FELLOWSHIP PROGRAM IN PEDIATRIC EMERGENCY MEDICINE
advertisement

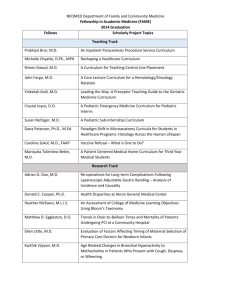
FELLOWSHIP PROGRAM IN PEDIATRIC EMERGENCY MEDICINE MUSC PEM Fellowship Handbook 1. Program Overview a. Role of Chair: departmental policy, financial, academic requirements b. Role of PEM Medical Director: operations, MUSC and ED policy, direction c. Role of Fellowship Director: education, organization (program requirements), evaluation (of program, faculty, trainees and rotations), documentation, support, advocacy d. Organization of Rotations: Requirements and Electives 2. Clinical Care and Leadership a. Progressive Autonomy by fellow year b. Bedside Teaching c. Billing and Documentation d. Procedures and tracking of procedures e. Resident work hours f. ED supervision: flow, conflict resolution, advocacy i. The Attending Role ii. Fellows shifts g. Tracking patients seen 3. Research a. ABP Requirements: “meaningful requirement” b. Biostats/Epi and other stats c. Research Mentor and Scholarship Oversight Committee d. Current projects and future ideas 4. Teaching a. Pediatric Didactics b. EM Didactics c. PALS/ATLS/ACLS 5. Fellow Education a. Book Review b. Core Competencies c. Journal Club d. Peds Fellows’ Conferences e. CME trips/meetings f. Spring Fellow Meeting (Dave Jaffe) 6. Administrative a. Committees/Meetings b. QI Projects 7. Personal a. Timeliness, dress code, hours (moonlighting), conference attendance b. Salary and benefits c. Vacation/sick time/leave-> accountability d. Camaraderie/outings e. Career objectives/development f. Evaluation process rotations/attending/program/conferences General Overview The fellowship is intended for physicians to acquire particular expertise and skills in clinical practice, teaching, investigative research and administrative functions related to the field of pediatric emergency medicine. Worthy applicants are selected through the National Residency Matching Program (NRMP) and are completing their primary training in general pediatrics. The clinical information and skills acquired during residency training will be sharpened and focused as the fellow gains new knowledge and experience pertinent to the emergency management of seriously ill and injured children. The fellow will participate in teaching of both medical and lay personnel on topics related to pediatric emergency medicine in a variety of formats. An understanding of clinical research will be fostered through course study in research design and the development and execution of a research project. In addition, exposure to the administrative aspects of managing an emergency department will be afforded the fellow during the years of training. Clinical Facilities/Experience The MUSC Children’s Hospital serves as the comprehensive regional pediatric center for Charleston and the surrounding area. The Children’s Hospital contains 166 beds and receives an estimated 6,200 admissions annually. It offers a full range of services, including a pediatric intensive care unit, neonatal intensive care nurseries, regional pediatric trauma center, burn unit, an infant/pediatric heart transplant program, kidney transplant program, bone marrow transplant program, and neonatal/pediatric transport services. The Emergency Department (ED) facilities encompass 6,040 square feet on the ground floor of the hospital, including 2 critical care/trauma rooms. There are 12 examination rooms. Within these facilities, care is provided for over 21,000 patient visits per year. Acuity ranges from minor pediatric illnesses to major multiple trauma, with 12% of ED visits resulting in admission to the hospital. The Emergency Department is staffed 24 hours a day by faculty physicians of the Division of Pediatric Emergency Medicine, Pediatric Nurse Practioners and residents from training programs in pediatrics, emergency medicine, and medicine-pediatrics. An emergency transport helicopter system provides excellent pre-hospital care to seriously ill or injured children who require air transport to the Emergency Department and a heliport is located on the top of the Children’s Hospital. The Emergency Department serves as medical control for all pediatric patients transported by Charleston County EMS units and often surrounding counties, as well. The James W. Colbert Education Center and Library is within the medical complex and is open and available to MUSC Children’s Hospital staff. Medline and PubMed search capabilities are available in the Emergency Department and Department offices. CURRICULUM Peds First Year Peds Second Year Peds Third Year PED PED Pediatric Anesthesia General EM PED PED PICU PED PED General Trauma PED Research Orthopedics/Sports Medicine PED PED Elective/Research Research Research PED Toxicology PED PED General EM PED PED PED Elective Research Research Research/Administrative PED General EM PED PED EMS/Transport PED The above time-line is a sample. As it is evident, the bulk of clinical time is physically spent in the Pediatric Emergency Department supervising the care of patients. During the months in which fellows are assigned to the Emergency Department, fellows will work 15 shifts per month. Structure of the Fellowship Program The fellowship is designed for 3 years for persons trained in general pediatrics. See below a sample list of rotations for each discipline: 36 month PEDS TRACK Pediatric ED (16 months) ED Orientation (1 month) Pediatric Anesthesia (1 month) Research (5-6 months) Pediatric Critical Care (1 month) Electives Plastics/Burn Trauma Peds Dermatology Ophthalmology Pediatric Radiology Pediatric Pulmonary Pediatric Cardio thoracic Surgery Pediatric Surgery Pediatric Orthopedics Toxicology High Risk OB/L&D EMS/Transport Administrative During the first year of training, PEM fellows will only work shifts with PEM and EM faculty members, who will supervise and direct patient care. After the first year, fellows will become part-time instructors and may begin to work independently in the pediatric ED, supervising and teaching residents and students and directing patient care. Ongoing documentation of procedural skills training will occur through use of a procedure log online. Each fellow will record each time they successfully perform or supervise a procedure in the Emergency Department or on another rotation in their procedure log. In this way, a record of each fellow’s acquisition of procedural skills will be maintained. The Fellowship Director will include a review of this material in each scheduled evaluation session and use the data to schedule additional procedural skills training as indicated. Fellows will be expected to complete Pediatric Advanced Life Support (PALS) Provider and Instructor course, Advanced Cardiac Life Support (ACLS) Provider course and Advanced Trauma Life Support (ATLS) Provider course during their fellowship. Research Experience Material pertinent to biostatistics and research design will be presented as part of the Pediatric Fellowship conferences, to provide background for performing and reviewing clinical research. Texts and supplemental reading material will be provided. In addition, fellows will be expected to attend and participate in monthly departmental journal club meetings, during which critical review of current literature pertinent to pediatric emergency medicine will be conducted. The Pediatric residents participate in an Evidenced-Based Medicine Curriculum throughout their three years of training; the fellows will be encouraged to attend these weekly educational conferences and review of current literature. Fellows will be expected to design and implement a research project during their three-year fellowship which will satisfy the “Meaningful Accomplishment in Research” requirement of the American Board of Pediatrics in order to sit for the Sub-board examination in Pediatric Emergency Medicine. The “gold standard” of meaningful research accomplishment is first-authorship of a research paper accepted for publication in a peer-reviewed journal. Chart reviews and case reports are rarely acceptable in that they usually do not represent hypothesis-driven research. Book chapters, abstracts, and review articles, while worthwhile exercises, are not acceptable in meeting research publication requirement of ABP. Neither does degree course work (for instance, attaining a Master’s degree) alone currently satisfy the Board requirement for meaningful research. While allowances are made for research which yields negative results, for some grant proposal approved by extramural organizations with critical review processes, and for some manuscripts submitted but not yet accepted for publication, the fellow should plan to acquire and apply the skills related to research design and implementation, data analysis, abstract preparation and presentation, and manuscript submissions during the fellowship tenure. We expect that fellows will submit their completed research projects to a national meeting for presentation. PEM Fellowship Research Mentor and SOC Our fellowship training program will provide a career mentor(s) for each fellow who will assist the trainee in developing an individualized learning plan for the entire training period. This mentor must be responsible for providing the ongoing formative feedback that is essential to the trainee’s attainment of competence in clinical care, teaching and scholarship. The mentor may come from a division or department other than Pediatric Emergency Medicine or Pediatrics. The mentor will be assigned during the first month of the fellow’s training and will become a member of the scholarship oversight committee (SOC), discussed in detail later. The fellow can change mentors after consultation with the fellowship directors. As described in detail later, the SOC will ensure scholarly research opportunity for success for each fellow. The mentor will ensure global scholarly success as mentioned above. To enhance these opportunities, the fellow will participate in several conferences and classes to learn research and teaching skills. These include but are not limited to: Departmental Fellows’ Core Curriculum, Clinical Research Methods, Research Coordinator Development Program, Grantsmanship Workshop, Peds ED Fellows’ Conference, Pediatric Grand Rounds, Apple Tree Society Lectures and GME Lecture Series. Fellows entering the training program are not assigned to a research program. Rather, each fellow is expected to meet with investigators and clinicians within the division to assess current division activities and interests of faculty. From these discussions, the fellow is expected to identify a research question and a mentor to assist the fellow in addressing that question. Each fellow will have a scholarship oversight committee (SOC) with appropriate expertise in scholarly research endeavors; the SOC will be appointed during the first quarter of fellowship. The SOC shall consist of at lease three individuals, one of whom will be a methodologist appropriate to the fellow’s area of scholarly activity and one shall be form outside the fellowship discipline. Fellows are supported if their interests lead to mentorship outside the division. This committee must assess and confirm the presence of adequate scholarly experience for each fellowship trainee, as well as, evaluate the product of the individual’s scholarly experience. The committee will provide a written report after each meeting to the fellowship director. The SOC is also responsible for approving all projects the fellow is involved in, therefore protecting the fellow from pressures to participate in research that would not further his/her training and protecting the fellow from becoming overly committed. By the end of the first year, the fellow should identify his/her research interest, identify his/her mentor, and begin designing his/her project. The research mentor and SOC are responsible for overseeing the development of the research question into a project, including a review of prior work in the area of interest, the generation of a testable hypothesis, the design of studies to test the hypothesis, data collection, and interpretation and presentation of results. In general, it is expected that these steps will be carried out over the next 12-18 months of training. A tool for the development of a timeline is available and encouraged to be used should the SOC and fellow desire. At certain intervals throughout this process, the fellow is expected to present his/her progress in our research portion of fellows’ conference. This is done with the supervision of each fellow’s research mentor. Presentation of results at external meetings is encouraged, with supervision of the SOC and research mentor. Practice sessions for these presentations will occur during research portions of the fellows’ conference. The final stages of the fellows’ research experience involve preparation of results for presentation and publication. This process is under direct supervision of the SOC and research mentor. It is expected that this will occur by the end of the fellow’s training program. Teaching Experience Fellows will prepare and present instructional lectures to students, residents, nurses, and other medical personnel (e.g., emergency medical services personnel) on topics related to pediatric emergency medicine. The department offers many additional opportunities to teach, including Pediatric Advanced Life Support classes, Suture/Wound Management and Splinting workshops, Mock Codes and Sim Lab courses. In addition, one-on-one teaching skills will be developed as fellows precept residents and medical students on clinical cases in the Emergency Department. Teaching activities will be monitored and periodic critique/feedback will be provided. Administrative Experience Fellows will participate in inter- and intra-departmental meetings as they relate to the Emergency Department. As part of this process, policies and procedures will be developed and reviewed. Teaching conferences will incorporate administrative topics such as billing, quality assurance, risk management, disaster planning, and personnel management issues. Fellows will perform quality assurance activities as appropriate within the scope of the department. Educational Conferences One day every other week will be set aside for fellowship educational conferences. The format will vary week-to-week but will include: didactic lecture presentations from faculty within the department and faculty from other disciplines on topics germane to pediatric emergency medicine; review of sections of a major textbook of pediatric emergency medicine; case conference presentations; research conferences; and critical review of contemporary articles taken from a variety of academic journals. Fellows will be expected to have read the appropriate material in preparation for conference and to participate actively in discussions. Attendance and participation will be evaluated. As they become more senior, fellows will be expected to coordinate conferences, arrange speakers, and present material themselves. This will allow them some administrative and teaching experience. See appendix for fellow conference schedule. Evaluation Process A formal review of each fellow’s progress will be made on a semi-annual basis. This will consist of a scheduled one-on-one session between each fellow and the Fellowship Director during which the fellow’s progress in the acquisition of clinical skills, teaching techniques and research endeavors will be assessed and goals created for the next evaluation period. The Fellowship Director will solicit the input of the Pediatric Emergency Medicine faculty regarding the fellow’s performance (clinical skills, bedside teaching, administrative skills, flow management, supervisory performance) in the pediatric ED. Evaluations from elective and required rotations as well as procedure logs and resident feedback regarding teaching will be reviewed. Progress toward satisfactory completion of a research project will also be examined. These semi-annual sessions will further serve as a mechanism for the fellow to provide feedback about the fellowship training program and his/her progress in it, as well as to evaluate the attending faculty on the Pediatric Emergency Medicine staff. Comments will be relayed to the attending staff and the division director in an anonymous fashion to allow for candid feedback from each fellow. In addition to these semi-annual reviews, informal feedback will be provided to each fellow on an ad hoc basis. General training goals for each rotation, required and elective, have been developed and will serve as a template for measuring the progress of the fellow. At the end of each rotation outside of the pediatric emergency department, the fellow will complete an evaluation form designed to assess the strengths and weaknesses of the rotation, as well as the attending faculty and residents supervising the fellow during the rotation. The appropriate faculty contact person for the rotation will also complete an evaluation form assessing the fellow’s performance. These will be reviewed with the fellow by the Fellowship Director in a contemporaneous manner and a copy of each evaluation placed on file. In this way, the fellow will receive ongoing feedback regarding his/her progress. Exceptional or substandard performance will prompt a counseling session between the Fellowship Director and the fellow, as appropriate. These sessions will also be documented and placed on file (see the last section for sample evaluation forms).