alcohol withdrawal: pathphysiology, diagnosis and treatment
advertisement

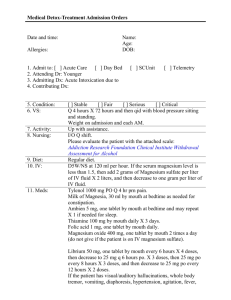
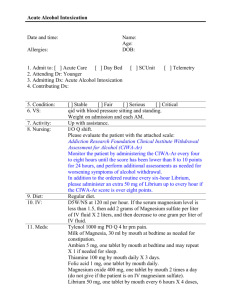
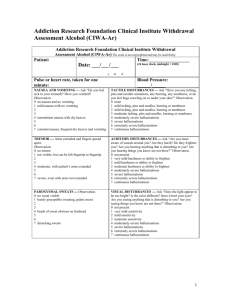
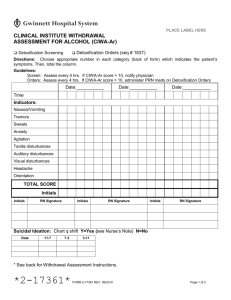
ALCOHOL WITHDRAWAL: PATHOPHYSIOLOGY, DIAGNOSIS ANDTREATMENT Carlos A. Hernandez-Avila,M.D. Department of PsychiatryUniversity of Connecticut School of Medicine Alcohol Medical ScholarsProgram Prepared: April 2005 I. INTRODUCTION Slide1 Slide2 A. Alcohol Dependence (AD), major cause of mortality and morbidity B. More than 2/3 of AD patients in clinical settings have Alcohol Withdrawal (AW) C. AW often presents as anxiety and insomnia. Misdiagnosis can be deadly D. Topics to be covered: Epidemiology Pathophysiology Clinical Picture and Diagnosis Treatment II. EPIDEMIOLOGY A. Epidemiology of Alcohol Use Disorders (AUD):1 Slide3 15.3 million have alcohol abuse or dependence 13 % of men and4 % of women over age 18 More frequent among European-Americans 15-30% of primary care and hospitalized patients 40% trauma patients have blood alcohol levels (BAL) 100 mg/dl B. Alcohol Use Disorders (AUDs) can bedefined:2 a. Slide4 1. Alcohol Abuse: b. Significant impairment/distress in a 12-month period c. Diagnosis requires 1+ of following: d. i. Failure to fulfill major obligations e. ii.Hazardous activities during intoxication f. iii.Legal problems iv.Social/interpersonal problems 2. Alcohol Dependence (AD): g. Significant impairment/distress in a 12-month period h. Diagnosis requires 3+ of following: i. i. Tolerance j. ii. Withdrawal k. iii.Larger amounts for longer period than intended l. iv.Persistent desire and unsuccessful attempts to cut down m. v. Excessive time spent drinking alcohol n. vi. Activities given up due to drinking o. vii. Continued use despite problems C. Epidemiology of Alcohol Withdrawal (AW):3,4,5,6 AW symptoms affect up to 70 % of AD patients Slide5 More frequent in the elderly No gender or ethnic differences 85% of patients with AW experience mild-to-moderate symptoms 15% severe symptoms with complicating conditions: a.Seizures, 10% of the cases b.Delirium Tremens, 5% i.In the past, mortality rate was 15-25% ii.Currently 1% III. PATHOPHYSIOLOGY OF ALCOHOLWITHDRAWAL A. Alcohol effects in the brain:7 Slide6 1. Variable effects as a function of duration of administration 2. No single site of action 3. Affects multiple neurotransmitter systems: a. Glutamate and aspartate b. GABA c. Dopamine d. Noradrenaline e. Corticotropin-releasing-factor B. Excitatory neurotransmitter systems and AW:8 Slide7 Glutamate: Main excitatory neurotransmitter ActivateNMDA receptors and voltage-operating channels: Calcium influx neuronal excitability Excessive activation seizures, neurotoxicity and cell death Effects of drinking on excitatory neurotransmission: 8 Alcohol antagonizes NMDA receptors Chronic drinking and tolerance to alcohol are associated with compensatory: NMDA receptors number Calcium (Ca) channels 3.Excitatory neurotransmission during AW: 8 Slide8 a. Rodents show glutamate / aspartate in brain regions related to: i.Reward (e.g. Striatum and Nucleus Accumbens [NAC]) ii. Alcoholcognitive disturbances and AW seizures (e.g. Hippocampus) b. Patients show Glutamate in cerebrospinal fluid (CSF) c. In summary:During AW there is excitatory neurotransmission C. Inhibitoryneurotransmission and AW: 9 Slide9 GABA: a. Maininhibitory neurotransmitter b. Activatesreceptor-operated öCL channels i. Membranehyper-polarization (stability) ii.Neuronal excitability Effects of drinking on GABA: 9 a. Acute alcohol GABAA receptorfunction bChronic drinking GABAA receptor sensitivity tolerance 3. GABA and AW:9 a. During AW GABAAreceptor remains impaired b. Repeated AWfurther impairs GABAA receptor neuronal excitability(e.g. neuronal ãkindlingä) AW seizures and delirium c. In summary,changes in GABA neurotransmission during AW translate: i. Impairment ofneuronal inhibitory mechanisms ii. Anxiety,sympatheticactivity and seizures E. Dopamine (DA):10 Slide10 Mainneurotransmitter mediating reward: a. Released bythe Ventrotegmental area (VTA) into the NAC b. Occurs inanticipation and during rewarding stimuli (i.e., food, sex) Effects of drinking on DA: 10 a. Acute alcohol DA in NAC b. Chronic drinking and tolerance DAin NAC 3. DA and AW: 10 Slide11 i. DAdeficit in NAC ii. Negativemoods (i.e., dysphoria, anhedonia or loss of ability to enjoy previously rewardingactivities) ii. Reassumingdrinking reverses DA deficit iv. Drinkingrelieves negative moods (i.e., negative reinforcing). 4. When AW iscomplicated with delirium and hallucinations: i.DAand homovanilic acid in CSF ii.GABAactivity leads to DA 5. In summary,during AW: i. DA deficit inthe NAC mediates negative mood states ii. However,delirium and hallucinations are associated with DA F. OtherNeurotransmitter Systems: Slide12 1. Norepinephrine and methoxy-4-hydroxyphenilglycol (MHPG):11 a. Plasma concentrations correlate with BP, pulse, tremors and diaphoresis b. 2-adrenoreceptor regulation of norepinephrine release 2. Corticotropin-releasing-factor (CRF): 12, 13 a. Long lasting CRF levels in CSF and amygdale b. CRFR1 receptor sensitivity i. Anxiogenic-likeresponse ii. CRFR1antagonists block this effect iii. Stress sensitivity even after acute AW symptoms subside AWPathophysiology: Key Issues:7 Slide13 Brainhomeostasis reflects a balance between: Excitatory Inhibitory neurotransmission Neuroadaptation: Chronic drinking neuroadaptation to maintain homeostasis Allows brain functioning while disturbed by alcohol During AW neuroadaptive mechanisms are out of balance: Neuronal overexcitation autonomic hyperactivityand seizures Reward deficit negative mood states and urges to drink G. Genetics of Alcohol Withdrawal:Association Studies: Slide14 1. AD patients differ in AWpredisposition even drinking similar amounts14 2. There is a predisposition tocomplications of heavy drinking (e.g., alcoholic liver disease) independentfrom genes predisposing to AD15,16 3. Evidence of genetic factorsconferring predisposition to AW: a.Genetic lines of rodents prone to AW seizures17 b.Human gene variants (e.g., alleles) associated with AW seizures and delirium: i. A9 allele ofDA transporter, DA clearance DA18 ii. Short alleleof 5-HT transporter, 5-HT clearance14 iii. A1 allele ofthe DRD2, DRD2 density depression during AW19 IV. DIAGNOSIS AND EVALUATION A. AW DiagnosticCriteria (DSM-IV):2 Slide15 1. Severity may bevariable: mild to life threatening 2. Begins a fewhours or days (1-2) after cessation or reduction of prolonged drinking 3. Symptoms causesignificant distress or impairment 4. Is not due toanother medical or mental disorder 5. Diagnosis: 2+of: a.Autonomic hyperactivity (e.g., sweating or pulse > 100) b.Hand tremor c. Insomnia d. Nausea orvomiting e. Transientvisual, tactile or auditory hallucinations or illusions f. Agitation g. Anxiety h. Grand malseizures B. OptimalAssessment of AW requires: Slide16 Completehistory, physical, and mental status exam Laboratorytest Standardizedassessments C. History andPhysical: 1. Predictors ofAW severity: a. Older age b. Severityof drinking and high tolerance c. Number of AW episodes and detoxifications d. History ofprevious AW seizures of delirium tremens e. Presence of AW symptoms despite high BAL f. Major medical or surgical problems g. Concomitantsedative/hypnotic use 2. Physical and mental status exam: a.Signs suggestive of chronic alcohol drinking: i.General: Underweight, chronic fatigue Slide17 ii. GI:Dyspepsia, gastritis, hepatitis or liver cirrhosis stigmata (jaundice, bleeding time, ascitis, GI bleeding, spider angiomas, bruises) iii.Immunological: Opportunistic infections iv.Cardiovascular: Hypertension, cardiomyopathy, arrhythmia v. Osteoporosisand pathological fractures vi.Neuropsychiatric: Neuropathy, seizures, delirium, encephalopathy and/ordementia, mood, anxiety and psychotic symptoms b. However,average alcoholic may present with a relatively normal appearance. D. LaboratoryTests:20 Slide18 No AW specific test. Lab testing identifies acute and/or heavy drinking (>5drinks/day). BloodAlcohol Levels (BAL): Doesnot detect heavy drinking but identifies acute intake (~ 12-18 hours) Poorprognosis when AW occurs with intoxicating BAL (0.08-0.10 g/dl) Gamma-glutamyltransferase(GGTP): Alcoholenzymatic induction GGTP Normalizationafter 2-3 weeks of abstinence Sensitivity:40-60%, specificity: 80% if value >35 IU/L CarbohydrateDeficient Transferrin (CDT):21 Heavydrinking induces deglycosylation of transferring Normalizesin 1-2 weeks Sensitivity: 60-80%, specificity:80-90% if value >20 IU/L CDT + GGTP best diagnosticcombination Erythrocytemean corpuscular volume (MCV): Alcohol/acetaldehydeinterfere with nuclear maturation of red blood cells macrocytosis Folicacid or B12 deficiency also macrocytosis(MCV >91.5 3) Upto a third of heavy drinkers Sensitivity:30-40%, specificity: 80% StandardizedEvaluation: The Clinical InstituteWithdrawal Assessment, revised (CIWA-Ar [Appendix 1]). 22 Slide19 1. Validated indetoxification, psychiatric and medical/surgical units 2. Severity scaleranging from 0 to 7, items include: Agitation Anxiety Auditorydisturbances Cloudingof sensorium Headache Nausea/vomiting Paroxysmalsweats Tactiledisturbances Tremor Visual disturbances 3. InitialCIWA-Ar severity and need of medication: Score8-10 (mild), usually some nausea,anxiety and headache no need for pharmacological treatment Score10-15 (moderate) marked autonomic activity Score> 15 (severe) impending deliriumtremens and urgency of pharmacological treatment 4. Subsequentassessments: Every4-8 hours to assess effectiveness of treatment Untilscore < 8-10 for 24 hours F. Natural courseof AW symptoms: Slide20 1. Progressioncan be divided in 4 stages (not everyone has all four): a.Stage 1 (24 ö 48 hours): i. 6-8 hours: anxiety, tremor, nausea andvomiting, heart rate and blood pressure ii. Insomnia,illusion and hallucinations ii. Peak severity occurs after 36 hours iii. 90% of AWseizures occur in this stage iv. Most AW casesare self-limited to this stage b. Stage 2 (48 ö72 hours): Intensified stage 1 symptoms Severe tremors Psychomotor agitation Hallucinations c. Stage 3 (72 ö105 hours): ãDelirium Tremens:ä i.Confusion and disorientation ii.Psychomotor agitation iii.Visual and auditory hallucinations iv. Severe autonomic hyperactivity Admission to an ICU may be warranted d. Stage 4 ( > 7 days): Not typically recognized asa part of the AW natural history. Also known as protracted withdrawal: i. Last 2 ö 4+weeks. Some symptoms last months ii. Anxiety,chronic fatigue, depression, sleep disturbances and headache iii. Symptomscontribute to relapse V. TREATMENT of AW A. Treatment Setting: Ambulatory orInpatient? Slide21 1. Outpatient(O/P) treatment overview:23 a. 80% can betreated b. AW severity: i.CIWA <8 ii.Some cases with CIWA 8 ö15 iii.No hx. of AW seizures or delirium iv.No serious medical/surgical problems v.No serious comorbid psychiatric or drug problems vi.Has social support vii.Supervision and housing available 2. Inpatient (I/P) treatment29 a. 10 -20% ofpatients: Baseline CIWA > 15 CIWA 8 ö15 plus other admission criteria Multiple episodes of AW and detoxifications High AW severity during previous episodes History of AW seizures and/or delirium tremens Major medical or surgical problems Slide22 Major psychiatric and/or drug problems Poor family/social support, homelessness Pregnancy B. Benzodiazepines and AW: 30 Slide23 1.Benzodiazepines: First line oftreatment. Provide the best combination of efficacy, safety and cost 2. Six prospectivetrials involving 5 different agents a.GABAAreceptor function b.Greater efficacy than placebo i.Seizure: ~ 90% ii. Delirium: ~ 70% c.Greater efficacy and safety than other sedative-hypnotics 3. Choice of abenzodiazepine: Slide24 Allbenzodiazepines are effective Longerhalf-life benzodiazepines (e.g., chlordiazepoxide [Librium], diazepam [Valium]) More effective than shorter half life in seizures: ~ 58% Smoother AW Shorterhalf-life agents (e.g., lorazepam [Ativan], oxazepam [Serax]) Less oversedation Indicated in the elderly and liver impairment 4. Fixed scheduletherapy: 30 Slide25 a. A typical benzodiazepine regimen consists:On day 1, one of the following Q 6 h: i.Chlorodiazepoxide, 50 ö 100 mg ii. Diazepam, 10ö 20 mg iii. Lorazepam, 2ö 4 mg iv. When symptomsnot controlled (or CIWA > 8 ö10) provide additional dose v.Dose 20% each day 5. However infixed standardized therapy with benzodiazepines: a.Dose to control AW symptoms vary greatly b. Fixed regimensfrequently do not properly treat AW (i.e., undermedicate or overmedicate) c.Treatment should allow i.Individualization ii.Rapid appropriate dosing 6.Symptom-triggered therapy: 30,31 Slide26 a.Allows objective titration to individual needs: i. CIWA-Ar assessmentand monitoring ii. Medicationadministration triggered by a severity threshold b.Two controlled clinical trials: i.Comparable efficacy to fixed schedule treatment ii.Less medication, less side effects, and shorter treatment ii. No seizures episodes c.One of these agents every hour when CIWA is 8-10: i. Chlorodiazepoxide,50-100 mg ii. Diazepam, 10 ö20 mg iii. Lorazepam, 2-4 mg C. Anticonvulsantsand AW 1. Carbamazepine(CBZ) and Valproate (VPA): 27, 28, 30, 3 2 Slide 27 a. CBZ: 6controlled trials, VPA: 1 controlled trial: i.Both better than placebo in mild to moderate AW ii. CBZ similarthan oxazepam and lorazepam but greater reduction of distress and faster returnto work ii. CBZ also protracted AW symptoms (i.e., insomnia, anxiety, psychological distress) ii. Both, CBZ andVPA prevent AW seizures in animals, limited human data iii.Anti-kindling effect so may future AW severity iv.Do not potentiate alcohol CNS and respiratory depression v.No impairment of psychomotor abilities or cognition vi. No abusepotential vii.Limited data on prevention/treatment of delirium viii. Nohematological or hepatic toxic effects when used for 7 days b.CBZ and VPA limitations i.In general not better than benzodiazepines ii.Side effects and potential toxicity iii.5 ö 10 times greater cost D.Other Agents: 30 Slide28 1. Antipsychotics a. Phenotiazines andbutyrophenones b. Less effective thanbenzodiazepines preventing delirium ii. seizurerisk iii. Mayhelp controlling agitation 2. -Adrenergicantagonist (propanolol [Inderal]) and α-adrenergic agonist (clonidine[Catapres]) a. Autonomic activity b. May hide impending seizures 3. Magnesium a. Levels during AW b. Supplementation does not AWseverity 4. Ethyl Alcohol a.No evidence of efficacy b.Toxic, expensive and risk of tissue damage 3.Nonpharmacological treatment: Slide29 a.Quiet environment to sensory stimulation b. Nutrition andhydration i. Oral thiamine(before glucose administration) and folic acid. Prevents Wernicke-Korsakoffsyndrome ii.Does not prevent seizures or delirium iii. Oral fluidsand electrolytes if necessary (magnesium, calcium and phosphates) c. Orientation toreality d. Supportivebrief interventions: Motivate to change e. Referral to AAand relapse prevention treatment F. Conclusions: 1. AW is a common problem inclinical settings Slide30 2. AW pathophysiology characterizedby: a. Imbalance ofneuroadaptive mechanism b. Excitatoryneuronal activity 3. Clinicians mustactively screen for AD and potential AW 4. If untreated can be deadly 5. Benzodiazepines are the mosteffective and safest treatment References: 1. Moore RD, Bone LR, Geller G, Mamon JA, Stokes EJ, LevineDM. Prevalence, detection, and treatment of alcoholism in hospitalizedpatients. JAMA. 261: 403-407, 1989. 2. APA, QuickReference to the Diagnostic Criteria for DSM-IV-TR., American PsychiatricAssociation: Washington D.C., 2000 3. Schuckit MA, Danko GP, Smith TL, Hesselbrock V, Kramer J,Bucholz K. A 5-year prospective evaluation of DSM-IV alcohol dependence withand without a physiological component. AlcoholClin Exp Res 27: 818-825, 2003. 4. SchuckitMA, Tipp JE, Reich T, Hesselbrock VM, Bucholz KK The histories of withdrawalconvulsions and delirium tremens in 1648 alcohol dependent subjects. Addiction. 90: 1335-1347, 1995 5. Schuckit MA, Anthenelli RM, Bucholz KK, Hesselbrock VM,Tipp J. The time course of development of alcohol-related problems in men andwomen. J Stud Alcohol. 56: 218-225, 1995 6. Saitz R,O'Malley SS Pharmacotherapiesfor alcohol abuse. Withdrawal and treatment. Med Clin North Am. 81: 881-907, 1997 7. De Witte P, Pinto E, Ansseau M, Verbanck P. Alcohol andwithdrawal: from animal research to clinical issues. Neurosci Biobehav Rev 27:189-197, 2003 8. Tsai GC, CoyleGT. The role of glutamatergic neurotransmission in the pathophysiology ofalcoholism. Annu Rev Med 49: 173-184, 1998 9. Dahchour A. DeWitte Ph. Amino acid transmitter systems in substance-related disorders. In:Dâhaenen H, den Boer JA, Westenberg H, Wilner P, editors. Textbook ofbiological psychiatry. New York: Wiley: 2002. p. 415 ö424. 10 Weiss F, Parsons LH, Schulteis G, Hyytia P, Lorang MT,Bloom FE, Koob GF. Ethanol self-administration restores withdrawal-associateddeficiencies in accumbal dopamine and 5-hydroxytryptamine release in dependentrats. J Neurosci 16: 3474-3485, 1996 11. Hawley RJ, Nemeroff CB, Bissette G, Guidotti A, RawlingsR, Linnoila M. Neurochemical correlates of sympathetic activation during severealcohol withdrawal. Alcohol Clin Exp Res. 18: 1312-1316,1994 12. Merlo Pich E, Lorang M, Yeganeh M, Rodriguez de FonsecaF, Raber J, Koob GF, Weiss F. Increase of extracellular corticotropin-releasingfactor-like immunoreactivity levels in the amygdala of awake rats duringrestraint stress and ethanol withdrawal as measured by microdialysis. J Neurosci. 15: 5439-5447, 1995 13. Rassnick S, Heinrichs SC, Britton KT, Koob GF.Microinjection of a corticotropinreleasing factor antagonist into the centralnucleus of the amygdala reverses anxiogeniclike effects of ethanol withdrawal.Brain Res. 605: 25-32, 1993 14. Schmidt LG, Sander T. Genetics of alcohol withdrawal. Eur Psychiatry 15: 135-139, 2000 15, Hrubec Z, OmennGS. Evidence of genetic predisposition to alcoholic cirrhosis and psychosis:twin concordances for alcoholism and its biological end points by zygosityamong male veterans. Alcohol Clin ExpRes. 5: 207-215, 1981 16. Reed T, Page WF, Viken RJ, Christian JC. Geneticpredisposition to organ-specific endpoints of alcoholism. Alcohol Clin Exp Res. 20: 1528-1533, 1996 17. Kosobud A, Crabbe JC.Ethanol withdrawal in mice bred to be genetically prone or resistant toethanol withdrawal seizures. JPharmacol Exp Ther. 238: 170-177, 1986 18. Schmidt LG, Harms H, Kuhn S, Rommelspacher H, Sander T.Modification of alcohol withdrawal by the A9 allele of the dopamine transportergene. Am J Psychiatry. 155: 474478,1998 19. Laine TP, Ahonen A, Rasanen P, Pohjalainen T, TiihonenJ, Hietala J. The A1 allele of the D2 dopamine receptor gene is associated withhigh dopamine transporter density in detoxified alcoholics. Alcohol Alcohol 36: 262-265, 2001 20. ConigraveKM, Davies P, Haber P, Whitfield JB. Traditional markers of excessive alcohol use.Addiction 98 Suppl 2: 31-43, 2003 21. LittenRZ, Allen JP, Fertig JB. Gamma-glutamyltranspeptidaseand carbohydrate deficient transferrin: alternative measures of excessivealcohol consumption. Alcohol Clin Exp Res. 19:1541-1546, 1995 22. Sullivan JT, Sykora K, Schneiderman J, Naranjo CA,Sellers EM. Assessment of alcoholwithdrawal: the revised clinical institute withdrawal assessment for alcoholscale (CIWA-Ar). Br J Addict 84:1353-1357, 1989 23. Prater CD, Miller KE, Zylstra RG. Outpatient detoxificationof the addicted or alcoholic patient. AmFam Physician. 60: 1175-1183, 1999 24. Myrick H, Anton RF. Clinical management of alcoholwithdrawal. CNS Spectrums. 5: 22-26, 2000 25. Ballenger JC, Post RM. Kindling as a model for alcoholwithdrawal syndromes. Br J Psychiatry133: 1-14, 1978 26. Malcolm R, Roberts JS, Wang W, Myrick H, Anton RF. Multiple previous detoxifications areassociated with less responsive treatment and heavier drinking during an indexoutpatient detoxification. Alcohol. 2000 Nov;22(3):159-64 27. Malcolm R, Myrick H, Roberts J, Wang W, Anton RF,Ballenger JC. The effects ofcarbamazepine and lorazepam on single versus multiple previous alcoholwithdrawals in an outpatient randomized trial. J Gen Intern 17: 349-355,2002 28. Malcolm R, Myrick H, Roberts J, Wang W, Anton RF. Thedifferential effects of medication on mood, sleep disturbance, and work abilityin outpatient alcohol detoxification. AmJ Addict 11: 141-150, 2002 29. Whitfield CL, Thompson G, Lamb A, Spencer V, Pfeifer M,Browning-Ferrando M. Detoxification of 1,024 alcoholic patients withoutpsychoactive drugs. JAMA. 239:14091410, 1978 30. Mayo-Smith MF. Pharmacologicalmanagement of alcohol withdrawal. A metaanalysis and evidence-based practiceguideline. American Society of Addiction Medicine Working Group onPharmacological Management of Alcohol Withdrawal. JAMA 278:144-151, 1997 31. Daeppen JB, Gache P, Landry U, Sekera E, Schweizer V,Gloor S, Yersin B. Symptom-triggered vsfixed-schedule doses of benzodiazepine for alcohol withdrawal: a randomizedtreatment trial. Arch Intern Med 162: 1117-1121, 2002 32. Myrick H, Brady KT, Malcolm R.Divalproex in the treatment of alcohol withdrawal. Am J Drug Alcohol Abuse 26: 155-160,2000 Appendix 1. Addiction Research Foundation Clinical InstituteWithdrawal Assessment Appendix 1 CIWA-Ar Patient:__________________________ Date: ________________ Time: _______________.(24 hour clock, midnight = 00:00) Pulse or heart rate, taken for one minute:_________________________ Blood pressure:______ NAUSEA AND VOMITING -- Ask "Do you feel sick to your stomach? Have you vomited?" Observation. 0 no nausea and no vomiting 1 mild nausea with no vomiting 2 3 4 intermittent nausea with dry heaves 5 6 7 constant nausea, frequent dry heaves and vomiting TACTILE DISTURBANCES -- Ask "Have you any itching, pins and needles sensations, any burning, any numbness, or do you feel bugs crawling on or under your skin?" Observation. 0 none 1 very mild itching, pins and needles, burning or numbness 2 mild itching, pins and needles, burning or numbness 3 moderate itching, pins and needles, burning or numbness 4 moderately severe hallucinations 5 severe hallucinations 6 extremely severe hallucinations 7 continuous hallucinations TREMOR -- Arms extended and fingers spread apart. Observation. 0 no tremor 1 not visible, but can be felt fingertip to fingertip 2 3 4 moderate, with patient's arms extended 5 6 7 severe, even with arms not extended AUDITORY DISTURBANCES -- Ask "Are you more aware of sounds around you? Are they harsh? Do they frighten you? Are you hearing anything that is disturbing to you? Are you hearing things you know are not there?" Observation. 0 not present 1 very mild harshness or ability to frighten 2 mild harshness or ability to frighten 3 moderate harshness or ability to frighten 4 moderately severe hallucinations 5 severe hallucinations 6 extremely severe hallucinations 7 continuous hallucinations PAROXYSMAL SWEATS -- Observation. 0 no sweat visible 1 barely perceptible sweating, palms moist 2 3 4 beads of sweat obvious on forehead 5 6 VISUAL DISTURBANCES -- Ask "Does the light appear to be too bright? Is its color different? Does it hurt your eyes? Are you seeing anything that is disturbing to you? Are you seeing things you know are not there?" Observation. 0 not present 1 very mild sensitivity 2 mild sensitivity 3 moderate sensitivity 7 drenching sweats 4 moderately severe hallucinations 5 severe hallucinations 6 extremely severe hallucinations 7 continuous hallucinations ANXIETY -- Ask "Do you feel nervous?" Observation. 0 no anxiety, at ease 1 mild anxious 2 3 4 moderately anxious, or guarded, so anxiety is inferred 5 6 7 equivalent to acute panic states as seen in severe delirium or acute schizophrenic reactions HEADACHE, FULLNESS IN HEAD -- Ask "Does your head feel different? Does it feel like there is a band around your head?" Do not rate for dizziness or lightheadedness. Otherwise, rate severity. 0 not present 1 very mild 2 mild 3 moderate 4 moderately severe 5 severe 6 very severe 7 extremely severe AGITATION -- Observation. 0 normal activity 1 somewhat more than normal activity 2 3 4 moderately fidgety and restless 5 6 7 paces back and forth during most of the interview, or constantly thrashes about ORIENTATION AND CLOUDING OF SENSORIUM -- Ask "What day is this? Where are you? Who am I?" 0 oriented and can do serial additions 1 cannot do serial additions or is uncertain about date 2 disoriented for date by no more than 2 calendar days 3 disoriented for date by more than 2 calendar days 4 disoriented for place/or person Total CIWA-Ar Score ______ Rater's Initials ______ Maximum Possible Score 67