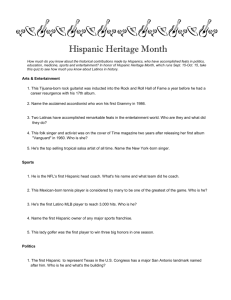
University - National Hispanic Medical Association
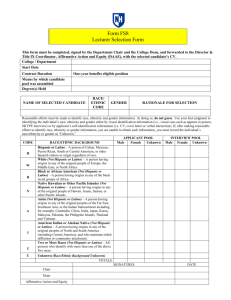
advertisement

13th Annual Conference Building a Healthcare Workforce for the Hispanic Community Brooklyn Bridge Marriott Brooklyn, NY March 19-22, 2009 CONFERENCE RESOURCE CD Table of Contents Speaker Abstracts FRIDAY Pfizer Inc. Breakfast Symposium: “Patient Prescription Assistance” Plenary Session 1: “National Vision for A Healthcare Workforce for the Hispanic Community” Plenary Session 2: “National Leadership Perspective” Plenary Session 3: “Lunch: Hispanics & Depression and Co-Morbidities” Plenary Session 4: “Federal Policy & Workforce Development” Workshop Sessions A Workshop Sessions B SATURDAY Breakfast Symposium: “Hispanics and Heart Disease” Plenary Session 5: “The Connection Between Addiction & Obesity” Plenary Session 6: “The Private Sector Perspective on Improving Workforce Diversity” Plenary Session 7: “Lunch: Challenges & Opportunities for Hispanic Health” Workshop Sessions C Workshop Sessions D SUNDAY Breakfast Symposium: “NHMA Federal Title VII” 2009 Hispanic Health Research Poster Sessions Additional Readings NHMA in the News National Hispanic Medical Association 1411 K Street, NW, Suite 1100 Washington, DC 20005 Phone: 202-628-5895 / Fax: 202-628-5898 / www.nhmamd.org Target Audience and Course Description Join Hispanic physicians, nurses, medical students, policymakers, and healthcare industry representatives at our annual conference. This year, NHMA celebrates its 13th Conference with partners from the Federal and State governments and the private sector. The CME conference brings together experts from across the nation to share their experience in eliminating health disparities for Hispanics and is accredited for CME* Hispanics have become the largest ethnic group in the United States and there is a great need to understand how to deliver culturally relevant health care services to them. Learn from experts on how to enhance academic programs, community-based research, medical practices, and health policies targeting Hispanics. Conference Educational Objectives Adopt new treatment modalities and strategies to educate Hispanic patients with diabetes, cancer, HIV/AIDS, obesity, cardiovascular disease, asthma, Alzheimer’s disease, depression and renal disease in order to decrease morbidity and mortality in their medical practices or in their organization. Analyze cultural competence, literacy, and language services programs Explain how current Federal health policy addressing eliminating disparities in health & programs affect the health status of the Hispanic community. Continuing Education Statements CME: The New York Academy of Medicine is Accredited by the Accreditation Council for continuing medical education to sponsor continuing medical education for physicians. The University of Texas Health Science Center at San Antonio School of Medicine designates this educational activity for a maximum of 17 AMA PRA Category 1 Credits. Physicians should only claim credit commensurate with the extent of their participation in the activity. STATEMENT OF DISCLOSURE: Faculty for the National Hispanic Medical Association programs are expected to disclose at the beginning of their educational presentation any relevant financial relationships with the commercial company. DISCLAIMER: The National Hispanic Medical Association (NHMA) its consultants and staff are not responsible for injury or illness resulting from the use of medications or modalities discussed during this educational activity. The NHMA does not endorse the use of "off-label" medications. BREAKFAST SYMPOSIUM “Patient Prescription Assistance” -sponsored by Pfizer, Inc. Moderator: Gary Pelletier Marketing & Communications, Pfizer Helpful Answers, NY Gary Pelletier, Director of Pfizer Helpful Answers. According to Gary, “Pfizer Helpful Answers is dedicated to helping people without prescription coverage to get the medicines they need”. He is excited that the initiative allows Pfizer to reach out to the community at a level where increasing rates of the uninsured, especially the Hispanics are enormous. Pfizer Helpful Answers plays an important role in delivering quality healthcare in communities through its Share the Care Program, a part of Pfizer’s Helpful Answers. Pfizer supports over 4oo community centers of patient assistance programs and continues these efforts considering the increasing rates of the uninsured, especially among Hispanics.” Its “Promotores Initiative” enables Pfizer Helpful Answers to reach out to the community at a level where our prescription assistance program is most needed,” added Gary. Pfizer Helpful Answers is excited and proud to continue these efforts considering increasing rates of the uninsured Amy Niles, Medical Relations Chair, Together Rx Access, Wilmington, DE Amy Niles serves as the Medical Relations Chairperson of Together Rx Access. The Together Rx Access Card was created by 10 pharmaceutical companies. It helps eligible Americans and their families gain access to meaningful savings on prescriptions right at the pharmacy counter.Most cardholders save 25 percent to 40 percent* on brand-name prescription products, including medicines to treat high cholesterol, diabetes, asthma, and many other conditions. Over 300 brandname prescription products are included in the program. Savings also are available on a range of generic products. The Card is accepted at the majority of pharmacies nationwide and in Puerto Rico.*Each cardholder's savings depend on factors such as the particular drug, amount, and pharmacy where it was purchased. Participating companies independently determine the level of savings offered and the products included in the program. Those decisions are subject to change. .Eighty-eight Pfizer medicines are available through Together Rx Access. Including non-Pfizer medicines, this program covers more than 300 brand name prescription medicines. Visit www.TogetherRxAccess.com for the most current list of brand-name medicines and products. Larry Lucas, Vice President, PhRMA, Partnership for Prescription Assistance, Washington, DC Larry Lucas serves as Vice President, Government Affairs/Diversity Programs for the Pharmaceutical Research and Manufacturers of America (PhRMA) where he works with the U.S. Congress and state legislators on issues impacting patient’s access to medicines, access to quality health care and the research-based pharmaceutical industry. At PhRMA, Lucas leads the association’s efforts to work with patients, healthcare providers, physicians, legislators and health organizations and educate them on the issues impacting the minority community and their access to quality health care. Lucas also writes a nationally syndicated monthly column about new developments in the pharmaceutical industry. At PhRMA, he has previously served as Deputy Vice President in the alliance development division where his responsibilities included coalition building and grassroots development, and state government affairs division working with African-American and Latino state legislators through out the country. Lucas brings to PhRMA extensive experience in federal and state legislative affairs, the private sector, and community affairs. Prior to joining PhRMA, Lucas held various public affairs roles at organizations such as Michigan Consolidated Gas Companies, Primark Corporation’s Hospital Satellite Network, and Gulf Oil Corporation in Houston, Texas. At Gulf, he served as a spokesperson for the company, traveling throughout the U.S. representing the company’s public affairs efforts with key leaders and government officials. Lucas spent 16 years at the Bureau of Census where he initiated a landmark outreach campaign for the 1980 census program that involved 86,000-plus government jurisdictions. This program was replicated in the subsequent 1990 and 2000 censuses. At the Bureau of Census, Lucas’ responsibilities varied from serving as liaison to the White House and the U.S. Congress, to coordinating with national leaders and government officials at all levels to promote effectiveness of the Census Bureau’s goals. Lucas is on the Board of Trustees for the National Association for the Advancement of Colored People (NAACP), and also is actively involved in their contribution fund and health committee. Lucas serves as the Corporate Advisory Council to the National Hispanic Medical Foundation; on the Congressional Black Caucus Institute and was recently appointed to the Africa Diaspora North Initiative Strategic Planning Committee Board, as well as The Joint Center for Political and Economic Studies Corporate Council. He served as Vice Chairman for the National Black Caucus of State Legislators’ Corporate Roundtable. Lucas also served on the boards of directors for the Congressional Black Caucus Political Education and Leadership Institute, Providence Health Foundation Providence Hospital, Yale University’s School of Nursing External Advisory Board, and is a founding member of the National Hispanic Caucus of State Legislators’ Business Board of Advisors. Previously, Lucas served as special assistant to the president of the Joint Center for Political and Economic Studies, on the Congressional Black Caucus Foundation, Inc.’s Board of Directors. Lucas received his B.S. degree in Education form Jackson State University in Mississippi and served in the United States Air Force. PLENARY SESSION 1 “National Vision for a Healthcare Workforce for the Hispanic Community” Ciro Sumaya, M.D., M.P.H.T.M., Chairman of the Board of Directors, HMA, Dean, School of Rural Public Health, Texas A&M Health Science Center College Station, TX Dr. Ciro V. Sumaya is the Chair of the Board of Directors of the National Hispanic Medical Association. A native of Brownsville, Texas, is dean of the School of Rural Public Health and holder of the Cox Endowed Chair in Medicine at Texas A&M University Health Science Center in College Station. He was a Presidential appointee for four years at the U.S. Department of Health and Human Services. He first served as administrator of Health Resources and Services Administration, a federal focal point for innovation in health care delivery and health professions education, and subsequently served as Deputy Assistant Secretary for Health, spearheading the federal initiative on the Future of Academic Health Centers. Before federal service, Dr. Sumaya was associate medical dean at the University of Texas Health Science Center at San Antonio, where he established the South Texas Health Research Center, Area Health Education Center of South Texas and a Medical Treatment Effectiveness Research Center. He has also held academic positions at the UCLA School of Medicine. Dr. Sumaya has published more than 110 professional journal articles and book chapters on pediatric viral infections, emerging as a leading physician-scientist in childhood infectious mononucleosis. His recent publications target national health policy issues. He was one of the six Founding Scholars in Academic Administration and Health Policy of the Association of Academic Health Centers and Executive Committee Member of the Surgeon General's National Hispanic Health Initiative. In 1993 he was selected as a group leader of the Health Care Workforce workgroup of the Presidential Task Force on Health Care Reform. He received a Bachelor of Arts degree with high honors from The University of Texas at Austin, where he was also selected to Phi Beta Kappa. His Doctor of Medicine degree was obtained from the University of Texas Medical Branch in Galveston, where he was selected or the Alpha Omega Alpha Honor Medical Society. Following a pediatric residency at St. Christopher's Hospital for Children in Philadelphia, Pennsylvania, Dr. Sumaya completed a postgraduate fellowship in pediatric infectious diseases at Tulane University School of Medicine. He earned a Master in Public Health and Tropical Medicine degree from Tulane University School of Public Health. His honors and awards include the Ashbel Smith Distinguished Alumnus Award from the University of Texas Medical Branch at Galveston; Distinguished Fellow of the Public Health Policy Advisory Board in Washington D.C.; Juan Carlos Finlay Award from the U.S. Public Health Service; and distinguished professor appointment at the Uniformed Services University of Health Sciences in Bethesda, Maryland. Richard F. Daines, M.D. New York State Health Commissioner Richard F. Daines, M.D., was confirmed as the 14th Commissioner of Health for New York State in March of 2007. As Commissioner, Dr. Daines heads one of the nation’s leading public health agencies with a budget of approximately $49 billion. Under his leadership, the Department of Health administers the state’s public health insurance programs, regulates hospitals and other health care facilities, conducts research in a premier biomedical laboratory, and supports public health prevention initiatives. During the past year he helped shape significant health care reforms that were adopted in the state budget, including increased access to health insurance coverage for the uninsured, greater emphasis on primary and preventive care, quality improvement initiatives, and investment in health information technology. Dr. Daines led the implementation of health care facility restructuring measures mandated by the State Legislature in connection with the Commission on Health Care Facilities in the 21st Century. He is currently leading an effort to reform health care through more effective local health care planning. Prior to becoming Commissioner, Dr. Daines was the President and CEO of St. Luke’s-Roosevelt Hospital Center from January 1, 2002 until January 2007. Previous to joining the Hospital Center as Medical Director in 2000, Dr. Daines served as Senior Vice President for Professional Affairs and Medical Director at St. Barnabas Hospital in the Bronx. Dr. Daines received a Bachelor of History degree from Utah State University in 1974 and served as a missionary for the Church of Jesus Christ of Latter-day Saints in Bolivia from 1970 to 1972. He received his medical degree from Cornell University Medical College in 1978. He served a residency in internal medicine at New York Hospital and is Board Certified in Internal Medicine. Ruben Font, Coordinator, National Network of Latin American Medical Students Elena Rios, MD, MSPH, President & CEO, National Hispanic Medical Association, Washington, DC Dr. Rios serves as President & CEO of the National Hispanic Medical Association, (NHMA), representing Hispanic physicians in the United States. The mission of the organization is to improve the health of Hispanics. Dr. Rios also serves as President of NHMA’s National Hispanic Health Foundation affiliated with the Robert F. Wagner Graduate School of Public Service, New York University, to direct educational and research activities. Dr. Rios also serves on the National Hispanic Leadership Agenda, Campaign Against Obesity, and the Partnerships for Prevention Boards of Directors, the American Medical Association Commission to End Health Disparities, the PacifiCare-UnitedHealthcare California Investment Committee and is Chair, the National Coalition on Hispanic Health. Dr. Rios has lectured and published articles and has received several leadership awards, including awards from the U.S. Department of Health and Human Services, the Congressional Black, Hispanic, Asian and Native American Caucuses, American Public Health Association Latino Caucus, Association of Hispanic Health Executives, Minority Health Month, Inc., Hispanic Magazine, Verizon’s First Pollin Community Service Award, and Amerimed. Dr. Rios was appointed to the Minority Alumni Hall of Fame of Stanford University in October, 2006. She was awarded the 2008 Latino Mental Health Advocacy and Policy Award in New York in October 2008. Prior to her current positions, Dr. Rios served as the Advisor for Regional and Minority Women’s Health for the U.S. Department of Health and Human Services Office on Women’s Health from November 1994 to October 1998. In 1993, Dr. Rios was appointed to the National Health Care Reform Task Force as Coordinator of Outreach Groups for the White House. In 1992, Dr. Rios worked for the State of California Office of Statewide Health Planning and Development as a policy researcher. Dr. Rios has also served as President, Chicano/Latino Medical Association of California, Advisor to the National Network of Latin American Medical Students, member of the California Department of Health Services Cultural Competency Task Force, Stanford Alumni Association and Women’s Policy Inc. Boards of Directors, and the AMA’s Minority Affairs Consortium Steering Committee. Dr. Rios earned her BA in Human Biology/Public Administration at Stanford University in 1977, MSPH at the University of California School of Public Health in 1980, her MD at the UCLA School of Medicine in 1987, completed her Internal Medicine residency at the Santa Clara Valley Medical Center in San Jose and the White Memorial Medical Center in East Los Angeles in 1990, and her NRSA Primary Care Research Fellowship at UCLA Division of General Internal Medicine in 1992. PLENARY SESSION 2 “National Leadership Perspective” Moderator: Jo Ivey Boufford, MD, President New York Academy of Medicine Jo Ivey Boufford, MD, is President of The New York Academy of Medicine. Dr. Boufford is Professor of Public Service, Health Policy and Management at the Robert F. Wagner Graduate School of Public Service and Clinical Professor of Pediatrics at New York University School of Medicine. She served as Dean of the Robert F. Wagner Graduate School of Public Service at New York University from June 1997 to November 2002. Prior to that, she served as Principal Deputy Assistant Secretary for Health in the U.S. Department of Health and Human Services (HHS) from November 1993 to January 1997, and as Acting Assistant Secretary from January 1997 to May 1997. While at HHS, she served as the U.S. representative on the Executive Board of the World Health Organization (WHO) from 1994–1997. From May 1991 to September 1993, Dr. Boufford served as Director of the King’s Fund College, London England. The King’s Fund is a royal charity dedicated to the support of health and social services in London and the United Kingdom. She served as President of the New York City Health and Hospitals Corporation (HHC), the largest municipal system in the United States, from December 1985 until October 1989. Dr. Boufford was awarded a Robert Wood Johnson Health Policy Fellowship at the Institute of Medicine in Washington, DC for 1979–1980. She served as a member of the National Council on Graduate Medical Education and the National Advisory Council for the Agency for Healthcare Research and Quality from 1997–2002. She is currently Chair of the Board of Directors for the Center for Health Care Strategies and serves on the boards of the United Hospital Fund, the Primary Care Development Corporation, the Village Center for Care, and MHRA. She was President of the National Association of Schools of Public Affairs and Administration in 2002–2003. She was elected to membership in the Institute of Medicine (IOM) in 1992 and is a member of its Executive Council, Board on Global Health and Board on African Science Academy Development. She was elected to serve four a four year term as the Foreign Secretary of the IOM beginning July 1, 2006. She received an Honorary Doctorate of Science degree from the State University of New York, Brooklyn, in May 1992. She was elected a Fellow of the National Academy of Public Administration in 2005. She has been a Fellow of The New York Academy of Medicine since 1988 and a Trustee since 2004. Dr. Boufford attended Wellesley College for two years and received her BA (Psychology) magna cum laude from the University of Michigan, and her MD, with distinction, from the University of Michigan Medical School. She is Board Certified in pediatrics. Dora L. Hughes, MD, MPH, FAACP, Counselor for Public Health & Science, Office of the Secretary, Department of Health and Human Services, Washington, DC Dr. Dora Hughes serves as the Counselor for Public Health and Science, helping to develop and lead Administration initiatives focusing on a broad range of health issues including health reform, public health, health workforce, drug, device and food regulation, and biomedical research. She previously served in the United States Senate, in the capacity of Deputy Director for Health for Senator Edward M. Kennedy on the Committee on Health, Education, Labor and Pensions, and Health Policy Advisor to Senator Barack Obama. Prior to working on Capitol Hill, Dr. Hughes served as Senior Program Officer at Commonwealth Fund, a national health foundation in New York City. She completed medical school at Vanderbilt University, residency at Brigham & Women’s Hospital and public health school at Harvard University. Dr. Hughes is board-certified in internal medicine. Abstract: The United States Department of Health and Human Services (HHS), is a Cabinet department of the United States government with the goal of protecting the health of all Americans and providing essential human services. Its motto is "Improving the health, safety, and well-being of America". Maria Soto Greene, MD, MPH President Hispanic-Service Health Professions Schools, Inc., Washington, DC Dr. Maria Soto-Greene is Professor and Vice Dean at New Jersey Medical School. She has amassed 22 years of experience in all aspects of medical education. Major teaching assignments throughout her years focused on 1st - 4th year students and ranged from courses in physical diagnosis education to precepting on general floors. She also played an active role in the education and supervision of senior students in the intensive and emergency medicine departments. Furthermore, in her capacity as faculty sponsor, she was instrumental in the development, implementation and clinical supervision of the critical care fellowship. She is committed to advancing the school’s cultural competency education. It is through her efforts that NJMS has core objectives and competencies related to cultural and linguistic competence education for all four years of medical education. This set the stage for the current roll out of the Physician’s Core Cultural Competency Module of which she played a key role. These initiatives place NJMS at the forefront of undergraduate medical education. In addition to her extensive educational portfolio, she has, over the years, been given increasingly more administrative roles. As former Senior Associate Dean for Education, she was responsible for the planning and coordination of the medical school accreditation process by the LCME which took place March 2005. Three major areas noted as strengths are attributed to work undertaken in her roles. These were the diversity of the student body, community service, and the inclusiveness of the curriculum renewal process. Beyond the educational setting, she has also had impacted the care of critically ill patients and has expertise in working with families, patients and house staff on issues related to end of life care. As Director of the Hispanic Center of Excellence for over 14 years, Dr. Soto Greene has gained a national reputation for promoting and implementing diversity and cultural competence. She has lectured, consulted and led workshops in these areas. At the federal level, she was selected to join a panel of experts which included highly regarded individuals with extensive expertise in cultural competence. She co-edited and co-authored a document on cultural and linguistic competence education for health professions. Furthermore, she has served as a consultant to others on how to achieve diversity at the medical student level. The current student diversity NJMS enjoys is a testament to her efforts at successfully competing for and administering educational grants such as the Robert Wood Johnson Foundation Summer Medical Education Program. To this end, Dr. Soto Greene, has also been instrumental in designing and implementing ways to develop young faculty. Through her grants, faculty has received the necessary release time to dedicate to academic pursuits. She has also shared lessons learned at forums such as the AAMC Minority Faculty Development Conference. Diana Bontá, RN, DrPH Vice President Kaiser Permanente Southern California, Pasadena, CA Diana Bontá joined Kaiser Permanente Southern California in 2004 and is responsible for overseeing public affairs programs, public policy, and managing the reputation of a region that has more than 3 million members. As a seasoned community health leader, Bontá directs Kaiser Permanente’s strategic approach to public health via a Community Benefit division that last year devoted $369 million to improve the health of underserved populations in Southern California. Under her direction, Community Benefit has launched significant initiatives to improve health care access, clinical quality, and technology in the region’s community clinics and programs. She also champions the Healthy Eating Active Living initiative – a nationwide Kaiser Permanente program to combat the obesity epidemic – and plays an important role in Kaiser Permanente’s efforts to reform health care in California and across the nation. Bontá continues to lend her talents and experience to public health issues such as anti-smoking, teen pregnancy prevention, prenatal care and nutrition, disease-prevention, and programs that expand access to health care for uninsured children. Before joining Kaiser Permanente, Bontá was director of the California Department of Health Services where she collaborated with Mexico to reduce incidence of disease on both sides of the border. She also helped develop the nation’s first hospital nurse-to-patient staffing ratio regulations and the state’s preparedness for potential bioterrorism. Prior to that, she was the director of Health and Human Services for the City of Long Beach. Currently, Bontá is a member of two dozen governance or advisory boards, including the U.S. Department of Health and Human Services’ Advisory Committee on Minority Health – a committee appointed by the Secretary of Health and Human Services – and the Council on Education in Public Health. She also is a member of the Board of Directors for Loyola Marymount University’s Center for the Study of Los Angeles, the Health Professions Education Foundation’s Board of Trustees, the Pat Brown Institute of Public Affairs, and the City of Los Angeles Board of Fire Commissioners. Academic achievements for Bontá include doctorate and master’s degrees in public health from the University of California, Los Angeles – where she is an adjunct associate professor – and a bachelor’s degree in nursing from the University of New York, Buffalo. Bontá’s contributions have been recognized with numerous awards. She has received the American Public Health Association’s Presidential Citation Award and was named to Hispanic Magazine’s list of 100 leading Latinas. Steven Dawson President, PHI Bronx, NY Steven Dawson is president of PHI — www.PHInational.org — a national nonprofit that promotes quality care through quality jobs within the long-term care system. He has helped lead PHI since its inception in 1992. Headquartered in the South Bronx, PHI’s 40 staff members work nationally and in 15 states to improve the lives of people who need home and residential care—by improving the lives of the workers who provide that care. Steven has co-authored several national publications on health care employment issues, including Direct-Care Health Workers: The Unnecessary Crisis in Long-Term Care, and Sectoral Strategies for Low-Income Workers. Along with Nancy Lundebjerg of the American Geriatric Society, Steven is co-convener of the national Eldercare Workforce Alliance — www.eldercareworkforce.org. PHI’s technical and policy services currently assist more than 50 long-term care agencies, state programs and key stakeholders across the country. Within New York City, PHI is the sponsor of Pathways to Independence, an entrepreneurial system of for-profit and nonprofit agencies that includes the 1500-employee Cooperative Home Care Associates, which is the largest worker cooperative in the U.S. and trains more than 500 women each year to become home health aides; and Independence Care System, a $90 million managed long-term care program for adults living with disabilities in their homes. Nationally, PHI staffs the National Clearinghouse on the Direct Care Workforce— www.directcareclearinghouse.org — the nation’s primary, on-line library for direct-care issues, which along with PHI’s organizational website receives more than 40,000 web visits each month. Abstract: Steven Dawson will introduce the new Eldercare Workforce Alliance (EWA), a group of 25 national organizations, joined together to address the immediate and future workforce crisis in caring for an aging America. The mission of the Alliance is to build a caring and competent eldercare workforce—joining in partnership with older adults, their families and other unpaid caregivers—to provide high-quality care, and improve the quality of life for, older adults and their families. The Institute of Medicine, in its historic report “Re-tooling for an Aging America: Building the Health Care Workforce,” called for immediate investments in preparing our health care system to care for older Americans. In response, we formed the national Eldercare Workforce Alliance—representing consumers, family caregivers, the direct-care workforce, and healthcare professionals—to propose practical solutions to strengthen our eldercare workforce and thereby improve the quality of care. Steven will also describe the work of his own organization, PHI, based in the South Bronx, which drives a quality care through quality jobs mission across the United States, focused specifically on the direct-care workforce. He will speak to the history of PHI’s affiliate, Cooperative Home Care Associates, which is a worker cooperative owned by its 1500 inner-city home health aides—more than 70 percent of whom are Latina. Steven will describe the growing importance of our nation’s 3,000,000 direct-care staff—home health aides, nurse aides and personal care workers—within the emerging debates in health care reform and economic recovery. PLENARY SESSION 3 “Hispanics and Depression and Co-Morbidites” Moderator: Katherine A. Flores, MD, Program Director UCSF-Fresno Latino Center for Medical Education and Research, Fresno, CA Born to migrant farm workers in the Central Valley and raised by her grandparents, Katherine Flores attended Stanford University, where she chose to pursue a medical career. Through her work as a practicing physician, medical educator, and mentor for high school and college students bound for health careers, Flores has dedicated herself to improving the quality of care in underserved communities and increasing the number of Latinos and other underrepresented minorities in the health professions. Flores established and managed the Sunnyside High School Doctor's and Junior Doctor's Academy and the University of California Latino Center for Medical Education and Research (LaCMER). For these and other programs, Flores recruited faculty and staff from diverse backgrounds. Flores also practices as a family physician in an all-woman, bilingual medical group in Fresno that serves families from widely varying economic and ethnic backgrounds. Flores serves as a faculty member of the University of California, San Francisco-Fresno Medical Education Program and as project director for the California Health Education Training Center and for LaCMER. Flores speaks frequently at events across the country, and says that she is continually reenergized by the needs of the Latino community and the dreams of students Pedro Ruiz, MD, Professor and Interim Chair Department of Psychiatry and Behavioral Sciences University of Texas Medical School at Houston Dr. Pedro Ruiz is currently a Tenured Professor and Interim Chair and Vice Chair in the Department of Psychiatry and Behavioral Sciences of the University of Texas Medical School at Houston. Born in Cuba, Dr. Ruiz conducted his pre-medical school studies at the University of Havana in Cuba and completed him medical school education at the University of Paris in France. Subsequently, he finished his graduate training in Psychiatry at the University of Miami Medical School in Florida. During his academic career, Dr. Ruiz was also Professor and Vice Chair in the Department of Psychiatry and Behavioral Sciences as well as Assistant Dean at the Albert Einstein College of Medicine in New York City and Professor and Vice Chair of the Department of Psychiatry and Behavioral Sciences at Baylor College of Medicine in Houston. He was also President of the American College of Psychiatrists, The American Board of Psychiatry and Neurology, and the American Association of Social Psychiatry. Currently, he is also currently President Elect of the American Psychiatric Association and Secretary for Meetings of the World Psychiatric Association. Dr. Ruiz has received numerous honors and awards; among them, the “Simon Bolivar Award”, the “George Tarjan Award”, the Administrative Psychiatry Award”, the Irma J. Bland Award, and a “Presidential Commendation” from the American Psychiatric Association. Also, the “Bowis Award” from the American College of Psychiatrists and the “Exemplary Psychiatrist Award” from the National Alliance for the Mentally Ill (NAMI). Dr. Ruiz has published over 400 original articles, invited articles, books, book chapters, abstracts and book reviews during his academic career. Among them, the well established textbook “Substance Abuse: A Comprehensive Textbook”. Additionally, he has served in numerous Editorial Boards, including the American Journal of Psychiatry, Psychiatric Services, World Psychiatry, and Addictive Disorders and Their Treatment where he is currently Editor-in-Chief. His areas of research interest are administrative psychiatry, psychiatric education, cross-cultural psychiatry and health services research. Clinical and Research Interests: Mood Disorders Anxiety Disorders Health Services Research Psychiatric Education Cross-Cultural Psychiatry Publications (selected): Johnson BA, Ruiz P, Galanter M (eds.): Handbook of Clinical Alcoholism Treatment (book). Baltimore, Maryland, Lippincott Williams &Wilkins, 2003. Ruiz P: Addressing Culture, Race and Ethnicity in Psychiatric Practice. Psychiatric Annals, 34(7): 527-532, 2004. Lowinson JH, Ruiz P, Millman RB, Langrod JG (eds.): Substance Abuse: A Comprehensive Textbook, Fourth Edition (book). Baltimore, Maryland, Lippincott Williams & Wilkins, 2005. Matorin AA, Guynn RW, Sexson S, Kapoor V, Ruiz P: Current and Future Psychotherapy Trends in U.S. Graduate Psychiatric Training. Revista di Psichiatria, 40(1): 26-30, 2005. Ruiz P, Bland IJ, Pi EH, de Zulueta F: Cross-Cultural Psychotherapy. In G.O. Gabbard, J. Beck, J. Holmes (eds.): Oxford Textbook of Psychotherapy. Oxford, United Kingdom, Oxford University Press, 2005, pp. 431-439. Ruiz P: APA’s Efforts to Eliminate Disparities. Psychiatric Services, 56(12): 1603-1605, 2005. Javier I. Escobar, M.D., M.Sc., Professor & Chairman, Department of Psychiatry, UMDNJ-Robert Wood Johnson Medical School, Piscataway, NJ Javier I. Escobar (M.D., M.Sc.,) is Professor and Chairman, Department of Psychiatry, University of Medicine and Dentistry of New Jersey (UMDNJ)-Robert Wood Johnson Medical School, Piscataway, New Jersey, USA. Dr. Escobar recently served as Senior Advisor to the Director of the National Institute of Mental Health (NIMH) in Bethesda, Maryland (2004) and was a member of NIMH’s National Advisory Mental Health Council. He has been an advisor to the World Health Organization (WHO) in Geneva, a member of the Food and Drug Administration’s (FDA) Advisory Committee on Psychiatric Drugs, and a standing member in several National Institute of Health (NIMH, NIDA, NIA) and Veterans Administration’s research review committees and other national task forces. Dr. Escobar has been an active researcher in the areas of clinical psychopharmacology, psychiatric epidemiology, psychiatric diagnosis and cross-cultural medicine and psychiatry. Currently he is the Principal Investigator of several projects funded by the National Institute of Mental Health in the areas of mental disorders in primary care (P20), treatment of somatoform disorders (R01), epidemiology of mental disorders and development and mentoring of new psychiatric researchers (R-13). He has published a total of 200 scientific articles in national and international books and journals. Phone: (732) 235-4440 Fax: (732) 235-5158 Email: escobaja@umdnj.edu Javier I. Escobar, M.D., M.Sc. is Professor and Chairman, Department of Psychiatry, at UMDNJRobert Wood Johnson Medical School. A native of Colombia, South America, Dr. Escobar came to the United States in 1969. He trained in Psychiatry and received a Masters degree in Psychiatry/Medical Genetics from the University of Minnesota in 1973. Between 1973-1985 Dr. Escobar went from Assistant, to Associate and then full Professor of Psychiatry during his tenure at the Universities of Minnesota, Tennessee and California (UCLA). At the University of Connecticut School of Medicine, in Farmington, he served first as Vice Chairman of the Department of Psychiatry, and in 1992 he became Interim Chair of the Department, a position he held until 1994. In 1994, Dr. Escobar became Professor and Chairman of the Department of Psychiatry at the UMDNJ-Robert Wood Johnson Medical School in New Jersey. Dr. Escobar is recognized as a national leader in academic psychiatry and has been an active teacher and researcher. His research background has focused primarily in the areas of clinical psychopharmacology, psychiatric epidemiology, psychiatric diagnosis and cross-cultural medicine and psychiatry. He has been PI or co-PI of several projects funded by the National Institute of Mental Health in the areas of Treatment of Somatoform Disorders, Epidemiology of Mental Disorders and Development and Mentoring of New Psychiatric Researchers. His most recent work focuses on the somatic presentations of psychiatric disorders in primary care. Currently he is PI and director of the “Medically Unexplained Physical Symptoms Research Center” at Robert Wood Johnson Medical School funded by the National Institute of Mental Health (2005-2010). Dr. Escobar also leads a mentoring program for stimulating young investigators to become researchers in the area of Hispanic Mental Health that is also funded with a grant from NIMH. Dr. Escobar has been a member of the National Advisory Mental Health Council at NIMH and worked at NIMH as Senior Advisor to the Director. At NIMH, he also led the council work group that prepared the NIMH report to address mental health disparities in the United States. He has published over 200 scientific articles in national and international books and journals. He received the Simon Bolivar Award for his work on behalf of Hispanic populations in 1998. David C. Henderson, MD, Associate Professor of Psychiatry, Harvard Medical School, Boston, MA David C. Henderson, MD, is Associate Professor of Psychiatry at Harvard Medical School and Director of the Schizophrenia Diabetes and Weight Reduction Research Program at Massachusetts General Hospital, both in Boston, Massachusetts. He also serves as Medical Director for the Harvard Program in Refugee Trauma at Harvard Medical School, Director of the Clozapine Program at the Erich Lindemann Mental Health Center, and Associate Director of the Schizophrenia Program at Massachusetts General Hospital. He is the former Coordinator of Psychopharmacology at the Massachusetts Institute of Technology. Dr. Henderson received his undergraduate degree at Tufts University in Massachusetts, and his medical degree at the University of Massachusetts Medical School. Following his internship at St. Elizabeth’s Hospital in Boston, he completed his residency at Massachusetts General Hospital and trained as Chief Resident and Research Fellow of the Freedom Trail Clinic at the Erich=2 0Lindemann Mental Health Center, also in Boston. Dr. Henderson’s main research interests focus on psychopharmacological and antipsychotic agents in the treatment of schizophrenia, impacts of antipsychotic agents on metabolic anomalies and glucose metabolism, and ethnic and cultural impacts on psychiatry. He also studies the impact of trauma in areas of mass violence and develops programs to assist vulnerable populations, including projects in Rwanda, Cambodia, East Timor, Bosnia, New York City, and Louisiana. PLENARY SESSION 4 “Federal Policy and Workforce Development” Garth Graham, MD, MPH, Deputy Assistant Secretary for Minority Health, U.S. Department of Health and Human Services, Rockville, Maryland Garth N. Graham, M.D., M.P.H., is the Director of the Office of Minority Health at the Department of Health and Human Services. The Office of Minority Health was created by the U.S. Department of Health and Human Services (HHS) in 1985 as a result of the Report of the Secretary’s Task Force on Black and Minority Health. The office operates under the provisions of the Health Professions Education Partnerships Act of 1998. The mission of the Office of Minority Health is to improve the health of racial and ethnic populations through the development of effective health policies and programs that help to eliminate health disparities. These populations include Blacks/African Americans, American Indians and Alaska Natives, Asian Americans, Native Hawaiians and Other Pacific Islanders and Hispanics/Latinos. As Director, Dr. Graham reports to the Assistant Secretary for Health and works closely with all agencies throughout the Department. The Office of Minority Health develops and coordinates Federal health policy that addresses minority health concerns and ensures that Federal, State and local health programs take into account the needs of disadvantage, racial and ethnic populations. Dr. Graham serves as the Executive Director of the HHS Council on Health Disparities. The Council made up of senior leadership across the department serves to coordinate and track progress on disparities related projects undertaken by the department. He was previously appointed a White House Fellow and special assistant to Secretary Tommy G. Thompson at the Department of Health and Human Services, the White House Fellows program is America’s most prestigious program for leadership and public service. Dr. Graham has significant experience working in minority communities, he founded the Boston Men’s Cardiovascular Health Project, a project designed to find behavioral explanations for decreased adherence to adequate diet and exercise by African American men. Dr. Graham was Founding Senior Editorial Board Member of the Yale Journal of Health, Law, Policy, and Ethics, and served on the Editorial Board of the Yale Journal of Biology and Science and as a reviewer for the Journal of Health Services Research. He has served on the Public Health Executive Council of the Massachusetts Medical Society, Board of Directors of Physicians for Human Rights, Chairman of the American Medical Association/MSS National Minority Issues Committee and on the Steering Committee of the Boston Men’s Health Coalition. Dr. Graham has taught on the Faculty of the Observed Structured Clinical Exam at Harvard Medical School and has authored scientific articles and presentations on cardiovascular disease, HIV/AIDS and community medicine and medical education. Dr. Graham earned an M.D. from the Yale School of Medicine, where he graduated cum laude was inducted into the Alpha Omega Alpha medical honor society and named a Yale President Public Service Fellow. He also earned an MPH from the Yale School of Epidemiology and Public Health with a focus in health policy administration and did his residency in Internal Medicine at Massachusetts General Hospital and was also a Clinical Fellow at Harvard Medical School. His award includes the 2002 American Medical Association Leadership Award, the Partners in Excellence Award and the Miriam Kathleen Dasey Award from Yale Medical School. Abstract: WORKSHOPS SESSION A A.1: Policy: Medicare and Medicaid Update Moderator: Mark Diaz, Alivio Medical Group, Sacramento, CA Dr. Mark A. Diaz is a graduate of Christian Brothers High School in Sacramento California. He received his Bachelor of Science Degree in Biological Sciences in 1974 at the University of California in Davis. He is a graduate of the University of California San Francisco Medical School class of 1979 and the Family Practice Residency at the University of California Davis. He completed a Song-Brown Family Practice Fellowship at UC Davis. He has taught Family Medicine for 24 years at the University of California Davis. He is Board Certified in Family Practice and Board Certified in Occupational Medicine. Currently he is the Medical Director of the Alivio Medical Group in Sacramento, California. He teaches parttime for the University Davis Department of Family and Community Medicine where he is an Associate Clinical Professor. He is a founding member of CHE, a Latino pre-med organization at UC Davis, Clinica Tepati, a free clinic in Sacramento, and the National Hispanic Medical Association. He currently serves on the Board of Directors of the National Hispanic Medical Association and on the Board of Directors of the National Hispanic Health Foundation. Nilsa Gutierrez, M.D., M.P.H., Chief Medical Officer, U.S.D.H.H.S. Region II, CMS New York Dr. Gutierrez serves as Medical Director for the Centers for Medicare and Medicaid Services’ Region II Office. Her central role is to provide medical and clinical advice to all program areas including Medicare, Medicaid and the State Child Health Insurance Program. She overseas medical and clinical activities including matters related to access to health care and quality of care provided to all beneficiaries, with a focus on health disparities. As Medical Director, quality monitoring includes program quality data analysis and direct involvement in complaint investigation activities in long term care, ESRD and renal transplant services, intermediate care facilities for the mentally retarded and EMTALA, in addition to advising staff on resolution of disputed matters. She serves as Region II liaison to medical societies and health professional organizations and in provider education and training activities. Just before her arrival at CMS, Dr. Gutierrez served as a consultant in Primary Care Delivery Systems. As an Internist and expert on HIV disease, she provided medical care in a mobile medical unit to people with HIV disease, residents in drug treatment settings and the homeless in neighborhoods throughout New York City. Dr. Gutierrez served as Medical Director and Director of the New York State AIDS Institute, responsible for statewide coordination and funding of HIV prevention, care, and treatment as well as the development of clinical guidelines and educational training, policy development, and strategic planning for HIV/AIDS service development in New York State. The Director advised New York State’s Governor, Commissioner of Health, and Legislature. She also served on the Presidential Advisory Council on AIDS between 1997 and 1999. She is a graduate of the State University of New York at Stony Brook Medical School, received her residency training at Harlem Hospital, Department of Internal Medicine and a Master of Public Health from Columbia University. ABSTRACT: Medicare Payment Reform: Value Based Purchasing and the Physician Quality Reporting Initiative Medicare’s various fee-for-service fee schedules and prospective payment systems are based on resource consumption and quantity of care, NOT quality. Transforming Medicare from a passive payer to an active purchaser of high quality, efficient health care is a goal of value based purchasing (VBP). Pay for reporting, pay for performance, and competitive bidding are all value based purchasing tools. This presentation will focus on factors influencing the support for VBP and laws passed over the past five years that authorize the establishment of Medicare pay-for-reporting and pay-for-performance programs. The presentation will cover the Physician Quality Reporting Initiative (PQRI), the first pay-for-reporting program for clinical provider groups, including physicians. Sue Kelly Associate Regional Administrator Division of Medicaid and Children’s Health Region II- New York Centers for Medicare & Medicaid Services Sue Kelly is Associate Regional Administrator for the Division of Medicaid and Children’s Health (DMCH) in the Centers for Medicare & Medicaid Services (CMS)-Region II. In this capacity, she oversees and monitors the program administration and financial management of State Medicaid Programs and the Children’s Health Insurance Programs (CHIP) in the states of New York, New Jersey, the Commonwealth of Puerto Rico, and the U.S. Virgin Islands. Ms. Kelly previously directed the Division of Medicaid and State Operations, which included responsibility for oversight of State survey and certification programs as well as Medicaid and S-CHIP policy functions in Region II. Ms. Kelly served in various capacities in New York State government over a twenty year period including appointments as Administrator, NYS Kidney Disease Institute, Assistant Director of the Health Care Survey and Certification Group, Executive Deputy Director, Office of Public Health, and New York State Medicaid Director. Prior to joining CMS in March l998, Ms. Kelly worked in the private sector as Plan Administrator for Adirondack Medicine, Inc., an independent practice association (IPA) of over 350 primary care practitioners and referral specialists providing medical services in the Saratoga- Lake George, N.Y. region, and as Regional Director, North Care Partners Health Plans, a commercial health plan formed in 1996 and operated in upstate New York. This health plan was also approved as a Medicaid managed care plan and Medicare risk contractor. Ms. Kelly has a Master of Science degree in Health Systems Management from Union College and a Master’s degree in Bioethics from Union Graduate College and Albany Medical College. A.2: Health Professions Education: Hispanics and Medical Professions: Tools to Increase, Improve and Facilitate a More Diverse Medical Workforce Moderator: Hector Castro, M.D., Medical Director, Beth Israel Latino Health Institute, New York Dr. Hector Castro is an expert in the fields of Internal Medicine, Pulmonary Disease and Critical Care Medicine. He is the Medical Director and a Founding Partner of Itzamna Medical Center in Manhattan, a modern facility dedicated to serving the health care needs of Latinos and all New Yorkers. When it opened in 2001, Itzamna was among the first private organizations to specifically address the many health challenges faced by Hispanics. The success of Itzamna led Dr. Castro to collaborate with the leadership of Beth Israel Medical Center in Manhattan to create and launch the Beth Israel Latino Health Institute in 2006. In 1966, Hector Castro emigrated with his family from Honduras to New York. He grew up in Hell’s Kitchen in Manhattan, attended public schools, and earned a Bachelor’s Degree in biology from Pace University in New York City. A graduate of Univerisidad Autonoma De Guadalajara School of Medicine, Dr. Castro has more than a decade of experience in private practice. He completed his Internal Medicine residency and Pulmonary and Critical Care Medicine Fellowship training at Cabrini Medical Center, an accrediting affiliate of New York Medical College. He went on to complete a Fellowship in Critical Care Medicine at the Mount Sinai Medical Center in New York, NY. In addition to his leadership roles at the Beth Israel Latino Health Institute and Itzamna Medical Center, Dr. Castro is an Attending Physician at Beth Israel Medical Center and Mount Sinai Medical Center. He also serves as the Medical Director of Student Health Services at the Julliard School in New York City. Dr. Castro is a Clinical Instructor of Medicine at The Mount Sinai School of Medicine in New York City, and an Assistant Professor of Internal Medicine and Assistant Professor of Family Medicine at New York Medical College in Valhalla, New York. Dr. Castro is a member of the Society of Critical Care Medicine, American College of Chest Physicians, American Medical Association and the New York Academy of Science. He was the first recipient of the Dr. Charles P. Fulton Pulmonary Fellowship Award in 1992. This award is given by the American Lung Association’s New York Chapter to help train minority physicians in Pulmonary Medicine. Jose Ramon Fernandez-Pena, M.D., M.P.A., Associate Professor, San Francisco State University, California José Ramón Fernández-Peña, MD, MPA, is an associate professor of Health Education at San Francisco State University and the director of the Welcome Back Initiative, a project developed to assist internationally trained health professionals in the process of re-entering the health workforce in the US. Previously, he was director of Health Education at Mission Neighborhood Health Center in San Francisco, where he oversaw the health education activities of the Center. Before coming to California, Dr. Fernández-Peña worked with the New York City Health and Hospitals Corporation in the areas of Quality Management, Medical Affairs, and Planning. His areas of expertise include the development and implementation of programs to diversify the health workforce and to improve cross cultural communication in health. Dr. Fernández-Peña holds an MD from the National Autonomous University of Mexico, and a Master’s in Public Administration from New York University. ABSTRACT: The Welcome Back Program: A New Approach to Improving Diversity in the Health Workforce It has been well documented that the lack of minority health professionals is compounding the Nation's racial and ethnic health disparities. To address this issue it is imperative to infuse the public health and health care workforce with a cadre of workers who speak the languages and understand the cultures of the populations being served. The Welcome Back Initiative has developed a successful model that assists immigrant health professionals to re-enter the health workforce. The model of service builds on community assets to achieve a higher degree of social capital among immigrant populations. While the project was built jointly by City College of San Francisco and San Francisco State University, it has been the program's ability to establish partnerships in the realms of academia, employment, government, and the non-profit sector that have proven critical to its ability to make in-roads in policy change that addresses health disparities. At the same time, these partnerships have provided a means to highlight this talented population of professionals living in our communities who hitherto have remained an unnoticed, unidentified and hidden population. The model is currently in operation at three sites in California, in Boston, MA and in Providence, RI. Results: More than 7,500 participants from 130 countries have been identified, 60% of them are from Latin America. Over 1000 individuals have returned to the health workforce. Jeff S. Oxendine, M.B.A, M.P.H., Associate Dean, School of Public Health Center for Public Health Practice, University of California at Berkeley Jeffrey Oxendine is Associate Dean for Public Health Practice at the UC Berkeley School of Public Health. He is also a faculty member in Health Policy and Management at the School of Public Health and the Haas School of Business. Jeff has been a health executive, educator and consultant for 25 years. He has devoted much of his efforts during that time to increasing workforce diversity. ABSTRACT: Connecting the Dots (CTD) is a statewide initiative to provide the evidence, tools, and guidance for the development of comprehensive strategies to increase health professions workforce diversity. This session will focus on the presentation and a facilitated discussion of selected CTD recommendations that leverage the resources and expertise of diverse stakeholders at the local and regional level. Particular attention will be given to expanded roles for health professions employers and community stakeholders, and to the coordination of efforts throughout the K-16 educational process. Presenters will draw from a range of specific examples to illustrate the practical application of recommendations. Presenters will also discuss the concept of a statewide Master Plan for health professions workforce development with a focus on the diversity component of that workforce. Finally, presenters will discuss the progress and lessons learned from development of a state-wide health professions consortium focused on increasing health professions diversity through coordinated, unified efforts to support pipeline programs, advocacy and research and student resources. Jorge Girotti, Ph.D., Associate Dean and Director of Admissions, University of Illinois, Chicago Dr. Girotti is Associate Dean and Director of Admissions and Special Curricular Programs at UIC College of Medicine. He is also an Assistant Professor in the Department of Medical Education. As Director of Admissions, he manages all admissions processes for the College. As Dean of Special Curricular Programs, he oversees joint programs (MD/MPH, MD/MBA), the baccalaureate/MD program, and the Urban Medicine curriculum. Dr. Girotti also directs the Hispanic Center of Excellence, which aims to nurture, admit and retain Latino students, increase the number of Latino faculty, expose Latino medical students to health issues in underserved communities, and develop curricula to address cultural competence for all medical students. He earned a doctorate in Educational Administration and Policy from UIC in 1990. Currently, he is an Assistant Professor of Medical Education. His professional activities include: member of the Illinois State Board of health; member of the Board of Governors, Institute of Medicine of Chicago; treasurer of the Hispanic Serving Health Professions Schools, among others. ABSTRACT: Hispanics and Academic Careers: From Premed to Professorship The Hispanic Center of Excellence at UIC-COM has developed three complementary programs. The first, “Medicina Scholars”, is a three-year curriculum taught by volunteer Latino faculty and physicians that engages undergraduate students in learning about health care issues and careers in health professions. The second program, for Latino medical students, provides additional instruction on professionalism, the history of medicine, public health policy, and cultural competence. Students gain exposure to clinical cases and research through attending Grand Rounds in clinical departments. Students participate in a summer research fellowship at the conclusion of the first year of medical school. This intensive experience aims to increase students’ understanding of research modalities, while developing working collaborations with medical professionals. The third program is a two-year faculty fellowship. During the first year, faculty participate in the “Scholars for Teaching Excellence Faculty Fellowship” which emphasizes the skills in instruction, curriculum development, assessment and evaluation, scholarship, and educational leadership. During the second year, participants engage in an individual scholarly project designed to meet the needs of the fellow and his/her department. Results: Ninety students have enrolled in Medicina Scholars. In May 2008, the first cohort “graduates” from the curriculum. Of 33 students who began three years ago, 28 (85%) have fulfilled all requirements. We are beginning to track their next steps in applying to medical schools. On average, 15 students participate each year in the Summer Research Fellowship; more than double the average during the 1990’s. We are collecting early career choice data for graduates of the medical college from 2002-2007 to assess the impact of research exposure on participants’ professional work. Eleven faculty have completed the fellowship and all remain in academic settings. Fellows have successfully obtained extramural research funding and have published in peer-reviewed journals. Javier Sevilla, M.D., Associate Professor of Clinical Family Medicine Indiana University-School of Medicine Javier F. Sevilla Mártir, MD is originally from Honduras where he completed medical school in 1992. Previous to coming to the United States, Dr. Sevilla practiced medicine in Honduras as a general practitioner for four years. This included a year of work with an ambulatory clinic, providing care for the Lenca tribes in the mountains of Honduras. After completing his internship in Family Medicine at Cook County Hospital in Chicago, Illinois, Dr. Sevilla transferred to Indiana University where he completed his residency. Dr. Sevilla joined the Indiana University Department of Family Medicine in 2002 where he completed a one year faculty development fellowship in underserved medicine and leadership and now he offers elective rotations in Underserved Medicine to medical students and residents with emphasis on quality of care, cultural competence and medical Spanish. He was appointed Director of International Medicine and Hispanic Health within the department in 2005. Dr. Sevilla is faculty advisor for the Society of Latino SOL medical students and the International medicine and global health medical students interest group, providing support and guidance in the development of educational and service activities in the community and Latin America. ABSTRACT: Addressing Health Disparities Through Curricular Innovation in Medical Education As an initial step, we surveyed the community to identify the most common barriers faced to access health care which included cost of services seen as a barrier by 52.4% of the participants followed by lack of health insurance 44%, language 37.7%, fear of system 27.8%, transportation 7.9%, lack of knowledge of available services 5.2%, and other 4.1%. Based on these findings we developed programs directed to meet those needs including clinical services through a partnership with a community health center and the collaboration with medical students and a network of community organizations to provide health education. Curricular innovations were implemented at different levels. At the Family Medicine clerkship intersession we implemented a workshop for the appropriate use of medical interpreters and an elective course titled Care for the Underserved with emphasis on cultural competence and medical Spanish. The long term emphasis has been placed on the curricular integration of Introduction to Clinical medicine I and II and grammar and medical Spanish now in its third year. These further supported by culture and language immersion experiences at end of first year and a global health elective in Honduras during third and fourth year providing students an opportunity to understand the needs of migrants from Latin-American. Results: Since 2002 to 2008 the number of Hispanic/Latino students had increased from 4 to 20, an average of 40 students have participated in the credit bearing programs/courses, research with students participation has been done, an annual state wide Hispanic/Latino health summit has been celebrated for the past 4 years as a result of collaborations with different organizations among other achievements an the number of bilingual providers had increased in the community. A.3: Clinical: Hispanics and Health Communications- Steps to Improve the Cultural, Linguistic, and Generational Approach to Communicating Health Needs Moderator: Michelle Bholat, M.D., M.P.H., Vice-Chair, Clinical Affairs, Department of Family Medicine, UCLA Dr. Bholat is working to certify the UCLA International Medical Graduate so that individuals on F1 visas can obtain student status and not pay places like Kaplan several thousand dollars a year to sustain student status. In regards to the UCLA IMG program, there are Latinos who have been very critical of the program citing a turning of the back on second generation Latinos. With the percentage of Latinos at 49 percent graduating from HS, the recruitment pool to medical school as well as the 25 year results demonstrate a flat line in Latino enrollment to US medical schools. Poor education and poverty perpetuate this unfortunate situation. The de-emphasis on race and ethnicity in central LA helps eliminate the fact that 60 percent of the folks living there are Latino. There are big dollars being spent on the PRIME programs and this is good as the need for the primary care physicians in CA is great. In March 2009, she is hoping to have 12 MDs placed in CA FM residency programs. Alfredo M. Lopez-Yunez, M.D., Medical Director, Alivio Medical Center, Indiana University – School of Medicine Dr. Lopez-Yunez was a Resident Physican in Internal Medicine and Neurology from 1993 to 1997 in Chicago, IL. In 1997-1999 he was a Fellow in cerebrovascular disease at Indiana University School of Medicine. In 1999, he continued at Indiana School of Medicine as a clinical lecturer in Neurology. From 2001 to 2003, he was co-director at IU/Wishard Stroke Unit. Currently, Dr. Lopez-Yunez is a Medical Director at Alivio Clinic and Principal at Neurohealth Ltc, both in Indiana. In 1996, Dr. Lopez-Yunez was Chief Resident of the department of Neurology at Loyola University. In 2000 , he was the examiner for the American Board of Psychiatry and Neurology. In 2003, he received first place as the mentor for Annual Research paper Department of Neurology and Internal Medicine “Transcranial Doppler Evaluation of Intracranial Pressure in Fulminant Hepatic Failure” – Author: Esgi Tiryaki, MD. In 2004, he was the winner of the Junior Achievement of Indiana “Best and Brightest” in the health care category. In 2006, Dr. Lopez-Yunez received the Leader Fellowship Award-National Hispanic Medical Association. ABSTRACT: Intercultural Negotiation and Health Literacy The Institute of Medicine (2004) defines health literacy as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” Health literacy is reported as lower among minority groups and nonnative speakers (Gazmararian et al., 2005). Most studies have relied on standardized tests of literacy and health literacy (most testing vocabulary) rather than testing comprehension of the medication information given to patients. The three-year funded project on health literacy and medication adherence reported here took a different approach. It relied on in-depth interviews among 50 Spanish-speaking diabetes patients to find out what sources are used to get information about the prescription medications they take and how well they understood the written information about the medication. The semi-structured interviews tested comprehension of medical information and identified breakdowns in communication along the information path from initial physician-generated, to nurse or office-generated, to pharmacy-generated, and finally to the family and the caregiver. The design of the study was influenced by a framework from intercultural linguistics (Canagarajah, 2006), comparing mismatches between patients’ level of understanding of medication information with the materials given by health care providers. Based on previous research on textual characteristics of Patient Information Leaflets (Connor, Ruiz-Garrido, Rozycki, Goering, Kinney, & Koehler, in press), patients’ comprehension of the leaflets was tested in the language of choice, first language or English. Patients’ adherence to medication and health regime was assessed through self-reporting as well as medical report data. Correlations were conducted between the dependent variable – adherence—and the variety of independent variables – demographic data, source of information, comprehension of textual and verbal information. The results will provide information about reasons for noncomprehension and for writing medical labels and patient information leaflets that can be better understood and followed. Manuel Angel Oscos-Sanchez, M.D., Associate Professor, University of Texas Health Science Center, San Antonia, Texas A native of San Antonio, Texas, Dr. Oscós-Sánchez received his MD from Stanford University School of Medicine, completed Family Medicine Residency at the University of Texas HSC at San Antonio, and completed a 3-year research fellowship at the University of California Los Angeles where he focused on the use of ethnographic methods to investigate Latino adolescent health issues. Director of the Youth Development Program in the Department of Family and Community Medicine at the University of Texas HSC at San Antonio, he has developed, implemented, and evaluated several multidisciplinary community based positive youth development programs with Latino adolescents and their families. Teen Health Camps are in their 8th year, the Teen Medical Academy is in its 6th year, Familias en Acción is in its 4th year, the Health Science Preparatory Academy is in its 2nd year, and Familias SUAVE is in its 1st year of operation. He has published findings of Latino adolescent health research in the Journal of Adolescent Health, the Western Journal of Nursing Research, Family Medicine, and Hispanic Healthcare International. He has been the Principal Investigator of two Minority Health Research and Education Grants from the Texas Higher Education Coordinating Board; Co-Investigator of Familias en Acción, a violence prevention research program funded by the National Institute of Nursing Research; and Principal Investigator of Familias SUAVE, a Community-Based Participatory Action Violence Prevention Research Grant from the National Institute of Child Health and Human Development. He is an Associate Professor of Medicine with Tenure and President of the Texas Society for Adolescent Medicine. ABSTRACT: Positive Latino Youth Development: A Multidisciplinary Community Based Approach In this presentation the results of five ethnographic and four randomized controlled intervention studies with Latino youth will be discussed. The series of five ethnographic studies conducted with Latino youth in Southern California and South Texas will be integrated to suggest essential elements and a theoretical framework for positive Latino youth development. The results of two randomized controlled evaluations of programs aimed at increasing academic achievement (the Teen Medical Academy and the Health Science Center-Preparatory Academy) along with the results of two programs aimed at decreasing risky sexual health and violence related behaviors (Respetar y Proteger and Familias en Acción) will be discussed. Results: Ethnographic Studies- A series of ethnographic studies with Latino youth in both Southern California and South Texas explored life experiences with multiple issues including sexual health, violence, and substance use. These studies explored inherent assets and processes used by Latino youth to deal with the challenges in their lives. Collectively, the findings of these studies suggest essential elements to include in strategies for positive Latino youth development. Strategies must recognize that Latino youth are actively maturing, interacting, and managing their world. Strategies must recognize that Latino youth are capable of, but struggle to maintain balance. The establishment and maintenance of a connection or bond to a prosperous collective or familial past, a moral or spiritual code, and caring adults within their families and community help them maintain balance. The development of self-reflection, empathy for others, and a balanced view of malefemale relationships increase their capacity to form successful attachments in social relationships. Strategies that recognize and provide the opportunity to heal the pain of wounded relationships within the family and with broader American society that often oppresses, denigrates, and devalues Latino youth are more likely to succeed. Teen Medical Academy (TMA)- An evaluation of the first three years of the TMA demonstrated that greater participation in the TMA was independently and significantly predictive of greater interest in medical and allied health careers; confidence in the ability to achieve a health career, learn surgical skills, and learn other health career related technical skills; sense of belongingness in a health career and among doctors; and commitment and motivation to achieve a health career and meaningful work. The effect was present after controlling for other potentially significant variables. The results echoed previous findings that an emphasis on academic enhancement and instructional enrichment increases the potential for success. The study found that along with participation in the TMA, higher GPA and the opportunity to participate in a greater number of extracurricular health career programs were predictors of interest, confidence, belongingness, and achievement motivation. Further analysis revealed that interest in a medical career predicted college enrollment in the same sample of economically disadvantaged South Texas youth. HSC-Prep had immediate post program effects. Evaluation of 3 and 15 month post intervention effects, with the use of a randomized control group that did not participate in HSC-Prep, is being conducted with a 2.5 hour practice SAT in September of 2008 and 2009. If program effects persist, HSC-Prep will be a model that can be used to increase the number of academically qualified college applicants from economically disadvantaged ethnic minority communities. Respetar y Proteger- A randomized control evaluation of the Respeto y Proteger curriculum with 336 adolescent mothers and their male partners in Los Angeles was conducted by Dr. Janna Lesser, one of Dr. Oscós-Sánchez’ research colleagues. Outcomes of this longitudinal study from baseline to 6 months, indicate that the probability of unprotected vaginal sex episodes was significantly reduced among males and females (p=.001) in the experimental group as compared to those in the control group. Further analysis explored the role of parental protectiveness (defined as the parentchild emotional attachment that positively influences parental behavior) as an intrinsic factor that promotes resiliency and motivates behavioral change. These analyses demonstrate the moderating role that male parental protectiveness (that is, the father-child emotional attachment that positively influences parental behavior) had in improving the effectiveness of the intervention for his female partner, the young mother. While there was little change in unprotected sex over time in the females in the control group, regardless of male protectiveness at baseline, females in the intervention group showed a decline in unprotected sex over time, with a sharper fall observed among those where the male partners showed high protectiveness at baseline. These findings help to substantiate the growing body of knowledge that indicates that health promotion programs for adolescent and young parents can build on the strengths of inherent assets among these youth to motivate change from previously risky behaviors to more protective health behaviors. Familias en Acción Familias en Acción is engaging a predominantly Latino community in San Antonio in individual, family, school, and neighborhood activities designed to change violence related attitudes and behaviors. The intervention includes implementation of the youth violence prevention curriculum El Joven Noble and the complementary parent/guardian curriculum Cara y Corazón. The intervention was implemented by community members trained in program implementation with 3rd, 4th, and 5th grade boys and girls in seven randomly selected elementary school after-school programs of the Harlandale Independent School District. The seven control schools in the same district, not selected as intervention sites, are currently receiving the same curriculums (delayed treatment). A Community Collaborative Council comprised of members of the target community, community-based organizations, and school district personnel has been working as an equal partner with the research team to guide all components of the intervention plan, the evaluation, and a long-term plan for sustaining the partnership. No statistically significant differences in violent behaviors were found between the intervention and control group in this study. However a significant finding of the study was that at 3 months post intervention those who reported having a friend in a gang were 15 times more likely while those who had a greater nonviolent conflict resolution self-efficacy were three times less likely to report a violent act in the past week. In phase two of the project, Familias SUAVE, the effects of the intervention among Latino youth in a disciplinary alternative education program are being examined. Glen Nowak, M.A., Ph.D., Chief of Media Relations, Centers for Disease Control and Prevention Glen Nowak is the chief of media relations at the Centers for Disease Control and Prevention. Prior to joining the Division of Media Relations in June, 2004, Dr. Nowak served five years as the associate director for communications at the National Immunization Program at the CDC. As NIP’s associate director of communication, Dr. Nowak was responsible for a wide range of communications activities, including websites, media relations, and public information campaigns targeted to Hispanics. Prior to joining NIP in January 1999, Dr. Nowak was an associate professor of advertising and communication at the University of Georgia. At Georgia, Dr. Nowak taught undergraduate and graduate courses in principles of advertising, communication and advertising management, social marketing and health communications. In the past twelve years, he has authored or co-authored a number of peer-reviewed journal articles on communications practices, social marketing, and health communications. Dr. Nowak received his B.S. in 1982 from the University of Wisconsin-Milwaukee, with majors in both economics and communications. He continued his studies at the University of Wisconsin-Madison, where he subsequently earned an M.A. degree in journalism (1987) and a Ph.D. in the field of mass communications (1990). ABSTRACT: Communicating Health Information to Hispanics Through the Media: Challenges and Strategies The Centers for Disease Control and Prevention (CDC) is considered the premier public health agency in the United States. The presenter will describe how CDC communicates health information to Hispanics through the media, including how the agency trains doctors and scientists to become effective media spokespersons. The presenter will also discuss some of the challenges the government agency faces in reaching Hispanics with credible bilingual, targeted health information via the media and the strategies it employs to protect and increase its credibility among both Hispanic and media audiences. Dirk G. Schroeder, Sc.D., M.P.H., Executive Vice-President and Co-Founder, DrTango, Inc., Georgia Dr. Dirk G. Schroeder is a tenured, Associate Professor of Global Health at Emory University where his academic efforts focus on improving the health of Hispanic and multicultural populations in the U.S. and abroad. Dr. Schroeder is also the Executive Vice-President and Co-Founder of DrTango Inc. For nearly 10 years, DrTango has been delivering culturally-appropriate solutions to many of the country’s preeminent hospital systems, including Tenet Healthcare, Yale New Haven, UCLA Medical Center, CHRISTUS Health, and 400+ other hospitals for their multilingual/multicultural patient populations. Dr. Schroeder has personally designed, delivered and evaluated these patient-centric programs for hospitals. At Emory, he teaches a course on Public Health Research Design and Evaluation to almost 100 MPH students, many of whom participate in evaluation efforts of hospital-directed solutions. Dr. Schroeder has written and presented widely on LEP, CLAS and SB853 regulations and the use of technology to delivery culturally- and linguistically tailored interventions that can narrow the health disparities gap. He is the Senior Director of a $2 million+ state-wide program for the State of Florida (www.HOPEFlorida.org), a three-year, Robert Wood Johnson Foundation research study on the efficacy of eHealth for Hispanics, and Merck’s global initiative on patient-centered care. He is on the board of the Hispanic Health Coalition of Georgia and a technical advisor to the Robert Wood Johnson Foundation and Technology and Child Obesity. He is the recipient of a Professor of the Year Award (Emory University), a Fulbright Fellowship (Indonesia), and Future Leaders Award (Dannon Nutrition Institute), among other accolades. He is the author of one book, numerous book chapters and over 80 scientific articles. Dr. Schroeder has lived and worked in over 75 countries and is fluent in Spanish and Indonesian. He has Doctoral and Masters Degrees in International Nutrition from Johns Hopkins University and a Post-doc from Cornell. He completed his undergraduate work, with honors and distinction, at Stanford University. ABSTRACT: Evaluation of a culturally- and linguistically-appropriate eHealth portal to facilitate improved diets, increased fitness-levels, and weight-loss among U.S. Hispanics – Phase II Maryland MiDietaTM/MyDietTM1 is the leading online diet, fitness and weight management portal for U.S. Hispanic/Latinos. MiDieta is bilingual (Spanish/English), based on Latino foods and habits and already available through dozens of media, hospital, and health plan websites. Hundreds of thousands of Hispanics access MiDieta each week. HHS selected MiDieta as one of the “20 most innovative health promotion and disease prevention applications” in the U.S. In Fall, 2004, DrTango, Inc. received a large, highly-competitive grant from the Robert Wood Johnson Foundation Health eTechnologies Initiative. In collaboration with CareFirst Blue Cross Blue Shield of Maryland (CareFirst), we conducted a randomized trial, assigning overweight Hispanics to one of six groups: (1) online MiDieta; (2) offline MiDieta; (3) online control; (4) offline control; (5) online and offline MiDieta; and (6) online and offline control. We enrolled and randomized a group of participants through CareFirst in November, 2007. A.4: Research: Hispanics and Clinical Trials: Increasing Participation to Decrease Disparities Moderator: Guadalupe Pacheco, M.S.W., Special Assistant to the Deputy Assistant Secretary for Minority Health, U.S.D.H.H.S. Guadalupe Pacheco serves as a Public Health Advisor and Special Assistant to the Deputy Assistant Secretary for Minority Health, U.S. Department of Health and Human Services. He has occupied mid-level and senior level management positions in State and Federal government agencies, as well as nonprofit organizations, focusing on health and human services program and policy issues. In his current capacity as Special Assistant to the Director for Minority Health, Mr. Pacheco is responsible for managing multiple projects that address health disparities of racial and ethnic minority communities. He staffs cultural competency activities through the Office of Minority Health’s Center for Linguistic and Cultural Competence in Health Care. Additionally, he staffs and coordinates initiatives and program activities that enhance service delivery to Hispanic Americans. Owen Garrick, M.D., M.B.A., Chief Operating Officer, HOV Clinical Research Dr. Owen Garrick joined HOV Clinical Research Inc. in 2006 as Chief Operating Officer and Director. He has overall responsibility for the Clinical Trials and Investigator Training business units. HOV is the leading company focused on increasing the participation of ethnic minority investigators and patients in pharmaceutical sponsored clinical trials. In addition to profit & loss responsibility for the business units, Dr. Garrick has oversight of all financial, administrative, and legal aspects of the parent company, and serves on the board of directors as corporate secretary. Dr. Garrick was formerly Director of Corporate Strategy and M&A at McKesson Corporation. He led McKesson's effort in vertical integration and was responsible for evaluating and managing new initiatives and business opportunities for the pharmaceutical division. His responsibilities included overseeing market analysis, monitoring competitive activity and defining vision, strategies, and tactics for the company. Dr. Garrick also provided leadership in the planning, designing and integration of acquired business. Some of his key accomplishments included the $450M acquisition of D&K Healthcare, the launch of McKesson's Generic Drugs Telesales Business Unit, and the development and launch of McKesson's Drug Adherence Business. Prior to McKesson, Dr. Garrick was the Executive Director and Global Head of M&A Negotiations at Novartis Pharmaceuticals. In this position he structured, negotiated and closed both M&A and complex license transactions. He specifically oversaw small and medium size company acquisitions, hybrid equity/license right deals, mature product divestments, and venture investments in biotechnology companies. Previously he spent four years at Goldman Sachs in New York, functioning as an investment advisor working with private healthcare companies as they sought to grow, raise capital, and perform initial public offerings. Dr. Garrick earned his MD from the Yale School of Medicine and his MBA from the Wharton School of Business. He holds an AB in Psychology from Princeton University and continues to be an active alumnus, serving on the national fundraising board. ABSTRACT: Hispanic Investigator Participation in Clinical Trials: A Means to Improve Health Disparities Pharmaceutical and biotech companies are facing more stringent requirements surrounding efficacy and safety on new drug applications, particularly as they relate to minority populations and women. As pharmaceutical and biotech companies struggle to find investigators and patients to fill their clinical trials in order to get FDA approval and get drugs to the market faster, thus increasing their potential to boost their profits. According to the U.S. Census Bureau ethnic minorities will be 50% of the total population by the year 2050. Hispanics represent the largest minority subgroup in the United States, and are disproportionately, and more severely affected as well as have a higher incidence of several diseases including: cardiovascular disease, diabetes, hyperlipidemia, asthma, obesity, hypertension, Stroke, congestive heart failure, certain cancers (colon, breast, cervix, prostate, etc.), Infective diseases (AIDS), Neuropsychiatric illnesses and cerebrovascular disease. Complying with the FDA guidelines regarding proportional inclusion of minorities and women in clinical trials has the potential for life saving medicines to be made available sooner as new products receive quicker approval and are brought to market sooner. Further, the Center of Drug Evaluation & Research (CDER) notes that 5% or less of the participants in 2500 clinical trials conducted between 1995 and 1999 were Hispanic. This trend continues today, even though it has been well established that certain drugs are metabolized differently in ethnic sub-groups and women. Thus, minority inclusion in clinical trials also serves to improve healthcare for all Americans. It has also been determined that a major barrier to successful drug development has been finding appropriately trained and experienced clinical investigators who have access to specific patient populations required to adequately test a drug’s efficacy and safety. In this regard, Hispanic physicians represent an important source of new clinical investigators that have ready access to this highly valued clinical population. Results: Diversifying the clinical investigator and patient pool will help ensure that new medications are efficacious in all populations. Hispanic physician practices can get involved in clinical trials if they understand the resources and commitment necessary Ricardo Senno, M.D., M.S., F.A.A.P.M.R., Medical Director, SENNOGROUP, Lincolnshire, IL Dr. Ricardo Senno has both an international and national reputation in the field of Physical Medicine and Rehabilitation, specializing in the subspecialty of brain injury. His extensive curriculum vitae is highly published, has lectured internationally, and has appeared in multiple media, including the Chicago Tribune, the Discovery Channel and Telemundo. Furthermore, Dr. Senno has conducted research for the Center for Disease Control (CDC). At the Rehabilitation Institute of Chicago Northwestern University, he was Medical Director of the Brain Injury Medicine and Rehabilitation Program. He was the medical ethics consultant in the Terry Schiavo case, lectured in Slovenia and Ecuador, has done research work in brain injury medicine as it relates to spasticity and continues to work for the CDC. In addition, he also holds a Master’s in Urban Planning, Policy Analysis and Public Management and is involved in the design of local and international health care facilities, (i.e. Brain Injury Floor of the Rehabilitation Institute of Chicago, Exploration Center in Ecuador and the International Inclusion Center for El Valor) Dr. Senno has volunteered to teach the Essentials of Clinical Medicine course for his third consecutive year in 2008-2009. Multiple students have nominated Dr. Senno for outstanding teaching and mentoring awards. In addition, he volunteers to teach the Hispanic Center of Excellence curriculum of Medicina Scholars, is al LPC preceptor, and volunteers to mentor students. Furthermore, he is an advocate of the Hispanic Center of Excellence and currently Medical Director of his clinic, Sennogroup Wellness and Rehabilitation in Lincolnshire, Illinois. ABSTRACT: Fundamentals and Current Concepts in the Treatment and Rehabilitation of People with Brain Injury: A Multidisciplinary Team Approach In the United States, a brain injury occurs every 21 seconds. The Center for Disease Control has declared this to be an epidemic. This is especially important given the number of veterans who are currently returning with and suffering from the consequences of brain injuries. Amelie Ramirez, Ph.D., Redes en Accion, University of Texas Health Science Center, San Antonio, TX Amelie G. Ramirez, Dr.P.H., an internationally known expert on health disparities among Latinos and other populations, is a professor of epidemiology and biostatistics at The University of Texas Health Science Center at San Antonio. She also is founding director of the Institute for Health Promotion Research (IHPR), which is dedicated to finding solutions to health disparities in South Texas and beyond, and has two endowments to support her research and that of the IHPR – the Dielmann Chair in Health Disparities Research and Community Outreach and the Max and Minnie Tomerlin Voelcker Endowed Chair in Cancer Healthcare Disparities and Outreach at the Cancer Therapy & Research Center (CTRC) at The University of Texas Health Science Center at San Antonio. Over the past 25 years, Dr. Ramirez has directed many state-, federal- and privatelyfunded research programs focused on human and organizational communication to reduce chronic disease and cancer health disparities affecting Latinos. She has authored many peer-reviewed articles and is frequently invited to speak at scientific meetings. Dr. Ramirez has been awarded state and national recognition for her work in public health and health disparities research and the advancement Latinos in medicine, public health, and behavioral sciences professions across the United States. Her long list of honors includes the following: 2007 election to the Institute of Medicine of the National Academies, 2007 Professor of Survivorship from Susan G. Komen For the Cure, 2003 Humanitarian Award from the American Cancer Society, and the 1996 Sarah Mazelis Award for Health Promotion from the American Public Health Association. Dr. Ramirez also is a member of many national and regional advisory groups and coalitions, including the CDC’s Breast and Cervical Cancer Early Detection and Control Advisory Committee, Komen’s Scientific Advisory Board, and the Lance Armstrong Foundation’s Board of Directors. ABSTRACT: A Patient Navigator Intervention to Improve Breast and Cervical Cancer Treatment Outcomes Among Hispanic Women Redes En Acción: The National Latino Cancer Research Network, a National Cancer Institutesupported Community Networks Program that is based at The University of Texas Health Science Center at San Antonio, aims to stimulate cancer control research, awareness, and training. In hopes of using its network to launch a national “patient navigator” (PN) program to help Hispanics access cancer care across the U.S., Redes is pilot-testing the efficacy of using a patient navigator program (using trained community lay health workers) to help female Hispanic patients access and use breast and cervical cancer care services at two community clinics in a large, low-income, MexicanAmerican neighborhood in San Antonio, Texas. The project aims to reduce lag times between abnormal breast cancer screening results and diagnosis and treatment. During the first six months of project implementation, investigators finalized protocols, obtained IRB approval, and recruited and finalized partnerships with medical services and the two community clinics managed by the Department of Family and Community Medicine at The University of Texas Health Science Center at San Antonio. They also conducted an environmental scan and a PN needs analysis before drafting a PN training curriculum, patient survey, and tracking database. They then trained a patient navigator and, in months 6-18, began meeting regularly, reviewing clinic records, recruiting patients to navigation services, refreshing the PN’s training, populating the PN database, administering pre- and post-surveys and comparing clinic data collection. In months 18-24, they will analyze results, report findings, and a develop manuscripts for publication. The goal was to recruit 116 women (58 in the intervention group and 58 in the control group). Intervention participants took frequent advantage of many of the patient navigator’s services, such as help with medical appointment scheduling, appointment reminders, transportation, financial aid, and extra health information in the participant’s primary language. “For one cancer patient who originally felt alone and confused in scheduling her appointments, I provided her help with transportation, appointment scheduling, and interpretation when she didn’t understand health information. She was happy knowing I was there for her, and her experience in this program even motivated her to educate her daughter about the importance of getting annual exams,” said Sandra Veronica Covarrubias, the project’s patient navigator. As the project progressed, investigators uncovered some vital lessons, including the importance of eliciting feedback from all program stakeholders so that, if needed, modifications can be made promptly and adequately. Also, in a project that requires a lot of effort and resources to implement, it’s also preferable to provide: an incentive to encourage participants to stick in the program; culturally appropriate training for patient navigators; and more than one navigator to help reach the intended audience. By project completion, the data collected will help design a model of cancer care using a patient navigator intervention to improve breast and cervical cancer treatment outcomes that can be replicated and disseminated in other communities where Hispanic women encounter significant disparities in cancer health care delivery. Guadalupe Pacheco, M.S.W., Special Assistant to the Deputy Assistant Secretary for Minority Health, U.S.D.H.H.S. Guadalupe Pacheco serves as a Public Health Advisor and Special Assistant to the Deputy Assistant Secretary for Minority Health, U.S. Department of Health and Human Services. He has occupied mid-level and senior level management positions in State and Federal government agencies, as well as nonprofit organizations, focusing on health and human services program and policy issues. In his current capacity as Special Assistant to the Director for Minority Health, Mr. Pacheco is responsible for managing multiple projects that address health disparities of racial and ethnic minority communities. He staffs cultural competency activities through the Office of Minority Health’s Center for Linguistic and Cultural Competence in Health Care. Additionally, he staffs and coordinates initiatives and program activities that enhance service delivery to Hispanic Americans. ABSTRACT: HHS Office of Minority Health’s : A Physicians’ Practical Guide to Culturally Competent Care: A Tool to Facilitate the Elimination of Racial and Ehtnic Health Disparities. A Physician’s Practical Guide to Culturally Competent Care was developed through a rigorous process that included: convening of a National Project Advisory Committee(NPAC); development of an Environmental Scan; topical commission papers; a Consensus-Building meeting; needs assessment focus groups; pilot and field testing of draft curricula, and ongoing input from the NPAC subject matter experts. The curriculum was subject to a systematic, mixed-methods evaluation in 2006. Quantitative and qualitative data was collected through surveys embedded in the curriculum and focus groups conducted across the country. Results were utilized to assess the validity and reliability of the curriculum, and inform what revisions should be made. Evaluation results will be presented. Results: A Physician’s Practical Guide to Culturally Competent Care is designed to increase awareness of cultural competency with the goal of reducing disparities. The evaluation findings indicate that curriculum participation results in enhanced self-awareness of cultural competency concepts. Over 88% of the program has over 20,000 users and has awarded over 73,000 continuing education credits, to date. The curriculum supports the mission of OMH and the National Standards for Culturally and Linguistically Appropriate Services (CLAS) in Health Care. Maria Botello-Harbaum, MS, EdD Evaluation Manager, Consumer Union, Best Buy Drugs, Washington, DC Maria Botello, MS, EdD, is the evaluation manager for the Consumer Reports Best Buy Drugs™, a public education project of Consumers Union, the publisher of Consumer Reports. Maria Botello completed her EdD in Health Education at Teacher’s College, Columbia University through the auspices of a 3-year NIDA Minority Research Award. The mission of the Consumer Reports Best Buy Drugs project is to provide consumers and their doctors with information to help guide prescription drug choices–based on effectiveness, a drug's track record, safety and price. The project aims to improve access to needed medicines for tens of millions of Americans–because they lack insurance coverage for prescription drugs, because the prices of many medicines today are so high, and because B.1: Policy: Hispanic Health Disparities: National Perspectives and Local Solutions Linda Griego, President, Griego Enterprises, Inc., Los Angeles, CA, Member – NHMA Board of Directors Linda Griego is an entrepreneur and former Los Angeles deputy mayor. Her career encompasses civic leadership, business management and government service. Griego is president of Griego Enterprises Inc., which produces television programming through Zapgo Entertainment Group. She is the managing general partner of Engine Co. No. 28, a successful downtown restaurant that she founded in 1988. She also owns and operates a lodge in northern New Mexico. Linda Griego rejoined the Robert Wood Johnson Foundation’s Board of Trustees in January 2005. She had previously served as a trustee from 1995 until 2003.From 1999 until 2000, Ms. Griego was the interim president and chief executive officer of the Los Angeles Community Development Bank, a $430 million federally funded development bank. From 1994 until 1997, she served as president and chief executive officer of Rebuild LA, a nonprofit corporation created in 1992 to spearhead a five-year riot recovery plan. From 1991 to 1993, she served as deputy mayor of Los Angeles. In January 1993, she resigned her post to run for mayor. In 1993, she worked for the late U.S. Secretary of Commerce Ron Brown. Ms. Griego currently serves as a trustee of the David and Lucile Packard Foundation and the Public Policy Institute of California. Griego has served on the boards of several national and local organizations. From 1998 until 2003, she served as a Los Angeles director of the Federal Reserve Bank of San Francisco. Griego was a presidential appointee to NAFTA's North America Development Bank from 1995 until 2000. She was a member of the California Community Colleges Board of Governors. In January 2004, she joined the Board of Governors of Cedars Sinai Medical Center in Los Angeles. Ms. Griego currently serves on the boards of directors of three publicly traded companies, City National Bank, Granite Construction, Inc. and Southwest Water Company. Throughout her career, she has received several leadership awards including the City of Hope, UCLA, Los Angeles Chamber of Commerce, the Mexican American Bar Foundation and the San Francisco Hispanic Foundation. Griego earned a B.A. in history in 1975 from UCLA. She was a senior fellow at the UCLA School of Public Policy from 1998 until 2000. Ernest Moy, M.D., M.P.H., Medical Officer, Agency for Healthcare Research and Quality, U.S.D.H.H.S. Ernest Moy, M.D., M.P.H. is a Medical Officer in the Center for Quality Improvement and Patient Safety at the Agency for Healthcare Research and Quality (AHRQ). At AHRQ, his work has included directing the development of the annual National Healthcare Disparities Report and National Healthcare Quality Report and supporting AHRQ’s Excellence Centers for the Elimination of Ethnic/Racial Disparities and AHRQ’s Patient Safety Organization program. Prior to joining AHRQ, he was Director of Research and Assistant Vice President of the Center for the Assessment and Management of Change in Academic Medicine at the Association of American Medical. Ernest is a graduate of Harvard College and New York University School of Medicine. Following internal medicine residency, he was a general internal medicine fellow at Columbia University, a Robert Wood Johnson Health Care Finance fellow at Johns Hopkins University, and an assistant professor of medicine at University of Maryland School of Medicine. Ernest’s research interests include disparities in access and quality of care, particularly as they relate to academic medical centers, patient safety, and technology diffusion. He is chair of the Racial and Ethic Disparities Committee of the American Public Health Association’s Medical Care Section and on the editorial board of Medical Care Research and Review. ABSTRACT: Health Care Disparities: Variations across States National data demonstrate that Hispanics experience many disparities in health care, but less in known about variation across States. Understanding geographic variation may enable policymakers to better target disparities interventions. Data come from the 2006 Behavioral Risk Factor Surveillance System. Five adult preventive care services were examined: 1) Mammogram among women age 40 and over; 2) Pap tests among women age 18-65; 3) Colorectal cancer screening among adults age 50 and over; 4) Flu shot among adults age 65 and over; and 5) Pneumococcal shot among adults age 65 and over. For each measure, differences in service receipt were examined between Hispanics and non-Hispanic whites. Differences were examined for all States in aggregate and for each individual State (50 States, DC, Puerto Rico, and Virgin Islands). Results: Wide variations in Hispanic disparities across States are observed. Hispanic-NonHispanic White differences are particularly large for colorectal cancer screening and immunizations. Matthew O’Brien, M.D., Clinical Scholar, Robert Wood Johnson Foundation Dr. O’Brien is a general internist, having completed medical school at Brown University in 2004 and residency in Internal Medicine at the University of Pennsylvania in 2007. During medical school, Dr. O’Brien was student director of a free clinic that served a new Hispanic immigrant community in Providence, RI. He also spent a year during medical school working in Chile and Guatemala providing public health education in rural villages. During residency at the University of Pennsylvania, Dr. O’Brien and his faculty mentor started a clinic (named Puentes de Salud) that provides primary care services to a rapidly growing Hispanic immigrant community in Philadelphia. Dr. O’Brien is currently a Robert Wood Johnson Clinical Scholar at the University of Pennsylvania. His research interests include alternative models of care delivery to redress disparities in access and outcomes among Hispanic immigrants. Dr. O’Brien is currently the PI on an NIH-funded study using community health workers, or promotoras, to improve Pap smear screening and promote early detection of cervical cancer. ABSTRACT: Cancer Control in Hispanics: Promotoras and Cervical Cancer in the South Philadelphia Hispanic Community Purpose: To implement and evaluate a cervical cancer prevention program led by community health workers, or promotoras, in the South Philadelphia Hispanic Community. Methods: We recruited 6 promotoras to lead a series of two 3-hour workshops with women in the community about the epidemiology of cervical cancer in Hispanic women, the pathogenic role of HPV, and screening procedures. The implementation of these classes will begin in November 2008. The study is a randomized trial of this educational intervention, with 60 participants in each arm. Using a CBPR model, the promotoras participated actively in the design on the study, planning of the intervention, and recruitment and enrollment of subjects. Cervical cancer risk, previous screening history, baseline cervical cancer knowledge, and self-efficacy was measured by a preintervention questionnaire. After the intervention and a subsequent 12-month follow-up period, the post-intervention questionnaire will measure the following outcomes: cervical cancer knowledge, self-efficacy, and receipt of Pap smear screening in the previous year. At the suggestion of community partners involved in the study design, the control group will receive the same promotora-led intervention after completion of follow-up. Results: Univariate analyses were performed using chi square, t-test, and the Mann-Whitney test. There were no statistically significant differences between the control and intervention subjects with respect to the following baseline characteristics: age, nationality, years of U.S. residence, health status, insurance status, smoking status, lifetime sexual partners, parity, or HIV positivity. Furthermore, univariate analyses revealed no significant baseline differences between the two groups on the outcome measures: cervical cancer knowledge, up-to-date Pap smear screening, and self-efficacy. Wilma E. Waithe, Ph.D., R.D., C.D.N Director, Office of Minority Health, New York State Department of Health Currently, Dr. Waithe is serving as the Director of the New York State Department of Health, Office of Minority Health, a position she has held since 1999. Her resultsoiented approach has helped to position this office as a nationally recognized leader in community participatory approaches for improving minority health. Dr. Waithe has also distinguished herself as a leader in public health nutrition through her work with the NYC Head Start Program, the Cornell Cooperative Extension Service, and the New York State Department of Health. She received her undergraduate degree in Home Economics and Dietetics from Brooklyn College and her Masters in Food and Nutrition from the New York University. Dr. Waithe earned her doctorate in Education at the State University of New York at Albany. Her research interests are adult learning, minority health disparities, and evaluation capacity building. She is a member of several professional organizations. Workshop Session B: Hispanic Health Disparities: National Perspectives and Local Solutions Presentation Title: Strengthening Public Health In New York State to End Health Disparities Presenter: Wilma E. Waithe, RD, CDN, PhD, Director, Office of Minority Health, NYS Department of Health Abstract According to the Institute of Medicine’s Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, a comprehensive, multi-level strategy is needed to eliminate health disparities. This presentation will focus on work underway in New York State to create a comprehensive State Department of Health solution for eliminating heath disparities. The presentation will also be an opportunity for participants to provide input regarding the proposed action plan priority areas and implementation strategies. B.2 Health Professions Education: Integrating Hispanic Culture in a Healthcare Setting – Cultural Competence Solutions Alfonso Vargas, MD Chairperson, NHMA Council of Medical Societies, Member – NHMA Board of Directors Alfonso Vargas, MD was born in Bogotá, Colombia in 1947. Graduated in 1973 from the School of Medicine of the Universidad Nacional de Colombia, where his father Professor Alfonso VargasRubiano was Dean and Honorary Professor of Pediatrics. He did his training in pediatrics and pediatric endocrinology from 1975 to 1979 at the University of South Florida College of Medicine, Tampa General Hospital, and All Children’s Hospital in Tampa and St. Petersburg, Florida under Professors Lewis Barness, Allen Root, Edward Reiter and John Malone. He continued there as Assistant Professor of Pediatrics. In 1985 he was appointed Chief of Pediatric Endocrinology at the University pediatric Hospital of “La Misericordia” and Assistant Professor of Pediatrics at the Universidad Nacional de Colombia in Bogota. He was a Founding Member of the Sociedad Latinoamericana de Endocrinologia Pediatrica – SLEP in 1987. From 1988 to present he has been a member of the faculty at the Louisiana State University Health Sciences Center – School of Medicine in New Orleans, where he is Professor and Vice-Chairman for Education and International Affairs of the Department of Pediatrics. He has received several awards for his contributions in education amongst them the LSUHSC “Humanitarian Professor of the Year 2002” and the “Robert Suskind and Leslie Lewinter-Suskind Professorship for International Collaboration in Pediatrics”. As Director of the International Scholars Program of the Lawson Wilkins Pediatric Endocrine Society he has helped more than forty young pediatric endocrinology faculty to receive grants and participate in scientific and research programs in academic centers in the USA and Canada. He has been a member of the Children and Adolescent Work Group of the National Diabetes Education Program – NDEP (www.ndep.nih.gov) a joint effort of the National Institute of Health–NIH and the Center for Disease Control-CDC. He belongs to several editorial committees and has been a “Guest Professor or Lecturer” in over a dozen of Latin-American countries, Italy, Switzerland, Spain, Czech Republic, and Australia. He has published more than fifty works in scientific journals and specialized books. He is the 2007-2009 President of the Hispanic American Medical Association of Louisiana – HAMAL (www.hamal-inc.org) and as such a member of National Hispanic Medical Association – NHMA (www.nhmamd.org) Council of Medical Societies Manuel A. Selva, Jr., M.D., M.B.A., Market Medical Director, United Healthcare Dr. Manuel A. Selva is a Board-certified Internist who for the past six years has been the South Florida Market Medical Director for UnitedHealthcare. His responsibilities include being the Hispanic spokesperson for UnitedHealth Foundation’s “America’s Health Rankings” project. Dr. Selva graduated from the Universidad Autonoma de Guadalajara Medical School, and did his Internal Medicine Residency at St. Vincent’s Medical Center in Staten Island, New York. He was in private practice in Northern California, and completed an MBA at the University of South Florida in 1997. Dr. Selva has appeared on national and local television and media events discussing topics relating to Hispanic health issues. ABSTRACT: “PlanBien”: Hispanic Healthcare for Hispanics Hispanics have become a minority “majority” in a number of areas in the US. They should be able to easily access health care that is respectful of their cultural and linguistic needs. This should include Spanish-speaking physicians and staff, along with Spanish-speaking Case Managers and Disease Managers. “PlanBien” a unique bilingual, bicultural health-information program for Spanish-speaking individuals and their families, was introduced in South Florida in July, 2008, to small business owners with a large percent of Hispanic workers. The goal was to provide cost-effective health benefits to the large Hispanic population in South Florida, who were either too intimidated or too confused with our managed care system to effectively access and receive necessary health care. Among the actions taken to meet these needs were bilingual:Plan Materials / Enrollment forms / Benefit summaries / Dedicated Customer Service / Disease Management and Case Management Nurses / health education fliers, tools and resources / websites. Results: The results will be evaluated by a look back at the number of enrollees who actually accessed some of the unique services referenced above. Jaime G. Gonzales, M.S.S.W., M.S.H.A., National Business Development Manager UnitedHealthcare, Latino Health Solutions Plano, TX Jaime González is the National Business Development Manager for UnitedHealthcare’s Latino Health Solutions Jaime has more than 20-years of experience in the insurance sector for 10-years, all of which have been with UnitedHealthcare and its subsidiary, PacifiCare, A UnitedHealthcare Company. Jaime has extensive healthcare experience in clinical case management, business development and marketing and health policy. In his role as National Business Development Manager, Jaime is based in the DFW Metroplex and covers almost the entire country supporting UnitedHealthcare’s sales and account management teams and training them on the use of UnitedHealthcare’s various bilingual (Spanish-English) materials, programs and services especially designed for clients with a Hispanic-employee base. Jaime also assists with the development of UnitedHealthcare’s health and wellness products and services especially designed for the Hispanic consumer. Jaime maintains close working relationships with numerous Hispanic Chambers of Commerce and Hispanic-based Professional Associations and Organizations in strategic locations nationwide, and manages various national partnerships with key publications and organizations across the country. In May 2008, Jaime was named the first-ever recipient of the UnitedHealth Group “Living the Mission Award” by the UnitedHealth Group Senior Leadership. Jaime earned a Master’s of Science Degree in Health Administration (MSHA) from Texas Woman’s University and a Master’s of Science Degree in Social Work (MSSW) from the University of Texas at Arlington. He is currently pursuing a doctoral degree in Public Health (DrPH) at the University of North Texas Health Science Center, School of Public Health. His concentration of study is Health Management and Policy with an emphasis in Hispanic/Latino Health. His dissertation research focuses on Hispanic health, health insurance and the health seeking behaviors of Hispanics. Gonzalez served on the organizing committee for the First National Latino Diabetes Forum, which was held in Atlanta in September 2005. The Forum resulted in the establishment of the National Hispanic-Latino Diabetes Federation Flavia Mercado, M.D., Medical Director, Grady Health Systems, Georgia Flavia Mercado is the medical director of the Department of Multicultural Affairs and the International Medical Center at Grady Health System in Atlanta, Georgia. She is an Assistant Professor in the Department of Pediatrics at Emory University School of Medicine. Dr. Mercado is an expert in Hispanic health issues and is interested in decreasing health disparities and increasing health care access for Hispanics and promoting workforce diversity by educating and training bilingual bicultural health care providers/researchers. ABSTRACT: The International Medical Center, La Joya del Sur/the Southern Jewel - How to Build a Holistic Bilingual/Bicultural Patient-Centered Clinic in an Academic Setting The presentation will provide the lessons learned on how to build a successful patient centered primary care clinic in a health system and academic setting. Results: Since its inception the IMC has been a unique and successful clinic for educating providers and patients. The IMC has been used as a recruiting tool for Internal Medicine residents considering coming to Emory and Grady due to the high level of satisfaction from the residents who have their continuity clinic at the IMC. Every year there is more demand from incoming residents to do their continuity clinic at the IMC than the IMC can accommodate. The IMC has graduated over 10 bilingual bicultural internal medicine residents who most have continued their academic training in subspecialties like cardiology, infectious disease and endocrinology. One of IMC’s goals is to increase primary care capacity at the IMC and within the Atlanta community and unfortunately this goal has still not been reached. Marilyn Fraser-White, M.D., Associate Director, Research and Training, The Arthur Ashe Institute for Urban Health Dr. Marilyn White is Associate Director of Research & Training at the Arthur Ashe Institute for Urban Health. Since joining the Institute in 2001, she has been instrumental in coordinating the breast and prostate cancer programs, facilitating health education workshops on breast health, providing health screening and securing funds to further the Institute’s work in the community. She is also a member of the faculty of the Institute’s Health Science Academy, serving as a mentor and instructor for talented minority students interested in the health professions. Dr. White serves as the co-director of the Community Outreach core of the Brooklyn Health Disparities Center. Dr. Marilyn White is a graduate of the Spartan Health Sciences University School of Medicine in St. Lucia, West Indies, where she maintained an enviable scholastic record. She obtained a bachelor’s degree in Chemistry from the City University of New York at Brooklyn College. During her medical education, she was afforded the opportunity to be exposed to various types of health care delivery systems, within the United States and abroad. Her medical training has included work in the West Indies, Mexico and various US cities such as Kansas City, Washington, DC and New York City. She has also worked at the New York City Department of Health, Bureau of Tuberculosis Control as a Public Health Advisor for it Regulatory Affairs Department. During her employment, she was responsible for educating and counseling patients about tuberculosis, as well as writing orders of detention for patients with tuberculosis who refused to comply with medical treatment for tuberculosis. Her knowledge as a clinician combined with her experience with delivering grassroots, culturally competent, disease prevention messages and her genuine devotion and caring for people has been a valuable asset. ABSTRACT: Stylists were selected from the target communities of Sunset Park, and Williamsburg/Bushwick in Brooklyn. Stylists were selected from salons within each community and asked to participate in the focus group. The recruitment of the stylists consisted of site visits by a bilingual outreach worker to the various salons. A recruitment packet was generated to be distributed to the stylists during the field visits. This packet contained a letter of invitation describing the program, two letters of support from stylists, and a list of beauty salons that were previous participants in Institute’s Nuestra Belleza project. The initial phase of the recruitment entailed conducting an evaluation of the salon. The evaluation was used to obtain information about the specific salon including contact information for the owner/ manager, number of stylists working at salon, average number of customers served on a busy day, as well as the most convenient day for a training and/or focus group, based on stylist opinion. During the field visit, each stylist was (1) invited to participate in the focus group on a particular date and time; (2) informed that refreshments would be served and a stipend ($100 honorarium) would be issued at the conclusion of the workshop. All additional contact or correspondence with stylists included a description of the activity, incentives, and one of three tentative dates from which they could select up to two. In previous Institute projects, Monday was used for meeting dates since most salons were closed on Mondays. However, an increasing number of salons are open for business on Mondays as well. Nevertheless, the day for the meeting was determined based on stylists’ majority response as to best date for the focus group. The focus groups were all held in salons within the community which were convenient for stylists. The focus groups were conducted in Spanish and facilitated by a bilingual psychologist. Each session lasted for approximately two hours, and was audio-taped and transcribed. Results: The focus groups marked the first step in the development of an intervention focused at addressing cardiovascular disease in the Latina population. Some of the common themes reported are as follows: o Many of the stylists expressed knowing quite a lot about cardiovascular disease (CVD), primarily due to personal experience (i.e. knowing someone with cardiovascular disease). o Stylists expressed having a “trust” relationship with their customers, often serving as “therapists or clinicians.” o Lack of insurance and economic hardships were mentioned as reasons why people do not obtain medical care o Other barriers to seeking medical care included fear of doctors, fear of finding out about an ailment, lack of trust in the medical system, immigration status, as well as some cultural fatalism of “having to die of something anyway.” Stylists mentioned that some of their customers would rather obtain home remedies and medications from their country of origin than going to the doctor. o Health related conversations are common to the salon setting o Stylists expressed importance of having referral sites for both screening and treatment, if needed o Regarding message delivery, all stylists participating in the focus groups expressed that stylists would be good health messengers, and they all stated that they would be willing to speak to their customers about heart disease. Alberto Manetta, M.D., Senior Consultant to the Vice Chancellor for Health Sciences, School of Medicine – University of California-Irvine A native of Argentina, Alberto Manetta came to this country in 1968 to begin his residency in obstetrics and gynecology. His primary research interest is in the area of cancer prevention, specifically cervical cancer. Dr. Manetta is a Gynecologic Oncologist and Professor Emeritus in the University of California, Irvine Department of Obstetrics and Gynecology, division of Gynecologic Oncology and Department of Inter-al Medicine, division of Epidemiology. He currently serves as Senior Consultant to the Vice Chancellor of Health Affairs at UC Irvine. Dr. Manetta has a strong commitment to medical education. He currently serves as Associate Dean for Diversity in the UC Irvine School of Medicine and previously served twelve years as Senior Associate Dean for Educational Affairs there. In this position, he had administrative responsibility for the education of physicians, including the educational programs leading to the MD degree, graduate medical education (residency and fellowship programs) and continuing medical education for practicing physicians. His commitment is further evidenced by his receipt of numerous teaching awards and by his development of several outstanding programs on physician training during his tenure as head of the Office of Educational Affairs. Most recently, he developed and implemented the Program in Medical Education for the Latino Community (PRIME-LC). Dr. Manetta instituted this five-year combined degree training program at UC Irvine in response to an increasing demand for physicians who are culturally sensitive and linguistically competent to address specific needs of the Latino community. The program also prepares students for leadership roles in the health care community and for academic roles that can enhance the visibility of health care issues in the Latino community. PRIME-LC is the first program of this nature in the country and has been adapted by the four other medical schools in the UC system. The inaugural group of PRIME-LC students will graduate in May 2009. Dr. Manetta has been funded by the National Institutes of Health to study means of simplifying the screening of cervical cancer in minorities. As Special Consultant to the Government of Nicaragua, he is assisting in development of a program for primary cervical cancer prevention. A desire to gain understanding of the legislative and budget process in order to more effectively help ensure access to health care and health care education to all the state’s residents led him to spend sabbatical time working in the office of California State Senator Sheila Kuehl. Dr. Manetta is actively involved with several non-profit organizations, including Latino Health Access, where he serves as chairman of the board of directors. His clinical awards include Good Housekeeping’s “Best Doctor for Women in America.” Dr. Manetta is married and has two adult children and a beautiful grandchild. He is an accomplished wood turner whose work is shown in Southern California galleries. B.3: Clinical: Hispanics and Vision Loss- The Impact of Vision Loss to the Hispanic Community Rosalio Lopez, M.D., Senior Vice-President & Chief Medical Officer, Presbyterian Intercommunity Hospital, Whittier, CA, Member – NHMA Board of Directors As Vice President of Medical Affairs, Rosalio J. Lopez, M.D., works closely with White Memorial's medical staff to continue to improve the quality of care for our patients. He is responsible for the departments of Case Management, Pharmacy, and Medical Directors and Hospital-Based Physicians. Prior to this, Dr. Lopez was the Chief Medical Officer of the Adventist Health / Southern California Medical Foundation. Dr. Lopez has also worked for AltaMed Health Services, MedPartners Inc., Pioneer Hospital and Mullikin Medical Centers. In these various roles, his contributions include pioneering, developing and implementing programs in utilization management, quality management, physician leadership development, hospital management, disease management, medical operations, strategic planning, mergers and acquisitions, regulatory compliance and financial planning. Dr. Lopez's career has progressed from clinical practice into administration, with 21 years of clinical experience and 18 years in medical executive management. He is a board certified family medicine physician, who was born in Mexico. He came to the United States when he was 16 and grew up in Boyle Heights. Dr. Lopez is the youngest of four children. His mother, brother, and sister still live in Boyle Heights. After graduating Valedictorian from Roosevelt High School, he went to Loyola Marymount University and the University of Southern California School of Medicine, on full academic scholarships. He completed his internship and residency in Family Medicine at the Sacramento Medical Center and University of California at Davis. Additionally, Dr. Lopez has a master's degree in business administration from the University of Redlands, and a degree in physician executive leadership from the Graduate School of Management at the University of California Irvine. Andrea Zaldivar, M.S., A.N.P.-B.C., C.D.E., Director, Geriatrics and Diabetes, Lighthouse International, New York Andrea Zaldivar is the Director, Geriatrics and Diabetes at the Lighthouse International. The Lighthouse International (LI) is the largest and oldest organization involved in vision rehabilitation the United States. She is also an Adult Nurse Practitioner and Certified Diabetes Educator. Her primary professional interest include understanding the issues surrounding diabetes treatment and management in high-risk populations, especially those issues involving Spanish- speaking adults with diabetes. As an educator Ms. Zaldivar has developed and implemented recognized diabetes education programs, both in Spanish and English, targeted towards patients, clinicians and the lay community. Her clinical expertise has been in treating adults with diabetes in underserved areas. Ms. Zaldivar has served on numerous local and national boards and committees, including the American Diabetes Association and the American Nurses Credentialing Committee. Ms. Zaldivar has served as committee chair for the Centers of Disease Control and Prevention’s National Latino Expert Consultant Group. She is currently a member of the Centers for Disease Control and Prevention’s National Diabetes Education’s Hispanic/ Latino work group. ABSTRACT: Vision Health: It’s impact in achieving positive diabetes outcomes –real life examples This session hopes to share real life patient stories of individuals struggling with diabetes and vision loss and how these individuals are at a severe disadvantage in achieving positive diabetes outcomes. A special emphasis will be placed on discussing how vision loss impacts the Latino community. Session participants will be provided with practical tools and strategies in assisting individuals with diabetes and vision loss, reach positive diabetes related goals. Session will use case presentation and group discussion to actively engage session participants in learning process. Bruce Rosenthal, O.D., F.A.O.O., Chief of Low Vision Clinical Practices, Lighthouse International, New York Dr. Bruce P. Rosenthal is the Chief of the Low Vision Clinical Practice at The Lighthouse International in New York City. He is a Diplomate in Low Vision, as well as being an Adjunct Professor at Mt. Sinai Hospital, a Distinguished Service Professor at SUNY, and Asst. Professor at the University of Missouri. He is the recipient of numerous prestigious awards including the Bietti Award, has been author or co-editor of 8 books on vision impairment, has written 17 chapters, and lectured extensively throughout the world. Dr. Rosenthal serves as the immediate Past-Chair of the Scientific Advisory Board of the AMD Alliance International and Low Vision Section of the American Academy of Optometry. ABSTRACT: Vision loss: A crisis in Latino communities The Lighthouse International (LI) is the largest and oldest organization involved in vision rehabilitation the United States. Through its clinical and research expertise, the Lighthouse is respected on a local and international level as being on the forefront of addressing vision health related issues. The LI has been proactive in addressing the issue of vision health disparities in Latino community by raising awareness through educating providers, legislators and patients. Results: Presentation will focus on sharing research findings targeting Latino vision health. Manuel Puig-Llano Opthalmology, Private Practice, Chula Vista, CA Dr. Manuel Puig-Llano attended Universidad Nacional Autonoma de Mexico, MD, 1969 And his residency was at UCSF, Opthalmology, 1976 and was a fellow at UCSF, Vitreous & Retina, 1978 and UCSF, Cornea, 1977. He has a Board Certification from theAmerican Board of Ophthalmology, Ophthalmology, 1981 Dr. Puig-Llano was board certified in Ophthalmology in 1981. Dr. Puig-Llano received his medical degree from Universidad Nacional Autonoma De Mexico in 1969 and served his residency specializing in Opthalmology at University of California – San Francisco. B.4: Research: Conducting Medical Research in the Hispanic Community Elizabeth Lee-Rey, M.D., M.P.H., Assistant Professor of Family and Social Medicine, Albert Einstein College of Medicine, Bronx, NY (need bio and abstract) Vivianne R. Aponte Rivera, M.D., Director of Hispanic/Latino Research Team and Clinic, Emory University, Atlanta, GA Vivianne Aponte-Rivera is the lead psychiatrist and director of a Hispanic/Latino research team and clinic. She is an assistant professor in the Department of Psychiatry and Behavioral Sciences at Emory University School of Medicine in Atlanta, Georgia. Dr. Aponte-Rivera is a child and adolescent psychiatrist and she is interested in the mental health aspects of immigration and acculturation. She is also interested in the impact of cultural differences on the manifestation of psychiatric illnesses. ABSTRACT: Clinical research with Hispanic/Latino patients: Establishing a bilingual and bicultural research team and clinic for mood disorders The effective treatment of mood disorders can be difficult to achieve. Multiple clinical research studies continue to be conducted in order to gain further knowledge about mood disorders as well as to identify effective treatments. Many of these studies focus on Caucasian and African American populations, making us wonder about the applicability of the results to other populations. In view of the growing Hispanic/Latino population in the United States, Emory University decided to establish a bilingual and bicultural research team and clinic in order to conduct clinical research on mood disorders in the Hispanic/Latino population. The development of this type of team and clinic has its unique challenges and can constitute a valuable learning experience for future research. It will provide an opportunity to further understand the manifestations of mood disorders in Hispanic/Latino patients as well as to identify ethnic differences, if any, in terms of response to treatment. Results: Emory University has established a unique partnership with Grady Health System to add Hispanic/Latino patients to their research studies on mood disorders. Emory University provides the clinical research expertise and oversight while the International Medical Center at Grady Health System is providing the cultural and linguistic knowledge. The initial phase has been the process of determining how successful clinical research projects can be replicated in Spanish and with a Hispanic/Latino population. The first aspect of this phase was the process for recruiting, hiring and training of bilingual and bicultural health personnel (including a psychiatrist, psychologist, research coordinator and rater) to form the research team. This team then proceeded to evaluate and translate the tools, documents and consent forms. The protocols and procedural information were then reviewed to make sure that they were culturally and linguistically appropriate. The next phase is the recruitment of Hispanic/Latino patients in the community. Further information about the recruitment process and some preliminary results should be available at the time of the conference. Kaney Fedovskiy, M.D., M.P.H., Medical Director of Community Outreach Services, Grady Health System, Georgia Kaney Fedovskiy is the Medical Director of Community Outreach Services at Grady Health System and an Assistant Professor in the Department of Psychiatry and Behavioral Sciences at Emory University School of Medicine. Kaney began providing needed mental health services at the International Medical Center during her fellowship in Community Psychiatry. She has published research on Intimate Partner Violence (IPV), MDD and PTSD based on research conducted at the International Medical Center. She received an American Psychiatric Association/ Pfizer Minority Research Fellowship Grant to conduct her recently- completed study on the Mental Health Sequelae of IPV among Immigrant Latino Women. ABSTRACT: Addressing Intimate Partner Violence, Mental Health Outcomes and Barriers to Health Care Access at the International Medical Center In a facilitated panel discussion, representatives of Grady’s International Medical Center (IMC) will discuss a research project characterizing the mental health sequelae of Intimate Partner Violence (IPV) among a clinic population of immigrant Latino women with a known high prevalence of IPV, Depression and Post-Traumatic Stress Disorder (PTSD). This is a collaborative, women-focused study to understand the connection between IPV, mental and sexual health outcomes, and health care access barriers among immigrant Latinas by utilizing focus groups, questionnaires and validated measures. This study furthers a dialogue about stigmatized health issues important to immigrant Latinas and intends to foster social transformation by using the study outcomes to improve mental health services at the IMC. IMC physicians directly involved in the research study and program development at the clinic will facilitate the panel discussion. The IMC team will provide a succinct overview of the study. The focus group phase of the IMC study, the development of the “Barriers to Health and Mental Health Care Access Questionnaire” for use among Immigrant Latino Women will be highlighted. We will also present the significant results of phase two of the study titled, “the Mental Health Sequelae of Intimate Partner Violence (IPV) among Immigrant Latinas”, in which the focus group- informed barriers to health care access questionnaire was added to a larger set of measures addressing history of IPV, mood and psychotic symptoms, PTSD and sexual dysfunction. The focus group and questionnaire development phase of the IMC study will demonstrate some of the challenging issues in capturing the perspectives immigrant Latinas, and translating them into culturally relevant questionnaires for use in research. Please see the following abstract. Purpose: To conduct focus groups addressing perceived barriers to health and mental health care access among Latina immigrants. To develop a questionnaire, based on focus group data, of barriers to health and mental health care access. To pilot the developed barriers to health and mental health care access questionnaire and assess relevance for its use in future studies. Results: The focus groups discussed several mutable barriers to health and mental health care access, including the cost of health care, lack of health information, lack of health insurance, communication difficulties (Language barriers with health care providers and/or interpreter unavailability), immigration/recent arrival status, work and schedule conflicts, lack of childcare, and stigma. Focus group findings and literature review resulted in the development of questionnaire items within 9 question domains. The subsequent questionnaire study showed that, even among a clinic sample of immigrant Latino women, many of the same barriers to health and mental health care access experienced by the focus group participants existed. Sergio Aguilar-Gaxiola, M.D., Ph.D. Professor of Internal Medicine, University of California-Davis, Founding Director, Center for Reducing Health Disparities, National Hispanic Science Network on Drug Abuse Steering Committee Member Sergio Aguilar-Gaxiola, M.D., Ph.D., is Professor of Internal Medicine, School of Medicine, University of California, Davis, and Founding Director of the Center for Reducing Health Disparities and the Director of Community Engagement of the UCD Clinical Translational Science Center (CTSC) at the UC Davis Health System. Dr. Aguilar-Gaxiola’s research includes crossnational comparative epidemiologic research on patterns and correlates of mental disorders and substance abuse in general population samples and the development and testing of culturally sensitive mental health diagnostic instruments. His applied research program has focused on identifying unmet mental health needs and associated risk and protective factors to better understand and meet population mental health needs and reduce mental health disparities in underserved populations. He is also very active translating mental health and substance abuse research results into practical information that is of public health value to consumers, service administrators, and policy makers. He is the Immediate Past Chair of the Board of Directors of Mental Health America, an ex-member of the National Advisory Mental Health Council (NAMHC) for the National Institute of Mental Health (NIMH), and a Steering Committee and Research Scientist member of the National Hispanic Science Network on Drug Abuse (NHSNDA). He holds several World Health Organization (WHO) advisory board and consulting positions, and is the Coordinator for Latin America and the Caribbean of the WHO World Mental Health Surveys (WMH) Consortium and a member of the International Advisory Committee of the CARSO Health Institute. He is the author of many scientific publications, and the recipient of numerous awards, including the Medal of Congress (“Medalla de la Cámara de Diputados”) of Chile, the 2002 Outstanding Latino Faculty in Higher Education Award by the American Association for Higher Education, Hispanic Caucus, and the U.S. DHHS' Office of Minority Health's 2005 National Minority Health Community Leader Award (Hispanic Community). Most recently he received the 2007 Excellence in Hispanic Mental Health Advocacy, Leadership, and Research Award from the National Resource Center for Hispanic Mental Health, the 2007 UC Davis Academic Senate Scholarly Distinguished Service Award, Davis and the 2008 Latino Mental Health Conference Excellence in Science and Research Award, in New York. He has been recognized as a distinguished member of the 100 most influential Hispanics in the United States in the October, 2006 issue of Hispanic Business Magazine and a member of the 101 top leaders in the U.S. Latino Community in 2006, 2007 and 2008 by the Latino Leaders Magazine. He was a member of the IOM/NRC Committee on Depression, Parenting Practices, and the Health Development of Young Children (2007-2009). Dr. Aguilar-Gaxiola received his M.D. degree at the School of Medicine, Autonomous University of Guadalajara in Mexico and his Ph.D. in Clinical-Community Psychology at Vanderbilt University and completed a post-doctoral fellowship in health services research at the University of California, San Francisco. ABSTRACT: Gregory A. Talavera, M.D., M.P.H., Professor and Head, Division of Health Promotion and Behavioral Sciences, San Diego, CA Dr. Talavera is a bilingual, bicultural physician trained in public health and preventive medicine. During the early part of his career he practiced ambulatory medicine in the Spanish-speaking, underserved communities of San Diego's border region. His current research interests explore the culture-specific beliefs that serve as barriers to chronic disease prevention and control. Currently he is associate professor at the Graduate School of Public Health, Division of Health Promotion and Behavioral Sciences. He is co-director of the Center for Behavioral and Community Health Studies. BREAKFAST SYMPOSIUM “Cardiometabolic Risk in Hispanics and Update” Moderator: J. Emilio Carrillo, MD, PhD, MPH, Associate Professor of Clinical Public Health and Clinical Medicine, Weill Medical College, Cornell University, President & Chief Medical Officer, NY Presbyterian Community Health Plan Dr. J. Emilio Carrillo serves as President and Chief Medical Officer of the New York-Presbyterian Community Health Plan. He is also Vice President of Community Health Development at the New York-Presbyterian Hospital. Dr. Carrillo is an Associate Professor of Clinical Public Health, and Associate Professor of Clinical Medicine at the Weill Medical College of Cornell University. Dr. Carrillo co-founded the Health Plan in 1994. He developed all of the medical management and quality improvement systems and earned several awards for excellence in quality performance. As President, he has grown the Plan more than tenfold while maintaining operational success and quality excellence. He graduated from Columbia College and received his M.D. and M.P.H. degrees from Harvard University, and subsequently trained in Internal Medicine at the Cambridge and Massachusetts General Hospitals. For ten years he served in the faculties of Harvard Medical School and Harvard School of Public Health, where he practiced and taught medicine. While there he also administered primary care programs and conducted pioneering research on infant mortality prevention, smoking prevention and cross-cultural primary care. In 1990, Dr. Carrillo was recruited through a national search to head the New York City Health and Hospitals Corporation. As the twelfth President of the nation's largest municipal hospital system, he implemented a multitude of health promotion and cultural competence initiatives, strengthened primary care services and laid the foundation for managed care readiness. Emilio was an original founder of the Boricua Health Organization. He later founded the Journal of Latin Community Health and the Journal of Multicultural Community Health and now serves on the Board of Directors of the National Hispanic Medical Association. He has published widely, received numerous awards and has been appointed as a Fellow of the New York Academy of Medicine. Dr. Carrillo has also served the Robert Wood Johnson Foundation as a Senior Fellow in Residence - Eliminating Racial and Ethnic Disparities in Health and Health Care. He currently cochairs the Steering Committee of the National Quality Forum’s project, Endorsing a Framework and Preferred Practices for Measuring and Reporting Culturally Competent Care. Eric J. Velasquez, MD, FACC, FACP, FASE, Director, Cardiac Diagnostic Unit, Division of Cardiovascular Medicine, Duke University Medical Center, Duke Clinical Research Institute, Durham, NC Dr. Eric Velasquez is currently an associate professor and serves as director of the Cardiac Diagnostic Unit and Echocardiography within the Division of Cardiovascular Medicine at Duke University Medical Center. He went to medical school at the Albert Einstein College of Medicine of Yeshiva University in New York and graduated in 1994. He held his residency in internal medicine at the Duke University Medical Center from 1995-1997. In 1999 he became a member of the intern selection committee in the department of medicine at Duke University and he continues to hold that position. He had a fellowship for cardiovascular disease in 2001 and since 2002-2006 he still is an active member or director in the following positions: Member of the performance Improvement board; Director of Phase III/IV Cardiovascular Trials Unite; Director of Heart Failure Research at Duke Heart Center. Dr. Velasquez also was involved in at least 50 selected peer-review publications regarding his clinical interests in cardiovascular imaging, the care of post-cardiac surgery patients, and the evaluation and management of heart failure especially in association with coronary artery disease, hypertension, and valvular disease. He also remains involved with an ongoing research support position regarding surgical trials in treatment of ischemic heart failure (STITCH). In addition he has completed research support on Valsartan in Acute Myocardial Infarction (VALIANT) trial and registry as well as a Percutaneous Ventricular Restoration in Heart Failure (PARACHUTE) trial. Dr. Velasquez also was a fellow twice, once within the American college of Cardiology and then within the American College of Physicians. Carlos Rodriguez, MD, MPH, FACC, Assistant Professor of Clinical medicine & Clinical Epidemiology, College of Physicians and Surgeons, Mailman School of Public Health, Division of Cardiology Columbia University, NY As assistant professor of clinical medicine - cardiology (P&S) and clinical epidemiology within the Mailman School of Public Health at Columbia University, he has been chosen as a Robert Wood Johnson Foundation (RWJF) Scholar and one of 12 nationally who were accepted into the Harold Amos Medical Faculty Development Program, an RWJF initiative to increase the number of faculty from historically disadvantaged backgrounds who achieve senior ranks in academic medicine. Dr. Rodriguez will receive $550,000 over four years for salary support and for research studies on hypertensive heart disease in Hispanics; mentoring and faculty development counsel are a part of the program. PLENARY SESSION 5 “Imaging Obesity and Addiction” Moderator: Conchita Paz, MD, NHHF Board of Directors, Las Cruces, NM Nora D. Volkow, M.D. Director, National Institute on Drug Abuse National Institutes of Health U.S. Department of Health and Human Services Nora D. Volkow, M.D., became Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health in May 2003. NIDA supports most of the world’s research on the health aspects of drug abuse and addiction. Dr. Volkow’s work has been instrumental in demonstrating that drug addiction is a disease of the human brain. As a research psychiatrist and scientist, Dr. Volkow pioneered the use of brain imaging to investigate the toxic effects of drugs and their addictive properties. Her studies have documented changes in the dopamine system affecting the actions of frontal brain regions involved with motivation, drive, and pleasure and the decline of brain dopamine function with age. She has also made important contributions to the neurobiology of obesity, ADHD, and the behavioral changes that occur with aging. Dr. Volkow was born in Mexico, attended the Modern American School, and earned her medical degree from the National University of Mexico in Mexico City, where she received the Premio Robins award for best medical student of her generation. Her psychiatric residency was at New York University, where she earned the Laughlin Fellowship Award as one of the 10 Outstanding Psychiatric Residents in the USA. Dr. Volkow spent most of her professional career at the Department of Energy’s Brookhaven National Laboratory (BNL) in Upton, New York, where she held several leadership positions including Director of Nuclear Medicine, Chairman of the Medical Department, and Associate Director for Life Sciences. In addition, Dr. Volkow was a professor in the Department of Psychiatry and Associate Dean of the Medical School at the State University of New York (SUNY)-Stony Brook. Dr. Volkow has published more than 420 peer-reviewed articles and more than 60 book chapters and non-peer reviewed manuscripts, and has also edited three books on the use of neuroimaging in studying mental and addictive disorders. During her professional career, Dr. Volkow has been the recipient of multiple awards, including her selection for membership in the Institute of Medicine in the National Academy of Sciences. She was recently named one of Time Magazine’s “Top 100 People Who Shape our World”, and was included as one of the 20 people to watch by Newsweek magazine in its “Who’s Next in 2007” feature. She was also named “Innovator of the Year” by U.S. News & World Report in 2000. PLENARY SESSION 6 “The Private Sector Perspective on Improving Workforce Diversity” Moderator: Elena V. Rios, M.D., M.S.P.H. President & CEO, National Hispanic Medical Association President, National Hispanic Health Foundation Dr. Rios serves as President & CEO of the National Hispanic Medical Association, (NHMA), representing Hispanic physicians in the United States. The mission of the organization is to improve the health of Hispanics. Dr. Rios also serves as President of NHMA’s National Hispanic Health Foundation affiliated with the Robert F. Wagner Graduate School of Public Service, New York University, to direct educational and research activities. Dr. Rios also serves on the National Hispanic Leadership Agenda, Campaign Against Obesity, and the Partnerships for Prevention Boards of Directors, the American Medical Association Commission to End Health Disparities, the PacifiCare-UnitedHealthcare California Investment Committee and is Chair, the National Coalition on Hispanic Health. Dr. Rios has lectured and published articles and has received several leadership awards, including awards from the U.S. Department of Health and Human Services, the Congressional Black, Hispanic, Asian and Native American Caucuses, American Public Health Association Latino Caucus, Association of Hispanic Health Executives, Minority Health Month, Inc., Hispanic Magazine, Verizon’s First Pollin Community Service Award, and Amerimed. Dr. Rios was appointed to the Minority Alumni Hall of Fame of Stanford University in October, 2006. She was awarded the 2008 Latino Mental Health Advocacy and Policy Award in New York in October 2008. Prior to her current positions, Dr. Rios served as the Advisor for Regional and Minority Women’s Health for the U.S. Department of Health and Human Services Office on Women’s Health from November 1994 to October 1998. In 1993, Dr. Rios was appointed to the National Health Care Reform Task Force as Coordinator of Outreach Groups for the White House. In 1992, Dr. Rios worked for the State of California Office of Statewide Health Planning and Development as a policy researcher. Dr. Rios has also served as President, Chicano/Latino Medical Association of California, Advisor to the National Network of Latin American Medical Students, member of the California Department of Health Services Cultural Competency Task Force, Stanford Alumni Association and Women’s Policy Inc. Boards of Directors, and the AMA’s Minority Affairs Consortium Steering Committee. Dr. Rios earned her BA in Human Biology/Public Administration at Stanford University in 1977, MSPH at the University of California School of Public Health in 1980, her MD at the UCLA School of Medicine in 1987, completed her Internal Medicine residency at the Santa Clara Valley Medical Center in San Jose and the White Memorial Medical Center in East Los Angeles in 1990, and her NRSA Primary Care Research Fellowship at UCLA Division of General Internal Medicine in 1992. George Thibault, M.D. President Josiah Macy, Jr. Foundation, New York, NY George E. Thibault, M.D. became the seventh president of the Josiah Macy, Jr. Foundation in January 2008. Dr. Thibault graduated summa cum laude from Georgetown University in 1965 and magna cum laude from Harvard Medical School in 1969. He completed his internship and residency in Medicine and fellowship in Cardiology at Massachusetts General Hospital (MGH). He also trained in Cardiology at the National Heart and Lung Institute in Bethesda and at Guys Hospital in London, and served as Chief Resident in Medicine at MGH. In 1977, he founded and became the first director of the Medical Practices Evaluation Unit, and was named director of the Medical ICU/CCU at the MGH. In 1978, he became the Director of the Training Program in Internal Medicine and Assistant Chief (subsequently Associate Chief) of the Department of Medicine, MGH. In 1988, he was named Chief of the Medical Services at Brockton/West Roxbury VA Medical Center and Vice Chairman of Medicine at Brigham and Women’s Hospital (BWH). In 1990, he was also named Director of Health Services Research at the Brockton/West Roxbury VA Medical Center. In 1995, Dr. Thibault was named the Chief Medical Officer at the BWH. Since January 1999, he has been Vice President of Clinical Affairs at Partners HealthCare System, Inc. He is a Professor of Medicine at Harvard Medical School (HMS). In September 2001 he was chosen as the first Director of The Academy at HMS. The Academy has been created to recognize teaching excellence and to promote curriculum innovation at HMS. In 2005, he was named the first Daniel D. Federman Professor of Medicine and Medical Education at HMS. His research has focused on the evaluation of practices and outcomes of medical intensive care units and variations in the use of cardiac technologies. In addition to an active research and clinical career, Dr. Thibault has served in many capacities at Harvard Medical School, including leadership roles in the New Pathway Project and in the current medical education reform effort. He has also served on, and has chaired, numerous committees of national organizations, including the Institute of Medicine, the Department of Veteran’s Affairs, the National Institutes of Health, and the American College of Physicians. He is past President of the Harvard Medical School Alumni Association and was recently named Director of Alumni Relations for HMS. Dr. Thibault has been the recipient of numerous awards and honors from Georgetown (Ryan Prize in Philosophy, Alumni Prize, and Cohongaroton Speaker) and Harvard (Alpha Omega Alpha, Henry Asbury Christian Award and Society of Fellows). He has been a visiting Scholar both at the Institute of Medicine and Harvard’s Kennedy School of Government and a Visiting Professor of Medicine at many medical schools in the U.S. and abroad. PLENARY SESSION 7 Lunch Plenary: “Challenges and Opportunities for Hispanic Health” Welcome to Brooklyn The Honorable Marty Markowitz, President, Brooklyn Borough, Brooklyn, NY No one works harder for all 2.5 million-plus Brooklynites than Marty Markowitz. Since entering Borough Hall in January 2002, Marty has reinvigorated the office of borough president, serving as the tireless chief advocate for Brooklyn’s economic, social, and cultural interests, while initiating and promoting efforts to improve Brooklynites’ quality of life. His goal is to ensure that all Brooklynites have the opportunity to share in the historic renaissance sweeping across the borough — and if he puts a smile on your face while he’s at it, even better! Born and raised in Crown Heights, Marty graduated from Wingate High School in 1962. He received his B.A. in Political Science after attending night school at Brooklyn College from 1962 to 1970. Marty began his career in public service in 1971, at the age of 26, by organizing the Flatbush Tenants Council, which grew into Brooklyn Housing and Family Services, the largest tenants’ advocacy organization in New York State. He is also widely known for creating two of New York City’s largest and longest-running free concert series: the Seaside Summer Concert Series in Coney Island, and the Martin Luther King Jr. Concert Series, in Flatbush. Marty was elected to the New York State Senate in 1979, where he served 11 consecutive terms representing Central Brooklyn. But he always dreamed of serving all of Brooklyn, a goal he achieved as the first borough president elected in the new millennium. He was honored to be re-elected to a second term in 2005. As borough president, in addition to setting an ambitious agenda focused on the core issues of his more than three decades in public service — housing, neighborhood preservation, and community development — Marty has enacted programs to boost civic pride, improve health, empower young Brooklynites, and generate more resources for the borough’s businesses and residents. When the NBA Nets were put up for sale in 2002, Marty saw a chance to fulfill his campaign promise of returning a national sports team to Brooklyn for the first time since the Dodgers left for Los Angeles in 1957. Marty has actively supported moving the team from New Jersey to a new Downtown arena at Atlantic Yards. The team hopes to play its first game in Brooklyn in the fall of 2009. Combined with comprehensive plans for Downtown Brooklyn’s additional development, and the burgeoning BAM Cultural District, Marty is helping to establish a vibrant new center of life for Brooklynites and all New Yorkers. With the goal of maintaining Brooklyn’s ethnic and economic diversity, he consistently seeks to maximize the amount of affordable housing for lower- and middle-income Brooklynites in every residential project that comes before him for review. More than 2,200 of the rental units planned at Atlantic Yards will be affordable housing, as will an estimated 3,000-plus of the new units resulting from the 2005 Greenpoint-Williamsburg rezoning. In addition, Marty’s own Brooklyn Housing Development Fund has helped create hundreds of affordable-housing units to date. Marty also works with Brooklyn communities to preserve their historic character and prevent outof-scale development. Sections of Park Slope, Sunset Park, Midwood, Bay Ridge, and Bensonhurst have all been down-zoned by the City Planning Commission, and similar plans are moving forward in Canarsie, Dyker Heights, Sheepshead Bay, Plum Beach, Homecrest, Greenpoint-Williamsburg, and Fort Greene-Clinton Hill. Through efforts large and small, Marty also helps create the jobs Brooklynites need. He oversaw an historic community benefits agreement for Atlantic Yards, guaranteeing that the majority of the new jobs generated by the project will go to Brooklynites who need them most, including residents of nearby public housing. He has been a tireless advocate for bringing the cruise-ship industry to Brooklyn, and in April 2006 the Queen Mary 2 will begin docking in Red Hook, followed by the Crown Princess in June, creating new jobs and introducing thousands of visitors to our great borough. Marty also chairs the Initiative for a Competitive Brooklyn, an innovative partnership to expand core economic sectors in Brooklyn, including health services, real estate and construction, the food industry, and tourism. In February of 2004 he launched the Brooklyn Tourism & Visitors Center, making Brooklyn the first borough with its own tourism center. Also in 2004, he launched the annual “Dine In Brooklyn” restaurant week, which attracts thousands of diners to the hundreds of restaurants that are fast making Brooklyn the culinary capital of America. In August 2005, a law introduced on his behalf by Council Member David Yassky to wipe out no-fault insurance “medical mills” and reduce skyhigh auto insurance rates for Brooklynites and all New Yorkers. The bill was passed unanimously by the Council and signed into law by Mayor Bloomberg in May 2006. Also in 2005, Marty became party to a lawsuit to force ExxonMobil and ChevronTexaco to clean up an oil leak under Newtown Creek that has contaminated Greenpoint for decades. In 2004, he founded the Brooklyn Center on Health Disparities, fulfilling a pledge he made with Deputy Borough President Yvonne Graham to help reduce rates of cardiovascular disease, HIV/AIDS, tuberculosis, infant mortality, asthma, and diabetes among Brooklyn’s minority communities. Marty married his wife, Jamie, in 1999. They are the proud parents of Beep, an African Grey Parrot. Dr. Maria de los Angeles Fromow Rangel Head of the Coordinating Unit of Social Participation and Entailment, Secretariat of Health Mexico, DF Dr María de los Ángeles Fromow Rangel has performed in the Mexican private and public sectors beside being active in the academic realm. She is currently Head of the Coordinating Unit of Social Participation and Entailment at the Mexican Secretariat of Health since January 2007. She read Law at UNAM (National Autonomous University of Mexico) where she graduated with Honors. She has postgraduate studies in Constitutional Law and Political Sciences at the Constitutional Studies Center at Madrid. She has a Master’s degree in Fiscal Revenue from the Financial Studies Center at Madrid, Spain, and she is Doctor in Law, Apto Cum Laude, by the Universidad Complutense of Madrid, Spain. In the private business sector she has been a corporative lawyer at Cemex, while in the public service she has been Secretary General of the Electoral Federal Court and Specialized Prosecutor for Electoral Crime (FEPADE). She has taught Administrative Law I, II and III at the Faculty of Law and Criminal Electoral Law at the National Autonomous University of Mexico (UNAM). She has given conferences and lectures in topics as International Corporative Law, Quality Systems, Electoral Justice System in Mexico, Electoral Crime, Crime Prevention, Democracy, Civic Culture, and Citizen Participation in numerous countries as Mexico, Brazil, Spain, US and the Dominican Republic. As an author she has published several articles concerning electoral and criminal issues. During her administration at FEPADE she was awarded national prizes for implementing a System of Total Quality Control. ABSTRACT Ventanillas de Salud (Health Counters) The Ventanillas de Salud (VDS), is a program financed by the Secretariat of Health and the Secretariat of Foreign Relations, and implemented by the Institute of the Mexicans Abroad (IME) through the Mexican consular network in the United States together with the partnership of health agencies, non-governmental organizations and local community groups in order to provide information to Mexican citizens living abroad about the different medical options and available health insurances in their communities of residence, to evaluate their health needs, and to prevent the most common illnesses that affect them. The VDS is not an MD providing outpatient clinic services in the consulate. The VDS objectives are: 1. Increasing the knowledge and use of public health programs. 2. Improving the health conditions and enhancing prevention mechanisms of Mexican families in the US. 3. Decreasing the use of emergency rooms by Mexican population in the US. 4. Becoming a trustable information center that provides reference and materials in health education for Mexican families in the US. 5. Educating the clients in prevention issues relevant for them. 6. Establishing a direct and effective collaboration between the Mexican consulates and private and public health institutions and agencies in the US. In 2008 alone the VDS had provided information to half-million people, by March 2009, there are 30 VDS working in the Mexican consular network across the US, and during this year the plan is to open ten more. C.1: Policy: Safety Net Providers and the Hispanic Community Angel J. Seda Comas, M.B.A., Treasurer, Puerto Rico Operations, Member – NHMA Board of Directors Georgetta Robinson Health Disparities Program Manager, Office of Clinical Standards & Quality, CMS, USDHHS, Baltimore, MD Georgetta Robinson, M.S. is currently the Health Disparities Program Manager (CMS). In her role as Health Disparities Program Manager Ms. Robinson oversees the day to day operations of the CMS Health Disparities Program. She acts as the advisors to the Director, Chief Medical Officer and Deputy Chief Medical Officer on all health disparities issues as it relates health disparities programs. Currently CMS is undergoing a sub national implementation of Diabetes Self management programs as well as building health disparities technical expert panel and the CMS health disparities forum. Ms. Robinson serves on several committees for the federal government on health disparities issues such as the 2020 Health Information Technical committee and Federal Collaborative on Health Disparities Research and the National Partnership for Action to End Health Disparities, HHS Federal Internal Management Team. She also serves on the University of Maryland Business and Technology Alumni board, The Towson University Women and Leadership Alumni council, Boys Hope Girls Hope Mentoring Baltimore Mentoring Program, The National Association of Mental Illness Public Policy program committee member and the Maryland American Medical Association Chapter Executive Steering Committee. Georgetta received a B.S. degree from University of Maryland and received her M.S. degree from Towson University. She completed a residency at Mayo Clinic in Rochester, Minnesota and subsequently served as a Fellow at Sinai Community Institute in Chicago, Illinois. Prior to assuming the Acting Budget Officer role Georgetta was the Special Assistant for Director and Deputy Director of the Office of Clinical Standards and Quality, central office. She was the recipient of the OCSQ Achievement Award, the Directors highest honor, following her first year of public service at CMS (2005) and has also been the recipient of The Quality Improvement Team Award for the U.S. Department of Health & Human Services in 2008. ABSTRACT: Improving Health Outcomes Among Diabetic Hispanic/Latino Medicare Beneficiaries Utilizing narrative approaches, a meta-analysis of published literature, and the application of logistic regression to data generated by the Medicare QIOs who are implementing the disparities prevention sub-theme, this presentation will chronicle the history of Every Diabetic Counts and, based upon the data generated, assess the impact of the DSME workshops upon Hispanics/Latinos relative to other population groups. The presentation will also explore the implications of the findings for Hispanic/Latino-serving providers. Results: CMS anticipates that during the immediate period, the knowledge levels of diabetic Hispanic/Latino Medicare beneficiaries regarding management of their disease will significantly increase (P<.05). Over the short-run, CMS expects Every Diabetic Counts to generate improved Hemoglobin A1C test scores, improved blood pressure, and cholesterol, as well as improvements in all established diabetes performance measures. Over the long run, CMS hypothesizes that the complications from diabetes in Hispanic/Latino diabetic Medicare beneficiaries will decrease. These projected results will be evaluated on an annual basis. . Wendy Jameson, M.P.H., M.P.P Director, California Health Care Safety Net Institute, Oakland, CA Wendy Jameson, MPH/MPP has served as the Director of the California Health Care Safety Net Institute since its inception in 1999. As such, she has overseen SNI’s initiatives to improve quality and enhance efficiency, eliminate health care disparities and create coordinated delivery of care at public hospitals and health systems. She also manages CAPH/SNI’s partnership with Kaiser Permanente. Prior to launching the Safety Net Institute, Ms. Jameson worked for four years as a senior health policy specialist at the California Association of Public Hospitals and Health Systems (CAPH), addressing critical policy issues associated with the expansion of Medi-Cal managed care in the 1990s. She currently serves on the National Advisory Committee to the Conferences on Quality Health Care for Diverse Populations as well as several other advisory committees. Ms. Jameson holds the degrees of MPH/MPP from UC Berkeley. Abstract: Sharon Lee Voytush, R.N., M.S., Executive Director, Beth Israel/Latino Health Institute, New York Sharon Lee Voytush, RNMS, is executive director of the Latino Health Institute at Beth Israel Medical Center in New York City. A registered nurse and health care administrator, Ms. Voytush’s areas of specialization include health care education, risk analysis, cost containment and health care delivery systems. A long-time champion of building healthier communities, Ms. Voytush was instrumental in the launch of Itzamna Medical Center in 1999, a private medical practice dedicated to improving the health of Hispanic residents in New York City. The success of Itzamna Medical Center led to the creation of Beth Israel Latino Health Institute. Earlier in her career Ms. Voytush served in senior administrative positions at Bellevue Hospital and Cabrini Medical Center in Manhattan, where she led initiatives dealing with the equitable allocation of health care resources, health policy, and recruiting and training more minority health care professionals. Ms. Voytush is currently an advisory board member of the Epilepsy Foundation, a charitable organization dedicated to helping people with epilepsy and supporting research to find a cure. She is also a member of the advisory board for the Emily N. Carey Harbor School, one of New York City’s first charter schools, which educates underprivileged children from Spanish Harlem, Harlem and the South Bronx. In addition, Ms. Voytush represents Beth Israel Medical Center in the Hispanic Federation’s Health Disparities Action Network. The Hispanic Federation is a membership organization that aims to promote the social, political and economic well-being of the Latino community. Ms. Voytush earned her B.S. in Business from Regis University in Colorado and her M.S. in Human Resource Management and Organizational Development from Chapman University in California. ABSTRACT: Health Care Reform: Is the economic crisis an opportunity to fix holes in the social safety net? As economic conditions in America continue to worsen, safety net programs are feeling the strain of increased demand while politicians in many states are cutting budgets. But a lack of equitable access to health care ultimately spells serious economic pain for the U.S. Government and business leaders need to recognize the link between healthcare and economic productivity when making policy and budget decisions. It is time for reformers to save both money and lives by changing the way health care is organized and delivered. Federal and stare policy makers, physicians, hospital administrators, medical schools and other health care providers must change the way health care is delivered and paid for. But to advance Latino health, any reform proposals must be equitable, guaranteeing health care for all people, and address health disparities C.2: Health Professions Education: Culturally Sensitive Approach to Diabetes, Chronic Renal Failure and Asthma Amparo Gonzalez, RN, BSN Director, Emory University Latino Diabetes Education Program Atlanta GA Amparo Gonzalez assumed the role of president of the American Association of Diabetes Educators (AADE) on January 1, 2008, for a one-year term. As president, she provides leadership to AADE, a multi-disciplinary organization of more than 11,000 health professionals dedicated to providing and advocating for quality diabetes self-management training. Gonzalez is currently affiliated with Emory University School of Medicine as the director of the Emory Latino Diabetes Program. Since December 2005, she has planned, designed and implemented a diabetes program conducted entirely in Spanish. By partnering with clinics in her area, the program has been administered to over 500 Latino patients. The goal of the program is to provide Latinos with up-to-date, high-quality diabetes care by eliminating barriers to understanding and providing information and instruction in patients’ native language. Gonzalez also serves as an adjunct professor at Emory University School of Nursing. An AADE Board member since 2002, Gonzalez has been an active member since 1994. She has served on many different committees: Annual Program, Finance, Strategic Planning, Personnel Practices and Bylaws/Policies and Procedures, as well as many different taskforces, including the Membership Taskforce, Diversity Taskforce, Governance Taskforce and the Environmental Scan Taskforce. In addition to her AADE activities, she has served on the Board of Directors of several different institutions including the Atlanta Diabetes University, and the National Hispanic/Latino Diabetes Federation. She is a Leadership Atlanta alumni and has also been active on many different committees of the American Diabetes Association. Reflecting her interest in diversity-related issues, Gonzalez served on the organizing committee for the First National Latino Diabetes Forum, which was held in Atlanta in September 2005. The Forum resulted in the establishment of the National Hispanic-Latino Diabetes Federation. She also serves as advisor to different organizations on topics related to healthcare disparity and Latino health issues. Gonzalez earned her Professional Nurse degree (Bachelor of Science equivalent) from the Universidad del Norte in Barranquilla, Colombia. She has been a certified diabetes educator since 1994. Ana Natale-Pereira, M.D., M.P.H., Director, Community-Based Networks, UMDNJ-New Jersey Medical School Ana Natale-Pereira, MD, MPH, is Associate Professor of Medicine with the Division of Academic Medicine, Geriatrics, and Community Programs, in the Department of Medicine at UMNDJ-New Jersey Medical School. Dr. Natale received her MD degree in 1996 from NJMA, and completed her Internal Medicine Residency at New Jersey Medical School as well. She was elected Chief Resident in 2000, and subsequently became a faculty member. In 2005, she received her Masters in Public Health in Urban health Administration from the UMDNJ-School of Public Health. She was also a junior faculty trainee of the National Hispanic/Latino Cancer Network, a fellow of the Cancer, Culture and Literacy Institute, at the H. Lee Moffitt Cancer Center in Florida, and a leadership fellow of the National Hispanic Medical Association. She is also a member of the Task Force on Cancer Prevention, Early Detection and Treatment in New Jersey in the Colorectal Cancer Workgroup, and the American Cancer Society colorectal cancer dialog for action. Dr. Natale’s research interest is in cancer health disparities and the impact of culture and health literacy on cancer prevention and chronic disease among the underserved. Her research addresses disease prevention and education about cancer and chronic diseases, increasing awareness, and improving outcomes using a community base approach for collaborative intervention; and the cultural competency of health professionals to address these issues. She is the recipient of American Cancer Society, National Cancer Institute and Centers for Medicaid and Medicare Services extramural funding to address cancer screening among Latinos and other minorities. As a result, New Jersey Medical School is one of the six sites to participate in the CMS-cancer prevention and treatment demonstration project- a multi-center national study to eliminate cancer disparities in minority populations. Dr. Natale has presented at many national meeting on topics related to cancer screening among minorities, cultural competency in cancer care, chronic illness disparities, barriers and facilitators for colorectal cancer screening, and addressing language barriers for patients with limited English proficiency, to name a few. Maria Lemus, Executive Director, Vision y Compromiso, El Cerrito, CA Maria Lemus is Executive Director of Vision y Compromiso a 501 c3 organization and its’ Network of Promotoras and Community Health Workers. Ms. Lemus enjoyed a respite from her administrative responsibilities with the California Department of Public Health while an at home mother. Her time home permitted her to hone her organizational skills as PTA president, coordinating school board elections and convening discussion groups for Latino community health outreach workers in 1998. The Network was established in 2000 with six expert Promotoras who believed in the vision of “Hacia Una Vida Digna y Sana” working toward a dignified and health life. Vision y Compromiso (Vision and Commitment) is the local, state and national voice for the practice and value of active community members, most commonly known as promotores and community health workers in the Latino community. Vision y Compromiso is a self-governing organization for and by promotoras and community health workers. As Executive Director, Maria is proud to represent the thousands of men and women who make a difference in their communities every day. ABSTRACT: Jorge Quel, MD Executive Director Hispanic American Allergy, Asthma & Immunology Association Marina del Rey, CA Dr. J.A. Quel is the Director of the Allery, Asthma, Sinus Center of Marina del Rey California and associated with Santa Monica Hospital UCLA (University of California Los Angeles), Brotman Hospital of Culver City and Marina del Rey Hospital. As an active member of various allergy societies, he lectures as well as coordinates workshops and symposiums. Dr. Quel is co-founder of the Hispanic American Allergy Asthma and Immunology Association and as its Executive Director has organized patient as well as physician education programs nationally and internationally for over 20 years. In addition, he is an active member of WHO/GARD. He also supervises the allergy training of students from Western University. As an active patient advocate, he has appeared in the State and National Capitols on legislative issues. Appointed as a member of the National Minority Quality Forum, he collaborated with the Center for Medicare and Medicaid Services on health disparities. Dr. Quel also serves on the Board of Directors and is Vice President of UNASMA (an International organization for education of allergy and asthma), and a member of the SLAAI (Sociedad Latinoamericano de Alergia, Asma e Imunologia). He is a member of the California Allergy Association, Los Angeles Allergy Association, Fellow of American Academy of Allergy Asthma and Immunology (AAAAI), Fellow of American College of Allergy Asthma and Immunology (ACAAI), among others Dr. Quel has chaired several committees including the Committee of the American College of Allergy and Asthma and Immunology (ACAAI) responsible for organizing joint sessions in Latin America. He has received many awards including Distinguished Fellow of the ACAAI as well as honorary appointments to numerous foreign allergy societies. Dr. Quel was the Director of the Allergy Department of Illinois Masonic Hospital of Chicago, Director of Allergy Research at Alpha Medical Laboratories Palos Heights Illinois, and professor at the Chicago Medical School. He also served as an appointed advisor to the Food and Drug Administration (FDA) in Washington D.C. and to the White House and was a Governor appointee to the Board of Medical Quality Assurance for the State of California. While Chair of the Aerobiology Committee of the AAAAI, he establishes a quality control system for pollen collection stations; he is a member of the Allergen Standardization Committee and is an appointed Liaison of the AAAAI. Along with lecturing nationally and internationally, Dr. Quell has written various medical articles and co authored several books including a 2008 edition on Aerobiology. He is Board Certified by the American Board of Allergy and Immunology, a conjoint board of the American Board of Internal Medicine and the American Board of Pediatrics. Dr. Quel was trained in pediatric and adult allergy-clinical immunology at several medical Universities: Ohio State University Hospital, Children’s Hospital in Columbus, Ohio, the University of Illinois, and Presbyterian St. Luke Hospital. A Post Doctoral degree in Allergy (awarded by the National Institute of Health, NIH) was obtained at the University of California Los Angeles. In addition to was trained in pediatric and adult allergy-clinical immunology at several medical Universities: Ohio State University Hospital, Children’s Hospital in Columbus, Ohio, the University of Illinois, and Presbyterian St. Luke Hospital. In addition to those institutions, Dr. Quel studied at several international Universities in South American including Argentina and Brazil. C.3: Clinical: An Interdisciplinary Approach to Creating Positive Health Outcomes Luis Aguilar, MD, Clinical Assistant Professor, Internal Medicine, University of Arizona College of Medicine, Tucson, AZ Dr. Aguilar, a product of the great Southwest, was raised in Nogales, Arizona, educated scholastically and experienced professionally in Tucson, Arizona. He has been practicing in Tucson since 1976. He holds acting staff status at Tucson Medical Center, El Dorado, Carondolet St. Joseph's and Palo Verde Hospitals.. Dr. Aguilar graduated from the University of Arizona in 1968. He attended the University of Arizona College of Medicine as a Dr. Samuel Humes Watson Medical Scholar. His residency in Internal Medicine at University of Arizona Affiliated Hospitals culminated in an additional year as instructor in Internal Medicine. His current teaching activities include preceptor for Tucson Hospitals Medical Education Program and the University of Arizona College of Medicine. In response to community needs, he participated on the Advisory Committee on the Health and Nutrition of Hispanic Communities (Hanes Study, 1979), on the Committee to develop the Catalina Foothills School District Education Foundation (1983), and its first president. He currently serves on the Board of the University of Arizona Foundation and Tucson International Mariachi Conference. He has been involved in numerous hospital based committees and medical organizations. He is currently a member of the Pima County Medical Society and The American College of Physicians. Lorena Drago, M.S., R.D., C.D.N., C.D.E., Senior Associate Director, Ambulatory Care Nutrition Programs, Lincoln Medical and Mental Health Center, New York Lorena Drago, MS, RD, CDN, CDE, is a registered dietitian, consultant and certified diabetes educator. She is Senior Associate Director of Ambulatory Care Nutrition Programs at Lincoln Hospital including: Director of the Diabetes Education Program and the Women, Infants and Children Supplemental Nutrition Program and maintains her own private practice. Lorena is a board member of the American Association of Diabetes Educators; past President of the Metropolitan New York Association of Diabetes Educators, and member of the American Diabetes Association Latino Committee. She is the author of Beyond Rice and Beans: The Caribbean Guide to Eating Well with Diabetes, published by the American Diabetes Association in October of 2006 and a contributing editor of Newsflash, a publication of the Diabetes Care and Education Specialty Practice Group of the American Dietetic Association. She is co-editor and contributing author of the book Cultural Food Practices and Diabetes soon to be published by the American Dietetic Association. Lorena, a Colombian native, graduated cum laude from Hunter College of the City University of New York with a Masters of Science degree in Food and Nutrition, and received her BA in Home Economics, Food and Nutrition from Queens College. Lorena specializes in the multicultural aspects of diabetes self-management education. She founded, Hispanic Foodways, and she developed the Nutriportion™ Measuring Cups that have the calorie andcarbohydrate amounts of common foods embossed on each cup and the Nutriportion™ Hispanic Food Cards that have pictures and nutrition composition of common Hispanic foods. Lorena is a frequent speaker at national and international diabetes conferences. This year she was an invited faculty member at the following annual conferences: Mexican Association of Diabetes Educators, Colombian Diabetes Association, American Diabetes Association, and American Association of Diabetes Educators. ABSTRACT: Nutrition Prescription for Hispanics with Diabetes: Practical Recommendations for Glycemic Control The prevalence of diabetes in the United States varies substantially by race and ethnicity. Trends show that minority populations are disproportionately affected. African-Americans, Hispanic/Latino Americans, Native Americans, some Asian Americans and other Pacific Islanders are at particularly high risk for type 2 diabetes. Culturally sensitive diabetes interventions are an effective way to overcome some of the barriers to medical nutrition therapy. To facilitate positive health outcomes, health care professionals must integrate evidenced-based nutrition recommendations into the patient’s dietary practices and food preferences. Upon diagnosis, physicians and nurses are in a unique position to make initial nutrition recommendations to patients prior to their first consultation with a registered dietitian and/or certified diabetes educator. The goals of this session are: to provide non-dietetic professionals with key nutrition counseling strategies that work in clinical practice; how to apply a cultural food practice model; and to provide valuable resources for delivering diabetes care to patients from different Hispanic subgroups. Results:Culturally appropriate nutrition interventions have resulted in improved glycemic control and other clinical and behavioral outcomes Paris Roach, M.D., Associate Professor, Clinical Medicine, Indiana University School of Medicine Dr. Paris Roach is Associate Professor of Clinical Medicine in the Division of Endocrinology at the Indiana University School of Medicine. He attended medical school and completed a residency in internal medicine at the IU School of Medicine and completed an endocrinology fellowship in the Diabetes Branch of NIDDK at the National Institutes of Health. He then worked on the clinical development of new insulin products for Eli Lilly and Company from 1995 to 2001 before joining the Division of Endocrinology at the Indiana University School of Medicine in 2001 to pursue a career in clinical care, teaching and health services research. His primary clinical interest is the application of intensive insulin therapy and his primary research interest is the development of tools to increase patients’ participation in their own care. He currently serves as the director of the endocrinology fellowship training program at the Indiana University School of Medicine. ABSTRACT: Communicating CVD Risk information to Spanish-speaking Persons with Type 2 Diabetes Using Multimedia Technology We have developed an English-language tablet computer-based multimedia presentation designed for a low-literacy audience that informs patients about their own CVD risk and facilitates dialogue between patients and providers regarding strategies to reduce risk. The 12-minute program includes simple graphic displays of patients’ own CVD risk scores and RF levels, engaging animations describing CVD, testimonials from patients who have experienced CVD events, and information about how risk can be reduced. The presentation has an accompanying audio track so that all patients can view the presentation regardless of their literacy status. One-page summaries of patient data are generated for use during the encounter. Preliminary results with English speakers, offered in the table below, suggest that the system is effective in increasing the frequency of discussion of CVD risk and risk control strategies between patients and their physicians. Adaptation of the program content for Spanish-speaking persons with T2DM has been initiated with the aim of developing a culturally relevant and meaningful content. A focus group consisting of eight Latino health care providers guided the initial program adaptation. Program content was then reviewed by a group of Latino patients with T2DM in order to qualitatively assess their understanding of the content and their perception of the suitability of the language and graphics employed. Elements reflective of Latino cultural beliefs and norms dominate the content of the presentations, and Spanish narrative with culturally appropriate syntax, culturally acceptable portrayals of health information, and testimonials by Latino patients have been included. Project Results: Results from the first 30 of 150 planned English-speaking subjects (INT: 3 PCPs/18 patients; C: 4 PCPs/12 patients) after one encounter with the INT are shown in the table. % INT Patients (n=18) 67 (12/18) 61 (11/18) 89 (16/18) 50 / 39 33 / 11 39 (7/18) 22 / 22 22 / 11 61 (11/18) 28 / 22 6 / 17 % C Patients (n=12) 25 (3/12)† 17 (2/12)* 75 (9/12) 17 / 17 25 / 25 33 (4/12) 0/0 0/8 16 (2/12)* 8/0 0/0 Discussed heart attack risk Discussed ways to lower heart attack risk Discussed ways to lower blood glucose Diet / Exercise Increase dose of / add new medication Discussed ways to lower blood pressure Diet / Exercise Increase dose of / add new medication Discussed ways to lower cholesterol Diet / Exercise Increase dose of / add new medication Discussed smoking cessation (current smokers) 75 (3/4) 25 (1/4) (*p=.025; †p=.06, Fisher’s exact test) Additionally, 15 of 16 INT subjects surveyed said the intervention made it easier to talk with their doctors. The frequency of therapeutic intensification and A1C, SBP and LDL levels are also being assessed. Maria Blanco-Castellanos, R.N., B.S.N., C.D.E., Clinical Nurse Manager, Charles Drew University-School of Medicine and Science, California Ms. Blanco-Castellanos is a clinical nurse manager at the Clinical Center for Research Excellence at Charles Drew University School of Medicine and Science. In her role as a clinical nurse manager, Ms. Castellanos is providing care for people with diabetes as an extended role-nurse, and works in collaboration with the primary care physicians at Hubert H. Humphrey Comprehensive Health Center. During the last 8 years she has worked directly with Mayer B. Davidson, MD, the center’s clinical director, to improve the health care outcomes of people with diabetes by implementing innovative programs such as the nurse-directed diabetes clinics and evaluating the effectiveness of the community health worker in the clinical setting. Additionally, she has worked with the California Diabetes Prevention and Control program as well as the National Diabetes Education Program to improve access to literacy and culturally appropriate health education for underserved populations. Her work has proven to be progressive and resulted in decreasing emergency room, urgent care and hospital admissions for people with diabetes at Hubert H. Humphrey Health Center (Diabetes Care 30:224, 2007). Ms. Castellanos is the chair of the Hispanic Latino Group in the American Association of Diabetes Educators (AADE) which is the national organization that guides and determines clinical practice for diabetes educators. She was also the recipient of a Health Care Leadership fellowship for the California Health Care Foundation Leadership Program and completed her fellowship in 2006. ABSTRACT: Primary Care Physician and Specially Trained Nurses Collaborating in Primary Care Settings to Improve Diabetes Health Care Outcomes in Latino Underserved Populations: A Model for Change The American Diabetes Association (ADA) has recommended goals of therapy that, if met, would markedly reduce diabetic complications. Unfortunately, these goals are not met in the majority of patients and outcomes remain poor. It is widely recognized that outcomes of diabetes care are even worse in minority populations. To address this situation, a carve out model of diabetes care was established in which 367 patients were treated for one year in a separate clinic by a specially trained nurse (supervised by an off site endocrinologist). The nurse (M B-C) followed detailed treatment algorithms that resulted in a mean A1C of 7.0% with 60% meeting the ADA goal of <7.0% and 82% meeting the LDL cholesterol goal in a minority population of 77% Latinos and 22% AfricanAmericans (Am J Manag Care 12:226, 2006). This model is not generalizable because there are too few endocrinologists, and importantly, patients are removed from their primary care environment leading to fragmented medical care. To see if these impressive results could be replicated on a wide scale basis and provide seamless medical care in a carve in model, the nurse, utilizing detailed treatment algorithms for hyperglycemia, dyslipidemia and hypertension, was placed in a Family Medicine Clinic and supervised by primary care physicians who referred patients to her (most likely their more challenging ones-see baseline A1C levels). *****C.4: Research: Evidence to Improve the Treatment of Hispanic HIV/AIDS Patientssupported by Gilead Sciences MODERATOR Liliana Ranon Alfredo Lopez-Yunez, M.D., Director, Alivio Medical Center, Indianapolis, IN Dr. Lopez-Yunez was a Resident Physican in Internal Medicine and Neurology from 1993 to 1997 in Chicago, IL. In 1997-1999 he was a Fellow in cerebrovascular disease at Indiana University School of Medicine. In 1999, he continued at Indiana School of Medicine as a clinical lecturer in Neurology. From 2001 to 2003, he was co-director at IU/Wishard Stroke Unit. Currently, Dr. Lopez-Yunez is a Medical Director at Alivio Clinic and Principal at Neurohealth Ltc, both in Indiana. In 1996, Dr. Lopez-Yunez was Chief Resident of the department of Neurology at Loyola University. In 2000 , he was the examiner for the American Board of Psychiatry and Neurology. In 2003, he received first place as the mentor for Annual Research paper Department of Neurology and Internal Medicine “Transcranial Doppler Evaluation of Intracranial Pressure in Fulminant Hepatic Failure” – Author: Esgi Tiryaki, MD. In 2004, he was the winner of the Junior Achievement of Indiana “Best and Brightest” in the health care category. In 2006, Dr. Lopez-Yunez received the Leader Fellowship Award-National Hispanic Medical Association. ABSTRACT: Establishing a DNA Bank for Hispanic patients with type 2 diabetes and coronary artery disease: Clinical and Research implications Prospective collection of blood samples and subsequent DNA extraction was started in September 2007. Age and gender matched control samples from healthy individuals are also collected. For all groups the following information is recorded: demographics, detailed clinical information, lipid profile, hemoglobin A1C, family history, regions of origin for three generations, social history. A stepwise testing of relevant genes in diabetes type 2 will be developed. Testing for TCF7L2 mutation is expected to be completed by January 2009. Results: The initial cohort comprises 430 patient samples, 220 diabetics and 210 healthy controls matched for age, gender and country of origin. Among diabetics, 76% have a positive family history of diabetes type 2, the majority being first-degree relatives. 34% have hypertension, 14% are smokers, 11% with coronary artery disease, 3% with history of stroke, all of which are significantly higher than in controls. Most patients are from Central and Southern Mexico (p<0.05), particularly from Oaxaca. Genetic testing for TCF7L2 expected to be completed by January 2009. Patricia E. Molina, MD, PhD Professor and Chair, Department of Physiology, LSUHSC, New Orleans, LA Dr. Molina completed her MD training at the Universidad Francisco Marroquin in Guatemala, Central America. Thereafter, she pursued a PhD in Physiology at LSUHSC under the mentorship of Dr. John J. Spitzer, presenting her dissertation on “Ethanol-endotoxin interaction with carbohydrate metabolism”. Her postdoctoral experience at Vanderbilt University was supported by a NIGMS Minority Supplement Grant under the mentorship of Dr. Naji N. Abumrad. She progressed through the academic ranks initially as an Assistant Professor of Surgery and Physiology at the State University of New York, Stony Brook and subsequently as Director of Surgical Research at North Shore University Hospital. During that period, she held a Guest Scientist appointment at Brookhaven National Laboratory prior to joining the Department of Physiology at LSUHSC as an Associate Professor. Since becoming a faculty member at LSUHSC, Dr. Molina has obtained tenure and promotion to the rank of Professor and more recently to the Richard Ashman, PhD Professor in Physiology. Dr. Molina’s research has been funded continuously since completing her PhD degree. She has mentored several undergraduate, graduate and post-doctoral trainees. Dr. Molina is a member of the faculty of the School of Graduate Studies, the Graduate Education Committee in Physiology, The Graduate Advisory Council, and is a mentor for the LSUHSC Interdisciplinary Graduate Program. Dr. Molina is an active member of several committees within the LSUHSC and is also actively involved in the Scientific Community outside the institution. Currently, she is the Vice-Chair for the National Hispanic Science Network on Drug Abuse, and Chair of the American Physiological Society Porter Development Committee. In addition, she serves a Councilor at Large for the Hispanic American Medical Association of Louisiana. Research in her laboratory focuses on the impact of alcohol and drug abuse on the cardiovascular, metabolic and immune consequences of acute traumatic injury and hemorrhagic shock. In addition, work in her laboratory also investigates the interaction of alcohol and drug abuse on the behavioral, metabolic, and immune consequences of HIV/AIDS. Currently, work in her laboratory is funded by NIAAA, NIDA, DOD, and the Board of Regents of Louisiana. Dr. Molina teaches the Endocrine Block in Medical Physiology (Spring semester) and in the Biological Systems Graduate Course (Spring semester). She is course director for Medical Spanish Elective (Spring semester), Perspectives in Alcohol and Drug Abuse Research (Spring and Fall semesters), and Graduate Endocrine Physiology (alternating Fall semesters) Yvette Calderon, MD, MS Assistant Dean, Office of Diversity Enhancement at AECOM, Jacobi Medical Center, New York As a Puerto Rican physician raised on New York City’s lower west side, I have always been strongly committed to the needs of my community and to creating solutions for the health care disparities I saw in my neighborhood. I was raised in the Chelsea projects. I received a college degree from Brown University in 1985 and a medical degree from the Albert Einstein College of Medicine (AECOM) in 1990. I completed an Emergency Medicine Residency at Jacobi Medical Center, and in my final year of training was selected as Chief Resident. Immediately following the completion of my residency in 1994, the chairman and residency director recruited me to become a full-time Emergency Medicine (EM) faculty member at Jacobi Medical Center (JMC), an inner-city public hospital where I have practiced for the past thirteen years. I was accepted by, the Hispanic Center of Excellence Faculty Development Fellowship at Albert Einstein College of Medicine and the Clinical Research Training Program (CRTP) at Einstein in order to get my Master’s in Clinical Research . I was also awarded a Research Supplement for Underrepresented Minorities (PA-01-079) from the National Institute of Child Health and Human Development (NICHD) during this time. In May of 2006, I was able to change my Master’s degree to an MS with distinction based on the publication of my thesis in the Annals of Emergency Medicine this July 2006. The focus of my thesis was on HIV counseling/ testing and prevention in the adult Emergency Department. This work was the basis of the BRIEF model that presently exists in the NBHN Emergency Departments. In addition to attaining a Master’s degree, I participated in the National Leadership Fellowship of the National Hispanic Medical Association (NHMA), an organization that promotes leadership development among Hispanic physicians. This one-year fellowship, under the supervision of faculty from the Robert Wagner School of Public Administration at New York University, provided an introduction to the information and skills needed to develop health policies on issues relevant to the health of Hispanic communities. The fellowship provided valuable experience in how clinical research can be translated into meaningful policy but did not provide the opportunity to enhance my research skills. In April, 2007 I received a K23 award from the National Institute of Child Health and Human Development (NICHD) to continue training and conducting HIV Prevention studies engaging adolescent and young adults. In 2007, she received a CDC sponsored Grant for HIV Rapid Testing in Clinical Facilities which has allowed her to expand HIV testing services to an additional ED and in-services areas with in two hospitals. All of my clinical research has been presented at the annual SAEM meetings throughout my career. The Centers for Disease Control and Prevention (CDC) has invited me to present all HIV related clinical research conducted at Jacobi at a forum, where the CDC was considering revisions to its guidelines for HIV testing. In addition, I have been invited to present at the Worlds Aids Day, China 2006, IAS, Australia 2007, and IAS Mexico 2008. I presented the evaluation of the rapid HIV testing program, BRIEF, at the National HIV Conference sponsored by the CDC in December 2007. D.1: Policy: The Current State of the American Health Care Reform Debate Luis Estevez, MD, MPH, MBA Founder and Principal Empire Blue Cross Blue Shield, Yorktown Hts, NY Dr. Luis Estevez is a graduate of the Mt. Sinai School of Medicine. He completed his residency training at the Montefiore Hospital Residency Program in Social Medicine, and subsequently received a Masters in Public Health from New York Medical College. He is Board Certified in Preventive Medicine and Public Health and Quality Management. Last year completed his studies at the University of South Florida where he earned a Masters in Business Administration. Dr. Estevez has served as a Medical Director of several organizations for the past thirteen years. His clinical leadership included health centers and HMOs, such as the Metro Plus Health Plan and the Morrisania Health Center where he provided clinical leadership for those organizations. His responsibilities included Quality Improvement, supervision of Clinical Department Chiefs, Grants Management, Strategic Planning, Program Planning and Development, Health Data Analysis and Medical Policy Development. He has also held several academic positions in New York, and served as a member of the Admission Committee of New York Medical College. He is a founding Board member and currently serves as Vice President of The National Hispanic Medical Association. In addition, he helped to establish the Boricua Health Organization, (now BLHO) and remains active in Latino health issues. He was a member of the White House Task Force on Health Care Reform, a Senior Health Policy Fellow with The National Association of Public Hospitals, and has testified before three Congressional Subcommittees on community health and child health issues. Currently Dr. Estevez is the Founder and Principal for Empire Blue Cross Blue Shield in Yorktown Heights, New York. John Ruffin, PhD. Director, National Center for Minority Health & Disparities, USDHHS, Rockville, MD, invited Dr. John Ruffin is the Director of the National Center on Minority Health and Health Disparities. He is a well-respected leader and visionary in the field of health disparities. He has devoted his professional life to improving the health status of minority populations in the United States and to developing and supporting educational programs for minority researchers and health care practitioners. His success has been due in large part to his ability to motivate others and gain the support of key individuals and organizations, as well as to his expertise in strategic planning, administration, and the development of numerous collaborative partnerships. For over 15 years, he has led the transformation of the NIH minority health and health disparities research agenda from a programmatic concept to an institutional reality. He has served as the Associate Director for Minority Programs, Office of Minority Programs; and the Associate Director for Research on Minority Health, Office of Research on Minority Health. His life-long commitment to academic excellence, improving minority health and promoting training and health disparities research, has earned him distinguished national awards. In January 2007, he received the Martin Luther King Legacy Award. Abstract: Robert Kolodner, MD, Director, Office of National Coordinator, USDHHS, Washington, DC On September 20, 2006 Robert M. Kolodner, MD joined HHS as the Interim National Coordinator for Health Information Technology (IT). He takes the lead at a time when HHS is making steady progress in advancing the President’s Health IT initiative, and his experience in patient care, health IT, and government is invaluable to those efforts. Dr. Kolodner comes from the Veterans Health Administration in the Department of Veterans Affairs (VA), where he has been serving as Chief Health Informatics Officer and has been involved with the development and oversight of VistA VA’s electronic health records systems and My HealtheVet - VA’s Personal Health Record for veterans. Dr. Kolodner’s long-standing interest in computers led to his early involvement with VA’s efforts to use automation in support of mental health care. He was a key clinical leader for the Decentralized Hospital Computer Program, VA’s healthcare information system starting in 1983 as chair of the Mental Health Special Interest Users Group, in 1989 as co-chair of the interdisciplinary Clinical Record Special Interest Users group, and in 1991 as chair of the Clinical Application Requirements Group. In 1993, Dr. Kolodner moved to Washington, DC into a health IT management position as the Director of the Medical Information Resources Management Office, leading all health automation activities in VA. In 1996 Dr. Kolodner was selected as Associate Chief Information Officer for Enterprise Strategy in the newly created Office of Information in the Veterans Health Administration. Since 1997 Dr. Kolodner has been actively involved in overseeing, promoting, and guiding VA activities related to the establishment of a life-long, comprehensive, computerized clinical record for military personnel and our nation’s veterans. He fostered the idea for the creation of My HealtheVet - a health portal for veterans and their families to access health information, tools and services via the Internet. He was also instrumental in establishing the Federal Health Information Exchange program - an interagency health technology initiative that supports improving care to veterans - and strengthening the working relationship between VA and the Department of Defense. Dr. Kolodner received his undergraduate degree from Harvard College and his medical degree from Yale University School of Medicine. He completed a clinical fellowship in Medicine at Harvard University School of Medicine and his Psychiatric residency at Washington University School of Medicine. Dr. Kolodner has medical specialty board certification in psychiatry. He is a member of numerous professional societies, task forces and editorial boards. He has authored and co-authored articles, book chapters and books in medical and medical informatics literature and has lectured on medical informatics throughout the United States. Peter Colby Amadio, M.D., Mayo Clinic Health Policy Center, Mayo Clinic, Rochester, MN Peter Amadio is a orthopaedic surgeon practicing at the Mayo Clinic in Rochester, MN, where he holds the academic rank of Professor in both Orthpaedic Surgery and Biomedical Engineering, and is Vice Chair for Research in the Department of Orthopaedic Surgery. In addition to work as a clinician and an NIH-funded investigator, he has had a longstanding interest in health policy and health disparities, and has worked to address both interests at Mayo Clinic and in national organizations. In addition to Mayo’s Health Policy Center, he is a member of the J Robert Gladden Society, a multicultural organization of orthopaedic surgeons, dedicated to increasing diversity an cultural competence in musculoskeletal care, and has served in the past on Mayo’s Transcultural Patient Care Committee. He is a past President of the Minnesota Medical Association, has chaired evidence based medicine committees for the American Academy of Orthopaedic Surgeons and the American Society for Surgery of the Hand, and is currently a member of the AMA Group Practice Advisory Council. Dr. Amadio was born in Pennsylvania, grew up in New Jersey, and during his professional education lived in New York, Massachusetts, and Virginia. He has spent the past 25 years in Minnesota, but still thinks that the winters are too long. He enjoys traveling, the arts (particularly theater) and spending time with his family. He once served as the campaign manager for a state legislator (she lost), which he considers to have been “interesting”. ABSTRACT: Cornerstones for Health Care in America The discussion will begin with a description of the Mayo Clinic Health Policy Center (HPC) and its work in health care reform to date. The goal of the HPC- a non profit, nonpartisan effort- is to influence stakeholders to implement substantive health care reform before 2011 that will preserve quality and availability to health care for all patients. Since 2006, through the active engagement of more than 2000 diverse stakeholders, including providers, employers, insurers, elected officials and –most importantly- patients, the Mayo Clinic Health Policy Center has developed four cornerstone recommendations for health care reform: 1. Create Value (Defined as Quality/Cost): Improve patient health outcomes and satisfaction with U.S. health care. Decrease medical errors, costs and waste. 2. Coordinate Care: Coordinate patient care services across people, functions, activities, locations and time to increase value. Ensure patients are active participants in this process. 3. Reform the Payment System to Pay for Value: Change the way providers are paid in order to improve health and minimize waste. 4. Provide Health Insurance for All Americans: Provide guaranteed, portable health insurance for all citizens, giving them choice, control and peace of mind. The discussion will also include thoughts on the current direction on Health Care Reform at the national level. Paul Cotton Senior Legislative Representative AARP Washington, DC Paul Cotton is a Senior Legislative Representative at AARP, lobbying Congress and the Administration on Medicare, Medicaid, and health care quality issues. He previously served as Director of Hearings and Policy Presentation at the Centers for Medicare and Medicaid Services Office of Legislation. He also worked for several years as a reporter for publications including the Journal of the American Medical Association. D.2: Health Professions Education: Advancing Women’s Health in the Hispanic Communitysupported by Wyeth Pharmaceuticals Nereida Correa, M.D., Private Practice, OB-GYN, Brooklyn, NY Nereida Correa is Medical Director of the MIC Women’s Health Services of the Medical and Health Research Association of New York. She is an obstetrician/gynecologist, a family physician and is also Education Core Director of the Bronx Center to Reduce and Eliminate Ethnic and Racial Disparities in Health at the Albert Einstein College of Medicine. She is a former Director and current member of the core faculty of the first Hispanic Center of Excellence in New York State at the Albert Einstein College of Medicine and of the first group of Hispanic Leadership Fellows of the National Hispanic Medical Association. She also serves as editor of the Caring for Hispanic Patients Journal of the National Hispanic Medical Association and of the American Academy of Family Physicians. Dr. Correa has an active clinical practice in obstetrics, gynecology and women’s health. In her role as clinician and founder of the OB/GYN 2000, she has been involved in caring for a largely Hispanic population in the Bronx and Washington Heights. She was born in Puerto Rico and grew up in New York City where she worked as a registered nurse prior to attending the Albert Einstein College of Medicine. She received a Masters in Public Health from Columbia University in the fall of 2005. Dr. Correa is a strong advocate for elimination of disparities in access to health care and for issues concerning women and their families. She has served as a member of the National Advisory Council for Maternal, Infant and Fetal Nutrition and is on the Advisory Council of Bright Futures for Women of the Division of Women’s Health of the Health and Human Services Administration. She has been active in advocacy groups in Albany and Washington DC and in the past several years has been working to promote cultural and linguistic competency in medical school and residency curricula. She is an Associate Clinical Professor in the Department of Family and Social Medicine and she participates in teaching of resident and medical students, particularly in the areas of cultural and linguistic competence. She is on the Leadership Commission of the New York State Academy of Family Physicians, President of the Bronx Gynecological and Obstetrical Society and a Fellow of the American College of Obstetrics and Gynecology. She was chosen as a Health and Human Services Primary Health Care Policy Fellow in 2004, was included in the Women in Medicine Exhibit of the National Institutes of Health Library of Medicine Exhibit, and was honored by El Diario/La Prensa as one of Fifty Hispanic Women selected in 2003. Joaquin Santolaya, M.D., Ph.D., Director of Genetics, Department of Obstetrics and Gynecology, Harvard Medical School Joaquin Santolaya, M.D., Ph.D., is currently the director for Fetal Medicine and Prenatal Genetics at Brigham and Women’s Hospital. From 1994 to 1999, Dr. Santolaya was an Associate Professor and Director of Reproductive Genetics and Fetal Medicine at the University of Illinois in Chicago. In 2000, Dr. Santolaya was the Professor and Director of Reproductive Genetics, Fetal Medicine and Ultrasound at Texas Tech University. Along with this position he was also the Executive Director of Amarillo Women’s Health Research Institute in Texas. In 2004, he was the Professor of Obstetrics and Gynecology at Wayne State University and Professor of Perinatology Research Branch at NICHD/NIH/DHHS. ABSTRACT: Genetics and Reproductive Options for Hispanic communities: Current Trends and Future Up to 4% of newborn infants of all cultural backgrounds suffer from a congenital defect and many of these can be diagnosed prior to birth. Moreover, the number of genetic disorders and genetic mutations with potential to cause diseases that can be detected prenatally are also increasing every year. For these two reasons, it is important to bring forward to our Hispanic communities the existence of reproductive genetic programs that include the pre-conceptional, pre-implantation and pre-natal periods. For these universal reproductive genetic programs to be efficacious it is important to develop a clinical culture that is culturally inclusive and avoids language and communication barriers. Our aims with this presentation are to discuss reproductive genetic programs in the context of: 1) their structure and function, 2) their efficiency and efficacy and, 3) the alternative options available to women seeking to form a family. In addition, we intend to present data contributed by Hispanic researchers aimed at developing novel therapeutic options to prevent catastrophic diseases of childhood. Sandra Estepa, M.S.W., Women’s Health Coordinator, Region II, U.S.D.H.H.S. Ms. Estepa has extensive experience in health care planning and administration in a variety of settings. As the Regional Women's Health Coordinator, Ms. Estepa works with federal, state, and local departments of health, community-based organizations, and professional associations in HHS Region II (consisting of New York, New Jersey, the Commonwealth of Puerto Rico, and the Territory of the Virgin Islands) to stimulate and support women's health initiatives across the life cycles. Ms. Estepa serves as an expert on a broad range of women’s health concerns, such as HIV/AIDS, intimate partner violence, and mental health and trauma issues, particularly for underserved and minority women. She has served as Program Policy Analyst in the Office for Women's Health at the New York City Health and Hospitals Corporation, as Program Officer covering the areas of health care services and services to people with disabilities at the New York Community Trust, and was the Founding Executive Director of the Latino Commission on AIDS, an AIDS advocacy organization in New York City. She has a Master's degree in Social Work from Columbia University and a Bachelor's degree in Social Work from the Catholic University of Puerto Rico. Laura M. Newberry, M.A., Manager, Health Policy, Abbott Nutrition, Columbus, OH Laura Newberry is Manager, Health Policy at Abbott Nutrition based in Columbus, Ohio. In this role, Laura is responsible for understanding breastfeeding advocacy in the U.S. and managing breastfeeding education and support programs for mothers, families, legislators, and healthcare professionals in both English and Spanish. Laura joined Abbott Nutrition in January 2007 from Claremont Graduate University, where she was a graduate student in women’s studies, and India and Pakistan, where she researched women ascetics and feminism. Laura earned her bachelor’s degree in Spanish and Classical Studies at The College of Wooster (OH) and her MA in Women’s Studies in Religion from Claremont Graduate University (CA). She also studied at the Universidad de Córdoba, in Córdoba, Spain. She speaks English, Spanish, and a little Hindi/Urdu. She was raised in Boulder, Colorado and now lives in Columbus, OH with her partner, David, daughter named Dyln, and two wily dogs Jules and Vincent. ABSTRACT: Nutrition and Women: Workplace Lactation Programs and other Hispanic initiatives Workplace Lactation Programs: Good for Working Families. Good for Business. TM, available on the Corporate Voices for Working Families website at www.cvworkingfamilies.org, is designed to help front-line managers implement lactation programs and educate hourly and lower-wage employees on how they can make a choice in infant nutrition. Material contained in the toolkit is available in both English and Spanish. The workplace lactation program will be distributed throughout the business community and to healthcare organizations, community groups and government agencies. The Workplace Lactation toolkit was developed in consultation with a select group of member companies and healthcare professionals, including: Ceridian; CVS Caremark; IBM Corporation; ICF International, Inc.; Knowledge Learning Corporation; LifeCare; Marriott International, Inc.; Metropolitan Life Insurance Company; PNC Financial Services Group, Inc.; and The TJX Companies, Inc. Results: Breastfeeding is the gold standard for infant nutrition but for many lower wage moms returning to work is a barrier to extended breastfeeding. As a leader in infant nutrition, Abbott's goal is to ensure optimal nutrition for infants, whether mothers choose breastfeeding, infant formula or a combination of both. Abbott has a long history of supporting healthcare professionals and parents with breastfeeding education materials and programs. D.3: Clinical: Addressing Children and Health in the Latino Community Onelia Lage, MD Associate Professor of Clinical Pediatrics and Director of Adolescent Medical Education and Community Health, Division of Adolescent Medicine/Department of Pediatrics at University of Miami Miller School of Medicine Onelia G. Lage M.D. is Associate Professor of Clinical Pediatrics and Director of Adolescent Medical Education and Community Health in the Division of Adolescent Medine/Department of Pediatrics at the University of Miami Miller School of Medicine (UMMSOM). She was appointed by Governor Charlie Crist to the Florida Board of Medicine and was elected Vice-Chair for 2009. She is the first Hispanic woman/pediatrician to serve in this distinguished position. She is also a member of the Minority Women Health Panel of Experts of the Office of Women’s Health/U.S. Health and Human Services. Dr. Lage completed her Pediatric training at Metropolitan Hospital Center’s New York Medical College Program and her fellowship in Adolescent Medicine at the UMMSOM/Jackson Memorial Hospital. She received her medical degree from Universidad Central del Este, D.R (graduate of honor commendation) and A.A. degree from Miami-Dade College with highest honors and distinction. She was board certified in Pediatrics in 1993 and is recertified in Adolescent Medicine (2008). Dr. Lage has been a member of the National Hispanic Medical Association since its inception in 1994. She has served on its national advisory board and membership committees and was selected as a Leadership Fellow in 2004. She has represented the NHMA on the National Coalition for Adolescent Health, AMA Adolescent Health Disparities Workgroup, NAACP, Robert Wood Johnson Childhood Obesity Summit and multiple other events. She has held numerous leadership positions including President of the Greater Miami Pediatric Society, University of Miami Medical Group Leadership Council and UMMSOM Institute for Women’s Health Leadership Team and UM Faculty Council. She has been actively involved in the education and training of medical students particularly minority students and pediatric residents and is Faculty advisor for the Hispanic American Medical Student Association at UMMSOM. She serves on the UMMSOM admissions committee and the Jackson Health Systems pediatric residency recruitment committee. Dr. Lage’s federally funded research has centered around minority adolescents and young adults particularly pregnancy prevention in adolescents with chronic illnesses such as asthma, diabetes, sickle cell and HIV and mental health issues in at risk youth. She has presented research nationally and has multiple abstracts/publications. She received the Miami-Dade County Volunteer Physician of the Year Award for her service at a faith based clinic with undocumented Hispanic immigrants and has been selected as Super Doctor and Top Doctors’ in Florida as well as Florida’s leading women in Medicine. Dr. Lage’s greatest accomplishment and fulfillment stems from her family with husband Eugenio of 28 years, son Daniel a Harvard sophomore and daughter Adrianne a freshman at Lourdes Academy. Her passion lies in helping minority young women especially Latinas achieve their ultimate potential in body, mind and spirit. Donna Mendez, M.D., Associate Professor, Pediatrics/Section of Emergency Medicine, Baylor College of Medicine I am an Associate Professor of Pediatrics/Section of Emergency Medicine at Baylor College of Medicine in Houston, Texas. I went to medical school at UTMB in Galveston, Texas, residency at UTHSC in San Antonio, Texas and Pediatric Emergency Medicine Fellowship at UT Southwestern in Dallas, Texas. I have an interest in traumatic brain injury which dates back when I was involved in neuroscience research under a NIH summer program while in medical school. I have published several papers in basic science as well as clinical medicine on the topic of traumatic brain injury. I currently am a collaborator on two NIH grants investigating the neuropsychological outcomes in children with traumatic brain injury. Nora Esteban-Crusciani, MD, MS Assistant Director, Division of Pediatric Hospital Medicine, Children’s Hospital at Montefiore, New York Nora Esteban, MD, MS is currently Associate Professor of Clinical Pediatrics at the Albert Einstein College of Medicine (Einstein) and Assistant Director of the Pediatric Hospital Medicine Division at the Children’s Hospital at Montefiore (CHAM), Bronx, NY; formerly Director of Clinical Services of the CHAM / Children’s Aid Society Outreach Program. She obtained her medical degree from the School of Medicine, University of Buenos Aires, Argentina, in 1980 and completed her pediatric training both at the Italian Hospital (Buenos Aires, Argentina) and at the Department of Pediatrics, Einstein/Montefiore Medical Center (Bronx, NY). She received research training at the National Institute of Child Health and Human Development, NIH, Bethesda, MD, and obtained a Masters degree on Clinical Research Methodology (M.S.) from the Albert Einstein College of Medicine, supported by Einstein’s HCOE. Dr. Esteban is Board Certified in Pediatrics and an active member of the American Academy of Pediatrics, the Academic Pediatric Association, and the Society of Hospital Medicine. She has been recognized as a “New York’s Top Doctor in Pediatrics” by Castle Connolly, and one of “America’s Top Pediatricians” by the Consumers’ Research Council of America. She received the 2006 Einstein’s Hispanic Center of Excellence Nora Esteban, MD, MS is currently Associate Professor of Clinical Pediatrics at the Albert Einstein College of Medicine (Einstein) and Assistant Director of the Pediatric Hospital Medicine Division at the Children’s Hospital at Montefiore (CHAM), Bronx, NY; formerly Director of Clinical Services of the CHAM / Children’s Aid Society Outreach Program. Dr. Esteban is currently involved in building a NYC Pediatric Hospital Medicine Consortium to promote interdisciplinary collaboration and excellence in medical care among NYC hospitals. She is an NHMA Fellow Alumni. ABSTRACT The Latino population has become the largest minority group in the Bronx. Language differences affect patient safety, trust and satisfaction, and contribute to healthcare disparities for limited English proficiency (LEP) Latinos. We describe the process towards overcoming language barriers at an inner-city academic children’s hospital in the Bronx, while simultaneously achieving academic excellence Project Summary/Methodology: Setting: Children’s Hospital at Montefiore/Albert Einstein College of Medicine. Design: Demonstration project; retrospective analysis (n=126). Outcome measures: Press Ganey post-discharge survey scores (58 questions, covering 13 domains). We compared Latino parents’ satisfaction and perception of language barriers during hospitalization before and after implementation of: 1) a weekly interdisciplinary leadership team meeting (CHAMSTAT) focusing on patient satisfaction; 2) a Pediatric Hospital Medicine program devoted to optimizing interdisciplinary communication and providing excellence in medical care. We focused on changing our own culture using resources already in place, including translated material. Project Results: In-patient satisfaction among Latino families rose in all domains (e.g. language: from 1-32% to 99%ile), achieving an overall 99%ile in 2008 (P<0.01). Our intervention focused on more effective utilization of resources already available, and did not require budgetary changes or additional hospital expenses. Length of stay for several common pediatric diagnoses decreased significantly (P<0.05), while in-patient census increase, as well as hospital revenues (30% within Pediatric Hospital Medicine). In addition, the Children’s Hospital at Montefiore received national recognition by: 1) the US News and World Report: listed among Best Pediatric Hospitals in USA; and 2) Press Ganey Success Story Award, for significant improvements in patient satisfaction.l D.4: Research: Chronic Disease Disparities in the Hispanic Community Ana Natale-Pereira, M.D., M.P.H., Associate Professor of Medicine with the Division of Academic Medicine, Geriatrics, and Community Programs UMDNJ-New Jersey Medical School Ana Natale-Pereira, MD, MPH, is Associate Professor of Medicine with the Division ofAcademic Medicine, Geriatrics, and Community Programs, in the Department of Medicine at UMNDJ-New Jersey Medical School. Dr. Natale received her MD degree in 1996 from NJMA, and completed her Internal Medicine Residency at New Jersey Medical School as well. She was elected Chief Resident in 2000, and subsequently became a faculty member. In 2005, she received her Masters in Public Health in Urban health Administration from the UMDNJ-School of Public Health. She was also a junior faculty trainee of the National Hispanic/Latino Cancer Network, a fellow of the Cancer, Culture and Literacy Institute, at the H. Lee Moffitt Cancer Center in Florida, and a leadership fellow of the National Hispanic Medical Association. She is also a member of the Task Force on Cancer Prevention, Early Detection and Treatment in New Jersey in the Colorectal Cancer Workgroup, and the American Cancer Society colorectal cancer dialog for action. Dr. Natale’s research interest is in cancer health disparities and the impact of culture and health literacy on cancer prevention and chronic disease among the underserved. Her research addresses disease prevention and education about cancer and chronic diseases, increasing awareness, and improving outcomes using a community base approach for collaborative intervention; and the cultural competency of health professionals to address these issues. \ She is the recipient of American Cancer Society, National Cancer Institute and Centers for Medicaid and Medicare Services extramural funding to address cancer screening among Latinos and other minorities. As a result, New Jersey Medical School is one of the six sites to participate in the CMS-cancer prevention and treatment demonstration project- a multi-center national study to eliminate cancer disparities in minority populations. Dr. Natale has presented at many national meeting on topics related to cancer screening among minorities, cultural competency in cancer care, chronic illness disparities, barriers and facilitators for colorectal cancer screening, and addressing language barriers for patients with limited English proficiency, to name a few. ABSTRACT: Navigating Latino Seniors to improve Cancer Disparities: Lessons learned from the CMS-Cancer Prevention and Treatment Demonstration Project. The overall aim of this project is to institute an innovative cancer care facilitation program for elderly Latinos in the city of Newark, NJ, to reduce cancer health disparities, by utilizing a multidisciplinary team approach to health care. The team will use the Multilevel Approach to Community Health (MATCH) planning model, integrating community outreach, education, access to screening, and patient assistance program using Community Health Workers (CHWs) and Patient Navigators (PN) to help Latino seniors navigate the health care system and facilitate screening, diagnosis and treatment of breast, cervical, colorectal, and prostate cancer. Participants will be invited to participate if they meet eligibility criteria set up by CMS ( Latinos, Medicare fee for service Part A and B recipients, age 40 or over, not participating in an HMO, not institutionalized). After eligibility is confirmed, and informed consent is administered and signed, the participants are asked to complete s two baseline surveys, and receive a $ 20 supermarket shopping card for their time and effort. Once the survey is completed, the participants are randomized (by CMS) to a control (education only) group or an intervention (navigation) group. Those in the intervention group are closely followed by the Patient Navigators, who begins to work with the participants to educate them about cancer screening and cancer prevention, and to help them complete their screening tests if these are not done. For those seniors who do not have a regular source of care, the team will assist in finding a doctor for this person. The effort is to recruit a total of 1384 participants over a three year period. Luis R. Castellanos, M.D., M.P.P., Fellow-Cardiovascular Medicine, University of California-Davis Medical Center Dr. Luis R. Castellanos is a recent graduate of the Commonwealth Fund/Harvard University Fellowship in Minority Health Policy. He received his training from the Harvard School of Public Health and specifically studied how to effectively utilize existing data collection instruments and datasets in order to identify, monitor, and develop strategies to eliminate racial and ethnic disparities in cardiovascular care. During his academic training, Dr. Castellanos has been involved in several independent research projects in cardiovascular medicine and has co-authored articles for the American Journal of Cardiology and the Journal of Cardiac Failure. Dr. Castellanos is finishing a fellowship in cardiovascular medicine at the University of California, Davis Medical Center, Sacramento, CA and plans to practice academic medicine and further advance medical science by formulating strategies geared towards studying and reducing cardiovascular risk factors in underserved populations, with special attention to the Latino community. From a health policy stand point, Dr. Castellanos has worked with the California Chapter of the American College of Cardiology and the American Heart Association in order to discuss health related legislation with state congressional representatives and senators. His community service efforts also include previous volunteer work with local middle and high schools in underserved areas. Dr. Castellanos received his medical degree from Harvard Medical School and completed an Internal Medicine residency from the University of California, San Diego Medical Center. ABSTRACT: Cardiac Quality Reporting Programs: Hispanics are More Likely to be Operated on by Cardiac Surgeons with Lower Quality Performance Scores Under state legislative mandates, California and Massachusetts-licensed hospitals providing cardiac surgery are required to report all isolated CABG to the California CABG Outcomes Reporting Program (CCORP) and Massachusetts Data Analysis Center (Mass-DAC). We analyzed clinical data from CCORP and Mass-DAC on all pts receiving isolated CABG during 2002-2004 by surgeons who performed ≥10 operations throughout this period. Surgeons were divided into four operative mortality performance groups based on their risk-adjusted operative mortality rates: top decile, top quartile, lowest quartile and lowest decile. The proportions of Hispanic and White patients in each quality performance group were analyzed. Results: In California, a total of 40,233 isolated CABG were performed by 276 surgeons. The cohort included 28,175 Whites (70%), 4,879 Hispanics (12%), 3,550 Asians (9%), and 1,480 Blacks (3.7%). The overall surgeons’ operative mortality rates for these ethnic groups were not significantly different (p>0.05) compared to the state average of 3.08%. Compared with Whites, Hispanic patients were 49% less likely to be treated by surgeons in the highest quality performance group, OR 0.51, 95% CI (0.35-0.75). In addition, Hispanics were the only subgroup that was more likely to be operated on by surgeons in the lowest quality performance group. Hispanics were almost three times more likely to be treated by surgeons in the lowest quality performance group when compared to the highest quality group, OR 2.85, 95% CI (1.82-4.47), pvalue <0.0001. By contrast, White patients were almost twice as likely to receive CABG from surgeons in the highest quality performance group than by surgeons in the lowest quality group (OR 1.75, 95% CI 1.52-2.02). Marjaneh Fooladi, Ph.D., F.N.P., Specialty Program Director, University of Texas, El Paso Dr. Fooladi received her Masters of Nursing Science, Women’s Health Care Nurse Practitioner a the University of Texas, El Paso. In 1996, she received her Post Masters of Science in Family Nurse Practitioner (FNP) at Texas-Tech University. She then received her Doctor of Philosophy at the University of Southern Mississippi, Hattiesburg. Dr. Fooladi was a Senior Nursing Consultant at the School of Nursing in Karachi, Pakistan in 2004. The main purpose was to develop the advanced practice program at the Aga Khan University. Dr. Fooladi is currently a Specialty Program Director at the University of Texas, El Paso. ABSTRACT: The Prevalence of Periodontal Disease among Pregnant Hispanic Women of Mexican Origin in El Paso, Texas We hypothesized the lower rate of low birth weight, preterm birth, and infant mortality among pregnant women of MO may (in part) be explained by the lower prevalence of periodontal disease before and during pregnancy. Our method was A prospective cohort study to: 1) Standardize eligibility criteria (reduce bias), 2) Standardize outcome assessments (reduce misclassification and identify bias), 3) Adequately assess for causative relationship between periodontal disease and adverse pregnancy outcomes. Inclusion Criteria: Pregnant women of MO Pregnant and over the age of 18 Gestational age < 20 wks No less than 20 teeth Exclusion Criteria: Pre pregnancy Hypertension < 20 wks gestation Pre pregnancy Diabetes: Type I & II Probing contraindications, e.g. : Heart disease HIV positive Project Results: This feasibility study identified the prevalence estimates of periodontal disease among the pregnant women of MO living in El Paso, Texas Our findings were similar to the prevalence of periodontal disease in United States, Mexico, and Canada Evelyn Montalvo Stanton, M.D., Assistant Professor of Pediatrics, Pediatric Pulmonology, UMDNJ-New Jersey Medical School Dr. Evelyn Montalvo Stanton is a Board Certified Pediatric Pulmonologist and Assistant Professor of Pediatrics who graduated from UMDNJ-New Jersey Medical School and completed her Pediatric Residency in 1988. She was also chief resident the following year. She completed her Pediatric Pulmonology fellowship at Columbia Presbyterian Babies Hospital. After completion of her fellowship, she practiced for the Atlantic Health System-Morristown Memorial Hospital, Respiratory Center for Children until 2004 and return back to UMDNJ-New Jersey Medical School that year. She was one of the Board of Directors for the New Jersey American Lung Association, and currently is an Assembly member of the national American Lung Association. Dr. Montalvo Stanton is the proud recipient of the 2000 Bernard Gregory Award for Cultural Diversity given by the National ALA. She was also awarded the Emily Bissell Award 2004 from the ALA of NJ. She is also chair of the Pediatric Section of the New Jersey Thoracic Society. She has a special interest in community medical education and was awarded a grant from the Healthcare Foundation of New Jersey and sanofi-aventis for the development of the Children’s RESPIRA Education program, which is designed to teach Latino families about their children’s asthma and become proactive in their children’s asthma care. She has also been awarded the Angel’s Family Foundation grant, which is to provide Spanish asthma educational materials, asthma equipment and medications to Latino families who participate in the Children’s RESPIRA program. The grant has also provided assistance to families who have no insurance. She also has an interest in lung growth and development as well as an interest in the management of chronic respiratory failure in children with chronic lung disease and neuromuscular disease. She has expertise in infant pulmonary lung function and Pediatric Flexible Bronchoscopy. ABSTRACT: Educating Latino Families about Asthma — Improvements in Knowledge and Health Resource Utilization Through the Children’s RESPIRA Education Program, we are providing bilingual asthma education to Latino families. Introductory education sessions are held for Latino parents and children in Spanish and/or English. Families receive follow-up contacts at 3 weeks, 2 months, and one year. Parents are surveyed at each interaction on hospital admissions, ER and doctor visits, and attitudes. Bilingual, age-appropriate surveys of asthma symptoms and of parents’ and children’s asthma knowledge are administered just before and after the intake educational session and at the first two follow-ups. The aim is to improve quality of life, increase compliance with therapy, and reduce emergency room (ER) visits and hospitalizations. Project Results: 78% of intake surveys were done in Spanish and 22% in English; 87% of families completed some or all survey forms in Spanish. Of the latter, 91% have continued after intake with program follow-ups, compared to only 65% of families responding only in English. Parents’ scores on asthma knowledge tests improved 27%, from a mean of 8.77 out of 13 questions answered correctly before the intake educational session to a mean of 11.14 correct answers after (n=228, 2-tailed p<0.0001, paired comparison); improvement was sustained at all follow-ups. Children aged 6-11 (n=112) showed a 20% improvement (p<0.0001, paired comparison) on 5 questions (means of 3.67 and 4.37), and this improvement was also sustained. In addition, 125 children younger than 6, and 25 over 11, were enrolled. Projected current accrual rate is 200-300 children per year. Compared to utilization prior to enrollment, overall observed rates of hospitalization dropped 0.55 event per child per year (a 52% reduction, p<0.0001) and ER use dropped 0.65 event per child per year (a 77% reduction, p<0.000001). This corresponded with only 45% of parents stating that their response to a mild acute exacerbation would be to “give a dose of rescue medication and call [their] doctor,” which increased to 83% by the time of our second follow-up. Percentages of families with an Asthma Treatment (Action) Plan for at least one child rose from 40% at enrollment to 66% by the time of the second follow-up. Parents with an Asthma Treatment Plan were significantly more likely to report that having a plan is helpful to manage symptoms (p<0.0001, 2-tailed). A bilingual approach is critical in providing care for Latino children with asthma, and fills a vital gap in our health care system. Our program is reducing children’s asthma hospitalization rates and ER use, with substantial projected cost savings to the health care system. Hilda Luiggi, MS Hilda Luiggi, MS, is the Associate Director of Minority Affairs at the School of Medicine and has been instrumental in carrying out a medical school recruitment plan that educates and encourages minority students‚ interest in pursuing a medical education. In this capacity, she attends national medical education conferences such as the American Association of Medical Colleges‚ Conference, the National Association of Minority Medical Educators Conference where she networks with medical school representatives. Moreover, she assists the Director with designing and implementing activities and programs for minority medical students. Mrs. Luiggi participates in the academic, financial and personal counseling of Penn medical students, and is also responsible for the coordination of student community health service activities for the School of Medicine. Mrs. Luiggi is the Coordinator for the Minority International Research Training Program, which helps underrepresented minority students obtain research experience in international laboratories. Mrs. Luiggi has a Master of Science degree from the Caribbean Center for Advanced Studies in Clinical Psychology, and an undergraduate degree in Mathematics from the University of Puerto Rico. She has extensive experience as both an educator and a psychologist, with a specialization in health-related programs in urban settings. Working in public schools, colleges, and public health agencies in Puerto Rico, Chicago, New York and Philadelphia, Mrs. Luiggi has developed insight into the educational needs of children living in large cities. She is a member of the National Hispanic Medical Association, the National Association of Medical Minority Educators, and the Pennsylvania Governor's Commission on Latino Affairs. She also serves as advisor to the National Boricua Latino Health Organization. 2009 HISPANIC HEALTH RESEARCH POSTER SUMMARIES NAME: Alberto J. Caban-Martinez, MPH (Student) Evelyn P. Davila, MPH David J. Lee, PhD Lora E. Fleming, MD, PhD Kathryn L. McCollister, PhD Kristopher L. Arheart, EdD William G. LeBlanc, PhD Sharon L. Christ, PhD, MS, MA Kenneth F. Ferraro, PhD Marcie Pitt-Catsouphes, PhD Janet Wilmoth, PhD UNIVERSITY: PHONE NUMBER: E-MAIL: University of Miami Miller School of Medicine 305-243-7565 acaban@med.miami.edu (Use additional space if needed) TITLE OF PRESENTATION: Do Young Hispanic Workers engage in Risky Health Behaviors? PURPOSE OF RESEARCH: The transition to adulthood is a time of risk-taking and experimentation. By and large, the leading cause of morbidity and mortality in this age group are behaviorally mediated. In addition, there remain many challenges in promoting individual healthy behavior change among minority populations, particularly Hispanics. Given that employed Hispanic young adults tend to work more hours per week than do NonHispanic whites, the workplace can serve as a venue in which to identify risky health behaviors among this minority population. Early intervention, targeting modifiable risky lifestyle behaviors may help thwart the later onset and progression of adult chronic diseases among Young Hispanic workers. For the present study, we examine risky health behaviors among all US Young workers, and among Hispanic workers in particular. METHODOLOGY: Data from the 1997-2007 National Health Interview Survey (NHIS), an annual population-based survey of the entire US civilian population, were analyzed with adjustment for survey design using the SAS System, v9.1. Employed respondents aged 18-24 years old reported on their occupation for the week prior to interview. Workers were grouped into eight industrial sector classifications which are now the focus of the National Occupational Research Agenda (NORA) at the National Institute on Occupational Safety and Health (NIOSH). The total estimated US young worker population, mean age, and the prevalence of risky behaviors, including smoking, risky drinking (defined as ≥10 drinks/week in men and ≥7 drinks/week in women, or ≥5 drinks/at one sitting one or more times in a year), low physical activity levels and obesity (BMI ≥ 30.0 kg/m2), were analyzed by gender and race/ethnicity. Risky health behavior was defined as those young US workers who reported engaging in at least two of the four unhealthy behaviors. RESULTS: An estimated 17,148,467 US workers 18-24 years of age (mean age ± standard deviation; 21.5±1.9) were actively employed across various NORA industry sectors, while an estimated 9,980,828 (20.7±2.0) were not employed from NHIS 1997-2007. Among all US young workers, Hispanics generally engaged in less risky health behavior (3.9% met two out of the four unhealthy behaviors) as compared to their non-Hispanic counterparts (5.3%). For example, Hispanics engaged in less risky drinking (6.9%) and smoking practices (17.4%) as compared to the their non-Hispanic counterparts (10.0%, and 28.0% respectively). However, Hispanic young workers had higher levels of obesity (16.6%) and lower levels of physical activity engagement (72.4% do not exercise) relative to their non-Hispanic counterparts (14.0% and 58.8%). Young workers employed as Motor vehicle operators (9.6%), Machine operators/ Tenders except precision (8.9%), and Health service (8.4%), engaged in the highest levels of risky health behaviors, while those employed in Mail and message distributing (0.0%), Health assessment/treating occupations (0.0%), and Health technologists/technicians (2.0%) were least likely to engage in risky health behaviors. CONCLUSIONS: Worksites provide access to 65% of the population aged >18 years, which makes them an ideal settings to implement strategies for reducing the prevalence and burden of risky health behaviors. Similar to schools, worksites allow access to adolescent employees that are transitioning to adulthood in a controlled environment through existing channels of communication and social support networks. While young Hispanic workers had lower rates of smoking and risky drinking, the prevalence of obesity and low levels of physical activity were higher as compared to their non-Hispanic counterparts. Given the significant growth in the US Hispanic population, the fact that young Hispanic workers work more hours per week relative to young workers of other ethnic backgrounds, worksite health promotion programs targeting young Hispanics workers are paramount, particularly those relating to weight management and cardiovascular fitness. NAME: UNIVERSITY: Andrea Pappalardo, MD University of Chicago Medical Center PHONE NUMBER: 773-702-1000 (pager 3344) or 630-863-1545 (cell) E-MAIL: andrea.pappalardo@uchospitals.edu (Use additional space if needed) TITLE OF PRESENTATION: Residents and Latino Communities Partnering to Improve Asthma Outcomes among Latinos in Chicago Authors: Andrea Pappalardo,MD, Flavia Lega, MD, Valerie Press, MD, Oscar Estrada, MD, Mary Johnson, Vinny Arora, MD, Monica Vela, MD PURPOSE OF RESEARCH: 1. To assess baseline patient knowledge regarding self-management of their asthma 2. To assess resident knowledge regarding asthma, including familiarity and skill in teaching patients how to use inhalers 3. To develop a community based patient education program regarding asthma self management and appropriate inhaler use METHODOLOGY: The Neighborhood BREATHE Project is a two-tiered education program. The first tier delivers resident run bilingual workshops to patients at local community-based clinics teaching the fundamentals of managing asthma. A pre-program survey in both English and Spanish will assess patient’s self-perceived difficulties with managing their asthma and these results will primarily drive the focus of each resident-patient group session. A post-program patient survey will assess the effectiveness of the program in improving the attitudes and knowledge level of patient’s selfmanagement. Spanish-speaking resident educators as well as asthma information handouts in both English and Spanish will be utilized to enhance teaching. The second tier involves a) assessing residents’ baseline knowledge and beliefs regarding asthma education and counseling regarding patient self-management and b) teaching them basic knowledge about assessing patient self-management as well as skills to address deficiencies. This aspect of our project already has begun and is ongoing. The resident education begins with a one-hour session during the second year ambulatory block. A pre-test focusing on resident baseline knowledge, comfort level and beliefs regarding patient self-management, specifically medication adherence vs. compliance is performed. The residents are then given clinical vignettes to address a potential problem with patient self-management to discuss in small groups. We then discuss these clinical scenarios as mechanism to teach tangible assessment skills. We also conduct a skill-based learn to demonstrate how to use inhalers to each other including a step-wise assessment of inhaler technique. The program is evaluated at the end of the month long ambulatory block with a resident post-test, evaluating for a change in knowledge, comfort level and perceived uptake of the skills in their clinics. RESULTS: A preliminary needs assessment of residents demonstrated that 40% (n=113) of residents were not comfortable partnering with patients to develop actions plans for home management of their disease; this is not surprising given that only 28% reported any prior education in patient self-management. Residents who received formal education were more comfortable with and were more likely to counsel their patients. Barriers to effective health promotion included lack of time (80% of residents) and lack of educational materials (50%), both of which will be addressed in this project. Most recently, we partnered with Corazón Community Services, a group formed in 2003 who seeks to improve the quality of life for largely Latino families, children and youth with programs including the Cicero Community Health Initiative. This initiative focuses on the identification and analysis of health conditions within the community with a focus on public awareness campaigns. With Corazón, we organized a focus group of 12 patients within the community at the Cicero Town Center which confirmed that Latino patients face numerous barriers to asthma care including lack of education on their disease, misunderstanding about medication purpose and communication between patient and healthcare workers. This included one patient who was adamant that using a cheaper and more available over the counter inhaler was an alternative to the new HFA rescue inhalers. Misinformation runs rampant throughout the community. Knowing this, we piloted a bilingual educational session for 8 participants led by Spanish speaking internal medicine residents that focused on triggers and symptoms also incorporating pre and post information surveys on this topic. Future sessions are underway. CONCLUSIONS: 1. Asthma is identified by community clinic practices as an area that deserves additional educational interventions for patients. 2. Inadequate self-management of asthma leads to significant increase in morbidity and mortality. 3. The policy change mandating a complete change to HFA type inhalers can potentially further complicate the problems already faced of patient-self management. 4. Residents lack training, time and comfort with counseling patients on self-management. 5. Directed training to residents regarding effective and efficient counseling for patients with asthma, particularly regarding the new HFA policy change is imperative to increase patients’ ability to self-manage their asthma. 6. Patients need further education and training in regard to their medication use and plans outside of the conventional physician visit. Please email form to: mbarnard@nhmamd.org NAME: Andrew Figueroa UNIVERSITY: SUNY at Stony Brook PHONE NUMBER: 631-664-1930 E-MAIL: amfiguer@ic.sunysb.edu (Use additional space if needed) TITLE OF PRESENTATION: Multiple Sclerosis and Neurocognitive Outcomes in Hispanic Children. PURPOSE OF RESEARCH: Multiple sclerosis is a complex immune mediated central nervous system (CNS) disorder. There is some evidence that pediatric multiple sclerosis (MS) is particularly common in the Hispanic population. However, little is known about the impact of the disorder on cognitive functioning in this population. This preliminary investigation was designed to improve our understanding of cognitive functioning in Hispanic individuals. METHODOLOGY: The sample involved a total of 17 patients: 5 males and 12 females. The mean age of the sample was 14 years and 9 months with a standard deviation of 2.01. These patients were seen at Stony Brook University Hospital's National Pediatric Multiple Sclerosis Center. The cognitive domains tested included: attention, executive function, visual spatial/visual constructive, visual and verbal memory, and psychomotor/processing speed. The battery of neuropsychological tests included the following neurocognitive instruments: the Conners Continuous Performance Test (CPT II); Tower of London-Drexel Version (TOL DX); Contingency Naming Test (CNT); Rey-Osterrieth Complex Figure (ROCF); and the California Verbal Learning Test-Children's Version (CVLT-C). The Wechsler Abbreviated Scale of Intelligence (WASI) test was used as an indication of general intellect along with visual spatial/visual constructive skills. Cognitive impairment was defined as 1.5 standard deviations below age norms on > 2 of 9 measures used to define cognitive impairment within the domains. RESULTS: 9 out of the 17 children were cognitively impaired. The tests that these children did poorly on included CNT, WASI, CVLT, TOL and ROCF. The most vulnerable areas for impairment were visual memory, executive function, and psychomotor/ processing speed. The mean value of number of subtests failed was 1.77 and the standard deviation was 1.60. CONCLUSIONS: Multiple sclerosis is a complex immune mediated CNS disorder that may put Hispanic children at risk for cognitive impairment. The domains most affected were visual memory, executive function, and psychomotor/ processing speed. Future research on this disorder with larger samples and additional follow-up is needed. NAME: N. Anton Borja, Terez Yonan, Danielle Barnett, Asad Siddiqi, Ayman Alsharbini, Katie Legare, Inga Schlingmann UNIVERSITY: A.T. Still, School of Osteopathic Medicine Arizona ~ Lutheran Family Healthcare Centers, Brooklyn, NY PHONE NUMBER: 347.831.0936 E-MAIL: nborja@atsu.edu (Use additional space if needed) TITLE OF PRESENTATION: A community project utilizing Patient Navigators to improve postpartum follow-up of Hispanic and other racial/ethnic minority pregnant patients in a Family Health Center. PURPOSE OF RESEARCH: The underutilization of maternal postpartum care by Hispanic, and other racial/ethnic minority women throughout Brooklyn, NY continues to be a significant health disparity. Minority patients have been shown to have significant inequalities in health care, and ultimately inequality in health status. Our community project will attempt to increase the number of postpartum visits in the Sunset Park FHC by implementing the use of Patient Navigators in postpartum care. METHODOLOGY: Patients at Sunset Park Community Health Center who were between 35-40 weeks gestation were identified. Thirty of these identified patients were recruited to receive support from patient navigators. Patient encounters were coordinated by navigators for subsequent prepartum clinic visits, post-delivery while in the post-partum department of Lutheran Medical Center, and finally by telephone calls and home visits. Patient navigators could perform any of the following duties as deemed necessary by the navigator and the patient: 1. Coordinate screenings and medical referrals; 2. Provide health literature for clients; 3. Identify resources related to health insurance, financial assistance, medication, home care and transportation; 4. Offer emotional support, and make referrals to support groups and classes; 5. Help clients overcome language and cultural barriers; 6. Coordinate a patient home visit; 7. Integrate maternal and pediatric care. The importance of returning for the post partum visit was stressed at each of the patient encounters. The primary outcomes measured are the rates for postpartum visits in patients receiving support from a patient navigator compared to return rates of patients without patient navigators. An entry survey was also provided to patients to identify the perceived value of a postpartum visit, the value of a patient navigator, and the possible difficulties which may prevent returning for a postpartum visit prior to receiving patient navigator follow-up. RESULTS: The project is currently underway, and the outcomes will be measured within the next few weeks. CONCLUSIONS: We are expecting to see an increase in the return rates for post partum visits among the Sunset Park Clinic patients receiving patient navigator support, compared with patients not followed by a patient navigator. NAME: Christina Mangurian, MD UNIVERSITY: Columbia University PHONE NUMBER: 212-543-6020 E-MAIL: cm2195@columbia.edu TITLE OF PRESENTATION: Adaptation of a Weight Loss Program for Latino Patients in a Community Mental Health Clinic PURPOSE OF RESEARCH: Patients with severe and persistent mental illness (SPMI) lose more than 25 years of potential life in comparison to the US general population. The leading cause of this increased mortality is cardiovascular disease, related in part to increased prevalence of risk factors like obesity, dylipidemia, hyperglycemia and hypertension. Latino patients with severe and persistent mental illness (SPMI) have a higher prevalence of the metabolic syndrome than schizophrenia patients in CATIE or Hispanics in the US, suggesting additive risk and a highly vulnerable population. A major risk factor for the metabolic syndrome is obesity. Behavioral weight control techniques have been shown to be effective in overweight/obese SPMI patients. However, there is almost no information on the effectiveness in higher risk populations, such as low-income Latino SPMI patients. Ganguli developed a behavioral therapy approach for overweight SPMI patients. For this study, we culturally modified Ganguli’s manual to determine if it could be feasibly delivered and effective in Latino SPMI patients METHODOLOGY: Subjects: The Washington Heights Community Service (WHCS) provides inpatient and outpatient services for SPMI patients living in Northern Manhattan. About 60% of the patients have schizophrenia spectrum disorders and 30% have bipolar disorder. The WHCS serves approximately 60% women and 40% men; with an ethnic distribution of 75% Hispanic, 15% African American, 9% Caucasian, and 1% Asian. The high proportion of Hispanic patients creates a unique opportunity to assess the efficacy of a behavioral treatment in this high risk group. Procedures: Ganguli’s protocol was translated to Spanish and modified to be culturally sensitive to this population. WHCS day-program patients with BMI greater than or equal to 25 were identified, informed consent was obtained, and baseline characteristics were collected. Primary outcome measures were course attendance and weight. After initial assessment, a 14-week culturally-modified behavioral therapy course was held. All participants were given pedometers and scales. After completion of the course, patients were re-weighed. Paired t-tests and the Sign test were used to examine pre-post effects on weight. RESULTS: 89% (65/73) of the day treatment patients were eligible for the study. 78% (51/65) consented to participate, with 20% (13/65) refusing and 2% (1/65) having a work conflict. The average age was 49 years old (range 23-79 years). 79% were female and 21% male. Most were Latino (83%), predominantly Dominican (79%); with the remaining 10% Caucasian, 3% African American and 3% other. Most participants (86%) were on atypical antipsychotic medications. Many also took medications to control metabolic co-morbidities, including antihypertensives (31%), hypoglycemics (17%), and lipid lowering medications (28%). Due to room availability, only some patients could be offered the course immediately. We present the preliminary results of those 29 patients. 90% (26/29) of the patients attended over half of the classes. The mean pre-course weight was 179.7lbs (SD=36lbs) and post-weight was 178.2lbs (SD=36lbs). Because some patients gained weight taking the course, the paired t-test was not significant. However, more patients were found to lose weight than gain weight (p=0.043), with 69% (18/26) losing weight, 4% (1/26) maintaining weight, and 27% (7/26) gaining weight. The three patients eligible for but not attending the class gained a mean of 2.67 lbs over the same time period, with only one losing weight and two (67%) gaining weight. CONCLUSIONS: This study provides preliminary evidence that a culturally-modified behavioral weight reduction course is feasible to implement for Latino SPMI populations treated in community settings, and further preliminary evidence that such a course can favorably affect body weight compared to no treatment. NAME: Evelyn P. Davila, MPH Alberto J. Caban-Martinez, MPH Lora E. Fleming, MD, PhD David J. Lee, PhD William G. LeBlanc, PhD Kristopher L. Arheart, EdD Kathryn McCollister, PhD Sharon Christ, PhD UNIVERSITY: University of Miami Miller School of Medicine PHONE NUMBER: 305 243 7929 E-MAIL: edavila1@med.miami.edu TITLE OF PRESENTATION: Are Young Hispanic US Workers at Greater Risk for Death? PURPOSE OF RESEARCH: Youth workers are a population more susceptible to harm while engaged at work as compared to older workers. In addition, Hispanics are reported to have a greater risk of workplace injuries relative to non-Hispanic whites. However, relatively little is known about the mortality risk among young adult Hispanic workers between the ages of 18 to 24 years. The present study assessed the association between self-reported Hispanic origin, gender, employment, and mortality risk among young adults using a nationally representative sample. METHODOLOGY: Data from the 1986-2000 National Health Interview Survey with mortality follow-up through 2002 were pooled and analyzed by Hispanic origin, employment status, gender and occupation. Mortality analyses were completed using SUDAAN software, with adjustments for the survey design, gender, and education, and included 121,478 young adults aged 1824 years with employment data at baseline, representing more than 24 million young adults over the survey period. RESULTS: Among all young adults age 18-24, employment was associated with greater all-cause (Hazard Ratio=1.38 [95% Confidence Interval (CI) 1.23-1.54]) and homicide mortality risk (1.98 [1.50-2.62]). Relative to young adults of non-Hispanic origin, young Hispanic adults had greater risk of all-cause mortality (1.42 [1.22-1.64]), homicide (1.66 [1.16-2.38]), and mortality from all causes “other than homicide, suicide, motor vehicle accidents” (1.54 [1.291.85]). Similarly, among employed young adults, Hispanics had greater risk of all-cause mortality (1.49 [1.23-1.82]), homicide (2.16 [1.30-3.59]), and mortality from all causes “other than homicide, suicide, motor vehicle accidents” (1.74 [1.33-2.26]) compared to young workers of non-Hispanic origin. Regardless of Hispanic origin or employment status, lower educational attainment and male gender were associated with increased mortality risk. CONCLUSIONS: Although we cannot ascertain if cause of death was work-related, the results show that young Hispanic workers are more likely to die relative to non-Hispanic workers. Greater research is needed to understand why Hispanic workers have the greatest mortality risk. Nevertheless the workplace can serve as a place for educating about the harms young Hispanic workers are susceptible to both on and off the job that may lead to premature mortality. NAME: Diana Montoya-Fontalvo (research mentor: Olveen Carrasquillo) UNIVERSITY: Columbia University PHONE NUMBER: (857)998-0390 E-MAIL: dcm2124@columbia.edu TITLE OF PRESENTATION: “Patient Perceived Barriers to Diabetes Self-Management” PURPOSE OF RESEARCH: The purpose of this qualitative research study was to examine how poorly controlled diabetic Latinos in Washington Heights perceive their own illness. Specifically, we were interested in seeing what factors patients themselves discerned as leading to uncontrolled diabetes as well as what factors they perceive as being the most helpful to successful management. The goal was to use this data on patient perceptions of their own poorly-controlled diabetes to inform the development of a new interventional model and tailor it to the beliefs of this particular population. METHODOLOGY: Participants consisted of ten 35 to 75-year-old Latinos living in Northern Manhattan who had a Hemoglobin A1C done within the past year, with the latest value being >= 8.0, and who were currently being followed by providers in CUMC’s Associates in Internal Medicine Clinic (AIM). At the start of each session, the researcher met with the nurse practitioners, diabetes educator, residents and attending physicians to determine if any of their scheduled patients met the study criteria. Once the patient arrived or if such a patient was in the waiting room, they were asked if they were interested in participating in the study. If the patient agreed, they were taken to one of the available exam rooms for a 30-45 minute open ended interview. At the end of the interview, subjects were compensated $15 for their participation. The study was terminated at ten subjects because thematic saturation was deemed reached at this point. RESULTS: The four main findings of this study were as follows: 1) Poorly controlled diabetics were well informed as to the methods by which one is supposed to control one’s diabetes (i.e. diet, exercise and adherence to medication) and acknowledge that this knowledge has benefited them. 2) Many poorly controlled Type 2 diabetics did not perceive themselves as having trouble controlling their diabetes. In their eyes, “control” signified being able to change their glucose levels if they wanted and sometimes having glucose readings in the normal range. 3) Many patients felt diabetes was a very “treacherous” disease with insidious complications that one could not always see coming. 4) Most patients reported emotionally challenging life circumstances and experiences as the main barrier to more effective management of their diabetes. CONCLUSIONS: In this hospital based clinic, Latino patients were relatively well informed about the risk factors that must be controlled (i.e. diet, obesity, lack of exercise). However, we identified several areas where diabetes patient education could be enhanced. First, the notion that diabetes control involves more than the occasional glucose reading within the desired range must be emphasized to patients, perhaps by spending more time helping the patient understand measures such as the HgA1C. Second, the danger of diabetes and its long term complications do not seem to be as prominent in health care discussions between patients and their providers early on in the disease course. Such discussions could prove worthwhile, not only for preventative reasons but also to help patients anticipate the chronicity, seriousness and complex regimens needed to manage this disease. Perhaps in this way, patients would be better equipped to engage in successful diabetes selfmanagement techniques even when faced with additional stressors and other social issues. However, our findings suggest that identifying and helping patients address psychological and social issues will need to be an important component of diabetes management. These findings have played an important role in helping develop the Diabetes Community Health Worker management program in Northern Manhattan. NAME: Estela Cabrera UNIVERSITY: University of Wisconsin-Whitewater PHONE NUMBER: 262-497-2553 E-MAIL: CabreraE28@uww.edu TITLE OF PRESENTATION: The Impact of Peer Pressure, Gender, and Age on Substance Abuse in Adolescents PURPOSE OF RESEARCH: During adolescence, parents blame the peers who their teen are surround with the most. Parents blame their children’s peers due to their adolescents’ new rebellious ways, new ways of challenging the “world”, and decrease in time spend with the family. However, parents often fail to focus on the other factors that lead their adolescents to such behavior. The research that will be presented here will examine substance abuse behavior during adolescence. This research focuses on how peer pressure, gender and age play a role in adolescents when it comes to substance abuse. The study compares gender differences in order to better understand which gender is more likely to be involved in substance abuse and in what circumstances. Peer pressure will also be examined to explore which gender is more influenced by their peers. Adolescents’ ages will be evaluated to better focus on when adolescents are influenced by others. Other factors that play a role on the adolescents’ substance usage will also be discussed. METHODOLOGY: A literature review was conducted in order to obtain information for this study. Scholarly articles in the field of psychology that focused on adolescents’ substance abuse were reviewed. Some of the articles include “Reviewing theories of adolescents substance use: Organizing Pieces in the Puzzle” from the American Psychological Association and “Peer influences and drug use among urban adolescents: Family structure and parent-adolescent relationship as protective factors” from the Journal of Consulting and Clinical Psychology. After gathering information, a research paper was completed in regards to this investigation. The most relevant findings of this research will be displayed in a poster research presentation for the 13th Annual National Hispanic Medical Association Conference. This research was made as part of the “Psychology of Adolescence” class offered at the University of Wisconsin-Whitewater under Dr. Joan Littlefield Cook, professor of psychology. RESULTS: Some of the relevant findings of this analysis are the following. Peer pressure is one of the main reasons why adolescents are involved in substance abuse. Since peer pressure is one of the main factors, it must be understood how it plays a role within adolescents populations. The definition of peer(s) is “people who are roughly the same age” (Steinberg. L.). According to Laurence Steinberg ( Adolescence 2005) peers serve four changes. The first change is that the amount of time that adolescents spend with their peers increases. The second change is less parental supervision. The third change is cross-gender relationships, which also increase. For example, the relationship among other gender adolescents’ form or increase, mixed gender friendship groups increase, and romantic relationships begin. The fourth change is crowds arise (small clicks start to develop among adolescents) due to the increase of mixed gender friendships. These four changes play a role on the influence that peers have on adolescents. Peers are primarily blamed for the random behavior of an adolescent especially when negative behavior increases dramatically. Other factors also influence why adolescents experiment with substances. Some of these factors are low parental supervision, one parent household, sexual abuse, and self experimentation. The research literature suggests that in one parent households, adolescents: become more influenced and pressured by his or her peers to use substances; have higher frequency of substance usage than those adolescents with both parents in a household. Furthermore, this literature indicates that abused victims have a higher likelihood of being involved in substance abuse compared to the non-abused adolescents. Additionally it has also been reported that abused victims tend to start substance abuse at a much earlier stage compared to the non-abused. Moreover, the results of gender comparison suggest that male adolescents that were physically or sexually abused when they were younger have a higher frequent use of substance abuse than female adolescents who were also abused. In regards to which gender is more likely to abuse substances and under what circumstances, one study showed that boys and girls had different motives for using alcohol. For “Young adolescent boys’ drinking was whether their friends drink, whereas girls’ drinking was more strongly related to levels of intrapersonal disorder. Peer pressure was a more important predictor of drinking among older adolescents girls, but, for boys, peer pressure remained highly significant throughout adolescence.” (Barber, J. G., Bertrand, L. D., Bolitho, F. 1998) The investigation also reveals reasons why adolescents start or quit their substance abuse. The main reason for adolescent males to start was if their friends used drugs. For females, the overt pressure to use drugs was a more important consideration. On the contrary, some of the reasons which have led adolescents to stop substance abuse behavior for both genders were fear of physical or psychological damage. CONCLUSIONS: Research findings emphasize that peer pressure, gender, and age impact substance abuse within adolescent populations. Also, the findings suggest that the parental involvement in an adolescent’s life can decrease the changes of an adolescent experimenting with substances as well as the peer pressure to use legal or illegal substances. The information provided by this study is important to both parents and adolescents. As mentioned previously, parents can decrease the influence that peers and substances have on their teens. Adolescents can benefit from this information by noticing and acknowledging what are the main factors that lead their peers to use legal or illegal drugs. For example, adolescents can decrease the pressure they put on their peers to do things in which they are not necessary comfortable. What can be done to help adolescents’ with this issue is constant communication with their parents as well as parental supervision. This will enable adolescents to be less influenced by peer pressure. NAME: Guillermo E. Espinoza-1st Author, Philip J. Smith-2nd Author UNIVERSITY: New York University School of Medicine PHONE NUMBER: (646) 238-6825 E-MAIL: Guillermo.espinoza@med.nyu.edu (Use additional space if needed) TITLE OF PRESENTATION: Control of Hypertension amongst Urban and Non-Urban Dwelling Salvadorians PURPOSE OF RESEARCH: To determine whether differences in population density play a role in both the availability and efficacy of hypertension control amongst the Salvadorian population. METHODOLOGY: Health surveys were administered to 510 patients seen at the Hospital Nacional Rosales and the mobile clinics of the Salvadorian organization CEDEINFA. 203 patients were from the greater metropolitan area of San Salvador, El Salvador’s capital, and 307 patients were from less-populated regions of the country. A total of 156 individuals were found to have hypertension, defined as having a systolic blood pressure of 140 mmHg or greater and/or a diastolic blood pressure of 90 mmHg or greater or individuals who were on antihypertensive medication(s) at the time of interview. For those individuals who were found to be on antihypertensive medication(s), the efficacy of their antihypertensive regimen was evaluated based on whether or not they had achieved blood pressures lower than the pre-set guidelines of the study. RESULTS: 73.8% (or 45/61) of the hypertensive individuals from San Salvador were on antihypertensive medication(s) compared to 51.6% (or 49/95) of the hypertensive individuals in the less-populated regions of the country. For the sample in the study, there was a statistically significant difference in the number of hypertensive individuals who were not on any antihypertensive medication(s) between the groups who were from San Salvador and those who were not (2=7.623809, P=0.0057, =0.05). However, of the individuals who were on medication and resided in less densely populated regions, 59.2% (29/49) were found to have blood pressures below the pre-set hypertensive guidelines for the study. By contrast, for individuals on antihypertensive medication(s) who resided in the capital, only 51.1% (23/45) had a blood pressure lower than the pre-set hypertensive guidelines. The study demonstrated a statistically significant difference between the efficacy of antihypertensive regimens between the hypertensive individuals on antihypertensive medication(s) from the capital and those from the less densely populated regions of El Salvador (2=3.198057835, P= 0.0737, =0.10). CONCLUSIONS: The data suggests that population density may play a role in the supply of healthcare available to Salvadorians in regions with different population densities. The reason for this observation, however, is unclear. The apparent lack of access to healthcare in the less densely populated regions of El Salvador could be due to an actual numerical imbalance between patients and healthcare providers, a distance barrier between healthcare centers and patients’ residences, or perhaps an economic barrier that might exist if the type of employment available in densely populated areas is more conducive toward seeking medical attention. Although less compelling but nonetheless important, is the fact that the data from this study also suggests that control of hypertension is more efficacious amongst those hypertensive Salvadorians who reside outside of the capital. The exact reason for this though, remains unclear. It would be difficult to find one specific factor which would explain the antihypertensive regimen efficacy difference observed between those individuals who reside in the capital and those who reside in less densely populated regions, since many factors influence the control of hypertension. Such factors include the duration of an individual’s hypertension (e.g. chronic vs. new on-set), the medication of choice for therapy, the individual’s adherence to the therapy, which may or may not be linked to the ability of the individual to obtain the necessary medication, the desire or ability of an individual to change lifestyle factors such as diet and exercise, as well as the attention that a given healthcare provider may pay to his/her patients’ conditions. It may be difficult to evaluate the roles that different socioeconomic and healthcare policy factors play in the availability and efficacy of the control of hypertension amongst Salvadorians from areas of different population densities. However, this feat is much easier to accomplish in a country as small as El Salvador because certain factors such as diet, race and ethnicity are, in theory, minimized due to the relative homogeneity of the Salvadorian population. Factors which can be improved upon such as medication and healthcare distribution, as well as physician quality control and patient education in urban as well as low density areas should be evaluated as possible causes for the differences observed. NAME: Jason P. Alvarado UNIVERSITY: University of Illinois College of Medicine at Urbana-Champaign PHONE NUMBER: 773-824-6410 E-MAIL: jalvar20@illinois.edu TITLE OF PRESENTATION: CARDIAC ARREST, CARDIOPULMONARY RESUSCITATION, AND END-TIDALCARBON DIOXIDE PURPOSE OF RESEARCH: To determine if, with an improved quality of cardiopulmonary resuscitation, end-tidal carbon dioxide threshold values are higher than previously considered. METHODOLOGY: Cardiopulmonary resuscitation was performed on in-hospital cardiac arrest patients using a modified external defibrillator with recording and feedback capabilities. Episodes were analyzed retrospectively and compiled into usable data sets for further analysis. RESULTS: Out of 107 patients included in the study, our data shows a successful resuscitation rate of 42%. The study cohort consisted of 54% male patients, 46% female, with the majority of patients being of African American descent (64.5%). Examining raw cutoffs using an EtCO2 value of 10 mmHg, only two patients were successfully resuscitated with mean and final measurements below that threshold respectively. CONCLUSIONS: As of yet no definitive statement can be made in terms of the validity of our hypothesis. It seems as though a trend towards increased thresholds does exist with improved QCPR, but more statistical analysis is required before that can be undoubtedly determined. NAME: Jazmin Castellanos UNIVERSITY: University of Wisconsin-Whitewater PHONE NUMBER: 262-510-5895 (cell) or 262-473-5765 (home) E-MAIL: CastellaJ10@uww.edu TITLE OF PRESENTATION: Tradition, Disease and the Development of Medicine in Latin America: Conflicts between Medical Doctors, Curanderos and Politicians. PURPOSE OF RESEARCH: The 18th century was a critical period for the development of medicine in Latin America. During this period, medicine became institutionalized meaning that medicine takes form of an established system within society. This process was not easy due to the fact that there were various conflicts between medical doctors, curanderos (people that practice folk medicine), and politicians. The medical doctors had to struggle against the curanderos. The medical doctors argued that the curanderos did not practice medicine correctly and were scamming patients. From the curanderos’ point of view, the medical doctors wanted to create a monopoly in order to gain control of the medical field and leave them without a job. However, the conflict was not just between medical doctors and curanderos; it also extended to the political world. Medicine and disease were used in this period as sources of power by politicians. Medicine has served in campaigns of fear towards the general population throughout history. The struggle between doctors, curanderos, and politicians still continue today. The purpose of this research is to: illustrate the process in which medicine develops in Latin America; give examples of conflicts between medical doctors and curanderos in Latin America; describe how medicine and disease have been used in order to create campaigns of fear, and discuss how politicians have taken advantage of medicine and disease in order to advance their agendas. METHODOLOGY: A literature review was conducted for this research. Scholarly books and articles related to the research were analyzed by using the library resources at the University of Wisconsin-Whitewater and the University of Wisconsin-Madison. Once resources were found, the books were read and relevant information from these sources was gathered. Some of the books included for this research were “Entre Medicos y Curanderos: Cultura, Historia y Enfermedad en la America Latina Moderna” and “Women’s Tales From The New Mexico WPA, La Diabla a Pie” as well as “Power” by French philosopher Michel Foucault. Once the information was gathered, a research paper was completed. The research was conducted under the supervision of Dr. Pilar Melero, Assistant Professor of Spanish, Chicano/a Literature, and U.S. Latino/a Literature at the University of Wisconsin-Whitewater. The findings of this study will be displayed in a poster research presentation at the 13th Annual National Hispanic Medical Association Conference. RESULTS: (Please note that the following is a preview of the significant findings of this research) In Latin America, the Spaniards were the first to use disease and medicine as tools in order to convert the indigenous population to Catholicism. An example of this occurred in the 16th century in Argentina. When the smallpox disease was introduced to this region during this time, the indigenous people believed that the smallpox was a divine punishment. The Spaniards took advantage of the situation by telling the indigenous people that if they did not become Catholics, their “divine punishment” would continue until they changed their religion. The Spaniards were not the only ones to use disease as a weapon. Other government officials have also used disease for their political agendas. After the smallpox vaccine was discovered, Argentina’s president Rosas did not allow the indigenous people to receive the vaccine against smallpox. Rosas’s action was an indirect strategy to ensure the extinction of the indigenous people in Argentina. Once disease was introduced to Latin America, the process of institutionalization of medicine began. Michel Foucault, a prestigious French philosopher, did an analysis on the politics of health of the 18th century. In his analysis, Foucault mentions that rules between health and individuals were established. These rules included that families were responsible in maintaining everyone within the family as healthy as possible, especially children. During this process, the concept that each person is responsible for his/her health arises during the 18th century. As medicine becomes institutionalized in Latin America, a new conflict arises. This new conflict is between medical doctors and curanderos. For example, the medical doctors gave treatments to patients based on scientific explanations and curanderos treated patients based on folk medicine. The medical doctors argued that the curanderos did not practice medicine correctly and were scamming patients. From the curanderos’ point of view, the medical doctors wanted to create a monopoly in order to gain control of the medical field and leave them without a job. Besides medical doctors and curanderos, midwifes also became important members of the community which primarily helped women to give birth during deliveries. As the field of medicine made progress, medical facilities were also created in Latin America. One example is the development of the first mental hospital in Mexico City in September 1910 which name was La Castaneda. During this time, one of the challenges for the people that founded the institution was to create an administrative program for it. At the same time, La Castaneda was used as an example of modernization that characterized the last years of command of Porfirio Diaz. The development of this mental hospital meant economic progress for Mexico as Porfirio Diaz’ goal was to modernize Mexico in order to help the country do well economically during his administration. However, economic growth did not occur since it was the foreign investors that had most of the profits and not the Mexican people. This is another example of how politicians in Latin America have used medicine and disease in order to advance political agendas. CONCLUSIONS: Conflicts between medical doctors and curanderos still exist. In different parts of Latin America curanderos and midwifes are still an important part of the medical landscape. Many people still use natural remedies for diseases rather than going to be seen by a medical professional. This tradition has increased during the last years. In fact, curanderos have become more popular in recent years, and today anyone can buy a book which contains natural remedies for any type of illnesses. In spite of the developments in medicine in Latin America, the legacy of conflicts between medical doctors and curanderos still exists. Furthermore, politicians use disease to instill fear towards the general population as they advance their political agendas. NAME: Jessica Blick, Gerry Maitland MD, José E Rodríguez MD UNIVERSITY: Florida State University College of Medicine PHONE NUMBER: 850 645 6850 E-MAIL: jose.rodriguez@med.fsu.edu, jlb07u@med.fsu.edu (Use additional space if needed) TITLE OF PRESENTATION: Pre and Post Natal Care of Neural Tube Defects in Coastal Ecuador PURPOSE OF RESEARCH: The incidence of spina bifida in developing countries tends to be higher than that of the United States due, in part, to inadequate nutrition and poor prenatal care. According to the World Health Organization, the prevalence of births of spina bifida in Atlanta, United States from 1993 to 1998 was 2.73 per 10,000 births, while in Ecuador in the same years it was 4.22 per 10,000 live births.2 The purpose of this research was to attempt to identify the etiology of the increased incidence of the disease though a focused study in Manta, Ecuador. METHODOLOGY: Eleven mothers of children with spina bifida were interviewed in Manta, Ecuador regarding various aspects of their pregnancies, past medical histories, and family histories. Their affected children were all current or former patients in a local physical therapy clinic. The child was always present for the interview, while other siblings and fathers were sometimes present. The mothers were asked the number of pregnancies, number and health status of other children, family history of spina bifida or other neurological diseases, chronic diseases or illnesses during pregnancy, access to prenatal care including ultrasounds during pregnancy, nutritional habits, vitamin intake during pregnancy, home remedies and alternative treatments during pregnancy, and proximity to chemicals or pesticides. RESULTS: Of the eleven afflicted children, only one case was identified prior to birth by an ultrasound at 8 months of pregnancy, despite the fact that seven underwent at least one ultrasound. The ages of the patients were between 11 months and 11 years. Three of the patients had only spina bifida, while eight had spina bifida with hydrocephalus; all required corrective surgery. No children were reported to have full control of their bladders. All afflicted children of school age were attending school. Interestingly, five of the eleven children were born in the months of November or December. The range of ages of the mothers at the time of their child’s birth was between 21 and 34. Two of the mothers had previous spontaneous abortions. Four of the mothers had illnesses in their pregnancy; 2 http://www.who.int/genomics/about/en/spinabifida.pdf two urinary tract infections, one dengue fever, and one “bone pain.” Only one mother reported a chronic disease, arthritis. However, most mothers were not tested for gestational diabetes. No other children in the families had neurological problems. Eight mothers reported a positive family history for some type of neurological problem. Four mothers reported spina bifida in a close relative: a father, a first cousin, an aunt, and an uncle. Other neurological problems include a seizure disorder, hemiparesis, club feet, Down syndrome, muteness and deafness. No mothers took folic acid or vitamin supplementation prior to conception. Six mothers were administered folic acid and/or vitamin supplementation after 30 days of pregnancy, while five did not take vitamins. All but one mother had access to some form of prenatal care. CONCLUSIONS: Ecuador is a developing country highly dependent on the crops of the season for nutrition. As half of the children were born in either November or December, more investigation is necessary to determine whether this is coincidence, a general trend in the population, or if the available vegetation in March and April has less folic acid than other times during the year. Thirty-six percent of the afflicted children had close relatives with spina bifida. The most critical finding was that none of the mothers had folic acid supplementation during the critical first thirty day period of gestation. Ecuador, like the United States has similar problems with unplanned pregnancies. Fortification of common foods with folic acid as done in the United States or educational campaigns directed towards the nutrition of women of child-bearing age would likely decrease the number of spina bifida cases due to folic acid deficiencies. NAME:Amanda Grondin, Alvaro Bada, José E Rodríguez MD UNIVERSITY:Florida State University College of Medicine PHONE NUMBER:(954) 579-5054 E-MAIL:arg07e@med.fsu.edu (Use additional space if needed) TITLE OF PRESENTATION: International Service Learning to Teach Cultural Sensitivity, Medical Humanism, and Latino Culture. PURPOSE OF RESEARCH: Students Interested in Global Health (SIGH), a medical student organization at the Florida State University College of Medicine (FSUCOM) developed aninternational service-learning trip in 2008 to Ecuador. Students were interested in the culture, customs and health beliefs of patients living in Ecuador. Students were also interested in applying knowledge learned in Ecuador to the large Latino population that they well be serving in the coming years. Students focused on reflective learning from the Ecuadorian health system and international global health efforts. METHODOLOGY: Seven medical students with one faculty member traveled to Ecuador to meet the above goals. Students worked with local medical professionals at public and private hospitals. At the medical facilities, students were given opportunities to hear from providers that left the US and Canada to serve the Ecuadorian people. They also visited and served local orphanages, elderly rest homes and international water projects. Students were able to observe first hand some of the aspects of daily life of Ecuadorian citizens, such as housing and dietary practices. From the outset, the students believed that although they would provide service in Ecuador, they would be more changed than the people they served. Students participated innightly verbal and written reflective exercises with their peers and faculty--reflecting on the days events and examining the question of how this experience will help them work with Latino patients in the US. RESULTS: Cultural Sensitivity: Early on, the reflections centered on differences between Ecuador and the US evident in: the healthcare system, multiculturalism, cultural sensitivity, and access to health care.Students were surprised by the willingness of the medical profession to accommodate traditional medicinein Ecuador. In an effort to be more sensitive to the indigenous population, the hospital in the small town of Alausí was constructing special rooms to accommodate for the traditional ‘vertical birth.’ Additionally, in another multipurpose clinic they had pediatrics, medicine with a lab, dentistry and acupuncture all under one roof. Medical Humanism: Students were shocked at the abandonment of the elderly visible at Hogar de Ancianos, a government elderly home. One student reflected, “Many of the residents live out the end of their lives without a loved one or family member, or hope to see one of them ever. I looked around the room, and saw despair, delight, and dementia. My own mortality struck me as I saw this group, and a fear gripped me that I could also be abandoned in the final years of my life.” Another student commented,“It was saddening to know there weren't enough beds for each resident, so the elderly patients were forced to share small beds with each other.” The residents of the elderly home were deeply moved by the visit from the students, as many of them had not received a visitor in years. The environment of the private orphanage provided a stark contrast to the Hogar de Ancianos. One student wrote, “The lives I had imagined they would be living before I arrived was radically different than what I saw that day and it made me feel happy knowing that they were in a much better place than most other people who lived outside their walls in the city.” While the children were fortunate to be taken into “the family” of the Ark Children’s Home, many of them had experienced abuse, abandonment, or both. For instance, one student wrote, referring to the orphanage, “Mi corazonestá en el Ecuador. Another student spoke of how not a single day passes without her thinking about Felipe [one of the kids]. They were also motivated to give to the orphanage as they saw what international donations and time could do for a child. Application to US Latino Population: Given the opportunity to stay with an Ecuadorian family, students were able to see the humble conditions that most Ecuadorians live in. Even being medical students that are in debt, each student could not help but gain a greater appreciation for his or her own quality of life in the US. Students feel that they will now have a better idea of where some of their Latino patients are coming from and why so many have immigrated to the US to find better quality of life. After experiencing the Ecuadorian people and their culture, the students feel they will be more receptive to the traditional beliefs and practices of their patients. Students also had ample opportunity to build relationships with people who did not speak English or Spanish. Students learned that Spanish proficiency was more than just “Medical Spanish.” Many of them left committed to improving their Spanish speaking abilities. CONCLUSIONS: Following the trip, student reflections on the elderly home and the orphanage were collected and published on the school web site. Students presented their experience to the FSUCOM community as part of the effort to spread awareness and inspire future groups to expand their knowledge of global health. The dedication of the medical professionals and volunteers encountered on the trip provided tremendous inspiration to the students in two ways: to continue medicine as a service instead of a lucrative career, and to increase service to theirown local underserved and Latinocommunities. Students began immediately upon return to volunteer in local free clinics as a result of this trip, and they gave time and money to support other patients in similar situations in our community. They have also committed to medical humanism, and many of them have produced thoughtful inspiring writing that will soon be published in a Humanism in Medicine journal. NAME: Julie St. John, MA, MPH UNIVERSITY: TX A&M Health Science Center School of Rural Public Health PHONE NUMBER: 956-202-2976 E-MAIL: jastjohn@srph.tamhsc.edu (Use additional space if needed) TITLE OF PRESENTATION: Hispanic Colonia residents along the South Texas border WIN: Women’s health Improvement Network PURPOSE OF RESEARCH: To demonstrate the effectiveness of utilizing promotores (community health workers) as service coordinators and to treat and detect breast cancer among Hispanic colonia residents in South Texas. METHODOLOGY: Local physician secures 250 free mammograms and the services of radiologists to read mammograms at no cost; - Recruit physicians from the local medical society to treat WIN clients needing additional follow-up care based on Medicaid reimbursement prices; - Design screening survey based on American Cancer Society risk factors; - Organize two large community screening events; - Prioritize screened women to receive free mammograms based on most to least number of risk factors; - Secure funding for specialty/follow-up care through a County grant for specialty care and case management/service coordination; - Train promotores (community health workers) in service coordination; - Schedule screening mammograms for WIN clients; - Send result letters; - Follow-up with clients with abnormal results and refer to primary care; - Promotores continue case management/service coordination for each client until case is closed. - Continue adding additional clients for screening mammograms based on available funds and provide service coordination/case management. - RESULTS: - Promotores (community health workers) trained in service coordination. - 606 women initially screened. - 250 Hidalgo County colonia women received free screening mammograms. - 31 of those original 250 clients needed follow-up up care. - To date, no breast cancer has been detected (one case of lung cancer). - 138 new clients were added in January 2009. - Project promotores are currently managing 147 WIN clients. - A total of 629 procedures and appointments (past and current pending) have been provided for clients by the WIN project. - 745 women have been served by the WIN project. CONCLUSIONS: - Promotores can be utilized to perform case management/service coordination to manage the disease process for clients in a culturally appropriate manner that is more cost effective (both in salaries and training) than traditional case managers/social workers. - There is some resistance in the medical field in working with promotores as case managers. - Hispanic women in South Texas felt comfortable in working with promotores in arranging needed services. - In the South Texas Health Status Assessment (2003) in Hidalgo and Starr Counties in South Texas, three-fourths of uninsured individuals (75.6%) reported having only “poor” or “fair” access to care, and over half (56.7%) often delayed care due to cost—this number increased to 84% for those without insurance. When provided resources for paying for needing tests and appointments, WIN clients DID NOT delay care and accessed needed services. NAME: Karin Reed UNIVERSITY: Wayne State University School of Medicine PHONE NUMBER: 562-761-1706 E-MAIL: karreed@med.wayne.edu (Use additional space if needed) TITLE OF PRESENTATION: A Clinically Relevant Rat Model of Controlled Hypothermia for Treatment of Brain Ischemia PURPOSE OF RESEARCH: Stroke and cardiac arrest affect over 1.1 million Americans annually, with indirect costs approaching $300 billion. The costs in human disability and suffering are incalculable. Risk factors for stroke, including hypertension, diabetes, and obesity, are more prevalent in Hispanics than non-hispanic whites, and pose a significant threat to this community. Hypothermia has a well-established neuroprotective effect on brain ischemia. Therapeutic hypothermia after resuscitation from cardiac arrest is increasingly used in the clinical setting, and may also find clinical application in focal ischemic stroke. Experimental models of hypothermia range from highly rudimentary (placing the animal in a “cold room”) to prohibitively elaborate. The state-of-theart is described by Colbourne et al, wherein an implanted brain temperature telemetry system is used to cybernetically control an array of heaters, misters and fans to maintain awake, freely-moving animals at target temperatures. Such systems, while effective and robust, are costly and impractical, and do not model clinical practice. Therapeutic hypothermia is usually instituted via water-cooled extracorporeal systems in conjunction with sedation, and with monitoring of body core temperature rather than brain temperature. We undertook the development and testing of a clinically relevant model of therapeutic hypothermia for use in the rat. METHODOLOGY: Several designs were attempted and discarded. Ultimately, veterinary warming blankets (REF TPI12E Mul-T-PadsTM) were purchased from Gaymar industries, resized for the rat, and re-sealed with a heat-sealer (Scotchpak). The pad was fitted to a gel transfer cooling tank (Multi-Temp IIITM, Amersham). Male Sprague-Dawley rats (N=5) were subjected to 2h focal brain ischemia under isoflurane/N2O using MCAO technique. Thermocouples (Physitemp) monitored brain, temporalis and rectal temperatures. Brain thermocouples were stereotactically implanted in the MCA distribution bilaterally. Mean arterial pressure, heart rate and blood glucose were monitored by arterial catheter. Hypothermia was instituted at the onset of reperfusion with an initial tank temperature of 15o C. Animals were sedated with lorazepam during the 4h hypothermic interval. Animals were reperfused for seven days, and brains were taken to cresyl violet staining to assess stroke volume. RESULTS: This system proved to be highly responsive and provided exquisite control of animal core and brain temperatures. Animals subjected to sham hypothermia showed no abnormalities in temperature, glucose or hemodynamics (not shown). Target temperature (32o rectal) was attained by 35 minutes all animals. Thereafter, core temperature was generally maintained to within 0.5o C. Difference between ischemic and contralateral brain temperatures was negligible. Brain temperatures were closely approximated by temporalis temperature, even during rewarming, when brain temperatures rose more slowly than core temperatures. Mean arterial pressure, heart rate and serum glucose did not undergo clinically significant fluctuations. Animals tolerated the procedure well. Evaluation of brains at sacrifice by inspection and TTC staining demonstrated appropriate placement of brain thermocouples. No significant temperature or hemodynamic differences were seen between sham-operated and non-ischemic animals. Because animals underwent invasive bilateral cranial surgery and short-term survival, a series of long-term-survival animals treated with hypothermia without invasive brain monitoring (using temporalis temperature as a surrogate value), incorporating evaluation of window-ofopportunity and dose-response properties, will be necessary to characterize the full neuroprotective value, if any, of this method. These studies are underway, and interim results suggest a robust neuroprotective effect. CONCLUSIONS: We have developed and characterized a novel experimental hypothermia system for use in small animals. This system is now being used for dose-response and window-of-opportunity studies, and will also find application in a translational study of therapeutic hypothermia and combination therapy in focal ischemic stroke. Neurohistological, neurobehavioral and biochemical data are being collected in nontreated ischemic animals, ischemic animals treated with hypothermia, and sham-operated controls. Because the model is both structurally and functionally similar to that used in current human models, successful interventions can be rapidly transferred to clinical human trials. NAME: Kelly Stimpert UNIVERSITY: Georgia State University PHONE NUMBER: 770-488-4355 E-MAIL: hen5@cdc.gov (Use additional space if needed) TITLE OF PRESENTATION: U.S. physicians’ knowledge of Chagas disease PURPOSE OF RESEARCH: Chagas disease, caused by the blood-borne parasite Trypanosoma cruzi, affects an estimated 100,000 or more Hispanic immigrants living in the United States. In the chronic phase, which can last for decades, the disease can be fatal. Because many people with Chagas disease do not have overt symptoms, it is important for physicians to recognize risk factors for the disease. Risk factors include a history of living in poor and often rural housing conditions of Latin America. It is hypothesized that a large number of physicians practicing in the U.S. are unfamiliar with Chagas disease, its diagnosis, and treatment. Knowledge deficits are particularly important for: (1) physicians serving the Hispanic population, as these patients are at an increased risk of having the disease, and (2) transplant surgeons, as infected persons may transmit the parasite that causes Chagas disease via organ transplantation. METHODOLOGY: Centers for Disease Control and Prevention (CDC) collaborated with the National Alliance for Hispanic Health (NAHH) to conduct a series of focus groups of Hispanic-serving physicians and their patients. These groups, which took place in four cities with large Hispanic populations, asked a variety of questions to determine participants’ familiarity with the disease. CDC also worked with Medscape LLC, the largest provider of online CME for physicians, to distribute a knowledge, attitudes, and practices (KAP) survey of physician members. Surveys were gathered online for approximately one month, on an opt-in basis only. Surveys targeted the following specialties: primary care, infectious disease, obstetrics/gynecology, cardiology, and transplantation. Approximately 1,000 surveys were completed. Questions from the studies included: familiarity with the disease, proportion of Hispanic immigrants patients served, and preferred sources for receipt of medical information. RESULTS: Preliminary results from both studies indicate a significant Chagas disease knowledge deficit in both the Hispanic community and the physicians that serve it. Physicians, including those serving Hispanic patients, rarely consider Chagas disease as a potential diagnosis, are unfamiliar with the etiology and manifestations of the disease, do not feel confident in their knowledge level of the disease, and express an interest in follow-up information regarding Chagas disease. CONCLUSIONS: Because the majority of physicians do not consider Chagas disease as a potential diagnosis for their patients, Hispanic persons living in the U.S. may not be appropriately diagnosed or treated for the disease. The results of these studies will be utilized: (1) to advocate for funding of Chagas disease research and outreach efforts, (2) educational activities directed to both healthcare providers and the public including print, electronic, and other media material in both English and Spanish. Additional studies are planned to more formally evaluate knowledge, attitudes, and practices for Chagas disease in the United States. Ultimately, this research will improve health outcomes for Hispanic immigrants living in the U.S. NAME: Bruneus Magalie , Medical Student ( Advisors: Dr Wylie-Rosett, Dr Hays) UNIVERSITY: Albert Einstein College of Medicine PHONE NUMBER: 347-420-7037 E-MAIL: mbruneus@aecom.yu.edu (Use additional space if needed) TITLE OF PRESENTATION: A review of the efficacy of recent clinical interventions in the management of chronic kidney disease (CKD) due to diabetes PURPOSE OF RESEARCH: Based on world wide epidemiological and pathophysiological studies, chronic kidney disease is a public health problem which may lead to end stage renal disease, renal transplant and is associated with an increased risk of cardiovascular disease and carries an enormous economic burden. There are more studies that describe the prevalence of CKD than ones that deal with the efficacy of goal-directed interventions to delay the progression of this disease. The aim of this report is to highlight specific interventions that have been proven to be successful in altering the course of this disease by increasing the patient’s adherence to therapy. We will specifically focus on the diabetic population with chronic renal insufficiency or advanced chronic kidney disease (greater than stage 3 or pre-dialysis) and compare various domestic and international approaches that have shown significant results. METHODOLOGY: We reviewed randomized controlled trials that evaluate the efficacy of educational and nutritional interventions as an adjunct to standard pharmacological therapy or as part of a community based intervention in adults older than 19 years of age with diabetic nephropathy or CKD. A literature search review was done using various key words and MESH terms via Cochrane review, Medline, EMBASE, PubMed and the National Kidney foundation website. Using the data obtained, a direct comparison of the outcomes of these interventions was done to assess their efficacy. Outcome measures were reduction in calculated glomerular filtration rate, creatine clearance, number of years before dialysis, survival rate after dialysis, increased awareness of CKD and improved psychosocial adaptation and greater adherence to dietary modification, fluid restrictions and treatment. RESULTS: The interventions found were mostly nutritional counseling, small group sessions, educational pamphlets, short videos, follow-up telephone calls, training of nurse practitioners and other primary care providers, identification and solution to barriers to therapy prior to starting dialysis and structured educational sessions with an informational and psychosocial component and even short-term hospitalizations. In contrast to the control groups, patients of comparable serum creatinine levels in the interventional groups experienced a lesser decrease in glomerular filtration rate over time, improved creatinine clearance, a greater recognition and awareness of CKD, longer survival rates after dialysis initiation, better adherence to fluid restrictions, dietary modifications and greater physical and psychosocial adaptations to this chronic illness as assessed by standardized questionnaires. CONCLUSIONS: Due to the heterogeneity and paucity of the available data that was evaluated, a direct contrast between the interventions was difficult to perform. However, the current data suggest that multidisciplinary interventions have been proven to be more effective in helping to delay the progression of CKD. Health care providers, including Diabetic educators can play a significant role in helping to alter the course of chronic kidney disease in diabetic patients. More studies are needed to further refine these models and perhaps these current studies can serve as an impetus to explore other potential interventions with clear goal-directed results for earlier stages of CKD to achieve a greater impact on this growing public health issue. NAME: Christina Mangurian, MD UNIVERSITY: Columbia University PHONE NUMBER: 212-543-6020 E-MAIL: cm2195@columbia.edu (Use additional space if needed) TITLE OF PRESENTATION: Adaptation of a Weight Loss Program for Latino Patients in a Community Mental Health Clinic PURPOSE OF RESEARCH: Patients with severe and persistent mental illness (SPMI) lose more than 25 years of potential life in comparison to the US general population. The leading cause of this increased mortality is cardiovascular disease, related in part to increased prevalence of risk factors like obesity, dylipidemia, hyperglycemia and hypertension. Latino patients with severe and persistent mental illness (SPMI) have a higher prevalence of the metabolic syndrome than schizophrenia patients in CATIE or Hispanics in the US, suggesting additive risk and a highly vulnerable population. A major risk factor for the metabolic syndrome is obesity. Behavioral weight control techniques have been shown to be effective in overweight/obese SPMI patients. However, there is almost no information on the effectiveness in higher risk populations, such as low-income Latino SPMI patients. Ganguli developed a behavioral therapy approach for overweight SPMI patients. For this study, we culturally modified Ganguli’s manual to determine if it could be feasibly delivered and effective in Latino SPMI patients METHODOLOGY: Subjects: The Washington Heights Community Service (WHCS) provides inpatient and outpatient services for SPMI patients living in Northern Manhattan. About 60% of the patients have schizophrenia spectrum disorders and 30% have bipolar disorder. The WHCS serves approximately 60% women and 40% men; with an ethnic distribution of 75% Hispanic, 15% African American, 9% Caucasian, and 1% Asian. The high proportion of Hispanic patients creates a unique opportunity to assess the efficacy of a behavioral treatment in this high risk group. Procedures: Ganguli’s protocol was translated to Spanish and modified to be culturally sensitive to this population. WHCS day-program patients with BMI greater than or equal to 25 were identified, informed consent was obtained, and baseline characteristics were collected. Primary outcome measures were course attendance and weight. After initial assessment, a 14-week culturally-modified behavioral therapy course was held. All participants were given pedometers and scales. After completion of the course, patients were re-weighed. Paired t-tests and the Sign test were used to examine pre-post effects on weight. RESULTS: 89% (65/73) of the day treatment patients were eligible for the study. 78% (51/65) consented to participate, with 20% (13/65) refusing and 2% (1/65) having a work conflict. The average age was 49 years old (range 23-79 years). 79% were female and 21% male. Most were Latino (83%), predominantly Dominican (79%); with the remaining 10% Caucasian, 3% African American and 3% other. Most participants (86%) were on atypical antipsychotic medications. Many also took medications to control metabolic co-morbidities, including antihypertensives (31%), hypoglycemics (17%), and lipid lowering medications (28%). Due to room availability, only some patients could be offered the course immediately. We present the preliminary results of those 29 patients. 90% (26/29) of the patients attended over half of the classes. The mean pre-course weight was 179.7lbs (SD=36lbs) and post-weight was 178.2lbs (SD=36lbs). Because some patients gained weight taking the course, the paired t-test was not significant. However, more patients were found to lose weight than gain weight (p=0.043), with 69% (18/26) losing weight, 4% (1/26) maintaining weight, and 27% (7/26) gaining weight. The three patients eligible for but not attending the class gained a mean of 2.67 lbs over the same time period, with only one losing weight and two (67%) gaining weight. CONCLUSIONS: This study provides preliminary evidence that a culturally-modified behavioral weight reduction course is feasible to implement for Latino SPMI populations treated in community settings, and further preliminary evidence that such a course can favorably affect body weight compared to no treatment. NAME: Mario Lopez and Tomas Mercado UNIVERSITY: University of Illinois PHONE NUMBER: 773-979-2525; 312 919-8169 E-MAIL: mlopez18@uiuc.edu; tmerca1@uiuc.edu (Use additional space if needed) TITLE OF PRESENTATION: Analgesic Use in Six Urban Emergency Departments PURPOSE OF RESEARCH: The objective of this study was to analyze analgesic use, route, dose, frequency of administration and time to treatment for patients presenting to the ED in pain due to migraines/cephalgia, wrist or ankle fractures, renal colic or abdominal pain due to cholecystitis or bowel obstruction. METHODOLOGY: Patients were prospectively surveyed at the time of discharge regarding the management of their pain and a retrospective review of their charts was completed. Pain severity, analgesic therapy, time to analgesic therapy, diagnosis, and patient disposition were determined. RESULTS: Of the 1652 patients analyzed, 1145 (70%) were assessed by a nurse using a pain scale. Of those assessed by a nurse, 61.5% rated their pain as severe (8-10), but only 55% were administered an analgesic. Approximately 22.5% of 1652 patients received an analgesic in 30 minutes or less after triage time. However, 30% of patients received an analgesic in two hours or more after triage time. Approximately 14% of patients that reported severe pain (8-10), received an analgesic in 30 minutes or less after triage time. However, 48.7% received an analgesic within 1-2 hours. The most commonly administered analgesics in the Emergency Department were morphine (16.6%), toradol (9.7%), and demerol (7.1%). Non-steroidal anti-inflammatory drugs (NSAIDs) were most often given to patients diagnosed with migraines, renal colic, upper and lower fractures. Patients diagnosed with abdominal pain due to cholecystitis or bowel obstruction most often received narcotics, most commonly morphine. Cholecystitis patients were administered morphine at a rate of 17.1% and bowel obstruction patients at a rate of 20.5%. The route of analgesic administration varied according to final diagnosis and analgesic type. The majority of non-narcotics were administered parenterally except for lower and upper fracture patient, to which were administered orally. The majority of narcotics were administered parenterally. The only exceptions to this were the lower and upper fracture patients, who were administered their narcotics both orally and parenterally. Approximately 62.5% of ED patients in the study received intravenous (IV) fluid intervention. Confirmation of final diagnosis was most frequently carried out with urinalysis, chemistry and CBC for renal colic. CBC, Chemistry, and CT of the head were more frequently employed for migraines. Confirmation of final diagnosis was most frequently carried out with a wrist x-ray for upper fractures, ankle x-ray for lower fractures. Also, amylase, CBC, and Chemistry tests were used for abdominal pain due to cholecysistitis and CBC, Chemistry and urinalysis for abdominal pain due to bowel obstruction. Approximately 65% of patients were sent home. CONCLUSIONS: A large majority of ED patients with significant painful conditions report initial pain to be severe. However, studies have reported that only a minority of these patients receive analgesics (reference?). Our retrospective analysis of ED patients from six urban hospitals diagnosed with renal colic, migraines, upper fractures, lower fractures and abdominal pain due to cholecystitis or bowel obstruction demonstrated a larger than expected proportion to receive analgesics. Of the 1652 patients analyzed 77% received an analgesic. Out of these patients, 22.5% of them received pain medication within 30 minutes, and roughly 30% of then received analgesics 2 hours after triage time. Approximately 90% of patients who reported severe pain (8-10) were given an analgesic but only 14% received an analgesic in less than 30 minutes, 50% within 1-2 hours and approximately 26% after 2 hours. Administration of analgesics and analgesic type is correlated with final diagnosis. Patients diagnosed with renal colic, migraine, or cholecystitis are more likely to be administered an analgesic compared to patients who present themselves with bowel obstruction, or fractures. Pain pharmacotherapy in the ED for these common diagnoses is predominated by narcotics, especially morphine (16.6%). Furthermore, the method for initial pain assessment was not consistent among the nurse and physician. Nurses were more likely to assess pain using a pain scale whereas physicians frequently wrote degree of pain or pain type on the patient’s chart. NAME: Lindsay Withers, Lauren Hughes, Mary Puttmann, Scott Robinson, Andrew Bazemore UNIVERSITY: The Robert Graham Center, Georgetown University SOM PHONE NUMBER: 513-505-7441 E-MAIL: Mary.M.Puttmann@gmail.com (Use additional space if needed) TITLE OF PRESENTATION: Health center mapping for migrant health centers: Challenges and benefits of transitioning to geographic information systems (GIS) use. PURPOSE OF RESEARCH: HealthLandscape is a geographic information systems (GIS) mapping tool developed to allow community health centers the capability of creating visual representations of patient data. The potential for GIS use in migrant clinics is immense, but often, there is a steep learning curve in adopting the system. We wanted to know what elements of the program were appealing to clinics and how best to conduct training sessions for use of the tool. METHODOLOGY: We reviewed the literature on GIS use in community clinics and on demographic and health data of migrant workers in the United States. Through partnership with Salud Migrante, a technical group investigating bi-national health insurance, we contacted four clinics/primary care associations. We provided each clinic with a survey regarding their strategic goals and anticipated use of HealthLandscape. We were particularly interested in whether clinics could use the tool for mapping service areas, projecting demand for health center services, defining the target population, identifying areas for health center expansion, and characterizing the local safety net health care services. We then arranged training sessions with the clinics and responded to questions regarding data entry and use of the program. RESULTS: Preliminary results from the three surveys back showed a variety of responses. While one clinic did not really see a role for HealthLandscape in achieving their strategic goals, other clinics have been using the program for some time. Training sessions helped to clarify many of the uncertainties clinic directors had and served as useful interactive sessions. CONCLUSIONS: This is phase one of a multi-step project to be continued through 2009. There were several barriers to successful adoption of HealthLandscape. First, how to incorporate a mapping tool for strategic planning was not self-evident for some clinic directors. Second, various data formatting issues arose. These required a significant time commitment on the part of the participating clinics to clean and prepare for mapping. Finally, the clinics are spread throughout the United States, and so opportunities for in-person meetings and exchanges are limited. Instead, training sessions were often difficult as they relied on desktop-sharing software and conference call lines. There have been several successes, however. Several clinics have uploaded their data and are delving into further analysis now that they are more comfortable using the web-based program. HealthLandscape has the potential to be a crucial tool in evaluating patient data, seeking funding, and designing outreach programs. The next phase will examine what information is available to answer these questions and how they are put into practice. NAME: Michelle Shuff UNIVERSITY: University of California, San Francisco and UC Berkeley PHONE NUMBER: 858-336-8475 E-MAIL: michelle.shuff@ucsf.edu (Use additional space if needed) TITLE OF PRESENTATION: Barriers to Accessing Quality, Safe Abortion Services in Mexico City: A Multi-Disciplinary Qualitative Study PURPOSE OF RESEARCH: In April 2007, Mexico City legalized first-trimester abortions and mandated that the Secretary of Health create programs to meet the demand of these services and provide abortion services to low-income women in an effort to continue to meet the UN Millennium Goal Five of decreasing maternal mortality. This process literally was changed overnight and programs had to be erected from scratch. The Secretary of Health has made both medical and surgical abortion available in 14 public hospitals throughout Mexico City. Thousands of women from the Mexico City and other states have been treated since. Although the Secretary of Health has made tremendous achievements in making safe, legal abortion accessible to all women, there has not been an interdisciplinary analysis assessing barriers and opportunities to give policy recommendations in order to improve access. Goals of this project: 1. Describe the main issues in abortion service and access in Mexico City almost 2 years since legalization. 2. Describe the overall opinions and experiences of experts from a variety of disciplines on the legal abortion program in Mexico City. 3. Identify the main barriers to access.4. Create clear policy recommendations that will be useful to the Secretary of Health and other decision-makers in Mexico City. METHODOLOGY: 11 in-depth interviews with key informants in Mexico City were conducted with specialists from a variety of disciplines including: directors of advocacy groups, clinic directors, research directors, and directors of the Secretary of Health (responsible for the implementation and oversight of all abortion services in the public sector). All interviews were voice-recorded and conducted in English, Spanish or both. The data will be transcribed, coded and analyzed using the software Atlas-ti. RESULTS: Preliminary analysis suggests that barriers can be organized in 3 major categories: Lack of Supply of abortion providers, supply of medication, lack of information. The supply of abortion providers in the city is a major problem for many reasons. First medical abortion and manual vacuum aspiration (MVA) must be performed by a surgeon or an Ob/Gyn. This is a major barrier because this level of specialization would generally not want to concern themselves with performing a simple procedure such as an MVA; they would prefer to use their training to attend to issues more complicated. In addition to the limitations of the pool of doctors who are legally permitted to perform abortions, the majority (85%) of these doctors choose to “consciously object” to providing these services for many reasons: fear discrimination within the medical community, religious reasons, fear ruining family reputation, and no monetary incentive to perform abortions (those who are performing have much longer work hours with no extra pay). Because there are only 38 providers in the public sector, there are long waiting times and some women must return to the hospital multiple days or if they have enough money they can go to a private clinic. The hospital itself presents another barrier to service since there are multiple levels of people that a woman will encounter when she enters the hospital. Women have faced discrimination from hospital police officers, social workers, nurses, administrators, and the physicians themselves. They have been erroneously charged for services, told the hospital doesn’t have that service, or simply treated in an inhuman manner. There are many more barriers that will be teased out during the final analysis that will provide more insight to decision-makers to make policy changes. CONCLUSIONS: Several policy recommendations can be offered based on preliminary findings: 1. Increased abortion-training programs for current physicians and for those in training, which would allow more types of practitioners in places where abortion is legal in order to 2. 3. 4. 5. meet the demand of patients and to replace those who are conscientious objectors of abortion. Abortion Guidelines created by the World Health Organization must be strictly followed and evaluated for quality and efficacy. Facilities that provide free abortion must be held to the strict standards as mentioned above and must be required to go through a re-training program such that services are done in a culturally appropriate, non-judgmental and compassionate manner. Physician educational and desensitization programs should be erected with the goal of encouraging discussion of abortion and thus changing attitudes of abortion. Attitudes are often greatly influenced by the environment and thus this may lead to more acceptances of abortion or at least to decrease such negative feelings toward it. This has shown to be true in the city itself of México City, as the citizens have been slowly accepting it more and more especially since the legalization, which allows for the behavior to be normalized. Allowing other practices that normally would not offer abortion service, such as a family practice clinic, the opportunity to provide medication abortion services. This has been shown to work well in rural areas of the US and other countries. 6. Legalize Mifepristone in Mexico City for use by practitioners, both physicians and Nurse Practitioners who perform medication abortion in order to follow current guidelines recommended by the WHO for safe first trimester abortion. 7. Create Guidelines for dispensing Misoprostol in México City pharmacies: if a pharmacy is to dispense it, he or she must discuss all uses and include instructions for use. This has been done in the United States when Plan B was first legalized to be dispensed in pharmacies without a physician’s prescription [14]. This can be expanded to other cities in Mexico but may be challenging due to the anti-choice sentiment of the Catholic community leaders. Other potential dangers are that this could lead to Misoprostol being taken off the pharmacy shelves in other parts of Mexico where abortion is still illegal. A Summer Preceptorship in Family Medicine: An Early Medical Student Experience Elizabeth Natal, M.D (Instructor) Alice Fornari, Ed.D (Associate Professor) Albert Einstein College of Medicine Family Medicine Department, Mazer 100 1200 Van Nest, Bronx NY 10461 718-772-2375 (m) 917-317-3830 (p) ENATAL@montefiore.org or Elizabeth_Natal@msn.com Background: With an aging and culturally diversifying population, we require a larger primary care work force to meet its medical needs. Medical institutions need to engage in activities to increase student awareness about primary care fields. To this end, a two-week summer preceptorship was created for medical students interested in learning more about Family Medicine as a primary care specialty that can address the needs of a growing diverse population, particularly a growing Hispanic population. Goals: To describe: 1. essential steps and tools used to plan, implement and evaluate a two-week summer preceptorship in Family Medicine. 2. successes and challenges of a two-week preceptorship. Methods: Preceptorship goals and necessary resources were discussed with the Dean and Department Chair. Participating students completed a two-week block. The faculty coordinator prepared materials, schedules and communicated with participants. Students rotated through ambulatory clinic settings, the Family Medicine inpatient ward and rounded with the Family Medicine Hospitalist. Students evaluated preceptors, completed a survey about their experience, wrote a self-reflective piece and participated in an evaluative focus group. Faculty members provided individual feedback to students. Results: Forty Family Medicine preceptors participated. Six students participated. Physician contact, practice variety, population diversity and rounding with the Family Medicine Hospitalist were highlighted as strengths. Suggestions for improvement included lengthening the preceptorship, adding orientation day and providing clinic population information. Two students expressed interest in a Family Medicine advisor. Conclusion: An early preceptorship model introduces students to Family Medicine as a primary care specialty serving the needs of underserved communities, in this case predominantly Hispanic communities. Designing a quality educational experience requires faculty leadership and support from the school and department. Implications: A preceptorship can enhance student interest in Family Medicine, increase awareness about primary care as a specialty and hopefully increase student interest in pursuing primary care professions. A breastfeeding educational workshop for Family Medicine Physicians: an interactive problem-based approach. Elizabeth Natal, M.D (Instructor) Surah Grumet, M.D., M.P.H (Instructor) Montefiore Medical Center Family Medicine Residency Program in Social Medicine 3544 Jerome Avenue, Bronx, NY 10467 2nd Floor, Dept #: 718-920-5521 Contact person: Elizabeth Natal Contact numbers: 718-772-2375 (m) 917-317-3830 (p) ENATAL@montefiore.org & SGrumet@montefiore.org Background: Despite known benefits of breastfeeding, declining rates has been the center of much debate. Leading organizations have campaigned to increase the support of exclusive breastfeeding. Physician knowledge and skills is an important component of breastfeeding counseling. It is well documented that residents have limited knowledge about common breastfeeding problems. In this study physicians serving a predominantly Hispanic and African American population were introduced to a workshop activity to provide them with knowledge and skills for effective breastfeeding counseling. Goals: To: 1. utilize a newly created workshop to enhance physician breastfeeding knowledge, attitudes and skills. 2. initiate a dialogue about the politics of breastfeeding. 3. review effective techniques with Family Medicine Faculty to enhance breastfeeding counseling efforts during precepting. Methods: In a recent study conducted at the Montefiore Family Medicine Residency program, physicians indicated a need for additional breastfeeding education. An online survey, based on the American Academy of Pediatrics survey, was emailed to physicians prior to a workshop intervention, to assess baseline breastfeeding knowledge, attitude and skills. The residents participated in 75 minute educational workshop. Faculty participated in 90 minute workshop focusing on key precepting techniques. Both interventions included didactics, instructional videos and problem-based role playing. After the workshop, the email survey was re-administered to participants to assess the impact of the intervention. Results: Statistical analysis is being performed utilizing the chi-square test and confidence intervals. Conclusions: Preliminary review of results is promising for positively impacting Resident and Faculty knowledge and skills. To assess attitude we will look for changes in physicians’ desire to more actively engage in breastfeeding counseling. Implications: Interventions which can enhance physician knowledge and promote breastfeeding counseling to physicians caring for large Hispanic populations will hopefully result in enhanced breastfeeding services and greater patient support to increase breastfeeding rates to meet HP2010 breastfeeding goals. NAME: Nicole de Jesus, Amy Haddock, Karina Walker, Dr. Jose Rodriguez UNIVERSITY: Florida State University College of Medicine PHONE NUMBER: 850-621-5384 E-MAIL: klw08f@med.fsu.edu (Use additional space if needed) TITLE OF PRESENTATION: Analysis of Availability and Accessibility of Primary Health Care in Leon County, Florida PURPOSE OF RESEARCH: The purpose of our research is to determine the availability and accessibility of primary health care providers as well as facilities that aid in healthcare maintenance for the Latino community in Leon County Florida. We propose that our efforts will help identify factors, in addition to socioeconomics, that prevent members of our community from receiving the health care they need and deserve. METHODOLOGY: Our plan involves the geographic mapping of primary care physician offices, hospitals, pharmacies, lab facilities, county health services, recreational facilities, grocery stores, and public transportation. In addition to our mapping procedure we will also survey a physician’s office staff representative for all participating primary care providers in Leon County. The survey will include questions regarding appointment availability, insurance acceptance, and Medicaid/Medicare acceptance. We will also inquire about services for members of the Spanish speaking community such as the availability of patient education materials in Spanish translation and patient translation/interpretation services. We will survey practitioners in primary care to include family medicine, internal medicine, pediatrics, geriatrics, and obstetrics/gynecology. We are currently mapping all areas of our community, and will focus on low income and minority, Latino areas. RESULTS: Preliminary results indicate that our community has disproportionate access to medical care. Initial mapping reveals that the highest concentration of medical providers is in one of the most affluent areas of our community. Areas of our community with high proportions of Latino and African American residents are shown to be severely underserved by medical professionals, both primary care and sub specialists. This observation indicates that the poorest members of our community must travel the greatest distance to receive medical care. In addition, a great majority of the medical practices in our community are closed to new Medicaid or Medicare patients. Our community has very few public transportation routes, which further increases the difficulty of accessing a practice that accepts Medicaid or Medicare. Preliminary comparison of different sections of our community also reveals that the rural areas (40% Latino) have the largest barriers to care, including lack of interpretation, acceptance of Medicaid and distance to health care facilities. CONCLUSIONS: This project documents the barriers to care for Latino and African American populations, as well as rural populations in our area. The findings from our study will be used to guide the research of other students and will help both providers and patients understand how primary health care is distributed in our community. Our findings will be presented to local heath care advocacy groups in effort to seek solutions to this ever increasing crisis. It is our hope this research will help inspire other students and health care providers to serve in our Latino and African American communities of Leon County Florida. NAME: Elizabeth Lee-Rey, Frank Penedo, Kiang Liu, Lorraine Silsbee , Paul Sorlie, Kant Bangdiwala, Greg Talavera UNIVERSITY: The Hispanic Community Health Study / Study of Latinos (HCHS/SOL) Investigators PHONE NUMBER: 718-430-4076 E-MAIL: rkaplan@aecom.yu.edu (Use additional space if needed) TITLE OF PRESENTATION: Career Development and Collaboration Opportunities in t he Hispanic Community Health Study / Study of Latinos (HCHS/SOL) PURPOSE OF RESEARCH: HCHS/SOL is a multicenter collaborative study of Hispanic/Latino communities. In addition to addressing specific research aims, HCHS/SOL has the goals of 1) providing opportunities for ancillary studies addressing additional research questions; and 2) providing training and career development for minority investigators. METHODOLOGY/RESULTS: HCHS/SOL is a prospective cohort study of health and disease among 16,000 Hispanic/Latino adults in four US communities (Bronx, Chicago, Miami, and San Diego). HCHS/SOL offers many career development and collaboration opportunities. This includes opportunities for academic projects and theses using HCHS/SOL data. Ancillary studies may be proposed, which are investigations that address a research question that is not funded under the main HCHS/SOL study. Ancillary studies typically require outside funding for collection of additional data from participants enrolled in HCHS/SOL, or laboratory measurements from stored HCHS/SOL biospecimens. The study Publications Committee also accepts proposals for data analyses, manuscripts, and presentations using HCHS/SOL data. Investigators interested in working with HCHS/SOL are not required to be located at one of the funded study centers but should seek sponsorship from one of the HCHS/SOL investigators. CONCLUSIONS: The HCHS/SOL scientific website provides information about the study design, protocols, ancillary studies, and manuscript proposals. Visit http://www.cscc.unc.edu/hchs. NAME: Aida Giachello , Brendaly Rodriguez, Joann Casado, Vanessa Torres, Natalie Meza, Paula Gildner, Larissa Avilés-Santa UNIVERSITY: The Hispanic Community Health Study / Study of Latinos (HCHS/SOL) Investigators PHONE NUMBER: 718-430-4076 E-MAIL: rkaplan@aecom.yu.edu (Use additional space if needed) TITLE OF PRESENTATION: Community Relations in the Hispanic Community Health Study / Study of Latinos (HCHS/SOL) PURPOSE OF RESEARCH: HCHS/SOL is a community-based epidemiology study of 16,000 Hispanic/Latino adults at Field Centers in four US communities (Bronx, Chicago, Miami, and San Diego). Success of the study depends upon recruitment of study participants, and retention of participants during the longitudinal phase of the study. The HCHS/SOL study aims also include providing community education and feedback regarding study findings, as well as providing information to improve the health of the communities in general. METHODOLOGY/RESULTS: The community relations activities in HCHS/SOL have three main objectives: a) to build community partnerships; b) to promote the HCHS/SOL through outreach and media campaigns; and c) to engage in community education. As a result, each of the four HCHS/SOL Field Centers has involved community stakeholders in local community advisory groups. The study also has a Community Relations Committee (CRC) that monitors the efforts to achieve these objectives; in particular, this includes encouraging the participation of national and local Hispanic organizations and leaders in the development of strategies for recruiting study participants and for maintaining community interest and support. Outreach activities include making presentations about the project to community block clubs, local places of worship, community-based organizations, consulate offices representing countries of origin, and other fora. Targets for outreach include potential study participants, as well as the larger Hispanic/Latino community. Bilingual study marketing materials include: posters, fact sheets, brochures, and local and national media campaigns carried out with the pro bono assistance of a Hispanic media firm. CONCLUSIONS: Community outreach is critical to the success of the HCHS/SOL project. NAME: LISA LAVANGE, MARTHA DAVIGLUS, JANICE BARNHART, LEOPOLDO RAIJ, GREG TALAVERA, LARISSA AVILÉS-SANTA, PAUL SORLIE UNIVERSITY: The Hispanic Community Health Study / Study of Latinos (HCHS/SOL) Investigators PHONE NUMBER: 718-430-4076 E-MAIL: rkaplan@aecom.yu.edu (Use additional space if needed) TITLE OF PRESENTATION: Design of the Hispanic Community Health Study / Study of Latinos (HCHS/SOL) PURPOSE OF RESEARCH: Data from previous studies show that US Hispanics/Latinos on average have lower coronary heart disease mortality rates, increased prevalence of obesity and diabetes, and fewer economic resources than the nonHispanic/Latino population. Validation of these findings is needed in more current studies with a diversity of Hispanic/Latino populations represented. The Hispanic Community Health Study / Study of Latinos (HCHS/SOL) is a longitudinal cohort study of 16,000 Hispanic/Latino adults recruited at four Field Centers. The research objectives of HCHS/SOL are: 1) To identify the prevalence of and risk factors for chronic diseases in US Hispanic/Latino adults; 2) To determine the role of acculturation and disparities in health and disease. HCHS/SOL addresses a wide variety of conditions, including heart disease, stroke, asthma, chronic obstructive lung disease, sleep disorders, dental caries, hearing impairment and tinnitus, diabetes, kidney and liver disease, and cognitive impairment. METHODOLOGY/RESULTS: Latino/Hispanic adults are recruited from randomly-selected households within each of the four designated HCHS/SOL communities (Bronx, NY; Chicago, IL, Miami, FL, San Diego, CA). HCHS/SOL participants attend a baseline clinic visit at a Field Center, which involves in-person administration of questionnaires, collection of clinical data, and blood and urine collection. Participants are contacted annually. The annual contacts obtain information on any doctor or hospital visits, and gather updated data on key health-related variables. During the follow-up phase of the study, primary cardiovascular outcomes include myocardial infarction, stroke and heart failure, and primary lung disease outcomes include chronic obstructive lung disease and asthma. CONCLUSIONS: The large sample size, inclusion of Hispanics/Latinos of diverse origins, population-based sampling approach, and longitudinal design of HCHS/SOL will help us to understand the causes of chronic diseases among Hispanics/Latinos and to identify strategies for their prevention. Results will inform policy makers regarding opportunities to reduce Hispanic/Latino health disparities. NAME: Sara Prieto UNIVERSITY: University of Illinois at Chicago PHONE NUMBER: 847-962-8346 E-MAIL: sprieto@uic.edu (Use additional space if needed) TITLE OF PRESENTATION: Promotora/Pharmacist Case Management of Latinos with Diabetes PURPOSE OF RESEARCH: There is a need to improve blood sugar levels of Latino patients with uncontrolled diabetes. This study evaluated the feasibility of Promotora/Pharmacist Case Management to address the barriers to medication adherence and adjustment and improve self-care. METHODOLOGY: We identified and trained a Promotora (community health worker) in diabetes self-management and health system navigation. We recruited Latino patients through the University of Illinois at Chicago Medical Center with uncontrolled diabetes receiving complex therapy. The Promotora worked with patients through home and clinic visits and phone support to provide education and address psychosocial barriers. The Promotora communicated with a pharmacist to receive assistance in medication management (reconciliation and adjustment). Participants received case management for 4-6 months. RESULTS: Of 55 patients referred for case management, six women and three men were successfully recruited. The mean age was 58 years and mean duration of diabetes was 21 years, and all had medical insurance (eight with public aid). The Promotora identified barriers to medication use including: fear, lack of knowledge and support, miscommunication, language, depression, cost, and transportation. The Promotora, with assistance from the clinic pharmacist, provided: education, social support, translation services, assistance in reducing drug cost, help in medication reconciliation, glucose monitoring, and medication adjustment. Promotora contact time in-person per participant ranged from 0 to 640 minutes, and phone call time ranged from 27 to 111 minutes during the study period. Eight participants had medication adjustments during the study period, with a maximum of seven adjustments per participant. Mean hemoglobin A1c declined from an average of 9.7% to 9.1%. Two participants demonstrating significant improvement in medication adherence and glucose control are described. CONCLUSIONS: We demonstrated that Promotora/Pharmacist Case Management is a feasible way to improve medication adherence by intensively addressing individual Latino patient barriers. Further research with a large sample is necessary to determine the long-term outcomes of this unique form of patient support. Also, there is a need to identify which individuals would most benefit from this case management. NAME: Yelile Maria Saca Kirbiyik UNIVERSITY: Columbia University, Mailman School of Public Health PHONE NUMBER: 917.232.5812 E-MAIL: yelile.saca@cdph.ca.gov (Use additional space if needed) TITLE OF PRESENTATION: Gender and Culture: More Matters PURPOSE OF RESEARCH: This presentation discusses strategies for improving the long term successes of Latino adult participants in two different behavior change programs (1) A social marketing campaign’s nutrition education intervention and (2) A web based smoking cessation program. The ultimate goal is to reduce inefficiencies and errors that can arise when researchers fail to consider gender and culturally/linguistically appropriate elements within their health interventions. METHODOLOGY: Evidence is primarily based on secondary sources and formative research, including informal interviews. While there will be a brief discussion related to best practices in market segmentation, most examples will involve two case studies; the Network for a Healthy California Latino Campaign’s social marketing efforts among low-income Latinos living in California and UCSF’s Latino Mental Health Research Project. RESULTS: By including gender based strategies and a culturally/linguistically appropriate perspective, public health programs can improve the effectiveness of their messages targeting Spanish speaking audiences. In addition, by implementing the market segmentation best practices learned from the private sector, public health interventions can more effectively meet the existing needs of Latinos that struggle with adopting healthier behaviors. Finally, attendees will learn how to capitalize on the role of the individual and the family when implementing successful interventions that seek to increase fruit and vegetable consumption, increase levels of physical activity and reduce cigarette consumption. CONCLUSIONS: Attendees will understand how to: apply a gender based perspective when designing a public health social marketing campaign apply a culturally/linguistically sensitive perspective when designing health education materials