disaster-preparedness-plan-manual
advertisement

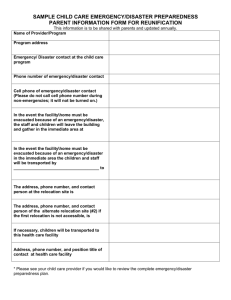
Disaster Preparedness Plan Policy Name: Disaster Preparedness Plan Approved Date: Section: Disaster / Safety Review Date: Policy #: Purpose: Revised Date: To establish protocol POLICY The Governing Body is responsible for the establishment and maintenance of an effective disaster preparedness plan. The Clinical Director will act as the disaster and safety officer within the facility. This disaster preparedness plan is established to provide an effective response to disasters or emergencies impacting the environment of care for the care of patients, staff and other individuals who are in the facility when a major interruption event occurs. The disaster preparedness plans are reviewed or updated annually or as necessitated by changes in staff assignments, occupancy, or the physical arrangement of the building. Fire safety and evacuation plans shall be available in the workplace for reference and reviewed by staff during staff in-service training. Copies will be furnished to the fire code official for review upon request. Reference NFPA LSC 101 Sections 20/21.7.1.1 and NFPS 99 Chapter 11. The disaster preparedness plan will: Designate and authorize key person(s) to be responsible for plan implementation. Define and, as appropriate, integrate the facility’s role into community-wide emergency preparedness efforts. Include mitigation, preparedness, response and recovery in emergency management planning activities. Identify specific response procedures to a variety of disasters, based on hazard vulnerability analysis. Establish procedures to notify personnel and external authorities of emergencies when emergency response measures are implemented. Assign staff primary and secondary roles and responsibilities to cover all needed positions during an emergency. Effectively manage patient, staff and family activities, critical supplies, security, and interaction with the public. Establish evacuation procedures, or establish an alternate care site, when the facility environment cannot support adequate patient care and treatment. Provide an alternate source of essential utilities and internal and external communication systems in the event of failure during a disaster or emergency. Include emergency management procedures and responsibilities in staff orientation and in-service programs. EMERGENCY RESPONSE This Governing Body will designate key individual(s) to authorize and assume responsibility for the implementation of facility emergency disaster plans. The facility will notify civil authorities of the facility scope of care and available resources. The facility is not staffed or equipped to offer emergency services, which limits our participation in community wide disaster programs. The facility emergency management plans aim to mitigate or minimize danger and the impact of staff, patients and visitors as well as prepare for, respond to and provide for recovery during a potential disaster or emergency. In the event of an emergency or disaster, actual or impending, which may affect the provision of services, (e.g., hurricane, flood, earthquake), patients and staff will be informed and scheduled procedures will be cancelled. Plans will include triage, emergency treatment (within the scope of the facility capabilities) and transfer of victims to the nearest emergency treatment center to address an emergency which causes damage or injury in or near the facility. By basing the planning of emergency management on realistic conceptual events, the plan reflects those issues or events that are predictable for the environment the organization operates in. Thus, such conceptual planning will focus on issues, such as severe weather typical in this locale, situations that can occur due to close proximity of industrial or transportation complexes; or earthquake possibilities due to local seismic activity. Planning for these events will focus on the capacity of the center to provide services during such an emergency. There is no way to plan for all possible emergencies, but by focusing on local conceptual events and operating capacity thresholds, the center has developed realistic plans as well as guidelines for staff to operate within those plans. RESPONSILITY FOR DISASTER MANAGEMENT: (Authority to Activate and Terminate the Emergency Management Plan) The decision to activate the disaster management plan will be made by the authority designated within this plan, in accordance with the activation criteria. The decision to terminate shall be made by the designated authority in coordination with the declaring governmental agency. Designated Authority Title Name Clinical Director The Clinical Director will delegate staff responsibilities including but not limited to: Assigning staff to cover all necessary positions, security (access, traffic control, and crowd control), identification and monitoring of all personnel and others (patients, visitors) in the facility. Interaction with the media, screening incoming telephone calls, shut down of equipment and utilities, as appropriate, patient activities including scheduling, modification or discontinuation of services, control of patient information and patient transportation, if needed, triage of incoming patients and recovering patients, staff/family support activities, logistics of critical supplies (medications, disposables, food, linen and water). NOTIFICATION, LOGISTICS AND MITIGATION The Clinical Director will initiate notification and logistic support for the facility. Emergency response staff and alternates will be identified and assigned specific responsibilities. The facility maintains surveillance of impending threats by monitoring television or radio. In the event that an imminent threat or emergency situation is identified, operations at the facility will cease and staff, patients and visitors will be notified. For emergencies occurring during operational hours, a plan will be activated, as necessary, for ceasing routine operations, triage, emergency treatment, transfer of victims to the nearest emergency treatment center, and evacuation of the facility. The current employee roster with telephone and pager numbers, when applicable will be available for employees at home as well as in the facility. Scheduling information will be available for assigned personnel to complete patient notification in a timely manner. When an alarm is activated or a code is announced, emergency response staff will respond immediately with appropriate equipment and supplies while awaiting the arrival of civil authority. If immediate evacuation is required, staff members will initiate evacuation while awaiting arrival of civil authority. The facility will maintain agreements with an area hospital and local ambulance service to facilitate patient transfer. EMERGENCY POWER AND SUPPLIES Emergency backup power will be available on a limited basis as required by code and generator size. The facility does not provide emergency services or overnight care; therefore planning and provisions are only for short periods of confining or sequestering emergencies. It is not feasible for the facility to stockpile supplies to support emergency situations not within the facility scope of services due to the limited storage space. The facility maintains only the supplies, food and water required for scheduled procedures. EMERGENCY EVACUATION The Clinical Director will determine the level of evacuation required for emergency management. Upon arrival at the facility, the civil authorities will assume responsibility for evacuation decisions. In the event of uncontained danger (e.g., smoke, fire, bomb, or other disaster), complete facility evacuation will be conducted by the Clinical Director or the civil authority present at the scene. Evacuees will assemble in a designated area furthest from the building. EMERGENCY TRANSFER Patients or victims that may require a higher level of care will be transferred to a hospital with which the facility maintains a transfer agreement or to the nearest emergency treatment center. If the condition warrants, facility staff may accompany patients. RE-ENTRY After an evacuation or a disaster that caused structural damage, the facility will be inspected by the civil authorities, the Clinical Director, and the maintenance coordinator to determine that conditions are safe for re-entry and resumption of operations. In the event of significant structural damage, approval also may be required from the local or state construction offices. The Clinical Director or civil authority in charge is responsible for authorizing re-entry into the facility and the resumption of operations. EDUCATION AND TRAINING Orientation and in-service programs will be conducted to train all employees on their roles and responsibilities, and to review the emergency disaster plan. Disaster drills will include all employees, medical staff, and other occupants of the building. If utilization requires more than one shift of operation, drills will be held on each shift. Documented disaster (other than fire) drills will be held at least annually. Documentation of disaster drills includes, but is not limited to types of emergencies, staff responsibilities in responding to an emergency, effectiveness of staff response, adequacy of equipment and the alarm system, the needs identified, and the plan for staff training to correct deficiencies. CMS 416.41(c) Disaster Preparedness Plan Standard Interpretive Guideline How We Met Standard Disaster Preparedness Plan The intent of this regulation is for an ASC to have in place a disaster preparedness plan to care for patients, staff and other individuals who are on the ASC‟s premises when a major disruptive event occurs. The governing body of the ASC is responsible for the development of this plan See Disaster Preparedness Plan). Hazard Identification Comprehensive emergency management includes the following phases, which should be taken into account in the development of the ASC’s disaster preparedness plan: Hazard Vulnerability (HVA) was assessed. ASCs should make every effort to include any potential hazards that could affect the facility directly and indirectly for the particular area in which it is located. List identified potential hazards for your facility Indirect hazards could affect the community but not the ASC, and as a result interrupt necessary utilities, supplies, or staffing. Hazard Mitigation Hazard mitigation consists of those activities taken to eliminate or reduce the probability of the event, or reduce the event’s severity or consequences, either prior to or following a disaster or emergency. Mitigation details should address provision of needed care for the ASC’s patients being prepared for procedures, undergoing procedures, or recovering from procedures, as well as how the ASC will educate staff in protecting themselves and others present in the ASC in the event of an emergency. Comprehensive hazard mitigation efforts, including staff education, will aid in reducing staffs' vulnerability to potential hazards. These activities precede any imminent or postimpact timeframe, and are considered part of the response. The emergency plan should include mitigation processes for patients, staff and others present in the facility at the time of the disaster or emergency. Preparedness Preparedness includes developing a plan to address how the ASC will meet the needs of patients, staff, and others present in the ASC if essential services break down as a result of a disaster. It will be the product of a review of the basic facility information, the hazard analysis, and an analysis of the ASC‟s ability to continue providing care and services during an emergency. It also includes training staff on their role in the emergency plan, testing the plan, and revising the plan as needed. List P&P’s for fire, bomb etc. Standard Interpretive Guideline Response Activities taken immediately before (for an impending threat), during and after a disaster/emergency event to address the immediate and short-term effects of the emergency. Recovery Activities and programs that are implemented during and after the ASC‟s response that are designed to return the ASC to its usual state or a "new normal. Coordination of the Plan The regulation requires that the ASC must coordinate its disaster preparedness plan with State and local authorities that have responsibility for emergency management within the State. Coordination should take place in addressing threats that either extend beyond the premises of the ASC, e.g., floods, earthquakes, or biochemical releases, etc., or threats within the ASC that require response from a community agency, e.g., fire department. How We Met Standard List coordination/participation with local/state agencies. The regulation does not require that ASCs be integrated into State and local emergency preparedness plans to address threats that extend beyond the premises of the ASC, since it will ultimately be the decision of the State and local officials whether and how they might utilize ASCs in a response to an emergency event. ASCs must, however, document that they have made efforts to communicate with their State and local emergency preparedness officials to inquire about potential coordination. Testing, Evaluating, and Updating the Plan At least once every year the ASC must conduct a drill to test the plan’s effectiveness. A drill that is conducted in concert with State or local authorities would qualify as an annual test. While the drill does not have to test the response to every identified hazard, it is expected to test a significant portion of the plan. For example, a fire drill does not qualify on its own as a sufficient annual drill of the ASC’s plan. Disaster drills are conducted annually. The ASC must prepare a written evaluation of each annual drill, identifying problems that arose as well as methods to address those problems. The disaster preparedness plan must be promptly updated to reflect the lessons learned from the drill and the needed changes identified in the evaluation. List date and type of drill Fire safety drills are conducted quarterly. Documentation of each drill is maintained. An evaluation is done after all drills to identify improvement potential. Disruption in Service Tool Utility Mfg. Book on file Contact Information What to do in case of malfunction Life Support Utilities Medical Gases □ Yes □ No □ NA Electricity □ Yes □ No □ NA The generator will kick in. Continue with patient care. Generator/Emergency Power System □ Yes □ No □ NA If the generator does not work, cases will be cancelled until the system is functional. Autoclave □ Yes □ No □ NA Negative Air in each operating room □ Yes □ No □ NA HVAC □ Yes □ No □ NA Filters will be changed at least quarterly and more often if needed Plumbing □ Yes □ No □ NA Shut off water main Water □ Yes □ No □ NA Shut off water main Fire Alarm System □ Yes □ No □ NA Fire sprinkler System □ Yes □ No □ NA Fire Exit Illumination □ Yes □ No □ NA Telephone System □ Yes □ No □ NA Paging systems Intercoms □ Yes □ No □ NA Nurse call system □ Yes □ No □ NA Code Blue Buttons □ Yes □ No □ NA Infection Control Systems Environmental Systems Communication System WATER Notify the Clinical Director of the surgery center. Only the current case in progress will proceed, all other cases will be cancelled until water is restored. Notify Water Company. Telephone Number: Restrict use of water. If possibility of contamination exists, turn off main water valve. Deliver adequate drinking water to each designated area. Consider the possibility of recovering and storing the water toilet tanks, water heaters and boilers. Inform personnel to be prepared to line toilets with plastic bags for removal of human waste. Plastic bags should then be considered infectious waste. Water shut off valve is located at: ________________________________ ____________ GAS Notify the Clinical Director of the surgery center. Notify Gas Company. Telephone number: _____________________________ If gas leak is evident, notify Fire Department. Evacuate all persons and open doors and windows to ventilate. Shut off local valve or main valve at meter. Do not use matches, candles, or other open flame devices; activate light switches, or other electrical appliances. Gas shut-off is located at: _____________________________________________ To turn off gas: _________________________________________________ ELECTRICITY Notify the Clinical Director of the surgery center. Only current cases will continue, all other will be cancel Notify electric company for repair services. Telephone number: ______________ Main power panel is located: ____________________________. To turn off electrical power you: _______________________________. For long duration of electrical power outage access: o o o Medication & Food sensitive items Test & Reprogram equipment Monitor emergency generator load COMMUNICATION Notify the phone company via cell phone (a cell phone will be available at the center) In case of emergency the cell phone is used to activate emergency services. MEDICAL GAS Shut off local valve or main valve on cylinder Medical gas valve located at: ______________________________________________ To turn off: ______________________________________________________________ If the current case is done under local, the case will be continued and portable oxygen will be used. Only local cases will be performed without medical gases Contact Medical Gas Company. Telephone number: ______________________________ If leak noted, provide ventilation to area, consider evacuation. HOT WATER SYSTEM Cases will continue without the hot water system. Notify the contracted maintenance service for repair The surgery center is not on a sewer system. Refer to the water shut-off protocol. Emergency Triage Telephone Call List Name Title Phone # Person for you to contact Name Clinical Director / Safety Manager Registered Nurse Registered Nurse Registered Nurse OR Tech Phone #