23) Moderate_Sedation
advertisement
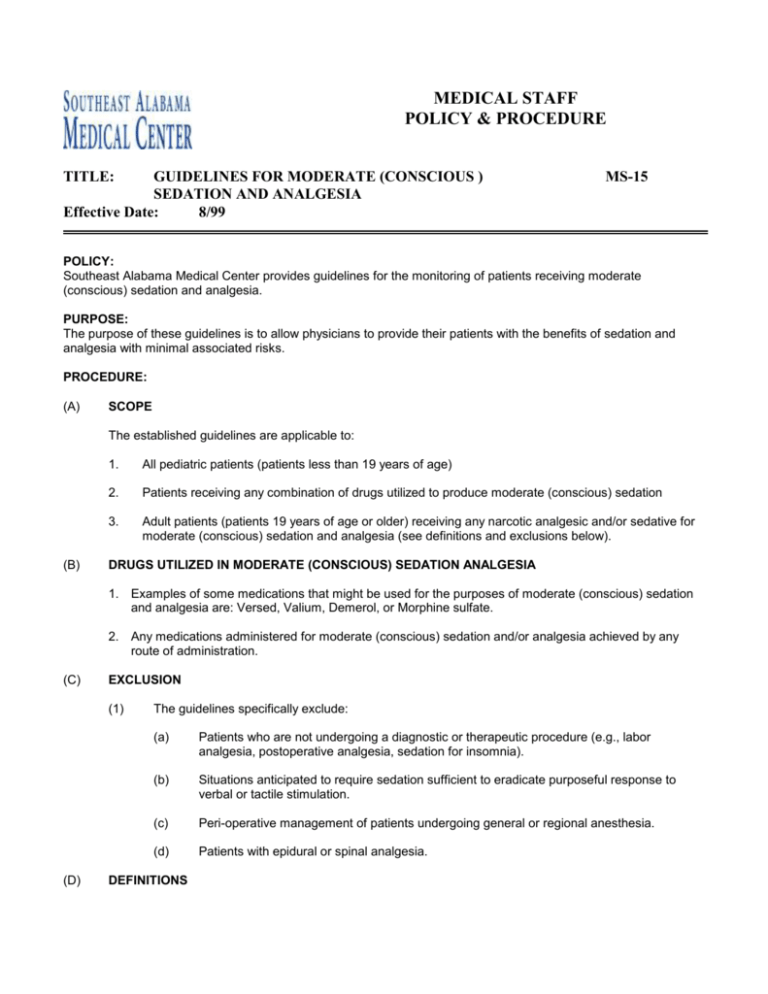
MEDICAL STAFF POLICY & PROCEDURE TITLE: GUIDELINES FOR MODERATE (CONSCIOUS ) SEDATION AND ANALGESIA Effective Date: 8/99 MS-15 POLICY: Southeast Alabama Medical Center provides guidelines for the monitoring of patients receiving moderate (conscious) sedation and analgesia. PURPOSE: The purpose of these guidelines is to allow physicians to provide their patients with the benefits of sedation and analgesia with minimal associated risks. PROCEDURE: (A) SCOPE The established guidelines are applicable to: (B) 1. All pediatric patients (patients less than 19 years of age) 2. Patients receiving any combination of drugs utilized to produce moderate (conscious) sedation 3. Adult patients (patients 19 years of age or older) receiving any narcotic analgesic and/or sedative for moderate (conscious) sedation and analgesia (see definitions and exclusions below). DRUGS UTILIZED IN MODERATE (CONSCIOUS) SEDATION ANALGESIA 1. Examples of some medications that might be used for the purposes of moderate (conscious) sedation and analgesia are: Versed, Valium, Demerol, or Morphine sulfate. 2. Any medications administered for moderate (conscious) sedation and/or analgesia achieved by any route of administration. (C) EXCLUSION (1) (D) The guidelines specifically exclude: (a) Patients who are not undergoing a diagnostic or therapeutic procedure (e.g., labor analgesia, postoperative analgesia, sedation for insomnia). (b) Situations anticipated to require sedation sufficient to eradicate purposeful response to verbal or tactile stimulation. (c) Peri-operative management of patients undergoing general or regional anesthesia. (d) Patients with epidural or spinal analgesia. DEFINITIONS MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION (1) Category 1: Minimal sedation (anxiolysis) -- A drug-induced state during which patients respond normally to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected; (2) Category 2: Moderate sedation/analgesia (“conscious sedation”)-- A drug–induced depression of consciousness during which patients respond purposefully to verbal commands either alone or accompanied by light tactile stimulation. No interventions are required to maintain a patent airway, and spontaneous ventilation is adequate. Cardiovascular function is usually maintained; 2 (3) Category 3: Deep sedation/analgesia – A drug induced depression of consciousness during which patients cannot be easily aroused but respond purposefully following repeated or painful stimulation. The ability to independently maintain ventilatory function may be impaired. Patients may require assistance in a maintaining a patent airway and spontaneous ventilation may be inadequate. Cardiovascular function is usually maintained; and (4) Category 4: Anesthesia -- Consists of general and spinal or major regional anesthesia. It does not include local anesthesia. General anesthesia is a drug-induced loss of consciousness during which patients are not arousable, even by painful stimulation. The ability to independently maintain ventilatory function is often impaired. Patients often require assistance in maintaining a patent airway, and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of neuromuscular function. (5) Drugs/Route of Administration: The drugs used and route of administration in no way determines whether or not anesthesia is present. Sedatives and/or analgesics administered via a non-intravenous route (IM, P0, and PR) can be less predictable than those administered intravenously in terms of depth of sedation and the time it is reached. (E) QUALIFICATIONS FOR ADMINISTERING MODERATE SEDATION AND ANESTHESIA (CATEGORIES 2-4) (1) (2) Moderate or deep sedation and anesthesia will be provided by qualified individuals. Those licensed independent practitioners should be qualified individuals who are well trained in professional standards and techniques: (a) to administer pharmacologic agents to predictably achieve desired levels of sedation and (b) to monitor patients carefully in order to maintain them at the desired level of sedation. Included in the qualifications of individuals providing moderate or deep sedation and anesthesia are competency-based education, training and experience in (a) evaluating patients prior to performing moderate or deep sedation and anesthesia; (b) performing the moderate or deep sedation and anesthesia to include methods and techniques require to rescue patients who unavoidably slip into a deeper than desired level of sedation or analgesia. (3) Practitioners must have appropriate credentials and be privileged to administer moderate sedation and rescue patients from deep sedation; (4) Practitioners must have appropriate credentials and be privileged to administer deep sedation and MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION 3 rescue patients from general anesthesia. (5) Practitioners intending to induce deep sedation must have appropriate credentials and privileged to manage an unstable cardiovascular system, compromised airway and inadequate oxygenation and ventilation. (6) Sufficient numbers of qualified personnel are present (in addition to the licensed independent practitioner) during procedures using moderate or deep sedation to (a) appropriately evaluate the patient prior to beginning moderate or deep sedation and anesthesia; (b) provide the moderate or deep sedation and anesthesia; (c) perform the procedure; (d) monitor the patient; (e) recover and discharge the patient from the post-sedation area and from the hospital premises. (F) PRACTICE GUIDELINES (1) The patient should have an intravenous access prior to the administration of moderate (conscious) sedation. If chloral hydrate is administered, this decision will be at the discretion of the physician/surgeon supervising the procedure. (2) Any procedure utilizing moderate (conscious) sedation should be documented on the Moderate (Conscious) Sedation Record or in a comparable format (i.e., computerized record) containing the required components of documentation. (3) Patients requiring conscious sedation should have a preprocedure assessment, cosigned by the physician/surgeon, which includes, but not limited to (a) A brief focused physical examination by the physician, to include auscultation of the heart and lungs; (b) Evaluation of the airway and the potential for airway obstruction under sedation (i.e., sleep apnea, heavy snoring, airway abnormality); (c) History of previous complications related to sedation analgesia or anesthesia in the patient or blood relatives; (d) Choice of sedation and documentation of patient’s acceptance; (e) ASA classification: ASA Class 1: No organic, physiologic, biochemical, or psychiatric disturbance; ASA Class 2: Mild to moderate systemic disturbance that may or may not be related to the reason for the procedure; ASA Class 3: Severe systemic disturbance that may or may not be related to the MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION 4 reason for the procedure; ASA Class 4: Severe systemic disturbance that is life threatening with or without the procedure; ASA Class 5: Moribund patient who has little chance of survival but is submitted to the procedure as a last result (resuscitative) Emergency Procedure: Any patient in whom an emergency procedure is required (f) History of drug use, including tobacco, alcohol, and other unprescribed or illegal drugs; (g) Time of last oral intake of solids and/or liquids of solids and liquids, or other factors that might increase the risk of aspiration (e.g., obesity, esophageal pathology, hiatal hernia, pregnancy, diabetes); (1) Vital signs: Heart rate, respiratory rate, blood pressure, and oxygen saturation; (2) Level of consciousness; (h) Proper consents signed with documentation of patient acceptance/agreement with the proposed sedation plan; and (i) Known pregnancy documented; (j) History of either heavy snoring or obstructive sleep apnea. (k) The patient is re-evaluated by the physician immediately before moderate or deep sedation use and before anesthesia induction. The assessment should include, but not limited to: (1) vital signs; (2) status of airway (l) Each patient’s moderate or deep sedation and anesthesia care is planned by the physician. The patient’s sedation or anesthesia care plan is communicated among care providers. (G) EMERGENCY EQUIPMENT Both adult and pediatric emergency equipment should be readily accessible in locations where conscious sedation is administered. See Attachment A. (H) PREPROCEDURE PREPARATION AND PATIENT EDUCATION (1) Pre-procedure preparation and patient education should include: (2) Obtaining informed consent. (3) An explanation of what to expect before, during, and after the procedure. (4) Instructions and physician orders for fasting should be patient specific. MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION (5) (I) 5 Young children and infants may be encouraged to consume clear liquids up to 2 hours prior to the procedure. MONITORING (1) Qualification of Monitoring Personnel: (a) Patients receiving moderate, deep sedation and anesthesia should be monitored by individuals who are nurses or individuals with ACLS certification. Pediatric patients receiving moderate, deep sedation and anesthesia should be monitored by nurses with current PALs (for pediatric patients ages 1-14 years or as appropriate to age and weight) or NRPs (neonates < 1 year) certification. (b) Individuals who will be monitoring moderate (conscious) sedation analgesia are required to attend an educational inservice on moderate (conscious) sedation annually. (2) Vital signs: (Blood pressure, heart rate, oxygen saturation, and respiratory rate) should be recorded prior to the initiation of sedation. (3) Documentation of Monitoring: The patient should be monitored continuously throughout the procedure and documentation should include: (a) Level of Consciousness: Patient response to verbal commands must be documented every 5 minutes during deepest sedation and drug titration. If not documented as positive, the sedation has converted to anesthesia. If the procedure does not allow patient verbalization, a "thumbs up" or similar appropriate response is acceptable; (b) Ventilation: Ventilatory function via assessment of respiratory rate, depth and adequacy of pulmonary ventilation should be continually monitored; (c) Oxygenation: All patients should be monitored every 5 minutes via pulse oximetry with digital and auditory displays; alarms should be on and loud enough to hear and set at a minimum of 90% saturation. The medical record should reflect SaO2 monitoring every 5 minutes. (d) Hypersensitivity reactions; (e) Hemodynamics: Blood pressure should be measured during the procedure, with the frequency determined by the status of the patient, the depth of sedation, and the degree of stimulation or stress caused by the procedure; (f) Electrocardiographic Monitoring: Heart rate should be continuously monitored. EKG is monitored with patients with significant cardiovascular disease or when dysrhythmias are anticipated or detected. (4) Frequency of Monitoring: Monitored parameters should be documented at least every 5 minutes but may be documented more frequently based on the patient’s condition. The least frequent recording of monitored parameters should include: (1) prior to sedation, (2) after peak sedative effect is reached, (3) on completion of the procedure, (4) during initial recovery, and (5) prior to discharge. MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION (J) POST-PROCEDURE DOCUMENTATION Post-procedure documentation should include the patient's tolerance, level of consciousness, vital signs including oxygen saturation maintenance on room air, and unit and name of person receiving the patient. (K) POST-PROCEDURE MONITORING (1) All patients receiving sedation analgesia should be monitored until appropriate discharge criteria are met. Post-procedure, the patient will be monitored until he/she has achieved a score of nine or ten (9 or 10) of a Post Procedure Observation score, (i.e. Aldrete score), that assigns 0-2 points for activity, respirations, circulation, consciousness, and color. (2) The medical records of patients receiving moderate (conscious) sedation should reflect documentation of post-operative monitoring of blood pressure, pulse and SaO2 (3) The following guidelines should be utilized to determine if the patient is ready for discharge: (L) (a) Patients should be easily arousable and oriented or at their baseline mental status. Health care personnel should instruct parents that infants and small children are at risk for airway obstruction if their head should fall forward while secured in a car seat. (b) Vital signs should be stable as compared to those taken pre-procedure. (c) If reversal agents are used, sufficient monitoring (minimum of 1 hour) should be allowed to evaluate potential re-sedation. Two hours should be allowed for pediatric patients. (d) A responsible adult should accompany a patient being discharged. DISCHARGE INSTRUCTIONS Written discharge instructions, including diet, activity level, medications, and an emergency number should be provided to the patient and his/her caregivers. (M) OUTCOMES Outcomes of patients undergoing moderate and deep sedation are collected and analyzed in the aggregate in order to identify opportunities to improve. 6 MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION 7 ATTACHMENT A EMERGENCY EQUIPMENT FOR AREAS ADMINISTERING MODERATE (CONSCIOUS) SEDATION The following is a guide for both adult and pediatric emergency situations. IV Equipment: Gloves, tourniquets, alcohol wipes, gauze pads, catheter sizes 16g to 24g,intravenous tubing (without obstructive filters) including "microdrip" (60 drops/ml), fluids (LR and 1/2 NS), needles (16g - 22g, intraosseous bone marrow needle), syringes (one ml - 50 ml), 3-way stopcocks, tape Airway Management Equipment: Oxygen source capable of providing 90% FiO2 for 60 min. (pipeline with flowmeter; o-tank with regulator) face masks (infant adult sizes), self-inflating bag, (infant adult sizes), oral and nasal airways (infant adult sizes), lubricant, suction source, Yankauer-type suction device, tonsil tip suction device, intratracheal suction catheters (infant adult sizes), regularly tested laryngoscope handles and blades (MAC 1, 2, & 3 and Miller 1, 2, and 3), endotracheal tubes (uncuffed 2.5mmID-6.0mmID and cuffed 6.0, 7.0 and 8.0mmID), endotracheal tube stylets sized appropriately to fit all tube sizes. Emergency Medications: Naloxone, Flumazenil, Epinephrine, Ephedrine, Atropine, Lidocaine, Glucose - 10% and 50%, Diphenhydramine, Hydrocortisone, ammonia spirits. MEDICAL STAFF POLICY: GUIDELINES FOR MODERATE SEDATION Date adopted by the Quality/Risk Management Committee: Date adopted by the Medical Executive Committee: Date adopted by the Houston County Healthcare Authority: Revisions: 8 August 24, 1999 September 14, 1999 September 28, 1999 January 23, 2001 March 27, 2001 July 30, 2002 January 28, 2003 December 13, 2005 January 13, 2009 January 25, 2010 March 23, 2011 September 15, 2011 February 2012