HCV RNA + HCV RNA
advertisement

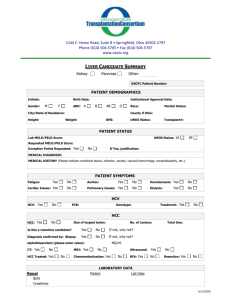
DISTRIBUTION OF HEPATITIS C VIRUS GENOTYPES IN PATIENTS ON REGULAR HEMODIALYSIS PROGRAM 1 Running head: HEPATITIS C VIRUS GENOTYPES IN HEMODIALYSIS PATIENTS KEY WORDS: Hepatitis C virus, anti HCV, HCV genotypes, reverse transcription polymerase chain reaction, chronic HD patients. Authors: Jasna Slaviček1, Zvonimir Puretić1, Smilja Kalenić2, Božica Rebrović2, Blaženka Grahovac3, Snežana Glavaš-Boras1, Zvonimir Mareković1, Vladimir Slaviček4 , T.Golubić,5 Institution: 1 Urology Department, University Hospital Centre Zagreb, Rebro, Kišpatićeva 12, 10000 Zagreb 2 Clinical Laboratory Diagnosis Institute, Microbiology Laboratory, University Hospital Centre Zagreb, Rebro, Kišpatićeva 12, 10000 Zagreb3 Transfusion Medicine Institute, Petrova 3, 10000 Zagreb ,4Traumatology Hospital, Draškovićeva 19, 10000 Zagreb , 5 Department of Infectology Hospital Čakovec Address of author: Jasna Slaviček M.D. M.S. Dialysis center, Urology Department University Hospital Center Zagreb Kišpatićeva 12, 10 000 Zagreb 2 J. Slaviček Abbreviations HCV hepatitis C virus HD hemodialysis HCV RNA hepatitis C virus RNA RT PCR reverse transcription polymerase chain reaction EIA enzyme immunoassay anti HCV hepatitis C antibodies 3 J. Slaviček ABSTRACT Background and purpose. Hepatitis C (HC) prevalence is relatively high in patients on regular hemodialysis (HD) program. Variations in the viral genome may lead to different clinical manifestations of the disease and to variations in the response to treatment. The distribution of HCV genotypes is related to the geographical area and depends on population-specific risk factors. The purpose of the study was to assess the distribution of HCV genotypes in patients on regular hemodialysis. Matherial and methods. Testing for HCV RNA was performed in 95 patients on regular hemodialysis in Dialysis Centre, Urology Department, University Hospital Center Zagreb, using Amplicor HCV test and quantitative Amplicor Monitor test. Inno Lipa HCV test was used for the determination of HCV genotype. Results: HCV RNA was positive in 40/95 patients (53.6%). In the group of 56 anti HCV+ (EIA 3 test), HCV RNA was positive in 38 (67.6%)patients. Positive HCV RNA was found in 2 anti HCV negative patients who later developed clinical signs of acute hepatitis C. Genotype 1b was dominant (29/40, 72.5%), followed by type 3 (8/40, 20%). Types 4 and 1a were found in two patients. In one patient HCV genotype could not be determined. All HCV RNA positive patients presented with viral load ranging from 5x103 to 6x106 copies/ml. Conclusion. The distribution and frequency of the HCV genotypes in hemodialysed patients followed the general distribution pattern recorded in Croatian blood donors with a predominance of types 1b and 3a that were found in 71.6% and in 10,7 % of cases respectively. The presence of four different HCV genotypes may be explained by the relatively high patient turnover in the 4 Center, where patients from other centers come for the treatment of complications of vascular access. J.Slaviček INTRODUCTION Hepatitis C virus (HCV) was discovered 1989 as the etiologic agent of non-A non- B hepatitis ( 1). It is transmitted primarily by the pareneteral route, and the infection tends to became persistent in approximately 60-80 % of infected persons. It can cause a wide spectrum of liver disease , ranging from asymptomatic acute hepatitis to cirrhosis and hepatocelular carcinoma (2).Prevalence of antibody to HCV ( anti HCV) positivity among chronic hemodialysis( HD) patients averages 10 % with some centers reported rates greater than 60 %(3). Both incidence and prevalence studies have documented an association between anti HCV positivity and increasing years on dialysis , independent of blood transfusion (4). These studies as well as investigation on dialysis –associated outbreaks of hepatitis C , indicate that HCV transmission might occur among patients in a HD center because of incorrect implementation of infection control practices (5,6). Patients on regular HD are a patient group at a high risk for the development of hepatitis C which is an important agent of liver disease in this clinical setting.The disease prevalence varies from 2% to 62% . In Northern Europe, for instance, this prevalence is below 10%, while in Eastern Europe is higher than 40% (7,8).In the past the use of non screened blood and blood products was a major mode of transmission of HC in HD centers At present , posttransfusional hepatitis C occurs in less than 5 % of hemodialysis patients. Nosocomial infection is considered the major mode of transmission of HC in HD centers (9-10). Exact mode of transmission of HCV in the hemodialysis population remain unresolved. 5 Hepatitis C virus is a heterogenous virus by nature of its replicative strategy. Major differences in the nucleotide sequences of HCV isolates are found throughout the genome and indicate the J. Slaviček presence of distinct HCV genotypes, defined as having nucleotide divergence of more than 20 %. The wordwilde distribution of the genotypes is variable : HCV genotypes 1,2 and subtype 3a appear to be the most prevalent in North America, Europe and Japan , and genotype 4 is common in Africa.Among American patients with chronic hepatitis C , nearly 75% have genotype 1 ( 11). Recent data for Croatian patients revealed the genotype 1b with 49 % as most common in patients with chronic hepatitis C.(12). HCV can be classified into six major genotypes according to nucleotide sequence in different regions of the genome.( 13,14) Genotypic differences have been observed with regard to the viral load , severity of liver disease and response to interferon therapy.( 15,16). The relative prevalence of HCV genotypes shows marked geografical variations with obvious clinical implications. Studies of HCV genotypes in patients on hospital hemodialysis are still insufficient. No study on HCV genotypes distribution in regular HD patients has been published in Croatia so far. The aim of our study was to determine the HCV genotype distribution in our patients on regular HD. 6 J. Slaviček PATIENTS AND METHODS Ninety-five (57 male and 38 female) patients on regular HD in the Dialysis Center, Urology Department, UHC Zagreb, were included in the study. Only patients regularly dialyzed in the Center were included. The patients are dialyzed three times weekly in three shifts. As a rule, patients are always dialyzed on the same machines, except when the machine is out of order; then it is replaced with a spare one. HCV positive patients are dialyzed on separate machines, in the same room with HCV negative patients, but in their half of the room. Hepatitis B positive patients are dialyzed in a separate room. A nurse normally cares for 4 HD patients. The staff caring for HCV positive patients usually does not attend to HCV negative ones, except if there are problems with AV fistula puncture. All dialysis equipment is disposable. Filters are not reused. Dialysis machines are sterilized with hypochlorite and citric acid after each shift. Hepatitis markers, HBsAg and anti HCV are routinely assessed trimesterally, and anti HIV twice yearly in patients and twice yearly in the personnel. Liver biochemistry analyses (AST, ALT, alkaline phosphatase, gamma-glutamyl transpeptidase (-GT), bilirubin) are routinely performed monthly. An earlier testing confirmed an anti HCV positivity in 54/95 HD patients (EIA 3rd generation, Ortho, Abbott and RIBA 3, Ortho). Serum HCV RNA was determined by means of PCR method ( Amplicor HCV PCR kit, Roche Systems, Basel , Switzerland), where reverse transcription (RT), amplification reaction and nonisotope hybridization are used. The sera were stored at 4-8o C if the test was performed within 72 hours, or at -20 o C or -80 o C if the test was done after a longer period of time. HCV genotypes were assessed using reverse hybridization reaction, the so-called line probe assay (LiPa, 7 J. Slaviček Innogenetics, Zwijndrecht, Belgium). In all patients serum aspartate (AST), alanine aminotransferase (ALT) were measured spectrophotometrically using multi-enzyme autoanalyzer. Here are the Hospital laboratory normal values: 6-26 U/L for AST and 6-34 U/L for ALT. RESULTS Demografic features of our patients are shown in table 1. In 40/95 ( 53.6%) patients on regular HD tested, HCV RNA was found positive. In the group of 56 anti HCV positive patients, HCV RNA was positive in 38 patients (67.6%). (Table 2). A positive HCV RNA was also found in 2 anti HCV negative patients. In the later course of the disease, they both developed acute hepatitis C with elevated transaminase levels and a seroconversion after 6-8 weeks. In one patient with a clinical presentation of acute hepatitis C, who became also anti HCV positive within a month, in spite of repeated testing in two different laboratories and using two different techniques, routine and in house method, serum HCV RNA was repeatedly negative. Viral load varied between 5x103 and 6x10 6 copies per milliliter of serum. HCV RNA positive finding correlated well with transaminase elevation ( Table 3). We did not find any significant correlation between viral load and transaminase levels. The patient with the greatest load (6x106) had quite normal transaminase levels for many years. This can be explained by an extrahepatic proliferation of the virus. The virus genotype assessment proved that type 1b is predominant in our Center. It was found in 29/40 patients (72.5 %), and type 3 in 8/40 ( 20%), respectively. The type 1a was confirmed in one patient and in one 8 J.Slaviček female patient type 4, which is otherwise exceptionally rare (Table 4). Due to a very low number of copies, genotype could not be assessed in one patient. DISCUSSION HCV infection is high prevalent in HD patients (4). HCV RNA was found in 67.6% of anti HCV positive patients. Among EIA 3 positive samples which were negative to RT-PCR method, 32.4% of patients either recovered from the HCV infection or their viral load is very low, below the sensitivity limit of RT-PCR, or they suffer from a fluctuant viremia . In a later testing we confirmed that HCV RNA became positive in two anti HCV positive patients, who were HCV RNA negative in the first assessment. Finally, HCV RNA negativity obtained by using RT-PCR technique in HCV infected patients may be caused by an exclusive localization of HCV in the liver or peripheral blood mononuclear cells ( PBMC) or in other non-blood compartments (16). This was the case with the patient in whom transaminase levels abruptly increased (ALT 340 U/L) and who seroconverted after 6 weeks, but remained HCV RNA negative over the whole follow-up period of 12 months. In 2 patients a positive HCV RNA was the first sign of HCV infection. In these patients transaminase levels increased after a week or two, and over 6-8 weeks the patients became anti HCV positive. HCV viremia with very high blood levels of virus particles, without biochemical signs of liver inflammation and with a negative HCV , could reflect extrahepatic proliferation of the virus (15, 16). This was the case with our patient with the greatest load (>6x106 copies/ml), but with normal transaminase levels ( ALT 6-8 U/L, AST 4-6 U/L, GT 10 U/L) over the entire 2-year follow-up period. 9 J. Slaviček There is a relatively small group of patients with a detectable serum HCV RNA, but who were still anti HCV negative. (17,18). We found HCV RNA in the serum of 3 anti HCV negative patients At the repeated testing at the same laboratory and additional controls in other institutions, however, all three patients proved HCV RNA negative. We explained this as a contamination. HCV has a high mutation rate. It exists in nature as a population of diverse, but closely related genomes (11,13,21). The determination of HCV genotypes is based on the comparison of nucleotide sequences of the virus genome and confirmed by phyllogenetic analysis. Both blood donors and patients with chronic hepatitis from countries in Western Europe and the USA all show frequent infection with genotypes 1a, 1b,2a,2b,and 3a, although the frequencies of each may vary. There is a trend for relatively more frequent infection with type 1 b in southern and eastern Europe. Type 1a and 3 a are more common in intravenous drug users in Europe (7,11,20,22).In Croatia a study of HC genotypes was done in blood donors.(12). The study proved that type 1b is dominant in Croatian blood donors, then types 1a and 3. Type 4 is very rarely found. In our HD patients type 1b is prevalent, similarly to HD populations in Korea, France and Japan . Type 3 is less frequent. Type 4 was found in only one female patient. This type is very rare in Europe and has been described in central Asia and in the Middle East (11). It was detected in a lady who was previously submitted to a surgery for the correction of a wrongly healed shin bone fracture. During the surgery, the patient received a blood transfusion, so 10 it may have been a posttransfusion hepatitis. The high prevalence of HCV infection in hemodialysis patients has been attributed not only to the frequency of blood transfusion among J.Slaviček these patients but also to increasing years on dialysis , suggesting that HCV may be transmitted between patients in the dialysis unit probably as a result of poor infection control practices ( 4,9). A precise route of transmission is not known. A transmission by contaminated hands from medical personnel or from patient to patient is presumed (4,6,14,20). The introduction of erythropoietin in the treatment of renal anemia and obligatory screening of blood donors to anti HCV has significantly reduced the spreading of posttransfusion HC. It is estimated that the risk for this type of hepatitis is 1: 100 000 blood units (6,10, 18). In smaller HD centers one HCV genotype only was found, which confirms the hypothesis of nosocomial spreading of HCV within a center.(12,17) Several different HCV genotypes in the investigated material can be explained by a relatively high patient fluctuation in our Center, to which patients from other smaller centers are referred for the treatment of vascular access complications. Spreading of HC in our Center is probably also a result of nosocomial infection, as a number of HCV positive patients have never received a blood or blood derivatives transfusion. There have been no data about other possible sources of infection, e.g. drug abuse or tattooing either. We would like to stress the need for a strict observing of measures of infection prevention in HD centers. 11 J. Slaviček Table 1 Demografic features of our hemodialysis patients N 95 Gender 57 m Age 16 yrs –75 yrs HD duration 1,4 yrs – 18,5 yrs , 38f 12 J. Slaviček Table 2 Relation between HCVRNA positivity and anti HCV positivity. Anti HCV+ (EIA 3) Anti HCV – ( EIA 3) n % n % HCV RNA + 40 71.5 2 5,1 HCV RNA - 16 28.5 37 92,3 Total 56 100 39 100 13 J. Slaviček Table 3 Correlation between transaminase values and HCV RNA HCV RNA + HCV RNA - ALT elevated 21 5 ALT normal 19 50 Total 40 55 p <0,5 Legend : ALT normal ( 6-26 U/L) ALT elevation ( exceeding the upper normal reference level) 14 J. Slaviček Table 4 Distribution of HCV genotypes in hemodialysis patients. HCV genotype N % 1b 29 72,5 3 8 20. 1a 1 2,5 4 1 2,5 unknown 1 2,5 Total 40 100 15 J. Slaviček References: 1. Choo Q-L,Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Isolation of c DNA clone derived from a blood –borne non – A, non- B ,viral hepatitis genome. Science 1989; 224:359-362. 2. Aledort LM. Consequences of chronic hepatitis C . A review article for the hematologist. Am J Hematol 1993; 44: 29-37. 3. Tokars JI, Miller ER, Alter MJ, Ardini MJ. National surveillance of dialysis associated diseases in the United State1995. ASAIO Journal 1998; 44: 98-107. 4. .Dentico P,Buogiorno R, Pastore G, Schiraldi O. Prevalence and incidence od hepatitis C virus in hemodialysis patients : study of risk factors. Clin nephrol 1992; 38: 49- 52. 5. Mondelli MV, Cristina G, Piazza V, Cerino A, Villa G, Salvadeo A. High prevalence of antibodies to hepatitis C virus in hemodialysis units using a second generation assay. Nephron 1992 ; 61: 350- 351 6. Mayer LA, Alter MJ. Hepatitis C virus in the hemodialysis setting: a review with recommendations for control. Seminars in Dialysis. 1994; 7 : 124-127. 7. Bingulac-Popović J, Grahovac B, Zambeli J, Mihaljević I, Dražić V, Pirc-Tiljak D, Petrovečki M, Balija M, Grgičević D. Detection of hepatitis C virus by polymerase chain reaction among Croatian blood donors and patients. Period biol 1998;100(3):389-394. 16 J. Slaviček 8. McOmish F, Yap PL,Dow BC, Follet EAC, Seed C, Keller AJ, Cobain TJ, Krusius T, Kolho E, Naukkarinen R, Lin C, Lai C, Leong S, Medgyesi GA, Hejjas M, Kiyokawa H, Fukada K, Cuypers T, Saed AA, Al- Rasheed AM,Lin M, Simmonds P. Geographical distribution of different hepatitis C virus genotypes in blood donors : An international collaborative survey. J.Clin Microbiol 1994; 32: 884-889. 9. Sampietro M, Badalamenti S, Salvadori S, Corbetta N. High prevalence of a rare hepatitis C virus in patients treated in the same hemodialysis unit: Evidence for nosocomial transmission of HCV. Kidney Int 1995; 47: 911-917. 10. Linn HH, Huang CC, Sheen IS, Lin DY, Liaw YF. Prevalence of antibodies to hepatitis C virus in the hemodialysis unit. Am J Nephrol 1991;11 : 192-194. 11. Fabrizi F, Bacchini G, Raffaele L, Erba G, Locatelli F. Anti HCV antibodies and transaminase concentrations in hemodialysis patients : a study with second-generation assays. Nephrol Dial Transplant 1993; 8: 740-743. 12. Kohler H . The prevalence of hepatitis C in different countries of the ERA/EDTA area. Nephrol Dial Transplant 1995; 10: 468-469. 13. Hruby Z, Sliwinski J, Molin I, Zalewska M, Knysz B, Czyz W, Steciwko A, Bogucki J, Gladysz A. High prevalence of antibodies to hepatitis C virus in three hemodialysis centres in south -western Poland. Nephrol Dial Transplant 14. Simonds 1993; 8: 740-743. P. Variability of hepatitis C virus. Hepatology ; 1995; 21:570-585. Dow BC , Follet EAC, Jordan T, Mc Omish F, Davidson J, Gillon J, Yap PL, Simonds P. Testing of blood donations for detection of hepatitis C virus. Lancet 1994; 343: 477( letter). 17 J. Slaviček 15. Fabrizi F, Lunghi G, Guarnori I, Raffaele L, Erba G, Pagano A, Locatelli F. Hepatitis C virus genotypes in chronic dialysis patients. Nephrol Dial Transplant 1996; 11: 679-683 17. Buck J, Purcell RH, Miller RH. At least 12 genotypes of hepatitis C virus predicted by sequence analysis of the putative E1 gene of isolates collected worldwide. Proc Nat Acad SciUSA 1993; 90:8234-8238. 18. Martell M, Esteban JL, Quer J. Hepatitis C virus (HCV) circulates as a population of different but closely related genomes: Quasispecies nature of HCV genome distribution. J Virol 1992; 66: 3225-3229. 19. Allander T, Medin C, Jacobson SH. Hepatitis C transmission in a hemodialysis unit. Molecular evidence for spread of virus among patients not sharing equipment. J Med Virol 1994; 43: 415-419. 20. Botte C, Janot C. Epidemiology of HCV infection in the general population and in blood transfusion . Neprol Dial Transplant 1996; 11( suppl 4) : 19 – 21. 21. Roth D. Hepatitis C virus:the nephrologist,s view. Am J Kidney Dis 1995;25:3-16. 22. Kanai K, Kako M, Okamoto H. HCV genotypes in chronic hepatitis C and response to interferon. Lancet 1992;339: 1543. 18