UNIVERSITY OF ILLINOIS COLLEGE OF MEDICINE AT PEORIA
advertisement

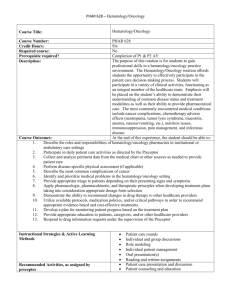
Hem/Onc Rotation Curriculum 2010 UNIVERSITY OF ILLINOIS COLLEGE OF MEDICINE AT PEORIA CHILDREN’S HOSPITAL OF IL/OSF SAINT FRANCIS MEDICAL CENTER PEDIATRIC HEMATOLOGY/ONCOLOGY SUBSPECIALTY ROTATION GENERAL INFORMATION On the first day of rotation, report to St. Jude Clinic at 8 AM. Contact at Hem/Onc is Mohamad Al-Rahawan, Page: 309-679-1000 Doctors Dr. Kay Saving Dr. Stephen D. Smith Dr. Pedro de Alarcón Dr. Mohamad Al-Rahawan Dr. Mary Beth Ross Dr. Karen Fernandez Clinic at St. Jude Midwest Affiliate 624-4945 General Hematology Clinic - Dr. Saving Mondays 9:00-11:00 A.M. Hemoglobinopathy Clinic - Dr. Saving First and third Monday each month 1:00 - 4:00 P.M. Pediatric Oncology Clinic - Drs. Saving, Smith, de Alarcón, Al-Rahawan, Ross and Fernandez 9:00 A.M. - 4:30 P.M. Oncology patients are seen five days a week for chemotherapy and/or other clinical needs. Long Term Follow-up Clinic: Drs. Smith, Al-Rahawan, Ross and Fernandez Wednesdays and Thursdays 9:00 a.m. – NOON General Hematology/Oncology Consults: Drs. Smith, Al-Rahawan, Ross and Fernandez Wednesdays and Thursdays 9:00 a.m. – NOON PATIENT CARE During this rotation, residents must be able to provide care to patients with hematologic and oncologic disorders. This care must be compassionate, medically appropriate, and effective for the treatment of this patient population. The goals of this rotation are to provide the resident with skills that enable him/her to: 1. Manage patients with common hematologic and oncologic problems. 2. Identify when subspecialty assistance for these problems is appropriate. 3. Function as a member of the multi-disciplinary team to optimize patient care. 4. Evaluate and support a patient with a malignancy in all phases of their disease. 1 Hem/Onc Rotation Curriculum 2010 The specific duties for residents are: 1. Manage the in-patient service with supervision: Pre-round with the attending physician at 7:30 on weekdays. Round on all hematology-oncology patients at Children's Hospital of Illinois before noon on weekdays. See all hematology/oncology consultations first and formulate a differential diagnosis and plan prior to discussing the patient with the attending and writing the consultation note. Obviously, some acute consultations may require attending input on a more emergent basis, prior to a complete evaluation by the resident. One weekend (Saturday and Sunday) per rotation. Round on all hematology-oncology patients at Children's Hospital of Illinois by the time agreed on by the attending on call. 2. Attend all outpatient clinics: Examine patients and discuss findings, diagnosis, and management with attending physician. Residents are responsible for a complete note on each patient seen. MEDICAL KNOWLEDGE The goals of this rotation are to expose the resident to a wide variety of hematologic and oncologic diseases through patient contact, case discussions, lectures, and individual readings. The specific topics to be covered during the rotation are: A. Anemia 1. Define "anemia" and outline the diagnostic approach to evaluation in a newborn and an older child with anemia. 2. Outline the appropriate laboratory evaluation, hematologic parameters, treatment, and followup of a child with iron deficiency anemia. 3. Recognize the most common age and presenting features, discuss the differential diagnosis, evaluation, and treatment of patients with hypoproliferative anemia. (Aplastic anemia, DiamondBlackfan anemia, transient erythroblastopenia of childhood.) 4. Recognize the clinical and laboratory features of the various common types of hemolytic anemias (enzyme deficiencies, red cell membrane defects, auto- immune hemolytic anemia). B. Hemoglobinopathies 1. Recognize the expected hematologic parameters of a child with sickle cell disease. 2 Hem/Onc Rotation Curriculum 2010 2. Discuss appropriate lab tests to diagnose and follow children with sickle disease. 3. Discuss the pathophysiology, clinical presentation, and treatment of patients with sickle cell disease who develop: anemic crises (aplastic, hyperhemolytic, splenic sequestration) vaso-occlusive crises (painful, dacytylitis, CNS insult) fever, infection 4. Plan appropriate general health maintenance for patients with sickle cell disease (including genetic counseling/patient & family education). 5. Briefly explain the underlying pathophysiology of the thalassemia syndromes. 6. Describe the clinical and lab features, and basics of management of patients with Alphathalassemia trait, Beta-thalassemia trait and Beta-thalassemia major. C. White Blood Cell Disorders 1. Propose and defend the diagnostic approach to the neutropenic child. 2. Plan an orderly work-up for a child with recurrent infections. 3. List three common causes of eosinophilia in children. D. Coagulation Disorders 1. Outline a differential diagnosis and diagnostic work-up of a child with abnormal bruising and bleeding. 2. State the clinical features, laboratory findings, complications, and treatment of: Factor VIII deficiency Factor IX deficiency von Willebrand disease vitamin K deficiency DIC E. Platelet Disorders 3 Hem/Onc Rotation Curriculum 2010 1. Define thrombocytopenia, and design an approach to evaluation of a thrombocytopenic infant and child. 2. Discuss the pathogenesis, clinical features, and treatment of acute and chronic ITP of childhood. 3. List common platelet function disorders, their clinical features, pathophysiology and the approach to evaluation. F. Oncology 1. List the common neoplasms of childhood, age at which they most commonly occur, and their presenting signs and symptoms. 2. Describe the common symptoms, physical and laboratory findings in acute leukemia (ALL and AML), and the pathophysiology of each. 3. Plan a diagnostic work-up for a child with suspected leukemia. 4. Compare and contrast general treatment objectives and prognosis of the two major types of childhood leukemia (ALL and AML). 5. Outline a diagnostic approach for a child presenting with a suspected malignancy in: soft tissue the chest the abdomen the brain the bone 6. List three important issues to address when approaching a dying child and his/her family. G. Oncologic and Hematologic Emergencies 1. Identify and treat common oncologic emergencies Spinal cord compression. Mediastinal Mass Fever in a neutropenic patient 4 Hem/Onc Rotation Curriculum 2010 Tumor lysis syndrome. 2. Identify and treat common hematologic emergencies Acute severe hemolysis. Intracranial hemorrhage / cerebrovasular accidents. Pulmonary embolism. H. Miscellaneous 1. Outline the diagnostic approach to the patient with hepatomegaly, splenomegaly, and generalized or localized lymphadenopathy. 2. Identify the indications for and complications of transfusion of various blood products. 3. Describe the typical features of post splenectomy infections, the usual infecting organisms, and methods to prevent such infections. 4. Efficiently examine a peripheral blood smear. 5. Describe the clinical importance, interpretation, and indications, for the following lab tests: RBC indices, RDW, reticulocyte count Coombs test (direct and indirect) serum iron, TIBC, ferritin, transferrin saturation, FEP hemoglobin electrophoresis PT, aPTT, mixing studies, BT, platelet aggregation studies 6. List three indications for hematopoietic stem cell transplantation (HSCT), sources of stem cells, and common complications encountered after transplant. PRACTICE BASED LEARNING The goals of this rotation are to allow the resident to 1. Be exposed to a wide variety of hematologic and oncologic diseases through patient contact, case discussions, lectures, and individual readings. 2. Conduct literature searches and be encouraged to write articles on appropriate patient cases or medical topics. 5 Hem/Onc Rotation Curriculum 2010 3. Study independently The following reference sources are available in the medical library and/or St. Jude Midwest Affiliate office for your use during the month's rotation: Manual of Pediatric Hematology & Oncology, Lanzkowsky, 2000 Neonatal Hematology, de Alarcón & Werner, 2005 Hematology of Infancy & Childhood, Nathan & Oski, 2009 Principles and Practice of Pediatric Oncology, Pizzo and Poplack, 2005 4. The resident will be responsible for reading about the hematology/oncology patients' diseases and serving as the "expert" and advisor for the general pediatric service residents/interns. INTERPERSONAL AND COMMUNICATION SKILLS In order to provide excellent care for patients with hematologic and oncologic disorders, residents must demonstrate interpersonal and communication skills that result in the effective exchange of information and collaboration with: 1. All members of the multi-disciplinary team while caring for children with chronic blood disorders or malignant conditions. 2. Supervising and primary care physicians. 3. Consulting physicians and health care professionals 4. Maintain comprehensive, timely and legible records 5. Patients, families and where appropriate the broader family group keeping in mind the cultural and socioeconomic context for this family. Specifically, residents are expected to: Inpatient care: 1. Serve as the subspecialty “expert” and advisor for the general pediatric service residents/interns. 2.Be responsible for an admission note and daily progress notes on all hematology-oncology patients at Children's Hospital of Illinois. 3. Write/dictate a consultation note when a hematology/oncology consultation is requested. 4. Write/dictate a procedure note on all procedures he/she participates in performing. 6 Hem/Onc Rotation Curriculum 2010 Outpatient clinic: 1. Obtain an interval history and perform a physical exam on clinic patients. 2. Discuss his/her finding with an attending physician. 3. Document the clinic visit in the chart (interval history, PE, differential for new diagnoses, and assessment and plan). PROFESSIONALISM While a part of the multi-disciplinary Hematology-Oncology team, a resident is expected to demonstrate professionalism. This means carrying out responsibilities designated to him/her while adhering to ethical principles: 1. Completion of appointed patient care duties. 2. Complete and timely documentation in the medical records. 3. Demonstration of compassion and respect for both team members and patients. 4. Respect patient privacy and autonomy. 5. Demonstrate accountability to both patients and team members. 6. Demonstrate sensitivity to diverse cultural backgrounds. SYSTEMS BASED PRACTICE In order to provide patient care, we all work within a larger system of health care. Residents are an important component of our health care system and as such play a pivotal role in providing quality care. While providing care for children with hematologic and oncologic disorders, residents are expected to: 1. Work effectively in both inpatient (CHOI) and outpatient (St. Jude Midwest Affiliate Clinic) settings. 2. Coordinate patient care between the two settings by interaction with specialty attendings and the inpatient resident team. 3. Advocate for quality patient care 4. Incorporate consideration of cost awareness and risk-benefit analysis while caring for this specialized patient population. 5. Work with the interdisciplinary team to ensure and enhance patient safety. 6. Participate in identifying system errors and developing solutions for these errors. 7