POLICY & PROCEDURE
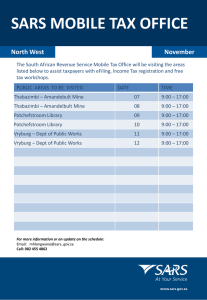
advertisement

POLICY & PROCEDURE MANUAL: NO. PAGE 1 OF 8 DATE: REV. DATE INFECTION CONTROL SECTION: VI - Significant Organisms APPROVED BY: POLICY PROCEDURE June 2003 GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH HIGH RISK PATIENTS PREAMBLE: During certain high-risk procedures that generate droplets and aerosols, health care workers may be exposed to a very high burden of respiratory secretions. Highrisk procedures include, but are not limited to the following: - administration of aerosolized/nebulized therapy - Intubation/extubation - Bag-valve mask ventilation - Tracheostomy - Chest tube insertion - Cardio/pulmonary arrest (may include any of the above procedures) - bronchoscopy - non-invasive ventilation (CPAP, BiPAP) - needle thoracotomy/open thoracotomy thoracostomy High risk procedures should be avoided whenever possible. However, in situations where they become necessary (e.g. intubation of a patient in respiratory distress), staff must follow the additional level of precautions outlined in this policy and procedure. Areas where high-risk procedures on high-risk patients may be performed include: a) Emergency Department b) ICU c) Rooms in which patients are placed on Droplet and/or Airborne Precautions d) OR High-Risk patients include: Patients - with an infectious respiratory disease (e.g. TB, probable or suspect SARS, or patient under investigation for SARS) - who develop new onset of symptoms (unexplained cough, unexplained high fever, hypoxia, shortness of breath or difficulty breathing) - with Congestive Heart Failure with/without concurrent pneumonia - with Exacerbation of COPD - with Exacerbation of Asthma - with pulmonary infiltrates and presumptive diagnosis (not SARS) Patients transferred - from a (SARS) Level 2 hospital - from a (SARS) Level 3 hospital POLICY & PROCEDURE MANUAL: NO. PAGE 2 OF 8 DATE: REV. DATE INFECTION CONTROL SECTION: VI - Significant Organisms APPROVED BY: POLICY PROCEDURE June 2003 GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH HIGH RISK PATIENTS 1.0 POLICY: 1.1 High risk procedures will be performed: i) in a private room with negative pressure, whenever possible (negative pressure rooms currently located in - ER Rm. 8, ICU Rm. 124, Medical Unit Rm. 165, Surgical Unit Rm. 264) ii) by the most experienced staff (whenever possible) iii) with a minimum number of staff present in the room (but adequate for the situation) iv) with strict adherence to infection control precautions and hand disinfection (see Procedure) DISTRIBUTION: Administration (Master) Nursing Infection Control Cardiorespiratory Food & Nutrition Service Pharmacy Environmental Service DI Laboratory LUK:aa POLICY & PROCEDURE MANUAL: NO. PAGE 3 OF 8 DATE: REV. DATE INFECTION CONTROL SECTION: VI - Significant Organisms APPROVED BY: POLICY PROCEDURE June 2003 GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH HIGH RISK PATIENTS 2.0 PROCEDURE: 2.1 FOR ALL NON-SARS PATIENTS: Personal Protective Equipment i) For emergency endotracheal intubation of patients, each patient unit will have: - a manual resuscitation bag with bacterial/viral filter in-line suction catheters intubation equipment, and full protective apparel (see ii below) for the individual performing the intubation, and for all other individuals in the room. ii) All individuals involved in performing high risk procedures (intubation, cardiopulmonary resuscitation interventions bronchoscopy etc.) will wear full protective apparel. This includes an N95 mask, a gown, gloves, eye protection (goggles), and full-face/head protection (full face Shield). iii) Protective apparel will be removed carefully at the end of the procedure to reduce the risk of contamination and reaerosolization of droplets (see Appendix IV). Note: Suctioning may be performed in the normal fashion in small children. Procedures i) ii) Nebulized therapies should be avoided. Respiratory medications will be delivered using the metered dose inhaler and aerochamber, when possible. The need for chest physiotherapy must be carefully assessed; recognizing that cough-inducing procedures may increase the risk of transmission. GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH PATIENTS IN CRITICAL CARE AREAS PAGE 4 OF 8 Procedures (con't) iii) Oxygen will be delivered DRY avoiding nebulized humidity. Maximum flow rate for nasal prongs will be 6 litres per minute. iv) If a patient requires up to 50% oxygen by mask, use a ventimask. v) If a patient required more than 50% oxygen, then the respiratory therapist (RT) must be notified. The nebulizer system will be emptied of the water from the prefilled water bottle. The water bottle will remain DRY. The RT will monitor and wean the patient to nasal prongs as soon as the patient can tolerate this. vi) Patients will receive frequent mouth care. vii) Patients with tracheostomies will be provided with humidity. viii) Patients who require oxygen greater than 50% must be referred to RT for set up and ongoing monitoring. ix) Non-invasive ventilation (CPAP/BiPAP) should be avoided. If ventilation is essential for the patient, the patient will be screened in consultation with the physician and infection control to ensure that a diagnosis of SARS has been ruled out. The procedure will be performed in a private room, when at all possible (Note: in ER, BiPAP will continue to be done in the trauma room with curtains closed, for patients diagnosed with Congestive Heart Failure ) Note: Children may receive nebulized therapy if MDI is not deemed to be appropriated. Full protective apparel must be worn by all persons in the room. For children, oxygen should be humidified as usual. 2.2 FOR SARS PATIENTS: See Appendix III for Protected Code Blue (sudden cardiorespiratory arrest in SARS patients) 1. Aerosol-generating and/or cough inducing procedures may be performed on patients who may have SARS only when deemed absolutely necessary by the attending physician and documented by him/her in the patient's chart. 2. The following procedures should not be performed on a routine basis on known, suspected or R/O SARS patients. a. Bronchoscopy b. Sputum induction c. Aerosol theapy (includes O2 aerosol and medicated aerosol) d. Non-invasive CPAP or BiPAP GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH PATIENTS IN CRITICAL CARE AREAS PAGE 5 OF 8 FOR SARS PATIENTS IN ALL CRITICAL CARE AREAS (Con't) 3. Equipment On all units that have designated SARS rooms (ER, ICU, Medical unit, Surgical unit and SARS unit) the following equipment must be included in the arrest (crash) cart: - manual resuscitation bag with bacterial/viral filter - in-line suction catheters - Personal protection system (PPS) or Positive Airway Pressure Respirator (PAPR) for 4 individuals - personal protective equipment (This includes gowns and/or front zip coveralls, gloves, full- face/head protection (face shields, goggles, beard hoods, caps and N95 masks) for Unit responders 4. Intubation and Bronchoscopy: Personal Protective Equipment: i) Those performing or assisting with the intubation will wear full personal protective equipment that provides full head, face and neck protection (see Appendix I and Appendix II). Personnel: i) ii) The most experienced staff members available will perform intubations and brochoscopies. The number of persons in the room will be kept to a maximum of 2-4 persons. Procedure: i) The procedure will be done in a negative pressure room. If one is unavailable, it must be done in a private room with the door closed. ii) After hand-washing and prior to entering the room, the individuals involved in the procedure will apply the personal protection system (PPS) as outlined in printed instructions (see Appendix V) iii) Staff in the room during the intubation must apply the personal protection system (PPS) (see Appendix V) iv) The intubation will be done while the patient is sedated and paralysed if medical condition permits GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH PATIENTS IN CRITICAL CARE AREAS PAGE 6 OF 8 FOR SARS PATIENTS IN ALL CRITICAL CARE AREAS (Con't) Procedure (con't): v) The ventilator and in-line suction device will be in the patient room to reduce time needed for bag ventilation and disconnecting bag from the endotracheal tube suctioning. vi) Protective apparel must be removed carefully at the end of the procedure to reduce the risk of contamination and reaerosolization of droplets (see Appendix V). vii) Minimize staff exposure by limiting staff re-entry into the room for approximately 2 hours post-procedure. viii) Other procedures requiring prolonged exposure to the patient (e.g. central line insertion) must be avoided until the room can be thoroughly cleaned (i.e. excess medications must be discarded at the end of any high risk procedure, immediate clean up of room and equipment must be done in such a way as to reduce the re-release of aerosols, contaminated equipment /surfaces must be discarded/disinfected and cleaned before room is left and potentially contaminated surfaces in the room must be wiped with a hospital-approved (eg. Enviro 256) disinfectant). ix) Critical care areas will preassemble medication/equipment for intubations performed in a SARS patient room. The preassemble kit will be in a disposable or easily cleaned container. Cleaning: i) ii) iii) iv) v) Excess medication s will be discarded at the end of the procedure Immediate clean up of room and equipment must be done slowly and in such a way as to reduce the re-release of aerosols. Staff performing the procedure must ensure that contaminated equipment and surfaces are discarded/disinfected and cleaned before leaving the room. Nursing staff are responsible for informing housekeeping whenever their services are required and for indicating what supplies/equipment can be discarded and what can be cleaned disinfected, and or sterilized for reuse. Potentially contaminated surfaces in the room will be wiped with hospital-approved disinfectant. GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH PATIENTS IN CRITICAL CARE AREAS 3. PAGE 7 OF 8 Management of SARS Patients on Mechanical Ventilation Note: Infectious respiratory secretions from SARS patients will contaminate respiratory equipment and be expelled into the surrounding environment. Procedure: i) ii) iii) iv) v) vi) vii) viii) Ventilators A hydrophobic submicron filter will be placed between the endotracheal tube and the ventilator circuit tubing. If possible, ventilators with built in bacterial/viral filters in the expiratory circuit will be used. If this is not possible, such a filter will be placed in the expiratory circuit of the ventilator Filters will be changed when fluid build-up impedes ventilation (at least every 24 hours) Disposal of filters will be considered a high-risk exposure and staff must protect themselves using full personal protective equipment following the maximal precautions Filters and respiratory circuits for known SARS cases must be single use and disposed of after use. Filters are to be bagged, sealed and then placed in a biohazardous bag for disposal. Heated wire circuits will be used on both the inspiratory and expiratory sides of the circuit. A water trap/filter combination will be placed at the end of the expiratory circuit Manual Resuscitation Bags: i) ii) iii) iv) v) vi) A Bacterial/Viral (B/V) filter will be attached to any manual resuscitation bagging device prior to its use on a patient A hydrophobic submicron filter must be placed between the endotracheal/tracheostomy tube and the bag when bagging an intubated patient B/V filters should be changed when fluid buildup impedes ventilation (at least every 24 hours). Disposal of filters is considered a high-risk exposure and staff will protect themselves following maximum precautions using full SARS protective equipment B/V filters will be bagged, sealed, and then placed in a biohazardous bag for disposal Equipment used for manual bagging will be disposed of after use, not cleaned. GUIDELINES FOR HIGH RISK PROCEDURES WHEN DEALING WITH PATIENTS IN CRITICAL CARE AREAS 2.3 PAGE 8 OF 8 PATIENTS WITH RESPIRATORY SYMPTOMS OR UNEXPLAINED FEVER AND UNKNOWN SARS RISK Treat as SARS until another diagnosis is confirmed. Follow all policies a s described in 2.2 until that time. 2.4 PATIENTS WITH NO RESPIRATORY SYMPTOMS OR WITH RESPIRATORY SYMPTOMS/FEVER DUE TO A KNOWN CAUSE OTHER THAN SARS Treat as non-SARS patients. ASSESSMENT: The Infection Control Co-ordinator, Nurse Managers and Department Managers will monitor activities and review all cases of SARS to ensure 100% compliance. DISTRIBUTION: Administration (Master) Nursing Infection Control Cardiorespiratory Food & Nutrition Service Pharmacy Environmental Service DI Laboratory LUK:aa Reference: SARS Provincial Operations Centre: Directives to All Ontario Acute Care Facilities for High-Risk Procedures, June 16, 2003. Appendix I PERSONAL PROTECTIVE EQUIPMENT For All Adult Intubations: N95 mask Gown Gloves that come up over sleeve of gown Hair/Head cover cap Goggles Full face shield Bacterial viral filter on bag Use in line suction only For SARS (and other communicable airborne/respiratory disease) Intubations: Full head , face and neck protection required; Positive Airway Pressure Respirator (PAPR) or Personal Protective System (PPS) N95 mask Double gown (or hooded coverall) Double gloves that come up over sleeve of gown Hair/Head cover cap (not necessary if hooded coverall worn) Goggles Full face shield Booties Bacterial viral filter on bag Use in line suction only Appendix II Source: Ministry of Health and Long Term Care, SARS Provincial Directives, May 13 & June 16, 2003 Appendix III Protected Code Blue To prevent the spread of communicable respiratory diseases to Health Care Workers, SARS precautions are essential and include eye protection (face shield and goggles), N95 mask, double gown and double gloves. However, in certain high-risk situations, such as cardiorespiratory failure requiring airway management, these may not be sufficient and a "Protected Code Blue" will be called. The Protected Code Blue (PCB) Team is an in-hospital team which consists of designated individuals, at least one of whom is highly skilled in intubation and resuscitation measures: 1. Physician (staff emergologist, Intensivist, Anaesthetist) 2. RT 3. RN from ICU 4. RN from ER A number of PCB Teams (consisting of 4 individuals in each team) will be established by the hospital. Members who are physicians will be selected by the Chiefs of the Emergency, Family Practice and Surgery Departments. Members who are RNs will be designated by the Nurse Manager of the ICU/ER. All Respiratory Therapists will be on the PCB Team. All designated Protected Code Blue Team members will receive special training (provided by the hospital initially and on an annual basis) and are expected to consistently adhere to skills and attend opportunities to maintain skills. A Protected Code Blue Team will be available in hospital 24/7 during times of serious regional outbreaks such as SARS, or if a patient is admitted with a known high risk communicable respiratory disease. During outbreaks with potential for large numbers of patients, the core PCB Teams will train staff in high risk areas such as emergency, ICU and affected medical and surgical units and operating room staff to assist in the PCB. Ideally, such patients should be placed in the hospital rooms with negative pressure, but may arrive unexpectedly in the emergency department in need of life saving care after being transported by family or paramedics. Each of these situations poses significant risk to all involved and has the potential to rapidly spread the disease. The following procedures must be adhered to: 1. Equipment ER, ICU, Medical, Surgical and SARS Unit must have crash carts which include: i. Manual resuscitation bag with bacterial/viral filter ii. In-line suction catheters iii. Personal Protective System (PPS) or Positive Airway Pressure Respirator (PAPR) 2. Preparation: Consider early ICU transfer or preferably transfer to another facility when deteriorating (50% O2 necessary) Consider early controlled intubation when patient's respiratory status deteriorates Keep all non-essential staff outside room All team members and unit staff must have completed fit test for N95 mask All staff involved with intubation procedures will have completed training for application and removal of PPS or PAPR All staff involved with a PCB will be familiar with the "Protected Code Blue" Protocol 3. Personnel (Protected Code Blue Team): "airway expert" physician ((staff emergologist, Intensivist, Anaesthetist) Respiratory Therapist 2 Trained ICU/ER RNs "Coach" Individual who is trained to assist with donning and removal of PPE and room entry/exit procedures (Unit Manager or designate, Unit staff member - first responder) This person must use checklist to ensure all steps are followed. All staff in vicinity of the patient's room must wear full SARS protective apparel. 4. Procedure: a) First Responder (First person to recognize non-responsiveness or cardiorespiratory arrest) i. Likely Wearing Full Personal Protective Equipment but no PPS ii. Must not perform high risk procedures (e.g. bag valve mask ventilation/intubation) or be present in the room when these take place if not wearing fPPS iii. Call "Protected Code Blue" iv. Puts N95 mask on patient v. Attaches cardiac monitor, if available; defibrillates if indicated (if trained) vi. If no pulse, performs chest compressions vii. Must leave room when PCB Team arrives viii. Gives report on leaving room ix. Assists dressing team in appropriate PPS as required x. Prepares any drugs or equipment requested b) PCB i. ii. iii. iv. Team Member - #1 Wears PPS Takes report and assumes responsibility Attaches cardiac monitor if not already done; defibrillates, if indicated Continues compressions, if indicated c) PCB i. ii. iii. iv. v. Team Member - #2 Wears PPS Prepares BVM with exhalation filter and intubation equipment If airway expert is not present, initiates BVM ventilation Prepares for intubation Assists with intubation d) PCB i. ii. iii. iv. Team Member - #3 Wears PPS Prepares appropriate drugs Administers appropriate drugs Records events e) PCB Team Member - #4 i. Wears PPS ii. Performs intubation iii. Provides ACLS assistance as directed by Team Leader 5. Termination: If resuscitation is successful, a member of the PCB Team must remain with the patient until transfer to another area of the hospital or to another hospital if possible. If there is a prolonged delay in moving the patient, this Team member must have back-up. Precautions for patient movement such as plastic tent over stretcher, etc. will be at the discretion of the PCB Team. Consideration should be given to termination of resuscitative attempts at the time survival is deemed to be futile (e.g. unwitnessed arrest, asystole) as outcome of resuscitation is inversely proportional to the length of time of resuscitation, and the risk to the providers increases. Reference: SARS Provincial Operations Centre: Directives to All Ontario Acute Care Facilities. May 13 & May 16, 2003. Protected Code Blue There are numerous infection control concerns that arise during acute resuscitation of patients, especially those under SARS precautions. Resuscitation requires performance of high-risk procedures (airway management - intubation, chest tube insertion etc) Time needed to put on additional personal protective equipment may introduce delays in response. The need to provide best care for the patient must be integrated with the need to protect health care workers. To prevent the spread of communicable respiratory diseases to Health Care Workers, additional personal protective equipment is required to be worn while performing high-risk procedures on high risk patients. SARS precautions are essential and include eye protection (face shield and goggles), N95 mask, double gown and double gloves. However, in certain high risk situations, such as cardiorespiratory failure requiring airway management, these may not be sufficient and a Protected Code Blue Team will be called. (PCB) Team is an in-hospital team which consists of designated individuals, at least one of whom is highly skilled in intubation and resuscitation measures: 5. Physician (staff emergologist, Intensivist, Anaesthetist) 6. RT 7. RN from ICU 8. RN from ER A number of PCB Teams (consisting of 4 individuals in each team) will be established by the hospital. Members who are physicians will be selected by the Chiefs of the Emergency, Family Practice and Surgery Departments. Members who are RNs will be designated by the Nurse Manager of the ICU/ER. All Respiratory Therapists will be on the PCB Team. All designated Protected Code Blue Team members will receive special training (provided by the hospital initially and on an annual basis) and are expected to consistently adhere to skills and attend opportunities to maintain skills. A Protected Code Blue Team will be available in hospital 24/7 during times of serious regional outbreaks such as SARS, or if a patient is admitted with a known high risk communicable respiratory disease. During outbreaks with potential for large numbers of patients, the core PCB Teams will train staff in high risk areas such as emergency, ICU and affected medical and surgical units and operating room staff to assist in the PCB. Ideally, such patients should be placed in the hospital rooms with negative pressure, but may arrive unexpectedly in the emergency department in need of life saving care after being transported by family or paramedics. Each of these situations poses significant risk to all involved and has the potential to rapidly spread the disease. The following procedures must be adhered to: 5. Equipment ER, ICU, Medical, Surgical and SARS Unit must have crash carts which include: iv. Manual resuscitation bag with bacterial/viral filter v. In-line suction catheters vi. Personal Protective System (PPS) or Positive Airway Pressure Respirator (PAPR) 6. Preparation: Consider early ICU transfer or preferably transfer to another facility when deteriorating (50% O2 necessary) Consider early controlled intubation when patient's respiratory status deteriorates Keep all non-essential staff outside room All team members and unit staff must have completed fit test for N95 mask All staff involved with intubation procedures will have completed training for application and removal of PPS or PAPR All staff involved with a PCB will be familiar with the "Protected Code Blue" Protocol 7. Personnel (Protected Code Blue Team): "airway expert" physician ((staff emergologist, Intensivist, Anaesthetist) Respiratory Therapist 2 Trained ICU/ER RNs "Coach" Individual who is trained to assist with donning and removal of PPE and room entry/exit procedures (Unit Manager or designate, Unit staff member - first responder) This person must use checklist to ensure all steps are followed. All staff in vicinity of the patient's room must wear full SARS protective apparel. 8. Procedure: f) First Responder (First person to recognize non-responsiveness or cardiorespiratory arrest) xi. Likely Wearing Full Personal Protective Equipment but no PPS xii. Must not perform high risk procedures (e.g. bag valve mask ventilation/intubation) or be present in the room when these take place if not wearing fPPS xiii. Call "Protected Code Blue" xiv. Puts N95 mask on patient xv. Attaches cardiac monitor, if available; defibrillates if indicated (if trained) xvi. If no pulse, performs chest compressions xvii. Must leave room when PCB Team arrives xviii. Gives report on leaving room xix. Assists dressing team in appropriate PPS as required xx. Prepares any drugs or equipment requested g) PCB Team Member - #1 v. Wears PPS vi. Takes report and assumes responsibility vii. viii. Attaches cardiac monitor if not already done; defibrillates, if indicated Continues compressions, if indicated h) PCB vi. vii. viii. ix. x. Team Member - #2 Wears PPS Prepares BVM with exhalation filter and intubation equipment If airway expert is not present, initiates BVM ventilation Prepares for intubation Assists with intubation i) PCB v. vi. vii. viii. Team Member - #3 Wears PPS Prepares appropriate drugs Administers appropriate drugs Records events j) PCB Team Member - #4 iv. Wears PPS v. Performs intubation vi. Provides ACLS assistance as directed by Team Leader 5. Termination: If resuscitation is successful, a member of the PCB Team must remain with the patient until transfer to another area of the hospital or to another hospital if possible. If there is a prolonged delay in moving the patient, this Team member must have back-up. Precautions for patient movement such as plastic tent over stretcher, etc. will be at the discretion of the PCB Team. Consideration should be given to termination of resuscitative attempts at the time survival is deemed to be futile (e.g. unwitnessed arrest, asystole) as outcome of resuscitation is inversely proportional to the length of time of resuscitation, and the risk to the providers increases. Reference: SARS Provincial Operations Centre: Directives to All Ontario Acute Care Facilities. May 13 & May 16, 2003.