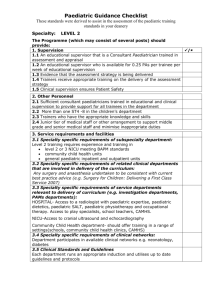
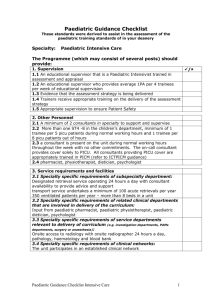
Standards for Speciality Training in Paediatrics

Paediatric Guidance Checklist
These standards were derived to assist in the assessment of the paediatric training standards in your deanery
Specialty: Level 3 General Paediatrics
The Programme (which may consist of several posts) should provide:
1. Supervision
1.1 An educational supervisor that is a Consultant Paediatrician trained in assessment and appraisal
1.2 An educational supervisor who is available for 0.25 PAs per trainee per week of educational supervision
1.3 Evidence that the assessment strategy is being delivered
1.4 Trainers receive appropriate training on the delivery of the assessment strategy
1.5 Clinical supervision ensures Patient Safety
2. Other Personnel
2.1 Sufficient consultant paediatricians trained in educational and clinical supervision to provide support for all trainees in the department
2.2 More than one ST4 -8 in the children’s department
2.3 Junior tier of medical staff or other arrangement to support middle grade and senior medical staff and minimise inappropriate duties
3. Service requirements and facilities
3.1 Specialty specific requirements of subspecialty department:
A comprehensive 24 hour, 7 day a week inpatient unit and outpatient department
3.2 Specialty specific requirements of related clinical departments that are involved in delivery of the curriculum:
Any surgery and anaesthesia undertaken to be consistent with current best practice advice (e.g. Surgery for Children: Delivering a First Class
Service 2007)
3.3 Specialty specific requirements of service departments relevant to delivery of curriculum (e.g. investigation departments,
PAMs departments, surgery or anaesthesia):
HOSPITAL- Access to a radiologist with paediatric expertise, paediatric dietetics, paediatric SALT, paediatric physiotherapy and occupational therapy. Access to play specialists, school teachers, CAMHS.
NICU-Access to cranial ultrasound and echocardiography
Community Child Health department- should offer training in a range of settings(schools, community child health clinics, CAMHS)
3.4 Specialty specific requirements of clinical networks:
Trainee attendance at Outreach Clinics with visiting sub-specialists
Department participates in available clinical networks e.g. neonatology, diabetes
3.5 Clinical Standards and Guidelines
Each department runs an appropriate induction and utilises up to date guidelines and protocols
/
Paediatric Guidance Checklist
These standards were derived to assist in the assessment of the paediatric training standards in your deanery
4. Educational activities and training
4.1 Specialty specific clinical exposure required to provide sufficient learning opportunities ( NB if giving workload data ensure it is explicit whether this is number per annum or number trainee would be expected to be exposed to over entire programme):
Level 3 programme consisting of a series of posts which allow adequate opportunity to cover the range of level 3 competences
Appropriate clinical activity
Assessment of 400 acute new presentations per trainee per year of training
During 6 months neonatal intensive care training opportunity to be present at 30 deliveries requiring attendance and to admit 20 infants to
NICU/SCBU
Maintenance of acute skills e.g. lead resuscitation at least 4 times a year, assess safeguarding cases at least 4 times a year
4.2 Specialty specific requirements for structured training opportunities to include courses:
Opportunities to attend Child protection training to enhance and consolidate competences as per Level 3 curriculum (e.g. Court Skills training)
Leadership and Management training appropriate to the Level 3 curriculum
Opportunities to revalidate resuscitation training if needed
4.3 Specialty specific requirements for other experiential
learning(excluding clinics and ward rounds):
Opportunities to develop leadership skills in multidisciplinary teamwork
Opportunities to lead and manage at the interface between hospital paediatrics and community child health
5. Working patterns
5.1 Safe cover arrangements for paediatric department out of hours in line with RCPCH guidance
5.2 Evidence of compliance with existing employment rules to working time
5.3 Working intensity and pattern that is appropriate for learning
5.4 Emphasis on providing opportunities for advanced paediatric clinical training as per the level 3 curriculum, including care of chronic conditions, leadership and management. There should be less need to participate in high activity, low complexity work.
5.5 This post forms part of a complete paediatric training programme which provides a minimum of 5 years of acute clinical experience, including out of hours duties
5.6 Working patterns which allow trainees to regularly attend at least
60% of regional training days
5.7 inappropriate attendance to the Delivery Suite
Clear local guidance should be in place to indicate which deliveries
Paediatric staff should attend, minimising presence where there is no proven need. Guidance should be reviewed on a yearly basis.
Paediatric Guidance Checklist
These standards were derived to assist in the assessment of the paediatric training standards in your deanery
6. Specific Post requirements
6.1 See specific module if developing special expertise
7. Enabled to learn new skills, necessary skills and curriculum coverage (specialty specific)
This section can be used to highlight marker conditions to which trainee should be exposed or the numbers of cases/procedures that trainee will be expected to see/do. Ensure that it is clear whether any numbers are for whole training programme or per annum
7.1 Specialty specific marker conditions trainee should be exposed to:
Community
Problems; looked after children, developmental delay, neurodisability, chronic disease, child abuse and neglect, faltering growth, speech delay, hearing and vision impairment, behavioural problems, enuresis, soiling, special educational needs, immunisation advice
Diagnoses; cerebral palsy, ADHD, ASD, Leaning difficulty, obesity, DCD,
NICU-
Prematurity, growth retardation, jaundice, necrotising enterocolitis, respiratory distress, hypoxic ischaemic encephalopathy, fits, narcotic abstinence syndrome
General Paediatrics-
Problems; Fever, fits, breathing difficulty, diarrhoea, vomiting, developmental delay, rashes, hypoxia, chronic disease, child abuse and neglect, prematurity, jaundice, faltering growth, behavioural problems, common post natal problems, post natal screening, resuscitation and stabilisation of a sick child, recognising and diagnosing uncommon conditions, leading on diagnostic dilemmas
Diagnoses; diabetes, epilepsy, asthma, cerebral palsy, respiratory distress syndrome, congenital heart disease, nephrotic syndrome, arthritis, anaemia, head injury, ingestion, infectious diseases, gastroenteritis, childhood cancer, cystic fibrosis
7.2 Specialty specific skills/procedures trainee needs to complete:
Writing child protection reports and statements with a view to court appearance
8. Access to clinics and ward rounds and long term care of patients
8.1 Specialty specific numbers and types of clinics expected to attend (including outreach clinics:
26 consultant supervised new patient clinics per year (seeing about 3 new patients per week), follow up clinics 26 per year
8.2 Specialty specific combined clinics expected to attend:
As needed to develop special interest
8.3 Specialty specific ward rounds consultant led and independent per week:
On average 2 ward rounds, 1 consultant led and 1 independent per week
8.4 Specialty specific involvement in transitional care:
As needed to develop special interest
Paediatric Guidance Checklist
These standards were derived to assist in the assessment of the paediatric training standards in your deanery
9. Meetings
9.1 Specialty specific number and types of MDT meetings
expected to be exposed to:
1 MDT meeting per month (e.g. Discharge planning, complex care, safeguarding)
10. Clinical Governance
10.1 Opportunities for trainees to take a leading role in aspects of clinical governance (risk management, supervising complete audit cycles, active management of critical incidents)
10.2 Opportunities for trainees to lead in aspects of clinical guideline development within departments
11. Teaching appraising and assessing
11.1 Opportunities to deliver formal and informal teaching (e.g. to medical students or peers) and receive feedback
11.2 Opportunities for involvement in assessment of others (e.g. giving feedback)
11.3 Opportunity to be involved in the appraisal of others (e.g. 360 degree Appraisal)
12. Research
12.1 Provide opportunity to acquire level 3 competences in research
12.2 Provide opportunities to be involved in clinical research
13. Management
13.1 Opportunities for active participation in management processes and meetings within departments and hospitals (e.g. departmental consultant meetings, departmental managerial meetings, Divisional Management
Boards, Clinical Director Forums, Patient Advice Liaison Service meetings)