Urgent: 1 hour Must be In-house: 2-4Hours filled to the External: 1 working Day line Urgent: 1 hour Must be In-house: 2-4Hours filled to the External: 1 working Day line Urgent: 1 hour Page 14 of 21 Further BHIS Information Code COAGSC COAGHEP PT APTT INRs only are INR stable for 24 hrs Warfarin Office WINR contact no. 01-8092083 Sample must be D-DIMER <8 hours old Sample must be FIBN <8 hours old Guidelines for Non-Routine Coagulation Specimens Specimen Container Required Mixing study Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Factor Assays Number of Vol /ml Expected Further Information BHIS samples sample Turnaround Code required Time 2 2 Thrombophilia screen Trisodium citrate 9 NC/2.9 mL (green capped) Protein C Antithrombin III Activated protein C resistance Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Document Number: HAEMG-LP-038 4 1 1 1 Must be 1 week Sample must arrive in MS filled to the Laboratory before 4 pm. line Must be Case dependent, Tests done in batches. For FII, FV, filled to the maximum urgent requests, contact the FVII, FVIII, line 14 days laboratory in the morning, FIX, FX, may be able to facilitate FXI, FXII testing that day. Must be 2-3 weeks Batch tested. TPSC filled to the The Thrombophilia Cannot order line screen (TPSC) includes on PIPE. the following tests: PT, Use a APTT, FIBN, D-DIMER, downtime LA, AT3,PC, FPS, APCR form, MUST and discuss 5LEIDENand PT_MUT. clinical Hence, these details with Tests do not need to be Haematology Ordered on an individual team first. basis. Must be 2-3 weeks Batch tested. PC filled to the Patient must be off line warfarin for a minimum of 2wks to perform this assay. Must be 2-3 weeks Batch tested AT3 filled to the line Must be 2-3 weeks Batch tested APCR filled to the line Page 15 of 21 Specimen Container Required Number of Vol /ml Expected Further Information BHIS samples sample Turnaround Code required Time Von Willebrand factor Trisodium citrate 9 Lupus anticoagulant Thrombin time Reptilase time Platelet function analyser (PFA-100) Factor V leiden PT mutation NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) Trisodium citrate 9 NC/2.9 mL (green capped) EDTA sample EDTA sample (pink) EDTA sample (pink) 2 1 1 1 1 Must be Case dependent, filled to the maximum 14 line days Must be 2-3 weeks Batch tested filled to the line VWF Must be 2 weeks filled to the line Must be 2 weeks filled to the line Must be 4 hours filled to the line TT EDTA & trisodium citrate samples are required. These must NOT be sent in the AV tube system as this may activate the platelets. They MUST be sent to the lab by the porters. 1 6-8 weeks 1 Only tested if APCR is positive. 6-8 weeks LA Order on a downtime form PFA 5LEIDEN PT_MUT 1 Same day turnaround times refer to results being available to the requesting clinician on the same working day. Results are available on ward look-up or on Healthlink. Clinicians receiving results by post will incur an added delay. Document Number: HAEMG-LP-038 Page 16 of 21 Guidelines for Coagulation Specimens referred to External Hospitals Test Specimen required Referral Laboratory Test Turnaround Time Mnemonic ADAMTS 13 Assay 2 fresh coag samples <4hrs old should be Haemostasis Research Unit, Hand written Note: Only processed to centrifuged immediately. Frozen plasma Haematology Dept, request facilitate storage in aliquots immediately in the -70ºC freezer University College London, 70ºC freezer, do not get st 1 Floor, 51 Chenies Mews, reports back London, WC1E 6HX, UK 00442076796416 Coag sample taken 4hrs post-heparin Coagulation Laboratory, tested every Anti-Xa Assay ANTI XA Batch administration. This can be sent fresh if within St. Vincent’s Hospital, Friday 4 hours of collection. Double spin, separate and Elm Park, Written reports: 4-6 freeze plasma aliquots in the -20ºC freezer if Dublin 6. weeks. being left over night. 01-2094395 Verbal report available Note: St Vincent’s must be phoned prior to within 2 days. the sample being sent. The type of LMWH must be written on the request form. Double spin, separate and freeze plasma Coagulation Laboratory, aliquots in the -20ºC freezer. NCHCD, 1 clotted sample, 1 coag sample, 1 vial of Rialto Gate, HIT Screen (Heparin-Induced heparin the patient was on. Stable un separated St. James’ Hospital, Thrombocytopenia) @ room temperature for a few hours or must be Dublin 8. frozen overnight., if they cannot be sent that 01-4162956 FXIII Platelet Aggregation Contact must be made by the Haematology team at Beaumont with the Haematology Studies team at St. James’ Hospital. The referral of the patient must be discussed by both teams. Ristocetin CoFactor 2 freshly drawn coag samples, sent immediately or separated & frozen in the (RICOF) -20ºC freezer. PLTAGG FXIII HIT reports: 4-6 reports: 5 Verbal report available within 2 days. day. Note: ideally the patient must not be on heparin and the APTT has returned to normal. Document Number: HAEMG-LP-038 Written weeks. Written weeks. By appointment only. reports:4-6 VWF_RCO Written weeks Verbal report available within 5 days. Page 17 of 21 Test Specimen required Referral Laboratory Test Turnaround Time Mnemonic (drug) Whole blood is not suitable, separated St. Thomas’s Hospital, WDL plasma or serum required. The haemophilia centre, 1ST Floor, North wing, Lambert Palace Rd,London SE17EH. This test is extremely sensitive to pre Biomnis, Plasminogen PAI-1 Activator Inhibitor analytical conditions. A freshly drawn coag Three Rock Road, sample must be mixed immediately by Sandyford Business Estate, gentle inversion at least six times following Sandyford, collection. Must be centrifuged Dublin 18 immediately after collection. Frozen 01-2958545 immediately and kept frozen until analysis. Freshly drawn coag samples, double spun, Free Protein S FPS separated & frozen in the -20ºC freezer. Warfarin Level Document Number: HAEMG-LP-038 Page 18 of 21 2-3 weeks 2 Weeks 2-3 Weeks Coagulation Reference Ranges Test APCR APR APTT AT3 COAGSC D-Dimer FII FV FVII FVIII FIX FX FXI FXII FVL FIBN INR LA MS PFA 100 PT PT_MUT PC RT TPSC TT VWF WINR Normal Range/result Negative 1.5-2.5 24-38 80-120 See PT and APTT <0.5 60-140 60-140 60-140 60-200 60-140 60-140 60-140 60-140 Negative 1.5-4.5 Different ranges depending on the reason the patient was put on Warfarin. Negative Corrected to within the PT and APTT normal ranges. CEPI<164 Units Ratio seconds U/dL μg/mL U/dL U/dL U/dL U/dL U/dL U/dL U/dL U/dL g/L Ratio CADP<116 12-15 Negative 70-140 <20 See individual requests APCR, PC, FPS, AT3 and LA. <22 43-150 Therapeutic Range is dependent on clinical condition seconds seconds U/dL Secs Document Number: HAEMG-LP-038 seconds secs U/dL Ratio Page 19 of 21 Haematology Reference Ranges Test FBC ESR HP IM M_PARA PNH RETFBC SICK_SC Test parameters Normal Range/Result Units Male Female 13-17.5 11.5-16.5 Hb 0.37-0.54 0.335-0.54 PCV 4-6.5 3.8-5.8 RCC 79 -96 MCV 27 -32 MCH 12.1-14.3 RDW 140 -400 PLTS 4.0 -11 WBC Neut 2.0 -7.5 Lymph 1.0 -4.0 Mono 0.2- 1.0 Eosin 0.04- 0.4 Baso 0.01- 0.1 1- 12 1-20 0.45-2.43 NEGATIVE NEGATIVE NEGATIVE RETIC % 0.2 -2.0 RETIC(Abs) 20 - 80 NEGATIVE Document Number: HAEMG-LP-038 g/dL L/L x1012/L fL pg % x109/L x109/L x109/L x109/L x109/L x109/L x109/L mm/hr g/L % x109/L - Page 20 of 21 Test Results Results when authorised, are available on the BHIS / PIPE. GP results are also available on Healthlink. Results falling outside defined alert limits will be telephoned to the appropriate ward/ personnel. Note: This may not be possible due to an inability to contact the relevant clinical personnel out of hours. In such cases, the critical alert value will be telephoned the following day. The Following Table is a list of these results that will be phoned: Table: Critical /Action Limits Test Hb PLT Neutrophils IM Malaria Screen Sickle Screen INR/WINR D-Dimer Fibrinogen Flow Cytometry Morphology Ward/ OPD GP/ Nursing Homes/ External Hospitals <7.0 g/dL <7.0g/dL 9 <20 x 10 /L <50 x 109/L <0.5 x 109/L <0.5 x 109/L Positive Positive Positive Positive Positive Positive >5.0 >8.0 (Mon-Thurs) >5.0 (Fri) >20µg/mL >5µg/mL <1.0 g/L <1.0 g/L New Leukaemia patients New Leukaemia patients When Haematology team Printed report sufficient, no suggests referral contact action necessary. the clinical team. If patient discharged, bring to attention of Haematology secretary to contact GP. Note: It is imperative that contact details of the requesting doctor and/or location of the patient are attached to the test request so that critical results can be phoned immediately. Document Number: HAEMG-LP-038 Page 21 of 21