CHAPTER 40 - Nursing Pharmacology
advertisement

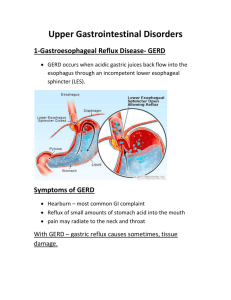
CHAPTER 40 DRUGS FOR PEPTIC ULCER DISEASE LEARNING OUTCOME 1 Describe major anatomical structures of the upper gastrointestinal tract. Concepts 1. The digestive system consists of two basic anatomical divisions: the alimentary canal and the accessory organs. The accessory organs of the digestive system are the salivary glands, liver, gallbladder, and pancreas. (Figure 40.1 illustrates the digestive system.) The digestive system is responsible for breaking down food, absorbing nutrients, and eliminating wastes. A mucosa layer lines the alimentary canal and provides a surface area for breakdown and absorption of food. Peristalsis is the name for the rhythmic contractions of the smooth muscle in the gastrointestinal tract. 2. The stomach contains two muscular rings. First, the cardiac sphincter keeps food from moving back up the esophagus. The pyloric sphincter regulates the flow of food out of the stomach into the small intestine. The stomach’s chief cells secrete enzymes, and its parietal cells secrete hydrochloric acid. Both of these accelerate the process of chemical digestion. A thick mucous layer and bicarbonate ion protect the stomach mucosa from the damaging effects of the acid. (Figure 40.2 illustrates the stomach’s defenses.) Figure 40.1 The Digestive System Figure 40.2 Natural Defenses Against Stomach Acid LEARNING OUTCOME 2 Identify common causes, signs, and symptoms of peptic ulcer disease and gastroesophageal reflux disease. Concepts 1. The term peptic ulcer refers to a lesion located in either the stomach (gastric) or small intestine (duodenal). Peptic ulcer disease is associated with the following risk factors: close family history of PUD blood group; smoking tobacco; beverages and food containing caffeine; drugs, particularly glucocorticoids and nonsteroidal anti-inflammatory drugs (NSAIDs), including aspirin; excessive psychological stress; infection with Helicobacter pylori. The primary cause of PUD is infection by the gram-negative bacterium Helicobacter pylori. Secondary factors include secretion of excess gastric acid and hyposecretion of adequate mucous protection. The characteristic symptom of duodenal ulcer is a gnawing or burning, upper abdominal pain that occurs 1 to 3 hours after a meal. The pain is worse when the stomach is empty and often disappears on ingestion of food. Erosion into the mucosa may lead to bleeding that may be evident as either bright red blood in vomit or black, tarry stools. Gastric ulcers are less common than the duodenal type and have different symptoms. Loss of appetite, known as anorexia, as well as weight loss and vomiting are more common. 2. Gastroesophageal reflux disease (GERD) is a common condition in which the acidic contents of the stomach move upward into the esophagus. GERD causes an intense burning (heartburn) sometimes accompanied by belching. In severe cases, untreated GERD can lead to complications such as esophagitis, or esophageal ulcers or strictures. The cause of GERD is usually a weakening of the lower esophageal sphincter. The sphincter may no longer close tightly, allowing the contents of the stomach to move upward when the stomach contracts. GERD is associated with obesity, and losing weight may eliminate the symptoms. Other lifestyle changes that can improve GERD symptoms include elevating the head of the bed, Adams_IRM Ch 40-1 avoiding fatty or acidic foods, eating smaller meals at least 3 hours before sleep, and eliminating tobacco and alcohol use. Figure 40.3 Peptic Ulcer Formation LEARNING OUTCOME 3 Compare and contrast duodenal ulcers and gastric ulcers. Concepts 1. Peptic ulcer disease (PUD) is caused by an erosion of the mucosal layer of the stomach or duodenum. A duodenal ulcer is more common than a gastric ulcer. It occurs most commonly in the 30 to 50 age group. The usual symptom is a gnawing or burning upper abdominal pain from 1 to 3 hours after a meal. The pain is worse when the stomach is empty. Clients also complain of nocturnal pain, nausea, and vomiting. Bleeding may occur and exhibit itself as bright red blood in the vomit or black, tarry stools. 2. Gastric ulcers are the less common type of ulcer. They are more common in the over 60 age group. Symptoms include pain that may be relieved after food or may continue after a meal, anorexia, weight loss, and vomiting. Remissions are infrequent or absent. Gastric ulcers are more commonly associated with cancer and require longer follow-up. LEARNING OUTCOME 4 Describe treatment goals for the pharmacotherapy of gastroesophageal reflux disease. Concepts The treatment of gastroesophageal reflux disease and peptic ulcer disease is similar. The primary goal is to reduce gastric-acid secretion. Classifications of drugs used to treat these problems include H2-receptor blockers, antacids, and proton pump inhibitors. Surgery may be necessary in some cases. LEARNING OUTCOME 5 Identify the classification of drugs used to treat peptic ulcer disease. Concepts Peptic ulcer disease is best treated by a combination of lifestyle changes and pharmacotherapy. Treatment goals are to eliminate infection by H. pylori, promote ulcer healing, and prevent recurrence of symptoms. Drugs used in the treatment of peptic ulcer disease include H2-receptor antagonists, proton pump inhibitors, antacids, antibiotics, and miscellaneous drugs. Ch 40-2 Adams_IRM LEARNING OUTCOME 6 Explain the pharmacologic strategies for eradicating Helicobacter pylori. Concepts The primary goal of treatment for H. pylori is complete eradication of the bacteria. Other treatment goals include interventions that cause the ulcer to heal more rapidly and remain in remission longer. There is a very high reoccurrence of peptic ulcers when H. pylori is not completely eradicated. Infection can remain active for life if not treated. LEARNING OUTCOME 7 Describe the nurse’s role in the pharmacologic management of patients with peptic ulcer disease. Concepts 1. The role of the nurse in the pharmacologic management of peptic ulcer disease involves careful monitoring of a client’s condition and providing education as it relates to the prescribed drug treatment. Obtain baseline medical, surgical, and drug history; lifestyle and dietary habits, including use of herbal or alternative therapies; and a detailed description of symptomology and current therapies. 2. H2-receptor antagonist therapy: Assess the client’s use of OTC formulations to avoid duplication of treatment. If using OTC formulations, clients should be advised to seek medical attention if symptoms persist or reoccur. Persistent epigastric pain or heartburn may be a symptom of more serious disease that requires different medical treatment. IV preparations of H2-receptor antagonists are occasionally utilized. Because dysrhythmias and hypotension have occurred with IV cimetidine, ranitidine (Zantac) or famotidine (Pepcid) are administered if the IV route is necessary. Assess kidney and liver function. Evaluate the client’s CBC for possible anemia during long-term use of these drugs. 3. Proton pump inhibitor therapy for PUD: Proton pump inhibitors are usually well tolerated for short-term use. With long-term use, liver function should be periodically monitored as well as serum gastrin, because oversecretion of gastrin occurs with constant acid suppression. Assess for drug–drug interactions. Proton pump inhibitors will affect the absorption of medications, vitamins, and minerals that need an acidic environment in the stomach. Obtain the client’s history of smoking, because smoking increases stomachacid production. These drugs should be taken 30 minutes prior to eating, usually before breakfast. These drugs may be administered at the same time as antacids. Proton pump inhibitors are often administered in combination with clarithromycin (Biaxin) for the treatment of H. pylori. 4. Antacid therapy for PUD: Obtain a medical history, including the use of OTC and prescription drugs. Assess the client for signs of renal insufficiency; magnesium-containing antacids should be used with caution in these clients. Hypermagnesemia may occur because the kidneys are unable to excrete excess magnesium. Magnesium- and aluminum-based products may cause diarrhea, and those with calcium may cause constipation. Adams_IRM Ch 40-3 LEARNING OUTCOME 8 For each of the classes listed in Drugs at a Glance, know representative drugs, and explain their mechanism of drug action, describe primary actions, and identify important adverse effects. Concepts 1. H2-Receptor Blockers: Prototype drug: ranitidine (Zantac). Mechanism of action: acts by blocking H2receptors in the stomach to decrease acid production. Primary use: to treat peptic ulcer disease. Adverse effects: Although rare, severe reductions in the number of red and white blood cells and platelets are possible; thus, periodic blood counts may be performed. High doses may result in impotence or loss of libido in men. (See Table 40.2.) 2. Proton Pump Inhibitors: Prototype drug: omeprazole (Prilosec). Mechanism of action: reduces acid secretion in the stomach by binding irreversibly to the enzyme H1, K1-ATPase. Primary use: for the shortterm, 4- to 8-week treatment of peptic ulcers and GERD. Adverse effects: generally minor and include headache, nausea, diarrhea, rash, and abdominal pain. The main concern with proton pump inhibitors is that long-term use has been associated with an increased risk of gastric cancer. (See Table 40.1.) 3. Antacids: Prototype drug: aluminum hydroxide (Amphojel). Mechanism of action: neutralizes stomach acid by raising the pH of the stomach contents. Primary use: most effectively used in combination with other anti-ulcer agents for the symptomatic relief of heartburn due to PUD or GERD. Adverse effects: minor; include constipation. (See Table 40.3.) 4. Antibiotics: These drugs are administered to treat H. pylori infections of the gastrointestinal tract. Two or more antibiotics are given concurrently to increase effectiveness and to lower the potential for resis tance. The regimen often includes a proton pump inhibitor and/or bismuth compounds, which inhibit bacterial growth and prevent H. pylori from adhering to the gastric mucosa. 5. Miscellaneous Drugs: Several additional drugs are beneficial in treating peptic ulcer disease. Sucralfate coats the ulcer and protects it from further erosion. Misoprostol inhibits acid and stimulates production of mucus. Pirenzepine inhibits autonomic receptors responsible for gastric-acid secretion. Table 40.1 H2-receptor Antagonists Table 40.2 Proton Pump Inhibitors Table 40.3 Antacids Prototype Drug ranitidine (Zantac) omeprazole (Prilosec) aluminum hydroxide (Amphojel) ANIMATIONS AND VIDEOS Mechanism in Action: Ranitidine (Zantac) Mechanism in Action: Omeprazole (Prilosec) Ch 40-4 Adams_IRM LEARNING OUTCOME 9 Use the nursing process to care for patients who are receiving drug therapy for peptic ulcer disease. Concepts 1. Patients Receiving Pharmacotherapy for PUD or GERD— Assessment: Obtain a complete health history including gastrointestinal, hepatic, renal, respiratory, or cardiovascular disease, pregnancy or breastfeeding. Obtain drug history including allergies, and possible drug interactions. Obtain a history of past and current symptoms, noting any correlations between onset or presence of any pain related to meals, sleep, positioning or associated with other medications. Assess client for signs of GI bleeding. Note what measures have been successful to relieve the pain (e.g., eating). Obtain vital signs and weight. Evaluate appropriate laboratory findings (e.g., CBC, platelets, electrolytes, hepatic or renal function studies). Assess level of consciousness. Assess for adverse effects: nausea, vomiting, diarrhea, headache, drowsiness, dizziness. Severe abdominal pain, vomiting, coffee-ground or hematemesis, blood in stool or tarry stools should be reported immediately. 2. Patients Receiving Pharmacotherapy for PUD or GERD— Nursing diagnoses: Acute Pain; Altered Nutrition, Less than Body Requirements; Deficient Knowledge related to drug therapy; Risk for Ineffective Health Maintenance (individual or family; dietary and lifestyle changes). 3. Patients Receiving Pharmacotherapy for PUD or GERD— Planning: The client will experience therapeutic effects (e.g., diminished or absent gastric pain, absence of related symptoms such as bloating or belching); be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). 4. Patients Receiving Pharmacotherapy for PUD or GERD— Implementation: Monitor use of OTC drugs to avoid drug interactions, especially with cimetidine therapy. Monitor client use of alcohol. Discuss possible drug interactions. Institute effective safety measures regarding falls. Explain need for lifestyle changes. Observe client for signs of GI bleeding. Administer H2-receptor blockers should be taken after meals; proton pump inhibitors before meals, antacids 2 hours before or after meals with a full glass of water. Monitor for any severe abdominal pain, vomiting, coffee-ground or hematemesis, blood in stool or tarry stools and report immediately. Monitor periodic hepatic and renal function tests and CBC, platelets, and electrolyte levels. Observe for dizziness and monitor ambulation until effects of drug are known. Instruct patient and/or family in proper self-administration of drug (e.g., during evening meal). 5. Patients Receiving Pharmacotherapy for PUD or GERD— Evaluation: The client will experiences diminished or absent gastric pain, absence of related symptoms such as bloating or belching; be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper self-administration of the medication (e.g., dose, timing, when to notify provider). Adams_IRM Ch 40-5